Abstract
This paper is a comprehensive review of the Doppler waveform appearance of ureteric jets. Six jet waveform patterns have been identified: monophasic, biphasic, triphasic, polyphasic, square and continuous. Details of the physical properties of jet patterns and their changes under various physiological conditions are illustrated. The immature monophasic ureteric jet pattern is common in infancy and early childhood up to around 4 years of age. This pattern is also noted to have a high incidence in older children with urinary tract infection/vesicoureteric reflux, nocturnal enuresis and in other special physiological conditions such as in children undergoing general anaesthesia, in women during pregnancy, and in patients who have had ureteric transplantation. A hypothesis of dual myogenic and neurogenic components is proposed to explain the mode of action of the vesicoureteric junction (VUJ). The implication of this hypothesis is that it alters the scientific basis of the understanding of the VUJ. Furthermore, the application of colour Doppler US to ureteric jets may provide a non-invasive technique to study the physiology or pathophysiology of the VUJ in humans. This might shed light on new novel approaches to the monitoring and treatment of diseases related to VUJ function.
Keywords: Ureteric jet, Vesicoureteric junction, Ultrasound, Doppler, Children
Introduction
When the bolus of urine being transmitted through the ureter reaches the terminal portion, it is ejected forcefully into the bladder through the vesicoureteric junction (VUJ). This creates a jet of urine that can be seen within the urinary bladder during cystoscopy and grey-scale ultrasonography (US). Ureteric jets are also occasionally visible during intravenous urography (IVU) and voiding cystourethrography (VCU).
In 2-D, grey-scale real-time US imaging the jet can be visualized as a stream or burst of low-intensity echoes emerging from the ureteric orifice. Each ureteric jet usually lasts for few seconds and is fast enough to produce a frequency shift; therefore the ureteric jet can be demonstrated by colour Doppler US. Colour Doppler US is in fact the easiest method for demonstrating the jet. It is also amenable to further characterization using a pulse-wave Doppler waveform. The US appearance of the jet has been documented in a number of studies and the jet can be consistently demonstrated in both humans [1, 2] and animals such as the dog [3].
This review is based on a number of previous studies that involve US scanning of a total of 2,128 subjects, which include a normal population of 1,341 subjects. The characteristics of ureteric jets in a normal population of 1,341 subjects are described and the effect of age, gender and bladder-filling (based on a subgroup of 102 normal adult females) are discussed. A summary of jet patterns seen in children with urinary tract infection/vesicoureteric reflux (VUR) (n = 98) [4] and nocturnal enuresis (n = 511) [5] is also presented. Special groups, including pregnant women (n = 107) [6], anaesthetized children (n = 16) [7] and subjects with ureteric transplantation (n = 55) [8] are also discussed to look at changes of ureteric jet patterns under specific physiological conditions. Overall the observations suggest a possible correlation of different jet patterns with functional sphincteric action of the VUJ. A hypothesis of dual myogenic and neurogenic components is proposed to explain the mode of action of the VUJ.
Discussion
Basic ureteric jet patterns on Doppler US
Jequier et al. [9] were the first to describe the ureteric jet. In their study of children, they demonstrated that ureteric jets had both crescendo and decrescendo forms. The jet waveforms ranged from a single to as many as four “humps”. Cox et al. [2] noted that the number of peaks (the “humps” of Jequier et al.) in the ureteric jet varied from one to four while Wu et al. [10] found only two or three peaks. Both the latter studies involved only adults. To the best of our knowledge, ours is the only group that has studied in detail ureteric jet patterns in a cohort of subjects with a wide age range, including a large paediatric population.
Six basic patterns have been identified according to the number of peaks within a single ureteric jet: monophasic, biphasic, triphasic, polyphasic, square and continuous [11] (Fig. 1). Among these, the square and continuous waveforms represent modified waveforms under the state of forced diuresis and they are deliberately avoided in most of the study analysis. The biphasic, triphasic and polyphasic waveforms are grouped under the category of mature complex jets while the monophasic jet is classified as the immature jet. We have shown that the majority of the population have a complex mature waveform of the ureteric jet while the immature monophasic waveform has a significantly higher incidence in young children. This is discussed in more detail below.
Fig. 1.
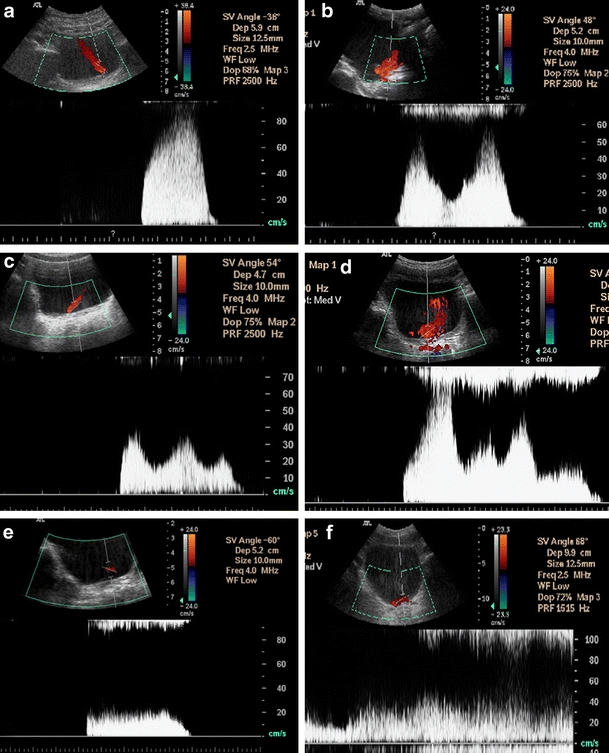
Six patterns of the ureteric jet: a monophasic, b biphasic, c triphasic, d polyphasic, e square, and f continuous
The initial slope, duration and maximum velocity (peak velocity) of the strongest jet are measured on every Doppler waveform for quantification purposes. Significant differences have been found in the above physical parameters among the four jet patterns monophasic, biphasic, triphasic and polyphasic. The monophasic jet has the shortest duration, lowest velocity and smallest initial slope [11].
Occasional modification features of the ureteric jet
Some interesting features have been observed in the jet patterns of some normal subjects. These features include (a) the presence of breaks, (b) a multispike pattern, and (c) change of angle of the jet between the beginning and the end. The number of cases with the above features is too small for statistical analysis; however, we sought to describe them in detail for completeness of the whole spectrum of ureteric jet patterns. These features also provide indirect supportive evidence for the hypothesis of functional sphincteric action at the VUJ and are discussed further in the final section.
Breaks
The presence of break is defined as the total absence of Doppler signal between peaks within a single ureteric jet waveform (Fig. 2). Breaks were identified in 5.7% (149/2,629 ureters) of the study population. Comparing different groups of subjects, it has been found that most breaks occur in adult females when their bladder is at maximum capacity, i.e. when the subjects experience an urgent desire to micturate (33.3% of adult females, P<0.05, chi squared test).
Fig. 2.
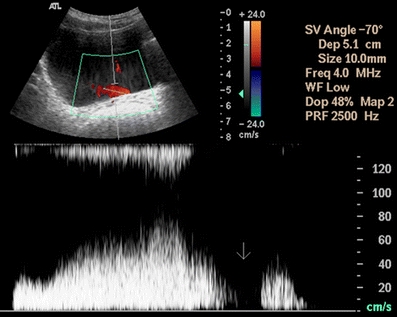
Break within a ureteric jet
Multispike pattern
A multispike pattern is defined as the pulsations noted within a single jet waveform as the result of pulsation transmitted from adjacent arteries (Fig. 3). The incidence of a multispike pattern was found to be 1.9% (50/2,629) in the normal population and is more commonly observed when the bladder is extremely full (forced diuresis).
Fig. 3.
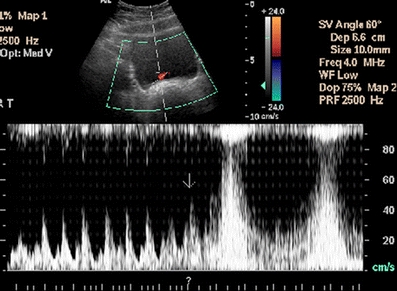
A multispike pattern of a ureteric jet
Change in angle of the jet
A change in the angle within a single jet waveform is illustrated given in Fig. 4. The incidence of change in angle of the ureteric jet in the whole normal population was 4.3% (113/2,629).
Fig. 4.
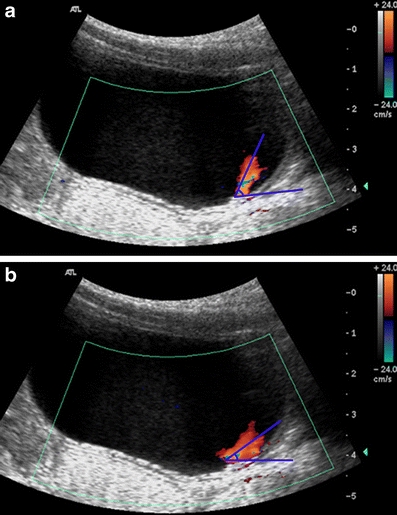
Change in angle of the ureteric jet (a) at the beginning and (b) at the end of the ureteric waveform
Ureteric jet pattern and physical properties of jets in normal subjects
General properties
Direction of flow Dubbins et al. [1] and Elejalde and de Elejalde [12] have found on both US and MRI that the ureteric jet is usually directed anteriorly or anteromedially (with or without crossing of the jets), while others have found ureteric jets directed in a more vertical direction or perpendicular to the bladder base [2, 9, 13–16]. Our US findings are in agreement with the above on the ureteric jet direction of flow.
Mean jet velocity In our studies, the mean velocity of ureteric jets in children was found to be 34.03 cm/s for the monophasic pattern and 61.82 cm/s for the complex pattern (Tables 1 and 2). These values are higher than those reported previously. The mean jet velocity previously reported in children aged from 26 days to 17 years varies between 18 and 31.6 cm/s [9, 17, 18]. The discrepancy between the findings of our study and those of previous studies can be explained by different proportions of children of different ages. The mean velocity in adults in our cohort was found to be 57.65 cm/s for the monophasic pattern and 78.89 cm/s for the complex pattern. These values are similar to those reported previously [2, 18, 19].
Table 1.
Mean values of jet parameters in children and adults with the monophasic pattern
| Right side | Left side | |||||
|---|---|---|---|---|---|---|
| Children | Adults | P value | Children | Adults | P value | |
| Number of ureteric jets | 83 | 18 | 80 | 18 | ||
| Initial slope (cm s−2) | 211.82 | 195.54 | 0.60 | 256.55 | 281.10 | 0.87 |
| Velocity (cm s−1) | 34.03 | 57.65 | <0.01 | 38.66 | 63.93 | <0.01 |
| Duration (s) | 1.17 | 1.91 | <0.01 | 1.17 | 1.90 | <0.01 |
Table 2.
Mean values of jet parameters in children and adults with the complex pattern
| Right side | Left side | |||||
|---|---|---|---|---|---|---|
| Children | Adults | P value | Children | Adults | P value | |
| Number of ureteric jets | 293 | 910 | 296 | 892 | ||
| Initial slope (cm s−2) | 293.32 | 271.21 | 0.09 | 264.48 | 309.13 | 0.13 |
| Velocity (cm s−1) | 61.82 | 79.89 | <0.01 | 61.97 | 73.83 | <0.01 |
| Duration (s) | 5.26 | 6.92 | <0.01 | 5.15 | 7.03 | <0.01 |
Mean jet duration In our studies, the mean jet duration in children was 1.17 s for the monophasic pattern and 5.26 s for the complex pattern. In adults, the mean jet duration was 1.91 s for the monophasic pattern and 6.9 s for the complex pattern (Tables 1 and 2). These values are similar to those reported previously. In adults, previously reported jet durations range from 3.5 to 15 s [2, 16, 18, 20], while in children previously reported mean jet durations in two different series were 2.77±1.53 s [9] and 1.8±0.2 s [18].
Laterality difference in ureteric jets In general, there are no significant differences in waveform pattern, initial slope, velocity and duration of ureteric jets between the right and left sides in both children and adults. This is in agreement with the study of Matsuda and Saitoh [18]. There were two exceptions in our cohort, which might not have clinical significance. Boys were found to have a higher incidence of the monophasic waveform in jets on the left side compared with girls (P<0.01, chi-squared test; Table 3), while adult males have a lower velocity on the left than the right (P<0.01, paired sample T-test) (Table 4).
Table 3.
Waveform patterns in children and adults in relation to sex (total of 2,629 ureteric jets in 1,341 subjects)
| Children | Adults | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | ||||||
| Right | Left | Right | Left | Right | Left | Right | Left | ||
| Number of ureteric jets | 166 | 164 | 211 | 215 | 567 | 560 | 373 | 373 | |
| Pattern | Monophasic | 28 (16.9%) | 19 (11.6%) | 55 (26.1%) | 61 (28.4%) | 14 (2.5%) | 12 (2.1%) | 4 (1.1%) | 6 (1.6%) |
| Biphasic | 54 (32.5%) | 53 (32.3%) | 59 (28.0%) | 63 (30.2%) | 219 (38.6%) | 224 (40%) | 110 (29.5%) | 89 (23.9%) | |
| Triphasic | 54 (32.5%) | 53 (32.3%) | 57 (27.0%) | 54 (25.1%) | 207 (36.5%) | 183 (32.7%) | 134 (35.9%) | 122 (32.7%) | |
| Polyphasic | 29 (17.5%) | 37 (22.6%) | 40 (19.0%) | 34 (15.8%) | 120 (21.2%) | 126 (22.5%) | 120 (32.2%) | 148 (39.7%) | |
| Square | 1 (0.6%) | 1 (0.6%) | 0 (0%) | 0 (0%) | 5 (0.9%) | 13 (2.3%) | 2 (0.5%) | 1 (0.3%) | |
| Continuous | 0 (0%) | 1 (0.6%) | 0 (0%) | 1 (0.5%) | 2 (0.4%) | 2 (0.4%) | 3 (0.8%) | 7 (1.9%) | |
Table 4.
Mean values of jet parameters in children and adults in relation to sex
| Children | Adults | |||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||
| Right | Left | Right | Left | Right | Left | Right | Left | |
| Number of ureteric jets | 165 | 162 | 211 | 214 | 560 | 545 | 368 | 365 |
| Initial slope (cm s−2) | 290.73 | 261.06 | 264.22 | 264.31 | 268.12 | 274.72 | 271.93 | 234.07 |
| Velocity (cm s−1) | 56.31 | 57.02 | 55.72 | 57.60 | 69.94 | 68.84 | 94.01 | 80.82 |
| Duration (s) | 4.64 | 4.56 | 4.21 | 4.20 | 6.37 | 6.43 | 7.52 | 7.69 |
Effect of age on ureteric jets
The distribution of the four basic patterns (monophasic, biphasic, triphasic, polyphasic) among children and adults has been previously described by our group. We have found a strikingly larger proportion of monophasic waveforms in children than in adults in a population of 1,010 subjects [11].
In this review, the above finding is substantiated after expanding the study population to 1,341 normal subjects. Children are found to have a higher incidence of the immature pattern than adults. The incidences of the monophasic waveform in children and adults are 22% and 1.9% on the right side, and 21.1% and 1.9 % on the left side, respectively (P<0.01, chi-squared test; Table 5). This immature pattern occurs constantly in the first 6 months of life [4]. In our previously reported cohort, the immature monophasic pattern in children changed to a mature complex pattern at a mean age of 4.54 years, which probably reflects the mean age of VUJ maturity in general. There is no significant gender difference for the mean age of VUJ maturity in children: boys show VUJ maturity at a mean age of 4.88 years and girls at a mean age of 4.34 years (P>0.05, simple Z test) [21].
Table 5.
Incidence of monophasic jet in children and adults (total of 2,629 ureteric jets in 1,341 subjects). Note that the total number of ureteric jets is less than double the number of subjects as jets in some subjects could not be satisfactorily demonstrated on both sides by Doppler US
| Right side | Left side | |||||
|---|---|---|---|---|---|---|
| Children | Adults | P value | Children | Adults | P value | |
| Number of ureteric jets | 377 | 940 | 379 | 933 | ||
| Monophasic pattern | 83 (22%) | 18 (1.9%) | 0.01 | 80 (21.1%) | 18 (1.9%) | 0.01 |
Adults have higher velocity (P<0.01, independent sample t test) and longer duration of the ureteric jet (P<0.01, independent sample t test) than children in both the monophasic and complex patterns. This finding has also been reported by Matsuda and Saitoh [18], suggesting that the stroke volume of urine in children is less than that in adults. The initial slope of the ureteric jet, however, shows no significant difference between children and adults (all P>0.05, independent sample t test; Tables 1 and 2).
Effect of gender on ureteric jets
In the adult population, males have a higher incidence of the polyphasic waveform than females (P<0.01 for both right and left sides, chi-squared test; Table 3). Male subjects also have a higher velocity (P<0.01 for both sides, independent sample t test) and longer duration of the ureteric jet than females (P<0.01 for both sides, independent sample t test; Table 4). In children, however, no significant differences in velocity, duration, initial slope or number of peaks within a single jet was observed between boys and girls (all P>0.05, chi-squared and independent sample t test; Tables 4 and 5).
Effect of bladder filling status on ureteric jets
In a subgroup of 102 adult females we demonstrated how jet patterns are affected by different bladder filling status. Jet characteristics are compared between two different time intervals: (1) when bladder volume was small and rate of diuresis was low, and (2) when bladder volume was large and rate of diuresis more active. We found that 42.2% of the subjects showed no change in the number of peaks within a single jet waveform, 28.9% showed a decrease and 26.5% showed an increase, and 2.4% had square and continuous jet patterns when the bladder was very full [11]. Among the group with changes in the number of peaks, 3.4% showed a change from a monophasic to a complex pattern and 3.9% showed a change from a complex to a monophasic pattern. In all subjects, the initial slope, velocity and duration of the jet were not affected by different stages of bladder filling (all P>0.05, paired sample t test; Table 6). Even though bladder filling was shown to have little effect on whether the subjects had an immature or complex pattern, we standardized the protocol of bladder filling in all our subsequent Doppler US studies of ureteric jets. Scanning was started in most subjects 20 min after water intake because the jet frequency is reasonably high at that time while the bladder is not yet too distended to make the subject feel uncomfortable.
Table 6.
Mean values of jet parameters in 102 subjects under different stages of bladder filling. Only the jet on the right side is shown for comparison as there was no significant difference between the two sides
| Jet parameter | Bladder status | P value | |
|---|---|---|---|
| Not full | Maximally full | ||
| Initial slope (cm s−2) | 245.27 | 209.44 | 0.39 |
| Velocity (cm s−1) | 62.81 | 58.30 | 0.37 |
| Duration (s) | 6.24 | 6.23 | 0.81 |
Characteristics of ureteric jet under specific physiological conditions
Pregnancy (physiological)
A total of 107 pregnant women and 375 non-pregnant women were investigated. The occurrence of the monophasic waveform was significantly higher in the pregnant women than in the non-pregnant women (18.7%, 41.1% and 1.6% at 20 weeks’ gestation, 32 weeks’ gestation, and 3 months postpartum, respectively, vs. 1.9% in the non-pregnant women) [6].
General anaesthesia (pharmacological)
Our previous study has documented loss of the complex jet pattern after general anaesthesia. A total of 16 children undergoing surgery under general anaesthesia were recruited. Before anaesthesia, 14 of them showed a complex pattern and two showed a monophasic pattern. After anaesthesia, all showed a monophasic waveform [7].
Ureteric transplantation following renal transplantation
Our previous study has shown that transplanted ureters do not have the normal regulatory function at the VUJ, but inherent peristalsis is retained [8]. From a comparison of 55 transplant patients and 817 healthy subjects, we found that the Doppler waveforms of transplanted ureters are distinctly different from those of healthy adult ureters. Basically, only two patterns were identified from transplanted ureters: more commonly a short monophasic waveform (66.1% vs. 2.6% in the health ureters), and less commonly a longer multiphase pattern that does not resemble the patterns of the healthy ureter.
Ureteric jet characteristics in paediatric conditions
Literature review
Previous studies have attempted to relate the ureteric jet seen during IVU in UTI, VUR and bladder neck obstruction. The studies of Kalmon et al. [22] and Nevin et al. [23] have suggested that identification of ureteric jets in IVU studies do not exclude VUR, but Kuhns et al. [24] found an association between the jet sign and absence of VUR. They postulated that the jet sign is produced by peristalsis through the ureteric sphincter. There might be an abnormal increase in the intravesical volume and pressure in the presence of reflux, thus preventing ureteric peristalsis so that no jet can be seen. Eklöf and Johanson [25], however, disagreed with this hypothesis, finding a lower incidence of visible jet in subjects without radiological proof of VUR (5.7% compared with 32% in the study of Kuhns et al.). Although infrequent, significant ipsilateral VUR is observed even when a ureteric jet is detected (10.7% [25] vs. 5.3% [24]). Eklöf and Johanson [25] concluded, therefore, that the low rate of bilateral jets detected on IVU restricts the potential clinical value of jet detection on IVU as an indicator of the absence of gross VUR and that voiding cystourethrography is necessary in the radiological work-up of children with UTI.
Marshall et al. [17] agreed with the view of Kuhns et al. [24] that visualization of a ureteric jet on IVU should not exclude VUR. In addition, they found a strong correlation between relatively lateral positioning of the orifice and the presence of VUR. The mean velocity of the ureteric jet is not related to VUR. A midline-to-orifice distance of >7 mm has been proposed as the cut-off for predicting VUR. The more laterally positioned the ureteric orifice, the more likely it is that reflux will occur [17].
Subsequent studies largely agree with the concept that the ureteric jet is just a normal physiological phenomenon. Gothlin [26] found that the ureteric jet can be identified in subjects with and without UTI. Neither sex nor age has an effect on jet visualization. He therefore concluded that the jet is just a physiological phenomenon and the roentgenographic finding is normal.
There are a number of previous studies evaluating characteristics of the ureteric jet based on Doppler US. Jequier et al. [9] found that the Doppler waveform parameters of jet direction, duration, frequency, velocity and shape do not help in predicting VUR. A lateral ureteric orifice is not seen in normal patients, but is identified in subjects with VUR and other urinary tract disorders.
Gudinchet et al. [27] found no difference between refluxing and non-refluxing ureters with regard to ureteric jet length, angle, and midline-to-orifice distance. They concluded that these parameters cannot be used to predict recurrence of reflux in children after endoscopic subureteric collagen injection (SCIN) for the treatment of VUR.
In two recent studies carried out by our group, we found a high correlation between the immature monophasic jet pattern in children with specific urinary disease entities. The details are discussed in the following sections.
Children with VUR and UTI
Ureteric jets of 241 healthy children and 98 children with UTI were studied. The incidence of monophasic jet (immature pattern) was 29% in healthy children overall, but varied greatly according to age. The immature pattern was universal in the first 6 months of life, but was markedly reduced to below 15% in late childhood. This immature pattern was more commonly seen in children with UTI (73.5%) and VUR (90.5%) than in healthy controls of the same age [4].
Children with nocturnal enuresis
A comparison was made between 511 children presenting with primary nocturnal enuresis and 266 age-matched normal controls. The incidence of immature monophasic jet was significantly greater in enuretic children (19.2% in both sides) than in normal children (6.4% on the right side and 8.3% on the left side). Furthermore, the immature waveform was more commonly seen in the enuretic group with a markedly thickened bladder wall and multiple urodynamic abnormalities [5].
Taking all the observations together, we postulate a hypothesis concerning the mode of action of the VUJ as illustrated in the last section.
Hypothesis of an active sphincter at the VUJ
There has been controversy regarding the anatomy and function of the VUJ for a long time. There are three schools of thought for the antireflux mechanism at the VUJ. In the first theory the VUJ is thought to be governed by a passive valve mechanism dependent on the length and obliquity of the intravesical ureter [28, 29]. In the second theory the VUJ is considered to possess mixed active and passive valvular action. In addition to the anatomical factors, the distal ureter also shows antireflux ureteric peristaltic activity so that contraction of the ureter can prevent retrograde leakage of the intraluminal contents [30–32]. In the third theory the VUJ is considered to be able to act as a sphincter. Noordzij and Dabhoiwala [33] have proposed a sphincteric function for the VUJ which might be activated by the intrinsic muscular meshwork of the trigonal region of the bladder complementing a purely passive antireflux mechanism.
Taking into consideration all the features observed in previous Doppler US studies of the ureteric jet, we postulate that the human VUJ can act as a functional sphincter. Only a monophasic ureteric peristaltic wave is demonstrated by M-mode study of the ureter [11] while the waveform of the ureteric jet emanating from the VUJ becomes more complex in pattern. Because the waveform of the ureteric jet is modified, an active sphincter mechanism is probably present at the VUJ [11]. Because the VUJ shows sphincteric activity, different patterns of ureteric jet can be identified under different physiological and pathological conditions with occasional modifications.
We hypothesize that dual components are present regarding the mode of action in the active functional sphincter. The first component is the “myogenic” (primary or “immature”) and the second component is “neural” (secondary or “mature”). The distal ureteric muscle and possibly part of the detrusor muscle may contribute to the functional sphincteric action at the VUJ. We postulate that the monophasic jet pattern is the result of contraction caused by the myogenic component of the VUJ, while the complex pattern is the result of modulation of the myogenic component of the jet by the neural component in response to the distal intraureteric pressure. The mode of the functional sphincteric action of the VUJ and the subsequent ureteric jet waveform vary depending upon whether or not the neural component is active.
In normal adults and in children reaching a certain age of maturity, the neural component modulates the myogenic component and complex patterns can thus be seen. When the neural component is absent, for example in a small immature child, under general anaesthesia or in certain pathological conditions, only the myogenic component is functioning, and thus the jet pattern reverses to the monophasic pattern.
In renal transplantation patients with ureteric reimplantation, the normal VUJ mechanism in the transplanted ureter is completely lost and the ureteric jet patterns observed are completely different from the patterns obtained from the native VUJ in normal subjects [8]. These distinct patterns could be explained by loss of both the normal myogenic and the neural components of the sphincter action.
Although the neural component governing the ureteric jet pattern is either present (resulting in a complex pattern) or absent (resulting in a monophasic pattern), the characteristics (initial slope, velocity, and duration) of the monophasic and complex pattern within the same age group remain distinct. Although there is a trend for a longer duration and higher peak velocity of the ureteric jet with increasing age, this could be explained by a larger bolus of urine in each jet in adults than in smaller children.
The neural component governing the sphincteric action of the VUJ appears to be affected under various physiological and pathological conditions. We have observed a marked increase in the incidence of a monophasic jet pattern in pregnant women. However, for those pregnant women who retain the complex jet pattern, the characteristics of the complex waveform remain similar to those seen in non-pregnant women [6]. The above observation suggests that the neural mechanism of the VUJ is lost in some pregnant women, but the underlying reason remains obscure.
In subjects undergoing general anaesthesia, the ureteric jet waveforms revert to the monophasic pattern with no difference in initial slope, velocity, and duration of the waveform when compared with the normal population [7]. This suggests that the ureteric jet in anaesthetized subjects is under myogenic influence solely, while the neurogenic influence is temporarily suspended. Histochemical study of the VUJ [34] has shown the muscular components of the VUJ to be innervated by both adrenergic and cholinergic nerves. However, because several drugs were simultaneously administered during general anaesthesia in our small cohort, the exact pharmacological action of these drugs on the neurogenic pathway could not be clearly determined.
The presence of VUR is highly correlated with the immature monophasic waveform [4]. This observation suggests that the complex jet pattern is associated with a more efficient antireflux mechanism than the simple monophasic waveform that is more primitive or immature. In those children with UTI, but without VUR, a high correlation with the immature monophasic pattern is still observed. It is not clear whether the monophasic pattern is a risk factor for or the consequence of UTI. However, the association of the monophasic jet waveform with VUR and UTI might partially explain why pregnant women with a higher incidence of the monophasic jet pattern are also more prone to VUR and UTI [4]. A higher incidence of the immature jet pattern is also found in children with nocturnal enuresis [5]. This suggests that there is a lower level of maturity of the VUJ in a proportion of enuretic children. This group of children also has more deranged parameters on urodynamic studies.
The hypothesis of dual components in the sphincteric action of the VUJ might also help explain some of the jet phenomena that we have described previously. The multispike pattern in the ureteric jet resulting from pulsations transmitted from adjacent arteries could probably be explained by premature relaxation of the VUJ that precedes the ureteric jet proper so that the transmitted arterial pulse becomes dominant. Premature relaxation of the VUJ is also likely to be governed by the neural mechanism seen in forced diuresis.
The modification involving breaks in the jet is predominantly observed when the bladder is maximally full. Under these circumstances the intravesical pressure would be very high, which might impose a countering effect on the pressure wave of the ureteric jet emitted from the VUJ. Breaks might therefore appear within the jet waveform when the jet velocity drops significantly to zero flow on entering the bladder.
In summary, based on all the above observations, we postulate that the human VUJ can act as a functional sphincter with two possible components: (1) a myogenic component which has a simple “open and close” action that gives rise to the monophasic jet pattern, and (2) a neural component that modulates the monophasic waveform into a more complex pattern. Further anatomical study to determine the exact nature of the sphincteric muscle governing VUJ function is warranted. The major implication of this overview of ureteric jet patterns is a change of concept for the human VUJ. Rather than being a passive valve, the VUJ functions as an active sphincter. This might lead to a novel approach to the management of VUR, UTI and enuresis in children which could replace traditional treatment.
Conclusion
This review has provided a comprehensive understanding of the physiological pattern of ureteric jets and contributes to our knowledge of the pathophysiology of urinary dysfunction in disease entities such as UTI, VUR and primary enuresis. The application of this technique in future studies might lead to novel approaches to the monitoring and prognosis of these conditions and more evidence-based treatment of related diseases.
References
- 1.Dubbins PA, Kurtz AB, Darby J et al (1981) Ureteric jet effect: the echogenic appearance of urine entering the bladder. Radiology 140:513–515 [DOI] [PubMed]
- 2.Cox IH, Erickson SJ, Foley WD et al (1992) Ureteric jets: evaluation of normal flow dynamics with color Doppler sonography. AJR 158:1051–1055 [DOI] [PubMed]
- 3.Lamb CR, Gregory SP (1994) Ultrasonography of the ureterovesical junction in the dog: a preliminary report. Vet Rec 134:36–38 [DOI] [PubMed]
- 4.Leung YF, Metreweli C, Yeung CK (2002) Immature ureteric jet Doppler patterns and urinary tract infection and vesico-ureteric reflux in children. Ultrasound Med Biol 28:873–878 [DOI] [PubMed]
- 5.Leung VY, Chu WC, Yeung CK et al (2006) Ureteric jet Doppler waveform and bladder wall thickness in children with nocturnal enuresis. Pediatr Res 60:582–586 [DOI] [PubMed]
- 6.Leung YF, Metreweli C (2002) Doppler waveform of the ureteric jet in pregnancy. Ultrasound Med Biol 28:879–884 [DOI] [PubMed]
- 7.Leung VY, Metreweli C, Yeung CK et al (2003) Ureteric jet in the anaesthetised child. Ultrasound Med Biol 29:1237–1240 [DOI] [PubMed]
- 8.Leung YF, Metreweli C (2002) Ureteric jet in renal transplantation patient. Ultrasound Med Biol 28:885–888 [DOI] [PubMed]
- 9.Jequier S, Paltiel H, Lafortune M (1990) Ureterovesical jets in infants and children: duplex and color Doppler US studies. Radiology 175:349–353 [DOI] [PubMed]
- 10.Wu CC, Yao WJ, Lin F Jr et al (1995) Spectral analysis of ureteral jets by color Doppler ultrasonography: a preliminary uretero-dynamic study. J Med Ultrasound 3:64–69
- 11.Leung YF, Metreweli C, Yeung CK (2002) The ureteric jet Doppler waveform as an indicator of vesicoureteric sphincter function in adults and children. An observational study. Ultrasound Med Biol 28:865–872 [DOI] [PubMed]
- 12.Elejalde BR, de Elejalde MM (1983) Ureteral ejaculation of urine visualized by ultrasound. J Clin Ultrasound 11:475–476 [DOI] [PubMed]
- 13.Burge HJ, Middleton WD, McClennan BL et al (1991) Ureteral jets in healthy subjects and in patients with unilateral ureteral calculi: comparison with color Doppler US. Radiology 80:437–442 [DOI] [PubMed]
- 14.Sweet CS, Silbergleit R, Sanders WP (1995) MRI demonstration of ureteral jet effect in a patient with a spinal ganglioneuroma. Pediatr Radiol 25:574–575 [DOI] [PubMed]
- 15.Patel U, Kellett MJ (1996) Ureteric drainage and peristalsis after stenting studied using color Doppler ultrasound. Br J Urol 77:530–535 [DOI] [PubMed]
- 16.Catalano O, De Sena G, Nunziata A (1998) The color Doppler US evaluation of the ureteral jet in patients with urinary colic. Radiol Med (Torino) 95:614–617 [PubMed]
- 17.Marshall JL, Johnson ND, De Campo MP (1990) Vesicoureteric reflux in children: prediction with color Doppler imaging. Work in progress. Radiology 175:355–358 [DOI] [PubMed]
- 18.Matsuda T, Saitoh M (1995) Detection of the urine jet phenomenon using Doppler color flow mapping. Int J Urol 2:232–234 [DOI] [PubMed]
- 19.Sperandeo M, Varriale A, Sperandeo G et al (1994) Ureteral jet during medical treatment of benign prostatic hypertrophy. Arch Ital Urol Androl 66:45–48 [PubMed]
- 20.Kremer H, Dobrinski W, Mikyska M et al (1982) Ultrasonic in vivo and in vitro studies on the nature of the ureteral jet phenomenon. Radiology 142:175–177 [DOI] [PubMed]
- 21.Leung VY, Chu WC, Yeung CK et al (2007) Gender difference in achieving rate of maturity of the vesicoureteric junction. Pediatr Radiol 37:189–193 [DOI] [PubMed]
- 22.Kalmon EH, Albers DD, Dunn JH (1955) Ureteral jet phenomenon. Stream of opaque medium simulating an anomalous configuration of the ureter. Radiology 65:933–935 [DOI] [PubMed]
- 23.Nevin IN, Cline FA, Haug TM (1962) Forceful ureteral spurt. A common Roentgen manifestation of urinary tract infection in children. Radiology 79:933–938 [DOI] [PubMed]
- 24.Kuhns LR, Hernandez R, Koff S et al (1977) Absence of vesico-ureteral reflux in children with ureteral jets. Radiology 124:185–187 [DOI] [PubMed]
- 25.Eklöf OA, Johanson L (1980) Occurrence of reflux in children with ureteral jets. Pediatr Radiol 10:95–99 [DOI] [PubMed]
- 26.Gothlin J (1964) Ureteral jets. Radiologe 4:398–400 [PubMed]
- 27.Gudinchet F, Oberson JC, Frey P (1997) Color Doppler ultrasound for evaluation of collagen implants after endoscopic injection treatment of refluxing ureters in children. J Clin Ultrasound 25:201–206 [DOI] [PubMed]
- 28.Paquin AJ (1959) Ureterovesical anastomosis: the description and evaluation of a technique. J Urol 82:573–583 [DOI] [PubMed]
- 29.Juskiewenski S, Vaysse P, Moscovici J et al (1984) The ureterovesical junction. Anat Clin 5:251–259 [DOI] [PubMed]
- 30.Hutch JA, Ayres RD, Loquvam GS (1961) The bladder musculature with special reference to the ureterovesical junction. J Urol 85:531–539 [DOI] [PubMed]
- 31.Roshani H, Dabhoiwala NF, Dijkhuis T et al (2000) An in vivo endoluminal ultrasonographic study of peristaltic activity in the distal porcine ureter. J Urol 163:602–606 [DOI] [PubMed]
- 32.Roshani H, Dabhoiwala NF, Dijkhuis T et al (2000) An electro-myographic study of the distal porcine ureter. J Urol 163:1570–1576 [DOI] [PubMed]
- 33.Noordzij JW, Dabhoiwala NF (1993) A view of the anatomy of the ureterovesical junction. Scand J Urol Nephrol 27:371–380 [DOI] [PubMed]
- 34.Gearhart JP, Canning DA, Gilpin SA et al (1993) Histological and histochemical study of the vesicoureteric junction in infancy and childhood. Br J Urol 72:648–654 [DOI] [PubMed]


