INTRODUCTION
Infections with the non-Candida yeast species Trichosporon have been recognised with increasing frequency over the last two decades.1 The majority of cases of invasive trichosporonosis have been reported from neutropenic patients with cancer and the mortality is high (64-83%).2 Other less commonly reported risk groups include patients with organ transplantation (including bone marrow transplantation), burns, prosthetic heart valves, human immunodeficiency virus infection and peritoneal dialysis.1 We report invasive infection with pathogenic Trichosporon species in a patient without these predisposing factors.
CASE REPORT
A seventy-one year old man with a history of non-insulin dependant diabetes mellitus sustained crush injuries to his abdomen, pelvis and lower limbs in a farming accident. Following laparotomy and lower limb vascular repair, he was admitted to the regional intensive care unit (ICU) for ventilatory and inotropic support where he rapidly developed metabolic acidosis, coagulopathy and acute renal failure requiring haemodialysis.
The patient developed a persistent Enterobacter cloacae bacteraemia despite receiving ciprofloxacin with gentamicin and, subsequently, meropenem. In response to continued pyrexia despite maximal antibacterial therapy, liposomal amphotericin B 500mg daily was added (5mg/kg for an approximately 100kg patient). Devitalised tissue on his left leg was a possible persistent septic focus so a left above-knee amputation was performed with demonstrable clinical improvement. Central venous catheters for inotrope infusion and haemodialysis were exchanged regularly in response to the patient's persistent pyrexia and positive blood culture isolates.
Blood taken for culture on the fourth day of amphotericin B therapy, became positive after seventy-two hours incubation with a germ-tube negative yeast, later identified as Trichosporon asahii by API 32C® (bioMerieux, Les Halles, France), with a 99.9% level of identification.
The patient received seven days treatment with liposomal amphotericin B to which the echinocandin antifungal, caspofungin was then added. Ten days after first isolation, on the fourteenth day of antifungal therapy, a second blood culture yielded T. asahii. Subsequently, a reference laboratory performed antifungal susceptibility testing using the microbroth dilution technique according to the guidelines of the National Committee for Clinical Laboratory Standards.3 Minimum inhibitory concentrations (MIC), and susceptibility breakpoints, were reported as amphotericin B 1mg/L (≤ 1); fluconazole 1mg/L (≤ 8); voriconazole 0.03mg/L (≤ 1); caspofungin 16mg/L (≤ 2).
Thirty-two days following admission the patient died as a result of severe systemic inflammatory response syndrome and multiorgan failure.
DISCUSSION
Infections with Trichosporon species have been recognised with increasing frequency over the last two decades.1 They can be found as commensals in the human gut or skin flora and in the environment, which may be relevant to our case given that the initial accident occurred in an agricultural setting.4,5 These non-Candida yeasts have a broad spectrum of clinical manifestations from self-limiting cutaneous infections to life threatening invasive disease in the immunocompromised host.5,6 This is similar to the pattern of disease seen with Candida species.
There is no clear antifungal agent of choice for the treatment of trichosporonosis and in vitro sensitivity assays have not been standardized. There are data to support the use of triazoles (fluconazole, voriconazole) and some authors have recommended combination therapy with amphotericin B.6 We were reluctant to add such an agent as our patient had severe acute liver failure. MIC's for the novel triazole, voriconazole, have been reported between 0.03-1.0, and it has been used to successfully treat disseminated T. asahii infection.7 There is concern however that the cyclodextran excipient of intravenous voriconazole can accumulate in patients undergoing haemodialysis. We gave consideration to using oral voriconazole, but it was felt that poor bioavailability in the setting of multi-organ failure would limit its usefulness.
We believe this to be the first report of T. asahii blood-stream infection not associated with endocarditis in a critically ill, non cancer patient in the UK and one of only a few described worldwide outside of the recognised patient groups listed above. We are unaware of other published cases of confirmed persistent fungaemia, in non cancer patients, despite aggressive antifungal therapy and vigorous attempts to achieve source control.2,8
In light of our experience and the available in vitro data, we conclude that amphotericin B cannot be considered optimal first line therapy for the treatment of invasive trichosporonosis.9 Furthermore, available evidence suggests there is no place for the use of caspofungin in treating trichosporonosis.10 Azole antifungals, alone or in combination, are probably the drug-class of choice for this infection and of these, voriconazole may come to be the preferred agent.11 However its usefulness in the ICU may be limited by patients’ unreliable gastrointestinal function and their frequent dependence on haemodialysis.
Figure 1.
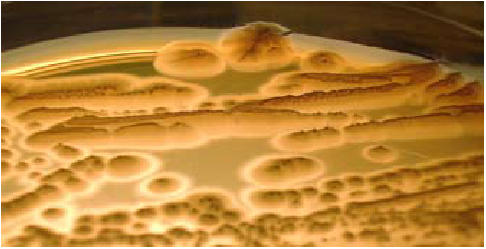
Cream-coloured cerebriform colonies of Trichosporon asahii isolated from our patient on Sabouraud-dextrose agar.
Acknowledgments
We are grateful to the Health Protection Agency Mycology reference laboratory, Bristol, U.K. for antifungal MIC evaluation; and to Sara O'Gorman for photography.
The authors have no conflict of interest.
REFERENCES
- 1.Ebright JR, Fairfax MR, Vazquez JA. Trichosporon asahii, a non-Candida yeast that caused fatal septic shock in a patient without cancer or neutropenia. Clin Infect Dis. 2001;33(5):E28–30. doi: 10.1086/322640. [DOI] [PubMed] [Google Scholar]
- 2.Krcmery V, Jr., Mateicka F, Kunova A, Spanik S, Gyarfas J, Sycova Z, et al. Hematogenous trichosporonosis in cancer patients: report of 12 cases including 5 during prophylaxis with itraconazol. Support Care Cancer. 1999;7(1):39–43. doi: 10.1007/s005200050221. [DOI] [PubMed] [Google Scholar]
- 3.National Committee for Clinical Laboratory Standards. Wayne, PA, USA: National Committee for Clinical Laboratory Standards; 1996. Reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard. NCCLS document M27-A2. [Google Scholar]
- 4.Sugita T, Nishikawa A, Ichikawa T, Ikeda R, Shinoda T. Isolation of Trichosporon asahii from environmental materials. Med Mycol. 2000;38(1):27–30. doi: 10.1080/mmy.38.1.27.30. [DOI] [PubMed] [Google Scholar]
- 5.Chan-Tack KM. Fatal Trichosporon asahii septicemia in a Guatemalan farmer with acute lymphoblastic leukemia. South Med J. 2005;98(9):954–5. doi: 10.1097/01.smj.0000177350.91609.ea. [DOI] [PubMed] [Google Scholar]
- 6.Wolf DG, Falk R, Hacham M, Theelen B, Boekhout T, Scorzetti G, et al. Multidrug-resistant Trichosporon asahii infection of nongranulocytopenic patients in three intensive care units. J Clin Microbiol. 2001;39(12):4420–5. doi: 10.1128/JCM.39.12.4420-4425.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fournier S, Pavageau W, Feuillhade M, Deplus S, Zagdanski AM, Verola O, et al. Use of voriconazole to successfully treat disseminated Trichosporon asahii infection in a patient with acute myeloid leukaemia. Eur J Clin Microbiol Infect Dis. 2002;21(12):892–6. doi: 10.1007/s10096-002-0841-y. [DOI] [PubMed] [Google Scholar]
- 8.Kontoyiannis DP, Torres HA, Chagua M, Hachem R, Tarrand JJ, Bodey GP, et al. Trichosporonosis in a tertiary care cancer center: risk factors, changing spectrum and determinants of outcome. Scand J Infect Dis. 2004;36(8):564–9. doi: 10.1080/00365540410017563. [DOI] [PubMed] [Google Scholar]
- 9.Ramos JM, Cuenca-Estrella M, Gutierrez F, Elia M, Rodriguez-Tudela JL. Clinical case of endocarditis due to Trichosporon inkin and antifungal susceptibility profile of the organism. J Clin Microbiol. 2004;42(5):2341–4. doi: 10.1128/JCM.42.5.2341-2344.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espinel-Ingroff A. Comparison of In vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J Clin Microbiol. 1998;36(10):2950–6. doi: 10.1128/jcm.36.10.2950-2956.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falk R, Wolf DG, Shapiro M, Polacheck I. Multidrug-resistant Trichosporon asahii isolates are susceptible to voriconazole. J Clin Microbiol. 2003;41(2):911. doi: 10.1128/JCM.41.2.911.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]


