Abstract
Objectives To compare mix of patients, scope of practice, and duration of visit in primary care physicians in Australia, New Zealand, and the United States.
Design Comparison of three comparable cross sectional surveys performed in 2001-2. Physicians completed a questionnaire on patients' demographics, diagnoses, and duration of visit.
Setting Primary care practice.
Participants 79 790 office visits in Australia, 10 064 in New Zealand, and 25 838 in the US.
Main outcome measures Diagnostic codes were mapped to the Johns Hopkins expanded diagnostic clusters. Scope of practice was defined as the number of expanded diagnostic clusters accounting for 75% of all managed problems related to morbidity. Exposure to primary care was calculated from duration of visits recorded by the physician, and reports on rates of visits to primary care for each country.
Results In each country, primary care physicians managed an average of 1.4 morbidity related problems per visit. In the US, 46 expanded diagnostic clusters accounted for 75% of problems managed compared with 52 in Australia, and 57 in New Zealand. Correlations in the frequencies of managed health problems between countries were high (0.87-0.97 for pairwise comparisons). Though primary care visits were longer in the US than in New Zealand and Australia, the per capita annual exposure to primary care physicians in the US (29.7 minutes) was about half of that in New Zealand (55.5 minutes) and about a third of that in Australia (83.4 minutes) because of higher rates of visits to primary care in these countries.
Conclusions Despite differences in the supply and financing of primary care across countries, many aspects of the clinical practice of primary care physicians are remarkably similar in Australia, New Zealand, and the US.
Introduction
Previous studies show that the strength of a country's primary care infrastructure is positively associated with health outcomes and negatively associated with healthcare costs.1 In general, these studies have relied on experts to rate the degree to which policies and organisational characteristics of healthcare systems support primary care practice, defined as accessibility, longitudinality, comprehensiveness, coordination, family centredness, and community orientation.2 Limited research has been done on the clinical content and duration of visits in primary care across countries.3 4 We sought to characterise the diagnostic scope of and exposure to primary care in three countries—Australia, New Zealand, and the United States—that vary in the supply of primary care physicians, the accessibility to primary care through health insurance, and the role of primary care physicians as gatekeepers to specialty care.
Of the three countries studied, Australia has the greatest number of primary care physicians per 100 000 population (112) and the largest proportion (56%) of physicians trained in primary care specialties (table 1). In Australia and New Zealand, primary care physicians are trained as general practitioners. In the US, general internists, general paediatricians, and family practitioners all contribute to the pool of primary care physicians.
Table 1.
Characteristics of primary care by country, 2001-2
| Australia | New Zealand | United States | |
|---|---|---|---|
| Primary care physicians/100 000 population | 1125 | 787 | 879 |
| Percentage of primary care physicians | 565 | 427 | 369 |
| Percentage of population uninsured for primary care | 0 | 0 | 1510 |
| Percentage with primary care gatekeeping for specialty care | 100 | 100 | 3811 |
| Mean No of primary care visits/person/year | 5.26 | 3.78 | 1.812* |
*Using methods described by Forrest and Whelan.13
In the US universal health insurance that covers access to primary care is not available for people under 65 years, as it is in New Zealand and Australia. During the study period about 41 million Americans14 (15% of the total population) were uninsured and another 16 million adults aged 19-64 were underinsured.15 These individuals use primary medical care services, but at a lower rate than they would if they had insurance.16 The national insurance benefits in New Zealand and Australia include cost sharing except for some low income patients. A portion of the population has private insurance to supplement public coverage, but private insurance does not typically cover primary care services.
In Australia and New Zealand, primary care physicians serve as gatekeepers who coordinate and manage access to specialists through their referrals. Some health plans in the US require patients to use primary care physicians to access specialty care, but this practice has been decreasing in recent years, and many patients access specialty care services directly.17
We hypothesised that there would be substantial overlap in the practice of primary care across the three countries, but key differences in the US healthcare system would contribute to some observed differences. For example, we expected that the range of problems managed in primary care would be narrower in the US because of the greater proportion of specialist physicians in their healthcare system and more direct access to specialty care for patients. We also expected that differences in the US physician workforce, in combination with a higher proportion of uninsured people, would contribute to a lower per capita exposure time to primary care physicians in the US than in Australia and New Zealand.
Methods
We used three independent nationally representative cross sectional surveys to compare mix of patients, scope of practice, and duration of visit among primary care physicians in Australia, New Zealand, and the US. We used the bettering the evaluation and care of health (BEACH) survey in Australia; the national primary medical care survey (NatMedCa) in New Zealand; and the national ambulatory medical care survey (NAMCS) in the US. The questionnaires include items on whether the encounter is for a new or follow-up patient, patients' demographics and diagnoses, and duration of visit. The reporting periods are spread evenly throughout the year to reflect seasonal differences.
BEACH is a continuous national survey in which a random sample of about 1000 of Australia's 17 500 general practitioners participate each year.18 Participating general practitioners complete (on paper encounter forms) information regarding 100 consecutive encounters with patients. Each general practitioner's encounters are weighted according to their clinical activity as measured through submitted claims for the previous three month period. For this study, we used data from the 12 month period 2001-2.
The NAMCS is a national annual survey of office based practice in the US.19 Physicians are sampled with a multistage probability design that involves primary sampling units, practices within those units, and patients' visits within practices. Depending on the size of their practice, participating physicians contribute anywhere from 20% to 100% of their encounters during the one week study period. For this study, we used the 2001 and 2002 samples and included physicians whose specialties were general internal medicine, general paediatrics, family practice, or general practice. We calculated national estimates using weights that accounted for the complex survey design.
The NatMedCa survey was performed in New Zealand in 2001-2 among a nationally representative probability sample of general practitioners and patients' visits.20 For two periods of one week, each selected general practitioner completed a questionnaire for a 25% systematic sample of patients' visits. The questionnaire was adapted from the NAMCS administered in the US. To obtain a nationally representative sample, the survey sampled geographic locations and sampled general practitioners from locations stratified by type of organisation and by whether the practice was in a rural or urban setting. General practitioners and visits were weighted take account of different sampling probabilities.
Analysis was limited to office based face to face encounters in which the physician recorded one or more diagnosis codes for morbidities treated during the visit. We excluded visits in which physicians recorded only administrative, process, or preventive care codes. Administrative codes are used in the US to indicate a personal or family history of a disease or an abnormal laboratory or other test result. Process codes are used in Australia and New Zealand to record diagnostic and treatment actions such cardiography or immunisation. We intended to describe preventive care practices for activities such as immunisations, routine health supervision, and cancer screening; however preventive care is not well described by diagnostic codes and differences in how preventive care is recorded in the classification systems used across countries made this problematic. Physicians recorded diagnoses in free text and trained coders converted these into the classification system used in that country. In Australia up to four free text diagnoses were classified according to the International classification of primary care, version 2 (ICPC-2).21 In New Zealand up to four diagnoses were classified into READ codes.22 In the US, up to three diagnoses were coded in ICD-9-CM (international classification of disease, 9th revision, clinical modification).23 To create a common taxonomy for this study, we re-assigned all diagnostic codes to an expanded diagnostic cluster. These clusters are clinically homogeneous groups of diagnostic codes that were developed by Johns Hopkins University.24 The original grouping algorithm was developed from ICD-9-CM For this project, three of the authors, who are practising primary care physicians, and a separate primary care physician in Australia, assisted in creating a linkage to the expanded diagnostic cluster taxonomy for READ codes used in New Zealand and ICPC-2 used in Australia. Match rates between diagnostic codes and expanded diagnostic clusters were 100% for the Australia and US datasets and 96% for the New Zealand dataset.
We defined a problem managed as a unique expanded diagnostic cluster within a visit. To characterise the scope of primary care practice in each country, we calculated the minimum number of expanded diagnostic clusters that accounted for 75% of the problems managed in primary care. This provided us with a means to summarise the comprehensiveness of primary care practice in each country without the complicating noise introduced by low frequency problems that skewed the distribution of problems managed in each country. We interpreted the analysis of the 75% of problems managed according to the principle that the higher the number of problems the greater the comprehensiveness of practice.
We recorded duration of visit in minutes of face to face time between a patient and physician. We excluded time spent waiting to see the physician, time receiving care from someone other than the physician, and time in documenting care in the medical record. We calculated the annual per person exposure to primary care for each country by multiplying the average duration times of primary care visits by the average number of primary care visits per person for the same time period derived from separate sources.
We age standardised results for the US and New Zealand to the Australian population using age categories of 0-4, 5-14, 15-25, 25-34, 35-44, 45-54, 55-64, 65-74, and ≥75. Because our parameter of the number of problems managed that comprise 75% of problems seen in primary care was a quartile (75th centile of the distribution of diagnosis), we used a bootstrap method to estimate the confidence interval.25
Results
The surveys included 79 790 office based visits to primary care in Australia, 10 064 in New Zealand, and 25 838 in the US. The excluded visits, in which only an administrative or preventive care code was recorded, ranged from 7% in New Zealand to 21% in the US (table 2). The remaining visits involved the management of at least one medical problem. Patients aged 65 years or older accounted for similar proportions of total visits in each country, but a greater proportion of visits in the US involved children (30%) than in Australia (17%) or New Zealand (27%). Females accounted for more than half of the visits to primary care, and new patients comprised less than 10% of the visits in each country.
Table 2.
Demographics of patients as weighted* percentage of primary care visits by country, 2001-2
| Australia (n=114 402) | New Zealand (n=15 523) | United States (n=42 144) | |
|---|---|---|---|
| Excluded† | 13 | 7 | 21 |
| Visits by patients who are: | |||
| 0-17 years | 17 | 27 | 30 |
| 18-64 years | 60 | 52 | 47 |
| ≥65 years | 23 | 22 | 23 |
| Female | 57 | 57 | 56 |
| New patients | 9 | 8 | 7 |
*Sampling weights that were specific to each country were applied to account for the complex survey designs to obtain national probability estimates of visits to primary care in each country.
†Visits for administrative, process, or preventive care services only.
In each country primary care physicians dealt with an average of 1.4 problems per visit. Those in the US, however, managed a narrower range of problems than their counterparts in New Zealand and Australia. In the US, 46 (95% confidence interval 45 to 47) conditions accounted for 75% of problems managed in primary care compared with 52 (52 to 53) in Australia and 57 (56 to 59) in New Zealand.
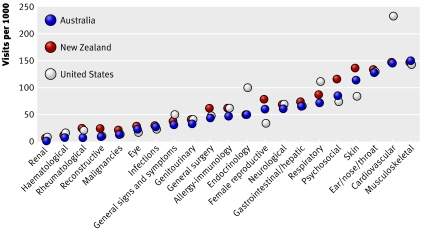
The relative frequency of health problems managed in primary care was similar across the study countries (fig 1). Correlations in the frequencies of managed health problems between countries were 0.87 for the pairwise comparison between US and New Zealand, 0.90 between Australia and the US, and 0.97 between US and Australia. One of the most striking differences was the higher rates of visits for endocrine and cardiovascular problems in the US compared with Australia and New Zealand. Nearly 18 per 1000 visits in the US were for obesity; almost twice the rate for this condition in Australia (11.3) and New Zealand (9.1). This is also reflected in substantially greater rates of visits per 1000 in the US for diabetes (64.0) and hyperlipidaemia (59.2) than in Australia (31.0 and 32.2, respectively) and New Zealand (25.9 and 11.7, respectively).
Fig 1 Age standardised frequency of health problems managed in primary care in Australia, New Zealand, and the US: 2001-2
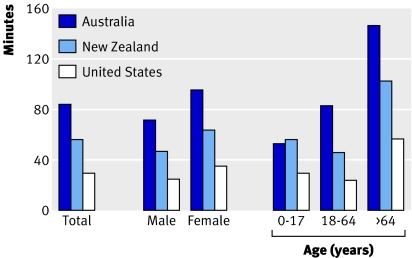
The average duration of a visit was about 10% longer in the US than in Australia and New Zealand. They were 16.5 minutes (16.4 to 16.6) in the US compared with 15.0 minutes (14.3 to 15.6) in New Zealand and 14.9 minutes (14.6 to 15.2) in Australia. Visit lengths were longer in the US for all age and sex groups. Because the average number of primary care visits per capita was greater in New Zealand and Australia, however, the per capita annual exposure to primary care physicians was substantially lower in the US. The mean time spent per year in primary care was 29.7 minutes (29.5 to 29.9) in the US, 55.5 minutes (52.8 to 57.8) in New Zealand, and 83.4 minutes (81.9 to 84.8) in Australia (fig 2).
Fig 2 Mean per capita annual exposure to primary care physicians by country and demographic subgroups: 2001-2
Discussion
Despite differences in the supply and financing across countries, many aspects of the clinical practice of primary care physicians are remarkably similar in Australia, New Zealand, and the US. There is a high level of agreement in primary care across countries in the number of problems that are managed per visit, the types of problems that are managed, and the duration of visits.
Diagnostic scope of practice
The similarity in the types of problems managed within primary care across countries implies that primary care practice is a definable area of clinical work and not merely the activities that are not performed by specialists. The finding that the range is narrower in the US than in Australia and New Zealand, however, also suggests that the comprehensiveness of primary care is influenced at the margin by the amount of specialisation in the healthcare system. The use of specialists is greater in the US than in either Australia or New Zealand.
The high proportion of specialist physicians in the US in combination with the ability of patients to self refer for specialty services results in some patients seeing only specialists for ambulatory care services.26 Our results extend these findings to suggest that the availability of specialist physicians might also contribute to defining the range of problems managed in primary care. For example, compared with Australia and New Zealand, the US has lower rates of visits in primary care for the management of reproductive problems in women. The US is also the only country of the three that provides most women with direct access to gynaecologists. The presence of general internists and general paediatricians among US primary care physicians may contribute to a narrower diagnostic scope of practice in the US. Differences in rates of visits for specific problems, such as cardiovascular disease in the US, might also reflect national differences in the prevalence of conditions or health seeking behaviour. Unfortunately, our data do not allow us to determine this.
Exposure to primary care
The biggest difference in practice across the three study countries is the substantially shorter time per capita in the US. Annually, the average American receives a little more than half the exposure to primary care physicians than people in New Zealand and just over a third of that in Australia. This difference may have real consequences in terms of preventive care and management of chronic conditions. The provision of prevention services recommended by the US Prevention Services Task Force requires an estimated average of 37 minutes a year for children and 40 minutes for adults.27 Not only does the time demand for such services exceed the annual time available to the average American in primary care, it does not consider the average additional need of 20-40 minutes a year for each chronic condition a person may have.28 More than half of US primary care physicians' time is spent on the management of acute conditions, and this role further limits their capacity to meet the prevention and chronic care needs of their patients.29
Of the three countries we studied, only Australia approaches a per capita exposure to primary care that could reasonably be expected to meet patients' demands for preventive and acute and chronic care needs. The severe shortfall of available time in primary care for prevention and chronic care management in the US could partially explain why the US does not have health outcomes that correspond to its overall investment in health care.30
Limitations
Exclusion of visits in which only administrative, process, or preventive care codes were recorded limits our ability to count the amount of preventive care that is actually occurring in primary care. Even with this exclusion, however, we have an accurate estimate of the exposure to primary care by country. This estimate includes all visits, even those in which only preventive, administrative, or process codes would have been recorded.
As with any comparison between countries, our results should be interpreted with caution. Firstly, we looked at only three countries and this limits its generalisability. Secondly, although the data were derived from similar surveys with large samples, there were differences in how some questions were asked and coded. We were careful to consider differences in the surveys and to create common methods of analysis that would limit the introduction of bias, but our results may still include measurement artefact. For example, the US had the highest percentage of visits excluded from analysis because they were coded only with administrative, process, or preventive care codes. These visits may reflect provision of primary medical care services that had they been included would have widened our assessment of the scope of practice in the US relative to Australia and New Zealand. Thirdly, the available cross sectional observational data limit our ability to draw causal inferences and lacked information that would allow us to determine how variation in practice is associated with differences in quality of care. None the less, our study is useful because most previous work has focused on hospital based care and procedures.
Summary
Despite the markedly different approaches countries take towards funding and organising healthcare delivery, a fundamental question remains regarding the role of primary care in a healthcare system.31 One of the current objectives of the UK government is to shift services from hospital based to primary care settings.32 This raises questions about the appropriate balance between services supplied by primary care physicians and specialists. Comparisons between countries offer an opportunity to learn from natural experiments and may provide insights into how primary care can best contribute to equitable, efficient, and effective healthcare systems.
What is already known on this topic
The strength of a country's primary care infrastructure is positively associated with health outcomes and negatively associated with healthcare costs
What this study adds
The number and type of problems managed per primary care visit in Australia, New Zealand, and the United States are similar
Primary care is less comprehensive in the US than in Australia or New Zealand and the average American receives about half the exposure to primary care physicians compared with people in New Zealand and about a third of that of people in Australia
We thank Robin Osborn and her staff at the Commonwealth Fund who encouraged and believed in the value of this international collaboration, Arpita Chattopadhyay for her assistance in developing the program for running the bootstrap analysis, and Glenna Auerback for her editorial assistance. We thank Lisa Valenti for assisting with the analysis of the BEACH data, and Peter Davis, Antony Raymont, Roy Lay-Yee, and the NatMedCa research team for access to their data.
Contributors: All authors contributed to conception, design, analysis, interpretation of data, and drafting and final approval of the article. ABB is guarantor.
Funding: Commonwealth Fund. BEACH 2001-2 was funded by the Australian Government Department of Health and Ageing, AstraZeneca (Australia), Aventis Pharma, Roche Products, Janssen-Cilag, and Merck Sharp and Dohme (Australia). The NatMedCa survey was funded by the Health Research Council of New Zealand. The National Ambulatory Medical Care Survey is administered and maintained by the National Center for Health Statistics of the US Department of Health and Human Services.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy 2002;60:201-18. [DOI] [PubMed] [Google Scholar]
- 2.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83:457-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okkes IM, Polderman GO, Fryer GE, Yamada T, Bujak M, Oskam SK, et al. The role of family practice in different health care systems. J Fam Pract 2002;51:72-3. [PubMed] [Google Scholar]
- 4.Deveugele M, Derese A, van den Brin-Muinen A, Bensing J, De Maeseneer J. Consultation length in general practice: cross sectional study in six European countries. BMJ 2002;325:472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Australian Institute of Health and Welfare. Australia's health 2004: the ninth biennial health report of the Australian Institute of Health and Welfare Canberra: Australian Institute of Health and Welfare, 2004. (AUS 44.)
- 6.Medicine Australia. Medicare benefits schedule group statistics reports Australia: Medicare Australia, 2001-2. www.medicareaustralia.gov.au/statistics/dyn_mbs/forms/mbsgtab4.shtml
- 7.Medical Council of New Zealand. New Zealand medical workforce in 2002 Wellington: Medical Council of New Zealand, 2004
- 8.Sutton F. Population-based funding for primary health care: methods and results Wellington: Health Funding Authority, 2000
- 9.United States General Accounting Office. Physician workforce: physician supply increased in metropolitan and nonmetropolitan areas but geographic disparities persisted 2003. http://frwebgate.access.gpo.gov/cgi-bin/useftp.cgi?IPaddress=162.140.64.21&filename=d04124.pdf&directory=/diskb/wais/data/gao
- 10.Bhandari Shailesh. Health status, health insurance and health services utilization: 2001 Washington: US Census Bureau, 2006. www.census.gov/prod/2006pubs/p70-106.pdf
- 11.Forrest CB. Primary care gatekeeping and referrals: effective filter or failed experiment? BMJ 2003;326:692-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. Ambulatory health care data. Atlanta, GA: Centers for Disease Control and Prevention, 2006. .www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm
- 13.Forrest CB, Whelan EM. Primary care safety-net delivery sites in the United States: a comparison of community health centers, hospital outpatient departments, and physicians' offices. JAMA 2000;284:2077-83. [DOI] [PubMed] [Google Scholar]
- 14.Mills RJ. Health insurance coverage: 2001 Washington, DC: US Dept of Commerce, Economics, and Statistics Administration, US Census Bureau, 2002. www.census.gov/prod/2002pubs/p60-220.pdf
- 15.Schoen C, Doty MM, Collins SR, Holmgren AL. Insured but not protected: how many adults are underinsured? Health Aff 2005;W5289-302. http://content.healthaffairs.org/cgi/reprint/hlthaff.w5.289v1.pdf [DOI] [PubMed]
- 16.Institute of Medicine. Coverage matters: insurance and health care Washington DC: Institute of Medicine, 2001
- 17.Ferris TG, Chang Y, Blumenthal D, Pearson SD. Leaving gatekeeping behind—effects of opening access to specialists for adults in a health maintenance organization. N Engl J Med 2001;345:1312-7. [DOI] [PubMed] [Google Scholar]
- 18.Britt H, Miller GC, Knox S, Charles J, Valenti L, Henderson J, et al. General practice activity in Australia 2001-02 Canberra: Australian Institute of Health and Welfare, 2002. www.aihw.gov.au/publications/gep/gpaa01-02/gpaa01-02.pdf
- 19.National Ambulatory Medical Care Survey (NAMCS). Atlanta (GA): Centers for Disease Control and Prevention, 2007. .www.cdc.gov/nchs/about/major/ahcd/namcsdes.htm
- 20.Ministry of Health. 2004. Family doctors: methodology and description of the activity of private GPs: the national primary medical care survey (NatMedCa): 2001/02. Report 1 Wellington: Ministry of Health. www.moh.govt.nz/moh.nsf/wpg_Index/Publications-Family+Doctors+NatMedCa+Report+One
- 21.Classification Committee of the World Organization of Family Doctors (WICC). ICPC-2: international classification of primary care 2nd ed. Oxford: Oxford University Press, 1998
- 22.De Lusignan S. Codes, classifications, terminologies and nomenclatures: definition, development and application in practice. Inform Prim Care 2005;13:65-9. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. International classification of diseases, ninth revision, clinical modification 2007. www.cdc.gov/nchs/about/otheract/icd9/abticd9.htm
- 24.The Johns Hopkins University ACG case-mix system. 2007. .www.acg.jhsph.edu/ResourceCenter.aspx?Type=Documentation
- 25.Efron B, Tibshirani RJ. An introduction to the bootstrap London: Chapman and Hall, 1994
- 26.Rosenblatt RA, Hart LG, Baldwin LM, Chan L, Schneeweiss R. The generalist role of specialty physicians: is there a hidden system of primary care? JAMA 1998;279:1364-70. [DOI] [PubMed] [Google Scholar]
- 27.Yarnall KSH, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health 2003;93:635-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ostbye T, Yarnall KSH, Krasue KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med 2005;3:209-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stange KC, Zyzanski SJ, Jaen CR, Callahan EJ, Kelly RB, Gillanders WR, et al. Illuminating the “black box.” A description of 4454 patient visits to 138 family physicians. J Fam Pract 1998;46:377-89. [PubMed] [Google Scholar]
- 30.Reinhardt UE, Hussey PS, Anderson GF. Cross-national comparisons of health systems using OECD data, 1999. Health Aff 2002;21:169-81. [DOI] [PubMed] [Google Scholar]
- 31.Bindman AB, Majeed A. Primary care in the United States: organisation of primary care in the United States. BMJ 2003;326:631-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Department of Health. Our health, our care, our say: a new direction for community services London: Department of Health, 2006. www.dh.gov.uk/assetRoot/04/12/74/59/04127459.pdf