Abstract
The proportion of the United States labor force ≥65 years of age is projected to increase between 2004 and 2014 by the passing of age 65 of the large post-World War II baby boom cohorts starting in 2010 and their greater longevity, income, education, and health [Toossi M (2005) Mon Labor Rev 128(11):25–44]. The aging of the U.S. labor force will continue to at least 2034, when the largest of the baby boom cohorts reaches age 70. Thus, the average health and functional capacity of persons age 65+ must improve for sufficient numbers of elderly persons to be physically and cognitively capable of work. This will require greater investments in research, public health, and health care. We examine how disability declines and improved health may increase human capital at later ages and stimulate the growth of gross domestic product and national wealth.
Keywords: disability declines, National long term care survey
Economic growth is determined by physical and human capital inputs and technological innovation (1–3). Developed country human capital dynamics are changing because of (i) population and labor force aging due to life expectancy increases, fertility restrictions, and enhanced education and training needs and (ii) biomedical research, health care, and public health innovations improving health and mental and physical capacity to increasingly late ages (4).
We review how models of human health and longevity dynamics suggest that research stimulates economic growth. These models, based on Romer's theory (5) of the role of research in economic development, involve processes by which research increases the variety of technologies and products in an economy with older technologies giving way to new ones (6). Jones and Williams suggest that social welfare in the U.S. is currently far from optimized because of underinvestment in research (7). The socially and economically optimal level of research investment could be 4 times the current U.S. levels (7). Studies also suggest research investment in Asia now surpasses that of the U.S. and will grow more rapidly (8).
The most valuable new technologies will both improve the elderly's standard of living and increase per capita labor productivity by extending work life and enhancing age-specific physical and cognitive capabilities. Murphy and Topel (9) evaluated the economic consequences of increases in quantity and quality of life. They suggest that the value of health increases for (i) larger populations, (ii) higher incomes, (iii) higher existing levels of health, and (iv) a population age distribution close to that of the age-at-onset of prevalent chronic diseases. They estimated declines in U.S. mortality 1970 to 2000 were worth $95 trillion; $60 trillion after removing health expenditures.
Murphy and Topel (9) concluded that half of the economic benefit of health improvements 1970–2000 were due to reduced cardiovascular disease mortality. Those reductions increase the future value of interventions for other causes of death, raising the value of a person year in 2000 by 18%. For example, cancer mortality rates started to decline in 1990, dropping >10% by 2004. Murphy and Topel estimate that a 1% reduction in cancer mortality has a value of $500 billion; thus, observed cancer mortality declines are worth $5 trillion.
Quality-of-life improvements both increase the value of an additional year of life and enhance the productivity of older workers. Murphy and Topel (9) didn't have data to directly examine changes in health quality. An estimate, assuming quality of life increased as fast as mortality declined, suggested that the economic benefits of health quality improvements could be twice those of mortality reductions (9). Fogel and Costa (10) proposed a model of technophysiological evolution that describes the mechanisms and economic consequences of improvements in individual health and functioning. They examined long-term changes in morbidity, disability, and longevity, using two databases. One had physician evaluations of Union Army veterans of the U.S. Civil War done when they applied for federal pensions in 1900 and 1910. They compared morbidity and disability prevalence at that time with that for white males evaluated in National Health Interview Surveys and National Health and Nutrition Examination Surveys done in the 1980s and 1990s and found chronic morbidity and disability declined 6% per decade (11, 12). Analyses of Union Army recruits compared with post-World War II studies of the health and fitness of military personnel verified that long-term improvements in physical capability (e.g., strength, waist-hip ratios, and pulmonary capacity) occurred concurrently with body size and life expectancy increases (13, 14).
Fogel (14) argued that the economic productivity and work capacity of individuals grew because of increased body size, better early health, and lower risk of infectious disease and environmentally induced physiological stresses. Improved nutrition (both fetally and in adults), water quality, and sanitation reduced both infectious and chronic disease risk.
U.S. cognitive performance also improved, with IQ increasing 25 points from 1918 to 1995 (15). Suggested mechanisms are improved nutrition in children and smaller families, better education, greater environmental complexity, and improved problem-solving skills.
Manton et al. (16) analyzed the ratio of active life expectancy (ALE) to total life expectancy (LE) from 1935 (start of Social Security) to 2000, using Fogel and Costa data and the 1982 to 1999 National Long Term Care Surveys (NLTCS). The ratio [an indicator of morbidity compression (17)] increased from 1935 to 2000 at both ages 65+ and 85+, suggesting health quality is increasing faster than life length, further increasing the value of each additional year of life. The per annum rate of decline in disability increased from Fogel and Costa's estimate of 0.6% to the 1.5% found in the U.S. elderly population 1982 to 2004. The rate accelerated to 2.2% per annum 1999 to 2004 (18, 19). Manton et al. (18, 20) found per capita, per annum Medicare costs for nondisabled males age 65–84, after inflation adjustment, declined 1.3% per annum from 1982 to 1999 (18). Thus, the slowing of Medicare cost growth due to increases in the nondisabled Medicare population is enhanced by declines in per capita per annum Medicare costs (inflation-adjusted) due to health improvements in nondisabled persons. Medicare costs at ages 65–84 were reduced $16.9 billion in 1999 because of disability declines 1982–1999. Declines in health expenses for nondisabled persons decreased Medicare costs in 1999 another $10.6 billion. Subtracting $1.6 billion in increases above age 85, total 1999 Medicare cost declines were $25.9 billion (14%) compared with what costs would have been without those reinforcing trends (18, 20). Savings in 2004 Medicare costs due to health improvements from 1982 were $43.7 billion and are projected to rise to $72.9 billion in 2009 (20).
Although recent U.S. health and per capita Medicare cost trends are positive, the causes of increases in LE and ALE need to be assessed to determine whether those trends will continue and how interventions can be designed to promote them. Cutler et al. (21) analyzed data on individuals from the 1982 to 1999 NLTCS linked to Medicare records and found much of the decline in chronic disability, and of the life expectancy increase, were due to improved medical management of cardiovascular disease. Costa (11) estimated that 24–41% of the long-term disability decline was due to medical care innovations ameliorating symptomatic consequences of chronic disease, with 37% due to reduced disease prevalence. Manton et al. (22) found declines in severe cognitive impairment at advanced ages in the 1982 to 1999 NLTCS. These declines were due to improved education in recent elderly cohorts and reductions in the effects of circulatory diseases (e.g., elimination of stroke sequelae) (23). Thus, a large and increasing proportion of declines in both physical and cognitive impairment is due to medical care innovation.
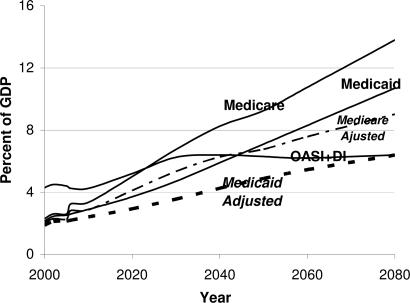
Recently, Medicare (inclusive of part D) and Medicaid (inclusive of state contributions) were projected to represent over 24% of U.S. gross domestic product (GDP) by 2080 (see Fig. 1), with less than 7% of GDP consumed by Social Security. Questions raised by those projections include (i) how much of GDP should be invested in health, (ii) how Medicaid and Medicare expenditures affect economic growth, and (iii) how investment in research affects health and function at late ages and human capital inputs to future economic growth.
Fig. 1.
Projected (to 2080) Social Security, Medicare, and Medicade GDP shares with and without adjustments to Medicare and Medicaid costs for disability declines and improved health.
The first question was addressed by Murphy and Topel (9). It had been argued that medical costs grew primarily due to technologic innovations (24). Jones (25) and Hall and Jones (26) argue those analyses are incomplete because (i) although expensive technologies may be developed, they do not have to be used, and (ii) the U.S. is investing heavily in developing those technologies, because U.S. health spending is as important as non-health spending in increasing economic welfare (9). Health spending is argued to be a superior good because consumer satiation occurs more rapidly for non-health goods (14, 26). Both Fogel (14) and Murphy and Topel (9) argue that health spending increases rapidly because its productivity is increasing and that growth in disposable income increases demand for health-related consumption. It is suggested GDP investment in health care could reasonably increase to 30% by 2050 (25, 26).
Jones (25) suggests changes in Medicare costs can be explained by the “march of science,” which produces new technology for increasing life expectancy and improving health and function. Jones (25) and others estimate new technology and improved health care explains half to three-fourths of health improvements. The march of science may reduce quality-adjusted costs 1–2% per year. Also constraining health cost increases is that, as ALE increases, health care costs are “diluted” because individual expenditures are concentrated in the final two years of life (27). For long-lived persons, per capita, per annum Medicare costs may be lower than for shorter-lived persons because costs are averaged over more years of healthy life. Medicaid costs at late ages are due largely to long term care (LTC), which is generally not covered by Medicare; thus, Medicare and Medicaid service mix and cost dynamics differ above age 65. Technical innovations are more likely for Medicare than Medicaid, because the latter focuses on LTC. Specifically, Medicare acute and postacute expenditures have the goal of improving the health and function of individuals and, in general, reducing the duration of care (28). For example, hospital lengths-of-stay showed a long-term decline after introduction of the Prospective Payment System in 1983–1984. Absolute declines in Medicare costs in 1998 and 1999 resulted from the 1997 Balanced Budget Act. The curative and rehabilitative efficacy of acute and postacute care could be further enhanced by (i) increased investment in research (with a change in health care and research from a disease management and curative paradigm to a molecular medicine-based preemptive-regenerative paradigm) and (ii) initiatives in the Medicare Modernization Act of 2003 to introduce prescription drug coverage, improve preventative services (e.g., disease screening), and reorganize reimbursement to emphasize the quality and efficacy of health care outcomes [i.e., the Payment for Performance program (29)].
Health care and biomedical research investment can affect other economic sectors by (i) increasing human capital at later ages and (ii) increasing innovation. If research affecting health care enhances productivity in other economic sectors, total GDP will grow, even beyond the direct benefits of human capital gains. The manufacturing of new products, devices, and materials leads to innovation across industries. Such spillover was evident in the 1960s and later due to federal investments in NASA research. Health spending may thus reduce the growth rate of Medicare and Medicaid costs relative to a total U.S. economy, whose growth is stimulated by the research and medical investments designed to improve health and function.
Additionally, the U.S. labor force is aging as fast as or faster than the U.S. population (30) because of declines in labor force participation rates of persons aged 16–19 (by 12.8% 1980–2004) and 20–24 due to increased educational requirements. In contrast, the labor force participation of persons aged 55 to 64 increased 6.6% 1980–2004. Even at age 65+, after declining to 10.8% in 1985, the labor force participation rate increased to 14.4% by 2004 (1.5% per year). The labor force aged 55+ will grow 4 times faster from 2004 to 2014 than the total labor force, or by 11 million persons. Increases in labor force participation rates at later ages are stimulated by (i) changes from defined-benefit to defined-contribution pensions (31), (ii) removal of policies restricting work at later ages (e.g., in 2000), (iii) increased education and earnings, and (iv) improved health. In this article, we examine the effects of continued improvement in health on economic growth under the assumption that much of the improvement (≈50–75%) is due to research and improved health care, with many facilitating changes in pensions, education, and earnings and removal of age-restrictive labor policies having occurred or are in progress.
An acceleration of ALE increases relative to LE suggests the SSA dependency ratio of persons capable of work relative to those who are not will be improved if declines in chronic disability continue and normal retirement ages are adjusted appropriately (19, 32). Improvement in functioning at later ages suggests the availability of more informal LTC resources and other types of social wealth. A critical question is whether research and medical interventions will cause ALE to continue to increase more rapidly than LE and help fiscally stabilize Medicare, Medicaid, and SSA (see Fig. 1).
Because of the interaction of the dynamics of health care innovation and the relative rate of change in LE and ALE, one could expect the age at crossover to dominance of LTC and Medicaid over Medicare per capita costs (now age 90) to be raised by increasing research (27). This is important because productivity gains for new technology in acute and postacute care (paid by Medicare) are generally greater than for LTC (partly paid by Medicaid) because of “Baumol's disease”; i.e., LTC costs are less responsive to technological innovation than acute care costs because of their larger labor component and because the age-trajectory of disease and disablement processes may be little affected by the palliative and maintenance LTC currently provided at late ages (28). Baumol's disease effects on LTC might be reduced if patient management in nursing homes was systematized by using electronic patient and account management systems and with progress on modulating the age course of chronically disabling diseases, such as osteoarthritis (by joint and cartilage replacement), cataracts (lens replacement), and cognitive impairment (by improved management of stroke and cardiovascular disease). Further prompting changes in Medicaid are Home and Community Based Service waivers whose availability was expanded by the 1999 Olmstead decision.
Results
Investment in Research.
Table 1 shows the socially optimal research investment for different parameters. A crucial parameter is the real (inflation-adjusted) interest rate, i. The real 75-year consensus interest rate for Social Security Trust Fund projections is 3.0% (33). Analyses of stock market returns 1802–1991 (34) suggest a 6.3% inflation-adjusted return. In our calculations we used real interest rates of 6.3% and 5.5%, the latter reflecting a weighted average of federal and private rates. Jones and Williams (7) considered an interest rate range of 4–14%.
Table 1.
Share of foregone consumption going to health, care research and development optimal for society, and differences between free market and decentralized planners' optimum research investment for real interest rate i
| Real interest rates and effects | λ |
||
|---|---|---|---|
| 0.3 | 0.5 | 0.7 | |
| i = 0.063 | |||
| Ssp | 0.0891 | 0.1275 | 0.1564 |
| Ssp-SDC | 0.0202 | 0.0586 | 0.0875 |
| Optimal federal investment, $ billions | 253 | 733 | 1,093 |
| i = 0.055 | |||
| Ssp | 0.1114 | 0.1540 | 0.1841 |
| Ssp-SDC | 0.0395 | 0.0821 | 0.1122 |
| Optimal federal investment, $ billions | 494 | 1,026 | 1,402 |
For λ = 0.5 (research redundancy; see Eq. 3) and i = 6.3%, the optimal level of research investment is 12.8% of GDP, or $1.6 trillion, similar to the $1.5 trillion suggested for a 7% interest rate (6). If federal investment had been maintained at 1964 levels (1.9%), the total 2005 U.S. research investment would be 2.1 + 1.9 = 4.0%, or $500 billion, $140 billion higher than current levels. The 1.9% rate of federal investment was motivated by the U.S.–Soviet space and arms race. Recent economic advances of China, India, South Korea, and other Asian countries may represent an even greater challenge to the U.S. (35).
Given that the profit-maximizing value of research and development for the private sector (λ = 0.5 and i = 6.3%) is 6.9%, an additional 5.9% should be provided from federal sources ($733 billion). Given a 2004 total federal investment in research of approximately $110 billion by the National Institutes of Health, the National Science Foundation, the Department of Defense, the Department of Energy, and other federal agencies, a significant increase in U.S. research investment is needed. If health care is an area of rapid growth and productivity increase that currently represents 15% of GDP, the desired level of federal research spending in the biomedical sector (e.g., the National Institutes of Health and biomedical research at the National Science Foundation) is $109.8 billion, ≈3 times current levels. For a real interest rate of 5.5% and a λ of 0.5, federal investment should be 8.2% of GDP or $1.03 trillion, with $153 billion for biomedical research, 4 times current levels.
Although these estimates may seem large, the dependency of economic growth on research and technology increases with declines in the lifetime of products (e.g., Moore's law in computing), the rapid emergence of new technologies (e.g., nanotechnology and nanomedicine), and faster rates of increase in research intensity and volume in economically competitive countries such as China (9.9% per annum), India (7.6%), and Russia (6.4%) (35). As problems with mature technologies emerge (e.g., declining oil reserves and costs of environmental degradation), research is needed to maintain current production levels as alternate and renewable energy sources and technologies are sought. Further, increases in human capital at later ages will be crucial to maintaining the U.S. labor force, whose rate of increase 2004 to 2014 is projected to drop to 1% per annum, even assuming rapid growth of the over-age-65 component (30).
Growth in federal research must respond to increased global competitiveness (and research and development outsourcing) due to increased U.S. corporate investment in countries where there are lower per capita labor costs for scientists and facilities and higher government subsidies. These factors make it appear attractive for IBM and other U.S. firms to locate research centers in countries such as China and India. Such a strategy for corporate research investment may, however, underestimate research cost and quality concerns; i.e., social and research infrastructure “weak links” (C. I. Jones, unpublished work). Costs of research investment in less developed countries must include the hidden costs of incomplete and unreliable social (and political) and research infrastructures; e.g., future problems with the health care infrastructure in China in maintaining human capital as its population and labor force age.
Economic Stimulus Due to Research: Labor Force and Human Capital Effects.
The optimal level of U.S. research determined by using the Jones and Williams model (6), consistent with their empirical research (7), is much higher than current research expenditures. The effective constraint on future U.S. research spending growth will be availability of funds (i.e., appropriable surpluses). The funds should come from increased economic activity and national wealth due to improvement of the health of the U.S. population, with increases in labor force size and technological spillovers into other economic areas.
We estimate the economic effect of health in two ways. One is examination of the effect of growth of the elderly labor force due to health improvements. However, because we focus on the over-age-65 population, this understates the full effect on national wealth, because nonwage social and economic effects are relatively large over age 65 (9). Thus, we examine wealth estimates for the 1990s that suggest the total economic impact of health capital growth is 20% larger than GDP increases (9), likely conservative for the over-age-65 population. Another important source of funds will be reductions in the rate of health cost increases as larger proportions of the elderly population remain healthy longer and as the initial costs of high technology medical care decrease (on a quality-adjusted basis) as technology matures.
We can determine the gain to the economy resulting from health improvements for those aged 65+ by measuring increases in national income due to improved health (i.e., enhanced and preserved human capital above age 65). Improvements in health will be measured (i) as long-term decreases in chronic disability prevalence tracked with the 1982–2004 NLTCS and (ii) by decreases in health service use (and costs) in nondisabled persons assessed from Medicare files linked to the 1982 to 2004 NLTCS. The increase in GDP for year t is
where g*y is the economic growth rate. With a decrease in disability (and improvements in health), the rate of increase in the labor force (m) used to calculate g*y is augmented by increases in the proportion of the labor force over 65; i.e., health improvements for those aged 65+ increase m and Y*t (see Eq. 4). Indirect gains are also realized by increases in gy produced by increases in health care research and development and innovations; e.g., reduced illness and disability costs for those under age 65.
Disability prevalence over age 65 decreased 1.5% annually 1982–2004 (19, 36); i.e., there were 2.7 million fewer chronically disabled elderly persons in 2004 than if disability risks had remained at 1982 levels. Continuation of the trend to 2034 would further reduce the disabled elderly population by 5.2 million. To reduce the prevalence of chronic disability, it is necessary to improve the health of nondisabled persons; i.e., slow the rates of progression of chronic diseases to more severe stages where serious disability emerges. This will occur because of improved early treatment and control of chronic disease processes like cardiovascular disease and diabetes (22, 23). Per capita inflation-adjusted decreases in Medicare costs (and health service use) for nondisabled elderly persons averaged 0.9% per annum 1982–1999. The improvements in health reflected by these lower costs are underestimated because of temporal lags between expenditures and health changes.
The effects are shown in Table 2. The growth of output for the U.S. economy given by Eq. 2 is a function of labor, m, through Eqs. 4 and 5. The proportion of the total U.S. labor force over age 65 is currently small [3.4% in 2004 (30)]. It is projected to grow to 5.4% of the labor force by 2014 (30). A projected increase of the 65+ U.S. population by 2034 to 20% of the total U.S. population (a relative increase of 57.5% from the 12.7% of the U.S. population elderly in 2004) suggests that 8.5% or more of the U.S. labor force could be age 65 + in 2034.
Table 2.
Per annum labor force and Medicare cost effects of improvement in health in the U.S. elderly population
| Year | DDR, % | MCI, % | Labor force increment to 2004 labor force (5,000,000) due to |
Tax revenues (20%) increases generated by assuming specific labor force participation rates, $ billions; in parentheses, elderly percentage of U.S. labor force |
Reductions in Medicare costs due to improvements in nondisabled persons' health (increased prevalence & reduced per capita costs), $ billions | Average projected funds for appropriation, $ billions assuming one of three labor force participation rates |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DDR | MCI, millions | Total | 30% | 50% | 100% | 30% | 50% | 100% | ||||
| 2014 | 1.5 | 0.9 | 1.0 | 2.7 | 3.7 | 30.0 (3.8) | 50.1 (4.2) | 100.2 (5.4) | 137.7 | 167.7 | 187.8 | 237.9 |
| 2.2 | 1.2 | 1.8 | 3.6 | 5.4 | 44.2 (4.1) | 73.7 (4.8) | 147.4 (6.4) | 152.6 | 196.8 | 226.3 | 300.0 | |
| 2034 | 1.5 | 0.9 | 5.2 | 13.7 | 19.0 | 281.3 (5.4) | 468.8 (7.3) | 937.6 (12.1) | 810.2 | 1,091.5 | 1,279.0 | 1,747.8 |
| 2.2 | 1.2 | 7.0 | 18.1 | 25.1 | 371.5 (6.6) | 619.2 (8.9) | 1,238.4 (15.2) | 1,442.9 | 1,814.4 | 2,062.1 | 2,681.3 | |
DDR, disability decline rate; MCI, Health Service Index reduction health improvement.
In Table 2, we assumed disability declines of 1.5% (and 2.2%, the decline 1999–2004), a 0.9% per annum rate of improvement in health (1.2% for the 2.2% disability decline) in the nondisabled population, increases in national income [i.e., GDP increase plus 20% for health capital as estimated for the 1990s (ref. 9, table 3), and the implied tax (at a 20% rate) for three labor force participation rates (for persons with improved health) of 100%, 50%, and 30%]. We include a rate of 30% because the Bureau of Labor Statistics' (BLS) projected participation rate for persons aged 65 to 74 in 2014 is 27% without explicit health improvements and should be a conservative lower bound in 2034. To achieve a 50% participation rate, the age at which full Social Security benefits are provided might need to be increased (e.g., to age 69 as proposed in Britain (4)), with further reductions in partial benefits before that age. The 100% rate was included because that is the rate necessary, assuming a 1.5% per annum decline in chronic disability, to achieve the 5.4% of labor force over age 65 in 2014 projected by the BLS. If the rate of disability decline were 2.2% (observed 1999 to 2004), then the BLS projection of 5.4% of the labor force being 65+ in 2014 could be achieved with a 68.7% labor force participation rate. Thus the BLS cohort-based projections seem to imply higher rates of disability improvement, possibly higher than the 2.2% per annum decline 1999 to 2004. Even with large increases in the 65+ labor force participation rate, the growth rate 2004 to 2014 of the labor force drops to 1%.
Using a per capita GDP in 2004 of $41,000 adjusted to worker equivalents (doubling the value to approximately $84,800), estimates (9) of the net increase in health capital (20% of GDP increases; likely an underestimate for persons over age 65) and GDP growth of 3% per year, an appropriable surplus (20% of taxable income and wealth) of $30 billion is produced in 2014 if only 30% of persons with improved health opt to work. This participation rate implies, however, that only 3.8% of the labor force is over age 65 in 2014. Adding Medicare cost reductions of $137.7 billion (2014) produces $167.7 billion dollars available for research using “pay-as-you-go,” or current-year, accounting. If the rate of disability decline is 2.2% (Medicare cost reduction is 1.2%), $196.8 billion dollars are available at the 30% labor force participation rate. The health cost reductions are conservative, because potential Medicaid reductions are not included. These estimated benefits are more than sufficient to support a doubling of biomedical research at the National Institutes of Health and National Science Foundation over 5 years (e.g., 2009–2014).
Benefits increase rapidly as baby boom cohorts pass age 65, with human capital growth playing an increasing role. By 2034, the potential surplus (30% participation rate) is $281.3 billion (constant dollars) in human capital gains and $810.2 billion (constant dollars) in Medicare cost reductions. The total, $1,091.5 billion, is more than sufficient to complete a quadrupling of the current biomedical research investment 2009–2034. Even assuming that only 30% of the projected Medicare savings were achieved (for the 1.5% rate of disability reduction) and that the labor force participation rate was 30%, the gain would be $524.34 billion in 2034.
Medicare and Medicaid Long-Term GDP Shares.
It is hazardous to make long-term (75-year) projections, but such exercises are necessary to examine the long-range fiscal soundness of Medicare and Medicaid. To assess the implication of health changes for future GDP shares of Medicare and Medicaid, we reduced their costs by the amount associated with a 1.5% per annum rate of decline in disability and the associated decline in per capita Medicare costs in nondisabled persons. In these analyses, we did not upwardly adjust the GDP rate of growth due to increases in human capital; i.e., we used long-term Medicare and Social Security Trust Fund projections of GDP growth. We did assume that the health benefits of biomedical research and improved health care extended to Medicaid recipients of all types.
Our 2080 projections of the GDP share for Medicare (13.8%) were taken from the 2005 Trust Fund report (37). This projection includes Part D benefits but does not include Medicare copayments, which are estimated to be 25% of the Medicare federal share. For Medicaid, CMS and CBO generally project only 10 years into the future. CBO occasionally produces 75-year projections, but uses simplifying assumptions that cause Medicaid costs to grow at rates similar to overall health care costs (38). Consequently, we used published projections for 2005 to 2045 (38) and extended them to 2080. This provided a 2080 estimate of Medicaid GDP share of 10.7% (combined federal and state shares), which reflects large long-term increases in the U.S. elderly and oldest-old population and, without projected improvements in chronic disability, significant growth in the need for LTC and nursing home use.
The projected increase (Fig. 1) to 24.5% of GDP for Medicare and Medicaid expenditures is reduced, assuming a 1.5% decrease in disability, by more than a third to ≈15.4% (9.0% for Medicare and 6.4% for Medicaid). If the faster rate of disability improvement (2.2%) is used, the reduction by 2080 is approximately half, or 12% of GDP.
Thus, without interventions, health care spending may, by 2080, exceed even a 30% GDP share (26) (i.e., 24.5% for Medicare and Medicaid and modest increases in private payments from the >8% observed in 2004). If, however, the projected long-term health improvements are realized, Medicare and Medicaid will consume 12–15% of GDP, which, allowing for reasonable increases in private health spending, is supportable given the arguments of Murphy and Topel (9), Fogel (14), and Jones (25) about future increases in disposable income and the elasticity of health spending, especially if Medicare and Medicaid provide a greater proportion of total future U.S. health costs due to population aging and changes in benefits.
Discussion
We evaluated the optimal level of investment in research in the U.S. economy, assuming that preservation of human capital at later ages stimulates growth as the U.S. population and labor force ages, with growing proportions of the elderly population surviving in healthier states.
The need for increased investment in research is driven by arguments about the growth-stimulating effects of increased human capital and their beneficial effects on Medicare and Medicaid costs and by the need for the U.S. to compete in the global market. Given the large size of the U.S. economy, the absolute investment in research in the U.S. is currently larger than for any other country. However, many economies that show aggressive policies toward the funding of research (e.g., China) are showing rapid increases in research spending because of their large purchasing power-adjusted GDPs and the rapid growth of their economies (35). The potential impact on the U.S. economy is illustrated by growing negative trade balances (especially for high technology, high value-added products first observed in 2002).
The model suggests that productivity increases generated by improving the health of a larger pool of older, trained, and experienced workers through advances in biotechnology, nanotechnology, and medicine stimulated by biomedical (and other) research could help maintain the U.S. competitive edge in the global economy. That is, the U.S. may better deal with the social, political, and economic consequences of population and labor force aging than, for example, China or India. This will occur in part by producing real GDP growth through enhanced growth in human capital. The necessary investment is a significant increase in federal expenditures in multiple research disciplines, where direct costs are recouped by the growth of GDP and federal tax revenues, and moderation of the relative rate of growth of GDP share spent on health to economically sustainable levels.
Failure of the U.S. to make such research and health care investments (including addressing the interface of Medicaid program benefits and the health needs of the uninsured) may have serious economic consequences by (i) further reducing the rate of labor force growth and (ii) failing to stimulate one of the currently most active U.S. economic sectors, health care, so that GDP does not increase as rapidly as projected. Thus, if health service demand increases because per capita health is not improved in the rapidly growing elderly and oldest-old population, the proportion of GDP invested in health care may increase even more rapidly than in current projections.
An additional implication is that a failure to increase research can lead to increases in prices and economic stagnation. That is, a critical parameter in research investment is the lifetime of a product. As research increases, product lifetime decreases, and prices stay low. An example is the decline in prices of electronic goods as technological development has followed Moore's law. This is crucial to reducing per unit prices for new medical technologies.
Materials and Methods
A Formal Model of GDP Returns to Investment in Research.
To estimate the optimal investment in research, we used the model of Jones and Williams (6), which includes four factors affecting the allocation of resources to research, two promoting underinvestment (surplus appropriability, knowledge spillover) and two overinvestment (creative destruction, duplicative externalities). This model was used to evaluate the robustness of empirical findings (7) that suggested a large underinvestment in U.S. research. The simulations suggested the empirical findings were robust, requiring very high interest rates (14%) and considerable research redundancy to produce overinvestment. We used the model to explain how increasing research spending, leading to improved health and functioning at later ages, affects economic growth, particularly with a rapidly aging population and labor force. We also use the model to determine how much economic surplus will be appropriable for research.
The model examines the relation of two levels of production; i.e., for final and intermediate goods. The final goods production function is based on a constant elasticity of substitution methodology (ref. 6, pg. 67) yielding
 |
where Yt is the product for the amount of labor Lt and types i of intermediate capital inputs/goods, x(i). ρ is the substitution parameter between different types of intermediate capital “goods.” Assuming a large number of firms produce intermediate goods, their gross mark-up ηu is determined by the elasticity of substitution ρ between intermediate goods, or
The constant elasticity of substitution production function severs a restrictive link of mark-up and capital share (6). Creative destruction relaxes the assumption that intermediate producers operate as unconstrained monopolists by breaking the link between equilibrium mark-up and consumer surplus implied by creating a new good. Allowing ρ to vary from 1.0 fixed empirical irregularities in Romer's model (6). Implicit in Eq. 2 is At, the set of production paradigms successfully used to produce intermediate products. α relates marginal productivity to labor and capital with 0 ≤ α ≤ 1.0.
Creative destruction requires identification of clusters of products. Not all products in “clusters” generated by research are “new.” The proportion of “upgrades” of existing products is ψ/(1 + ψ). The remainder, 1/(1 + ψ), represents products increasing variety in a cluster that help maintain product competition and control prices. As product life expectancy decreases, the value of research increases. Technical congestion λ and spillover φ also affect the production of new technology, At,
where Rt is investment in research, and δ is its productivity. λ (0 ≤ λ ≤ 1.0) is the nonredundant proportion of research. If λ → 0, duplication increases and the value of research declines. For λ = 1.0, there is no duplication. φ reflects benefits from prior research, At. When φ = 0, there is no gain. When φ > 0, prior research enhances productivity.
The economy-wide growth of production gy is, at equilibrium,
where m is the labor growth rate and σ = 1/ρ − (1 − α) reflects interactions of intermediate good substitution and marginal productivity. The dependence of productivity growth on research is,
The optimal share of research and development, assuming constant growth for a decentralized economy, is,
where i is the real interest rate, and ηc is the constrained mark-up for intermediate goods,
and where ηc is controlled by the size of clusters through ψ and the elasticity of substitution [in Romer (5) ρ = 1.0]; here ρ = 1.8 (empirical range 0.5–2.77; ref. 6).
The optimal social planner investment is
To assess how research investment affects economic activities, consider m, the rate of labor increase, in Eq. 4. Labor can be increased by birth, immigration, education and training, or investment in enhancing and preserving physical and cognitive facilities to later ages. Currently 3% of GDP is invested in research in the U.S (8).
Hall and Jones (26) suggest that at an interest rate of 7%, U.S. investment in research in 2004 should be 4 times current levels, or $1.5 trillion. Federal expenditures on research peaked at 1.9% of GDP in 1964 and declined to 0.8% of GDP by 2004. Industrial research spending increased from 0.6% to 2.1% of GDP 1957–2000 (8). However, in contrast to the 60% of federal research spending that flows to other sectors, only 2% of industrial research spending does so (8). Additionally, there are fewer restrictions on the dissemination of results from federally funded research. Thus, federal research investment has potentially higher per-dollar spillover, and growth stimulating, effects (28). Federal research spending also (i) tends to focus on basic research where the U.S. maintains an advantage, (ii) helps maintain research growth over short-term economic downturns such as occurred in 2001 and 2002 when corporate research retrenched, and (iii) provides basic inputs to industrial research and development stimulating their growth.
If Eq. 6 determines how much to increase research to improve returns on investment, optimal economic growth occurs when government increases research to the level given by Eq. 7. By assuming government research funds are exogenous, Eq. 7 underestimates the optimal government research investment by undervaluing its economic stimulus. The difference between SDC and SSP should be the smallest federal investment in research.
Acknowledgments
We thank Prof. Robert Fogel of the University of Chicago and anonymous reviewers for a thorough review of this paper and helpful suggestions, and Virginia Lewis for thorough editing and preparation of the manuscript. Funding was provided by the National Institute on Aging of the National Institutes of Health Grant R01–AG001159 and P01–AG017937.
Abbreviations
- ALE
active life expectancy
- GDP
gross domestic product
- LE
total life expectancy
- LTC
long term care
- NLTCS
National Long Term Care Surveys.
Footnotes
The authors declare no conflict of interest.
References
- 1.Jones CI. Q J Econ. 2005;120:517–549. [Google Scholar]
- 2.Jones CI. Am Econ Rev. 2002;92:220–239. [Google Scholar]
- 3.Jones CI. Finance, Research, Education, and Growth. New York: Palgrave Macmillan Press; 2006. pp. 49–74. [Google Scholar]
- 4.Geneva Association. Geneva Association Information Newsletter. 2006;39:3–5. [Google Scholar]
- 5.Romer P. J Political Econ. 1990;98:S71–S102. [Google Scholar]
- 6.Jones CI, Williams JC. J Econ Growth. 2000;5:65–85. [Google Scholar]
- 7.Jones CI, Williams JC. Q J Econ. 1998;113:1119–1135. [Google Scholar]
- 8.National Science Foundation. [Accessed May 16 2007];Science and Engineering Indicators 2006. www.nsf.gov/statistics/seind06.
- 9.Murphy KM, Topel RH. J Political Econ. 2006;114:871–904. [Google Scholar]
- 10.Fogel RW, Costa DL. Demography. 1997;34:49–66. [PubMed] [Google Scholar]
- 11.Costa DL. Demography. 2000;39:119–137. doi: 10.1353/dem.2002.0003. [DOI] [PubMed] [Google Scholar]
- 12.Costa DL. J Econometrics. 2003;112:175–192. [Google Scholar]
- 13.Costa DL. J Econ History. 2004;64:1–23. [Google Scholar]
- 14.Fogel R. Cambridge Studies in Population, Economy and Society in Past Time. New York: Cambridge Univ Press; 2004. pp. 1–216. [Google Scholar]
- 15.Neisser U. Am Scientist. 1997;85:440–447. [Google Scholar]
- 16.Manton KG, Gu X, Lamb VL. Pop Dev Rev. 2006;32:81–105. [Google Scholar]
- 17.Fries JF. N Engl J Med. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 18.Manton KG, Gu X. In: Ageing Horizons. Howse K, editor. Oxford: Oxford Institute of Aging; 2005. pp. 25–34. [Google Scholar]
- 19.Manton LG, Gu XL, Lamb VL. Proc Natl Acad Sci USA. 2006;103:18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manton KG, Lamb VL, Gu XL. J Aging Health. 2007;19:359–381. doi: 10.1177/0898264307300186. [DOI] [PubMed] [Google Scholar]
- 21.Cutler DM, Landrum MB, Stewart KA. NBER Working Paper Series 12184. Stanford, CA: National Bureau of Economic Research; 2006. pp. 1–55. [Google Scholar]
- 22.Manton KG, Gu XL, Ukraintseva SV. Advances in Gerontology. 2005;16:30–37. [PubMed] [Google Scholar]
- 23.Fox ER, Taylor HA, Benjamin EJ, Ding JZ, Liebson PR, Arnett D, Quin EM, Skelton TN. Stroke. 2005;36:546–550. doi: 10.1161/01.STR.0000154893.68957.55. [DOI] [PubMed] [Google Scholar]
- 24.Newhouse JP. J Econ Perspectives. 1992;6:3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- 25.Jones CI. NBER Working Paper Series 9325. Stanford, CA: National Bureau of Economic Research; 2002. pp. 1–37. [Google Scholar]
- 26.Hall RE, Jones CI. Q J Econ. 2007;122:39–72. [Google Scholar]
- 27.Spillman B, Lubitz J. N Engl J Med. 2000;342:1409–1415. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- 28.Pardes H, Lander ES, Ullian AD, Manton KG, Tolley HD, Palmer H. Science. 1999;283:36–37. doi: 10.1126/science.283.5398.36. [DOI] [PubMed] [Google Scholar]
- 29.Miller ME. [Accessed May 16, 2007]. Testimony presented before the Committee on Finance, US Senate, 27 July, www.medpac.gov/publications/congressional_testimony/testimony_P4P.pdf.
- 30.Toossi M. Mon Labor Rev. 2005;128(11):25–44. [Google Scholar]
- 31.Poterba J, Rauh J, Venti S, Wise D. NBER Working Paper Series 12597. Stanford, CA: National Bureau of Economic Research; 2006. pp. 1–49. [Google Scholar]
- 32.Singer, B. Manton KG. Proc Natl Acad Sci USA. 1998;95:15618–15622. doi: 10.1073/pnas.95.26.15618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Girola JA. US Department of Treasury Research Paper 2005-02. Washington, DC: US Department of Treasury; 2005. pp. 1–15. [Google Scholar]
- 34.Siegel JJ. Stocks for the Long Run. New York: McGraw Hill Professional; 2002. pp. 1–388. [Google Scholar]
- 35.Battelle Memorial Institute. [Accessed May 16, 2007];R&D Magazine (Battelle Seattle Research Center) :G1–G17. www.rdmag.com/pdf/RD_GR2006.pdf.
- 36.Manton KG, Gu X. Proc Natl Acad Sci USA. 2001;98:6354–6359. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Medicare and Medicaid Services. 2005 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. [Accessed May 16, 2007];2005 www.cms.hhs.gov/reportstrustfunds/downloads/tr2005.pdf. [Google Scholar]
- 38.Kronick R, Rousseau D. Health Aff. 2007;26:W271–W287. doi: 10.1377/hlthaff.26.2.w271. [DOI] [PubMed] [Google Scholar]