Abstract
Widespread early detection with prostate-specific antigen (PSA) has radically transformed the clinical management of prostate cancer. PSA has become valuable in the monitoring and risk stratification of recurrent disease following local therapy. In many ways, biochemical recurrence-free survival, or PSA outcome, has become a surrogate measure of treatment efficacy following primary local therapy. Given the inherent differences in PSA kinetics following these treatment approaches, the definition of biochemical success or failure is not uniform among therapies. An appreciation of the inherent strengths, limitations, and biases of the standard definitions of failure can provide a more meaningful context within which to interpret the reported outcomes of different treatment modalities.
Key words: Prostate-specific antigen, Prostate cancer recurrence, Biochemical failure, Brachytherapy, Radiotherapy, Hormonal therapy
More than in any other disease in urologic oncology, the integration of serum biomarkers has radically transformed the clinical management of adenocarcinoma of the prostate in the modern era. Following its introduction more than 2 decades ago, prostate-specific antigen (PSA) testing has fundamentally altered the landscape of diagnosis, treatment, and risk stratification for prostate cancer, the most common noncutaneous solid tumor in adult males and the third most common cause of death from cancer in US males.1
Widespread early-detection programs with PSA have led to a stage migration, allowing diagnosis at an earlier, more curable stage and allowing a much longer life expectancy than was historically the case.2–4 The resulting surge in the proportion of men presenting with clinically localized disease has dramatically increased the number of patients presented with the decision of undergoing surgery or radiation therapy with curative intent.
Although issues of personal preference in terms of potential quality-of-life outcomes and other individual concerns clearly factor into this decision-making process, the obvious question that invariably arises is that of the likelihood of cure with a given choice of treatment. PSA outcome, or biochemical recurrence-free survival, has become the de facto proximate measure of the effectiveness of definitive local therapy.5,6
The detection of recurrent disease was in fact the original clinical application of PSA in prostate cancer.7 This is a relatively straightforward task following radical prostatectomy, because the primary source for PSA production has been removed. Biochemical failure among surgically treated patients is generally defined as a measurable or detectable PSA level. As such, patients with biochemical “success” after surgery have been essentially cured of their disease. The definition of failure after radiation therapy is complicated, in that currently available technologies by design incompletely ablate all functioning prostatic epithelium. This limits the definition of a clinically meaningful post-treatment nadir analogous to the postsurgical undetectable PSA.
In an effort to standardize the definition of biochemical failure after radiation treatment, the American Society for Therapeutic Radiology and Oncology (ASTRO) convened a consensus conference in 1996. This resulted in the recommendation of a criterion that defined biochemical failure as 3 consecutive increases in PSA after a nadir, with the date of failure backdated to the midpoint between the daters of the nadir and the first or any rise great enough to prompt initiation of secondary (salvage) treatment.8 Subsequent studies illuminated a number of fundamental methodological limitations of this definition, and several alternative candidate definitions of failure have been presented in the literature (Table 1) in the past several years.9–10 In 2005, ASTRO convened another consensus panel meeting, which concluded that a PSA value of 2 ng/mL greater than the absolute nadir represents the best revised definition of failure following external-beam radiation monotherapy.11
Table 1.
Sensitivity, Specificity, and Biochemical Recurrence-Free Survival (BRFS) Probabilities for Definitions of Biochemical Failure Among Patients Treated With External-Beam Radiation Monotherapy
| 5-Year | 10-Year | |||
|---|---|---|---|---|
| Definition | Sensitivity (%)* | Specificity (%)* | BRFS (%) | BRFS (%) |
| ASTRO (1997) | 61 | 80 | 59 | 49 |
| Nadir + 2 | 74 | 82 | 68 | 44 |
| PSA > 0.2 ng/mL | 91 | 9 | 15 | 3 |
Performance characteristics with respect to the ability of the definition to predict subsequent clinical failure (local failure, distant failure, institution of hormonal therapy, and post-treatment PSA > 25 ng/mL).
Adapted from Kuban D et al.10
The novel process whereby this revised “nadir + 2” definition was selected—namely, its superior sensitivity and specificity among a panel of candidate definitions for biochemical recurrence destined to result in defined endpoints of clinical progression— provides a relevant context within which to consider its application in clinical practice. Whereas the conventional surgical definition of biochemical failure equates with any detectable disease, with its principal focus on sensitivity for detecting the absence of cure, the new standard definition of biochemical failure after radiation therapy was not selected on the basis of its correlation with the concept of cure per se. In the latter situation, the priority was placed on selecting a definition that would accept some limitation on the sensitivity for detecting failure in the interest of increasing specificity for detecting failures associated with specific subsequent clinical outcome.
Thus, the different definitions of biochemical recurrence after local treatment in men with clinically localized disease have inherently different performance characteristics, which in turn frame their respective strengths and limitations. Appreciation of these somewhat subtle but important biases provides a context for informed clinical decision making and information sharing with patients. This article aims to review this topic systematically and clarify the current state of knowledge in the context of the contemporary literature.
Defining Biochemical Failure After Surgery
Freedland and colleagues examined a series of cutpoints (0.1–0.5 ng/mL) for determining PSA recurrence after radical prostatectomy (RP), defining the most appropriate cutpoint as the lowest PSA level associated with a substantial risk of PSA progression within 1 year, along with a 100% 3-year risk of progression.12 For patients with postoperative PSA levels between 0.01 and 0.1 ng/mL, the risk of developing a PSA value greater than 0.1 ng/mL was 36% at 1 year and 67% at 3 years. Conversely, among patients with postoperative PSA levels of 0.2 to 0.3 ng/mL, the 1- and 3-year risks of additional PSA progression were 86% and 100%, respectively. Further increases in the cutpoint for failure resulted in apparent improvements in time to biochemical recurrence, but still high rates of progression. This led to their conclusion that 0.2 ng/mL represents the most conservative cutpoint to define PSA recurrence after RP.
Amling and colleagues performed a similar analysis, with markedly lower 3-year rates of PSA progression after a PSA of 0.2 ng/mL (49%); they found a higher rate of PSA progression only after PSA levels rose above 0.4 ng/mL (72%).13 These slightly conflicting findings underscore the point that many men with low but detectable postoperative PSA values may not have additional increases in PSA. Nevertheless, given the improved success of salvage radiation with lower PSA levels at the time of radiotherapy,14,15 the clinical rationale favoring the more stringent definition seems reasonable. The increased sensitivity of this approach to defining biochemical failure after surgery comes at the obvious cost of relatively decreased specificity for detecting cases that ultimately proceed to clinically relevant progression.
D’Amico and colleagues have commented on the relative limitations of the conventional surgical definition of biochemical failure as a surrogate endpoint for clinical progression in terms of the development of distant metastases and prostate cancerspecific mortality.16 In this context, Stephenson and colleagues recently performed elegant multivariate regression analyses on a series of 10 candidate definitions of biochemical failure after prostatectomy, testing their associations with the subsequent development of distant metastases.17 A definition of PSA 0.4 ng/mL and rising after prostatectomy best explained the development of distant metastases and was proposed as the standard for reporting outcome after radical prostatectomy.
Defining Biochemical Failure After Radiation Therapy
A lack of agreed-upon criteria for establishing the effectiveness of radiotherapy prompted the ASTRO Board to form a committee in 1994 to develop a standardized definition of PSA failure after external-beam radiotherapy. This led to the 1996 Consensus Conference and definition described above.8
The Consensus Panel’s requirement for 3 consecutive rises in PSA made the subsequent 1997 ASTRO definition highly sensitive to the duration and frequency of follow-up. Indeed, the Panel later explicitly recommended a minimum period of observation of 2 years, with PSA measurements quarterly for the first 2 years and semiannually thereafter.8 Vicini and colleagues subsequently demonstrated that the probability of biochemical recurrence-free survival varied from 71% when calculated with 3 years of follow-up versus 50.4% with 7-year followup.18 Other groups confirmed the observation that outcomes were substantially more favorable in the same data set at shorter follow-up periods.19 This finding is particularly important in the field of radiotherapy, where newer treatment modalities (with shorter follow-up) may be compared to previous methods with longer follow-up.
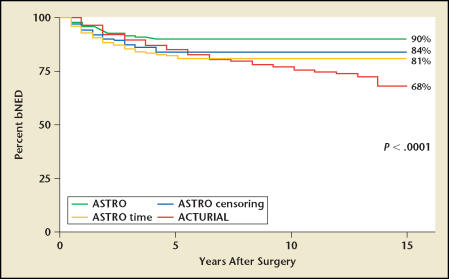
In addition, the requirement for 3 consecutive rises in PSA created biases because of informative censoring-in which patients with a high likelihood of failure (ie, those with 1 or 2 consecutive increases in PSA) are effectively removed from the calculation of survival rate, artifactually increasing the apparent survival rate.20 Furthermore, the use of backdating violates the mathematical assumptions underlying the construction of survival curves; a patient who fails is calculated against the inherently larger denominator of an earlier point in time, thereby diluting the failure rate. Gretzer and colleagues demonstrated that this inappropriate incorporation of the censoring pattern is particularly important in the case of localized prostate cancer, where the majority of patients are censored in survival analyses (Figure 1).21
Figure 1.
Evaluation of biochemical failure comparing ACTUARIAL (failure after first PSA 0.2 ng/mL or greater), ASTRO time (backdating failure to midpoint between date of surgery and first PSA 0.2 ng/mL or greater), ASTRO censoring (failure defined by 3 consecutive increases in PSA), and ASTRO bNED. bNED, biochemical non-evidence (or no evidence) of disease. Reprinted from Gretzer MB et al,21 with permission from the American Urological Association.
Accumulated experience underscored these inherent limitations of the 1997 ASTRO Consensus Definition, prompting a second consensus conference, jointly sponsored by ASTRO and the Radiation Therapy Oncology Group (RTOG) in Phoenix, AZ, in January 2005. This group specifically sought to address the above-mentioned shortcomings of the original ASTRO definition as well as, most importantly, the lack of correlation with clinical endpoints. The expert panel reviewed the performance of numerous candidate definitions of failure in data from multiple institutions in which patients received brachytherapy and/or external- beam radiation with or without hormonal treatment, with priority placed on their specificity for predicting subsequent clinical outcomes local failure, distant failure, institution of hormonal therapy or PSA > 25 ng/mL).
On the basis of this strategy, the panel recommended that “a rise by 2 ng/mL or more above the nadir PSA [“nadir + 2”] be considered the current standard definition of biochemical failure after radiotherapy with or without short-term hormonal therapy … [and] that the date of failure be determined ‘at call’ and not backdated.”11 The prioritization of correlation with clinical endpoints in the selection of the nadir + 2 definition of failure is a laudable goal with clear relevance to patients and treating physicians. The expert panel should be congratulated for the fruits of their thoughtful undertaking.
Nevertheless, this frame of reference renders the question of whether or not a patient was cured of prostate cancer—the sensitivity of the definitions— a secondary concern. The expert panel explicitly acknowledged this concern but decided that an endpoint linked to the notion of cure would result in an unacceptable number of false-positive, clinically insignificant recurrences. The sensitivity of a definition similar to the standard definition applied to surgical patients (≥ 0.2 ng/mL) for predicting clinical progression was shown to be very high (97%–99%); however, the specificities were only 9% for external-beam radiotherapy and 34% for brachytherapy.22 The explicitly stated rationale driving the selection of the nadir + 2 criterion, therefore, provides a context not only of the intrinsic value and purpose of this definition of failure but also its potential limitations and biases.
In spite of the limitations of the 1997 ASTRO Consensus Definition, the panel did not favor the complete abandonment of its use in clinical research and practice. Rather, they recommended that investigators continue to use the original Consensus Definition after external-beam radiation therapy or brachytherapy without hormonal therapy, provided that this use adhered to strict guidelines regarding the adequacy of follow-up. To avoid artifacts resulting from the sensitivity of the 1997 Consensus Definition to the duration of follow-up, the panel recommended that “the stated date of control be listed as 2 years short of the median follow-up. … Thus, to state a ‘5-year biochemical control rate’ a median follow-up of 7 years would be required.”11
These recommendations allow comparisons to the large body of literature utilizing the 1997 Consensus Definition. Nevertheless, the panel recommended that the 1997 ASTRO definition not be applied for the purpose of evaluating patients treated with combined hormonal therapy and radiotherapy. Finally, the comparative analyses by the expert panel showed that with short follow-up, biochemical relapse-free survival using the nadir + 2 criterion tended to be more favorable than with the 1997 ASTRO definition. With longer follow-up, however, relapse-free survival appeared to be worse. Strictly replacing the 1997 ASTRO definition with the nadir + 2 definition would create an artificial bias favoring a radiotherapy series with brief follow-up, underscoring the need to exercise clinical judgment in that setting.
As noted above, an important feature of the revised “nadir + 2” definition of failure is that it has been recommended as the standard not only for external-beam radiotherapy but also for patients receiving permanent radioisotopic-implant treatment or brachytherapy. The working group’s evaluation of the candidate definitions of failure leading up to the 2005 Consensus Conference included separate analyses in a cohort of more than 2500 patients treated with brachytherapy, published in more detail in a separate article.22 Though the 1997 Consensus Definition was not originally intended to be applied to the assessment of patients receiving brachytherapy, the more recent Consensus Conference concluded that it could be used for those patients, provided that the guidelines regarding adequacy of follow-up, as outlined above, were followed.
One feature of PSA kinetics following brachytherapy that is particularly important is the “PSA bounce” phenomenon, another limitation of the 1997 ASTRO definition. A median rise of 0.9 ng/mL was seen in 17% of patients after radiation-seed implant in the multi-institutional dataset used to test the candidate failure definitions. To this end, the nadir + 2 criterion offers the added value of augmenting the specificity of the failure definition, reducing false-positive “failures” resulting from benign fluctuations in serum PSA.
Conclusions
The efficacy of an oncological procedure is assessed by a variety of criteria: institution of secondary treatment, clinical progression-free survival, disease-specific survival, or overall survival. Given the protracted natural history of prostate cancer, PSA recurrence after primary therapy has become a common surrogate endpoint in defining the success of primary treatment. Given the absence of randomized clinical trials that directly compare different treatment modalities, physicians and patients are left with indirect comparisons of the outcomes of retrospective series of patients treated with surgery or with radiation therapy. The implicit limitations of such an approach are exacerbated by differences in the PSA kinetics and, hence, differences in accepted, defined standards of biochemical success or failure following the different modalities of primary local therapy.
Given these complex limitations, the comparison of biochemical recurrence-free survival outcomes following surgery and radiation for clinically localized prostate cancer is similar to the comparison of apples and oranges. Nevertheless, appreciation of the inherent biases and limitations of the definitions of failure that are commonly applied to the different treatment modalities provides the physician and patient with a more refined basis for educated decision making. As the 2005 ASTRO Consensus Panel concluded: “It is very important for the readers to note that the definitions proposed are to define success or failure in the context of a population, not an individual. Defining PSA/biochemical success for an individual versus a population are separate questions, with the former being guided by clinical judgment.”11
Main Points.
The definition of biochemical recurrence following radical prostatectomy is relatively straightforward, as the source of prostate-specific antigen (PSA) has been removed. A cutoff of 0.2 ng/mL has been associated with a high likelihood of subsequent PSA progression. More recently, 0.4 ng/mL and rising has been proposed as a definition associated more closely with development of distant metastases.
The definition of biochemical recurrence following radiation therapy is complicated by the incomplete ablation of all functioning prostatic epithelium, which creates difficulty in establishing a meaningful absolute nadir and the phenomenon of “PSA bounce.”
The 1997 ASTRO Consensus Definition of biochemical failure after radiation therapy is useful but has several shortcomings, particularly related to backdating artifact and substantial sensitivity to the duration of follow-up.
The 2005 ASTRO/RTOG Consensus Conference proposed a definition of failure after radiotherapy with or without short-term hormonal therapy as a rise by 2 ng/mL or more above the nadir PSA (nadir +2), with date of failure determined “at call.” This definition accepts some limitation on sensitivity in the interest of increased specificity for detecting failures associated with clinical outcomes other than cure.
Appreciation of the inherent strengths and limitations of various definitions of biochemical failure after primary therapy for localized prostate cancer provides a context within which to approach the interpretation of the published literature and convey accurate information when counseling patients.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics. CA Cancer J Clin. 2006;56:106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 2.Newcomer LM, Stanford JL, Blumenstein BA, et al. Temporal trends in rates of prostate cancer: declining incidence of advanced stage disease, 1974 to 1994. J Urol. 1997;158:1427–1430. doi: 10.1016/s0022-5347(01)64231-9. [DOI] [PubMed] [Google Scholar]
- 3.Hankey BF, Feuer EJ, Clegg LX, et al. Cancer surveillance series: interpreting trends in prostate cancer-part I: evidence of the effects of screening in recent prostate cancer incidence, mortality, and survival rates. J Natl Cancer Inst. 1999;91:1017–1024. doi: 10.1093/jnci/91.12.1017. [DOI] [PubMed] [Google Scholar]
- 4.Han M, Partin AW, Piantadosi S, et al. Era specific biochemical recurrence-free survival following radical prostatectomy for clinically localized prostate cancer. J Urol. 2001;166:416–419. [PubMed] [Google Scholar]
- 5.Oesterling JE, Chan DW, Epstein JI, et al. Prostate specific antigen in the preoperative and postoperative evaluation of localized prostatic cancer treated with radical prostatectomy. J Urol. 1988;139:766–772. doi: 10.1016/s0022-5347(17)42630-9. [DOI] [PubMed] [Google Scholar]
- 6.Lange PH, Ercole CJ, Lightner DJ, et al. The value of serum prostate specific antigen determinations before and after radical prostatectomy. J Urol. 1989;141:873–879. doi: 10.1016/s0022-5347(17)41037-8. [DOI] [PubMed] [Google Scholar]
- 7.Kuriyama M, Wang MC, Lee CI, et al. Use of human prostate-specific antigen in monitoring prostate cancer. Cancer Res. 1981;41:3874–3876. [PubMed] [Google Scholar]
- 8.Consensus statement: guidelines for PSA following radiation therapy. American Society for Therapeutic Radiology and Oncology Consensus Panel. Int J Radiat Oncol Biol Phys. 1997;37:1035–1041. [PubMed] [Google Scholar]
- 9.Horwitz EM, Thames HD, Kuban DA, et al. Definitions of biochemical failure that best predict clinical failure in patients with prostate cancer treated with external beam radiation alone: a multi-institutional pooled analysis. J Urol. 2005;173:797–802. doi: 10.1097/01.ju.0000152556.53602.64. [DOI] [PubMed] [Google Scholar]
- 10.Kuban D, Thames H, Levy L, et al. Failure definition-dependent differences in outcome following radiation for localized prostate cancer: can one size fit all? Int J Radiat Oncol Biol Phys. 2005;61:409–414. doi: 10.1016/j.ijrobp.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 11.Roach M, III, Hanks G, Thames H, Jr, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–974. doi: 10.1016/j.ijrobp.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 12.Freedland SJ, Sutter ME, Dorey F, et al. Defining the ideal cutpoint for determining PSA recurrence after radical prostatectomy. Prostate-specific antigen. Urology. 2003;61:365–369. doi: 10.1016/s0090-4295(02)02268-9. [DOI] [PubMed] [Google Scholar]
- 13.Amling CL, Bergstralh EJ, Blute ML, et al. Defining prostate specific antigen progression after radical prostatectomy: what is the most appropriate cut point? J Urol. 2001;165:1146–1151. [PubMed] [Google Scholar]
- 14.Leventis AK, Shariat SF, Kattan MW, et al. Prediction of response to salvage radiation therapy in patients with prostate cancer recurrence after radical prostatectomy. J Clin Oncol. 2001;19:1030–1039. doi: 10.1200/JCO.2001.19.4.1030. [DOI] [PubMed] [Google Scholar]
- 15.Chawla AK, Thakral HK, Zietman AL. Salvage radiotherapy after radical prostatectomy for prostate adenocarcinoma: analysis of efficacy and prognostic factors. Urology. 2002;59:726–731. doi: 10.1016/s0090-4295(02)01540-6. [DOI] [PubMed] [Google Scholar]
- 16.D’Amico AV, Moul JW, Carroll PR, et al. Surrogate end point for prostate cancer-specific mortality after radical prostatectomy or radiation therapy. J Natl Cancer Inst. 2003;95:1376–1383. doi: 10.1093/jnci/djg043. [DOI] [PubMed] [Google Scholar]
- 17.Stephenson AJ, Kattan MW, Eastham JA. Defining biochemical recurrence of prostate cancer after radical prostatectomy: a proposal for a standardized definition. J Clin Oncol. 2006;24:3973–3978. doi: 10.1200/JCO.2005.04.0756. [DOI] [PubMed] [Google Scholar]
- 18.Vicini FA, Kestin LL, Martinez AA. The importance of adequate follow-up in defining treatment success after external beam irradiation for prostate cancer. Int J Radiat Oncol Biol Phys. 1999;45:553–561. doi: 10.1016/s0360-3016(99)00235-7. [DOI] [PubMed] [Google Scholar]
- 19.Thames H, Kuban D, Levy L, et al. Comparison of alternative biochemical failure definitions based on clinical outcome in 4839 prostate cancer patients treated by external beam radiotherapy between 1986 and 1995. Int J Radiat Oncol Biol Phys. 2003;57:929–943. doi: 10.1016/s0360-3016(03)00631-x. [DOI] [PubMed] [Google Scholar]
- 20.Lu J. Statistical aspects of evaluating treatment and prognostic factors for clinically localized prostate cancer. Semin Urol Oncol. 2000;18:83–92. [PubMed] [Google Scholar]
- 21.Gretzer MB, Trock BJ, Han M, et al. A critical analysis of the interpretation of biochemical failure in surgically treated patients using the American Society for Therapeutic Radiation and Oncology criteria. J Urol. 2002;168:1419–1422. doi: 10.1016/S0022-5347(05)64464-3. [DOI] [PubMed] [Google Scholar]
- 22.Kuban DA, Levy LB, Potters L, et al. Comparison of biochemical failure definitions for permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2006;65:1487–1493. doi: 10.1016/j.ijrobp.2006.03.027. [DOI] [PubMed] [Google Scholar]