Urologists have tended to ignore the clinical importance and urologic realities of community-acquired urinary tract infections (UTIs) despite their significant prevalence, cost, morbidity, and increasing management problems. This is primarily because of our perception that uncomplicated UTIs are common but not a serious problem (patients do not die from uncomplicated UTIs), easy to diagnose (simple midstream urine culture), and simple to treat (short course of antibiotics). Nevertheless, data on increasing prevalence, cost, morbidity, antibiotic resistance, recurrence, and relapse suggest that the urological community needs to have another look at community-acquired UTIs. The joint meeting of the International Congress of Chemotherapy and the 17th European Congress of Clinical Microbiology and Infectious Diseases in Munich sponsored a working group symposium on March 31, 2007, to explore these issues. The conveners of this session were Dr. Kurt Naber (Germany), Dr. Reinhard Fünfstück (Germany), and Dr. Joichi Kumazawa (Japan).
Reinfections and relapses are common in women who develop uncomplicated UTI. Understanding the pathogenesis of UTI may lead to better methods of prevention and treatment. There are 2 theories as to cause of recurrence, whether reinfection or relapse. The classic model of pathogenesis is that E. coli emerge from an intestinal reservoir, colonize the vagina and periurethra, and ascend through the urethra to the bladder. To help shed more light on UTI pathogenesis, Thomas M. Hooton, MD,1 (USA) performed a study to identify temporal associations and dynamics between periurethral colonization with E. coli, bacteriuria, and recurrent UTI in 100 premenopausal adult women with acute cystitis. These women were followed for 3 months with daily urine and periurethral cultures; daily diary for symptoms, sex, and antibiotic use; and monthly fecal cultures. The E. coli strains causing recurrent UTI were identified in the periurethra of at least 75% of the women and in the urine of at least 35% 1 week prior to the onset of a new UTI. Furthermore, the recurrent UTI-causing strain was found in the rectum in 75% of women prior to the new UTI. These patterns overwhelmingly support the classic model of pathogenesis of UTI. A second hypothesis holds that some same-strain episodes of recurrent UTI may originate from uropathogens lying dormant in the bladder following a previous UTI. Anthony J. Schaeffer, MD2 (USA) presented new data that suggested some recurrences may be due to relapse from within the urinary tract. The report identified bacteriuric pods that sequester bacteria in the deep mucosal layers of the bladder even though the urine shows no growth. In Hooton’s study, described above, there were some patterns in which the recurrent UTI-causing strain was found in the urine without being detected in the periurethra just before onset of the new UTI. This is compatible with a bladder source for the recurrent UTI-causing strain. The prevalence of this phenomenon is unknown, but novel therapies should be considered for individuals with this predisposition to recurrent UTI.
Lindsay Nicolle, MD,3 (Canada) examined the duration of antimicrobial therapy for uncomplicated community- acquired UTI. The very high urinary concentrations of antimicrobials, the superficial nature of bladder infection, and effective voiding in this healthy population of women support the use of short-course antimicrobial therapy for treatment of acute uncomplicated cystitis. Although single dose is effective for up to 90% of episodes for some antimicrobials, the available data support short-course therapy with 3 days as the current accepted standard of therapy for acute uncomplicated urinary tract infection. Recurrent UTIs are best managed by low-dose antimicrobial prophylaxis, post-coital antimicrobial therapy, and patient-directed short-course therapy for symptomatic recurrences.
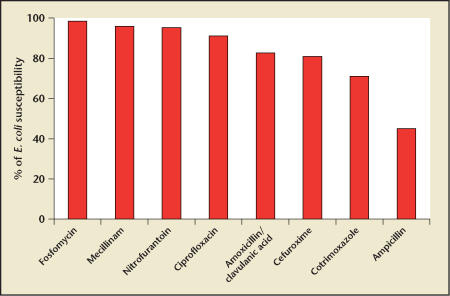
Giancarlo Schito, MD,4 (Italy) presented the results of a recent study examining the epidemiology and resistance in uncomplicated UTI in Europe and Brazil (Figure 1). The group performed an international surveillance study involving 9 countries, and monitored the antimicrobial susceptibility of uropathogens with the aim of ranking the present usefulness of drugs employed in the therapy of this condition. The investigators were able to base their recommendations for antimicrobial therapy on recent epidemiological data collected in 65 centers during 2004–2006. The study recruited 4241 eligible women aged 18–65 years with uncomplicated UTI, of whom 3172 patients showed positive bacteriuria (cfu ≥ 104/mL). As an example of the data collected, in E. coli bacteriuria (the primary uropathogen in this study), susceptibility was highest for fosfomycin (98.4%), followed by mecillinam (95.9%), nitrofurantoin (95.2%), ciprofloxacin (91.2%), amoxicillin/clavulanic acid (82.6%), cefuroxime (80.9%), cotrimoxazole (71.1%), and lowest for ampicillin (45.0%). According to these patterns of E. coli prevalence and resistance, ampicillin, cotrimoxazole, and cefuroxime should not be recommended for empiric therapy of UTI in all countries monitored. The increase in quinolone resistance among community- acquired urinary E. coli is a cause of concern. Fosfomycin, mecillinam, and nitrofurantoin have preserved their overall in vitro efficacy and represent effective options when dealing empirically with these common conditions.
Figure 1.
Antimicrobial susceptibility of E. coli bacteriuria among women aged 18–65 years with uncomplicated UTI. Data from Schito G.4
Worldwide, quinolones are being used as the most common antimicrobial for all UTIs, both complicated and uncomplicated. Raul Raz, MD,5 (Israel) explored risk factors for developing quinolone resistance in uropathogens in the community. UTI is the most common bacterial infection seen in the community, and E. coli is responsible for about 70% to 80% of all the uropathogens. Quinolones are one of the most widely used antibiotics in the community for the treatment of UTI, and it is this unfortunate excessive use of the agent that has led to a considerable and worrying increase in the rate of E. coli resistant isolates in many countries. The magnitude of the problem worldwide is becoming very apparent. Inasmuch as the major risk factor associated with the development of these microorganisms is overuse, physicians (including urologists) must practice antibiotic stewardship and avoid the empiric use of quinolones when other antimicrobials may be adequate.
Main Points.
A study found periurethral colonization with E. coli strains causing recurrent urinary tract infection (UTI) of women 1 week prior to the new UTI, supporting the classic model of reinfection by E. coli emerging from an intestinal reservoir. Other data suggested that some recurrences may originate from uropathogens lying dormant in the bladder. The latter phenomenon could require novel therapies.
Available data support short course antimicrobial therapy for acute uncomplicated UTI, with 3 days as the current accepted standard of therapy.
Fosfomycin, mecillinam, and nitrofurantoin have preserved their overall in vitro efficacy against urinary E. coli. Ampicillin, cotrimoxazole, and cefuroxime should not be recommended for empiric therapy of UTI.
Excessive use of quinolones for treatment of UTI has considerably increased the rate of E. coli resistant isolates in many countries.
References
- 1.Hooton TM. Relationship of vaginal flora to asymptomatic bacteriuria and acute cystitis; Combined Meeting of the 25th International Congress of Chemotherapy and the 17th European Congress of Clinical Microbiology and Infectious Diseases; March 31– April 3, 2007; Munich, Germany. [Google Scholar]
- 2.Schaeffer AJ. Recurrent UTI—relapse or reinfection?; Combined Meeting of the 25th International Congress of Chemotherapy and the 17th European Congress of Clinical Microbiology and Infectious Diseases; March 31–April 3, 2007; Munich, Germany. [Google Scholar]
- 3.Nicolle L. Success and failure with short-term therapy; Combined Meeting of the 25th International Congress of Chemotherapy and the 17th European Congress of Clinical Microbiology and Infectious Diseases; March 31– April 3, 2007; Munich, Germany. [Google Scholar]
- 4.Schito G. Epidemiology and resistance in uncomplicated UTI—a recent European study (ARESC); Combined Meeting of the 25th International Congress of Chemotherapy and the 17th European Congress of Clinical Microbiology and Infectious Diseases; March 31– April 3, 2007; Munich, Germany. [Google Scholar]
- 5.Raz R. Risk factors for quinolone resistance and ESBL-producing pathogens in the community; Combined Meeting of the 25th International Congress of Chemotherapy and the 17th European Congress of Clinical Microbiology and Infectious Diseases; March 31–April 3, 2007; Munich, Germany. [Google Scholar]