Abstract
This is a 10-year follow-up survey of a 1996 study of all dentists in Illinois holding a permit to administer sedation or general anesthesia. The survey describes the scope of sedation and anesthesia services provided in dental offices in Illinois. A mail survey was sent to 471 dentists who were registered with the department of professional regulation to administer sedation or general anesthesia. Classification by specialty area of practice showed: 63% (84% in 1996) are oral and maxillofacial surgeons, 20% (11% in 1996) general dentists, 6% (5% in 1996) periodontists, 9% (0% in 1996) pediatric dentists, 1% (less than 1% in 1996) dentist anesthesiologists. Advanced cardiovascular life support (ACLS) training was reported by 90% (85% in 1996) of the respondents. The total number of sedations and general anesthetics administered for the year was 115,940. Two mortalities and two cases of long-term morbidity were reported for the 10-year period. Respondents reported that 30 patients required transfer to a hospital but suffered no long-term morbidity. Other practice characteristics were detailed.
Keywords: Dental sedation, Dental anesthesia, Morbidity and mortality, Practice parameters
In 1996 a survey was conducted in Illinois of all dental practitioners with a Type A permit for parenteral conscious sedation, or a Type B permit for deep sedation/general anesthesia.1 Unlike previous studies, this survey did not focus on just one group of practitioners such as oral and maxillofacial surgeons, but included all dentists regardless of specialty.2–4 This survey was published in the journal, Anesthesia Progress. In 2006, a 10-year follow-up survey was undertaken. This survey was also sponsored by the Illinois Dental Society of Anesthesiology and the Illinois Society of Oral and Maxillofacial Surgeons (ISOMS). The survey was intended to accumulate data and information that describe the scope and many aspects about the sedation and anesthesia services offered in dental offices in Illinois. This type of information is useful to the profession, public health policy advocates, and regulatory agencies. In addition, Illinois, in the heart of the Midwest and the crossroads of America, is often a mirror reflecting trends occurring in other parts of the country.
Some of the issues addressed in the survey include: practitioner's age, years in practice, type of practice (specialty), advanced cardiovascular life support (ACLS) training, participation in peer review programs, office accreditation, staffing, agents used, intubation in office, number of cases treated, morbidity, mortality, use of automated external defibrillator, and office stocking of dantrolene.
Why was an updated survey done at this time? In addition to being the 10-year anniversary of the original survey, a number of changes have occurred during this period that have significantly impacted dental anesthesia and sedation. In Illinois this includes a number of regulatory changes.5 The Type A permit was changed in scope from “parenteral conscious sedation” to “conscious sedation.” The broader permit was intended to regulate all practitioners who administer conscious sedation, regardless of the route of drug administration. This revision includes providers of oral sedation. New rules also mandated that annual continuing education credits be earned in sedation/anesthesia for all practitioners with a sedation/anesthesia permit. In addition, the American Association of Oral and Maxillofacial Surgeons (AAOMS) passed a requirement for mandatory participation in its office anesthesia review program for all of its members.6
Other events had occurred apart from regulatory changes. New inhalation agents such as sevoflurane (Ultane) became available. The supply of methohexital (Brevital) was interrupted for many months due to manufacturing problems, and generic forms of propofol (Diprivan) and midazolam (Versed) had become available. Also, during this period, after making several unsuccessful attempts to be recognized as specialists, the practice of dentist anesthesiologists became more visible.
Questions about the morbidity and mortality associated with dental sedation/anesthesia continue to haunt the profession with conflicting anecdotal reports, closed claim reviews, and self-reported studies. All of the above created the climate for the 2006 survey.
METHODS
A mail survey was sent to all dentists in Illinois registered with the Illinois Department of Professional regulation with either a Type A or Type B sedation/anesthesia permit (n = 471). The survey consisted of 25 multiple-choice or fill-in-the-blank questions on 3 pages. The time frame referenced covered the period from January 1, 1996 through December 31, 2005. The identity of the respondents remained anonymous to the investigators. No identifying information was requested. The surveys were returned in sequentially numbered envelopes, which corresponded to the mailing list. A mailing manager opened the completed surveys, separated the envelopes from the surveys, and forwarded only the completed surveys to the investigators. A second mailing was made approximately 6 weeks later by the mailing manager to those practitioners who had not responded to the first mailing. No attempt was made at a third mailing. None of the questions requested any patient identity or confidential patient information. The data were entered into a computer database for evaluation and statistical analyses. The study was submitted to the University of Illinois, Chicago Institutional Review Board and was granted exempt status.
RESULTS
Of the 471 original mailings, 27 were excluded from the pool because they were returned as undeliverable or deceased. Of the questionnaires returned from the 2 mailings, a total of 305 were found usable. This was a response rate of 69%, which was comparable to the 71% response rate in 1996. A response rate for a survey of this type is considered “good” if it achieves a 70% return. Of the 305 usable responses, not all of the questions were answered in each survey. Therefore, the percentage results are based upon the number of responses made for each individual question.
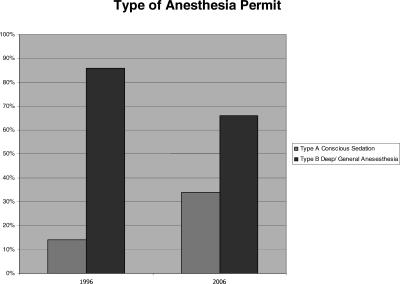
In 2006, 34% of respondents were practitioners with Type A permits for conscious sedation, while 64% had Type B permits for deep sedation/general anesthesia. For comparison in 1996 14% had Type A permits, while 86% had Type B permits. This change reflects an increase in the number of practitioners with type A permits (Figure 1).
Figure 1.
Increase in proportion of practitioners with Type A sedation permit.
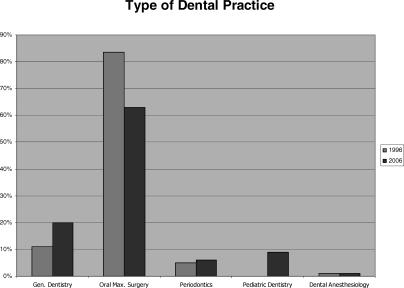
In 2006, the distribution of dental practitioners by type of dental practice was represented by the following: general dentistry 20%, oral and maxillofacial surgery 63%, periodontics 6%, pediatric dentistry 9%, and dental anesthesiology 1%. For comparison, in 1996 the types of practices represented were general dentistry 11%, oral and maxillofacial surgery 84%, periodontics 5%, pediatric dentistry 0%, and dental anesthesiology less than 1%. This distribution may reflect an increase over the 10-year period in the number of dental practitioners who now provide sedation/anesthesia services in areas other than oral and maxillofacial surgery. This increase in the number of pediatric and general dentists with permits is most likely due to the change in the law requiring a permit for oral sedation (Figure 2).
Figure 2.
Comparison in percentage of practitioners by practice type (specialty).
The mean number of years in practice was 20.7 years compared with 16.3 years in 1996. The mean age of the practitioners was 49.8 years, the median was 51.0 years, the minimum age was 30.1 years, and the maximum age was 78.0 years with a standard deviation of 9.7 years. (The age data for 1996 were not available for comparison.)
In the 2006 survey, 5% (n = 15) reported that they possessed a medical degree in addition to the dental degree. This showed a slight increase in comparison to 1996 when only 4% (n = 10) reported the MD degree.
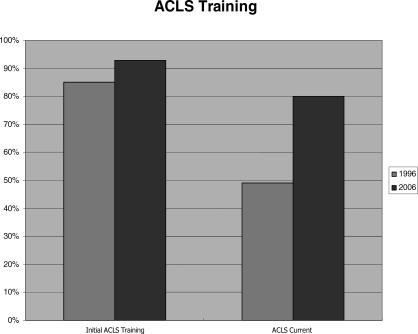
The 2006 survey found that 90% of all practitioners reported having ACLS training, with 80% reporting that their training was current, within the last 2 years. This showed a significant improvement since 1996 when only 85% reported ACLS training, and only 48% had completed recertification (Figure 3).
Figure 3.
Increase in percentage of practitioners reporting initial advanced cardiovascular life support (ACLS) training and current recertification.
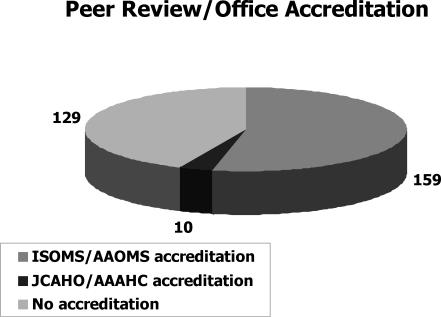
A mixed response was received regarding questions about peer review and office accreditation. Of respondents, 43% (n = 129) did not participate in any peer review or office accreditation process; 53% (n = 159) did participate in the ISOMS/AAOMS office anesthesia evaluation program. Only 4% (n = 10) of respondents had their facilities accredited by either the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) or the Accreditation Association for Ambulatory Health Care (AAAHC) (Figure 4).
Figure 4.
Number of respondents reporting participation in peer review or office accreditation. Abbreviations: ISOMS, Illinois Society of Oral and Maxillofacial Surgeons; AAOMS, American Association of Oral and Maxillofacial Surgeons; JCAHO, Joint Commission on Accreditation of Healthcare Organizations; AAAHC, Accreditation Association for Ambulatory Health Care.
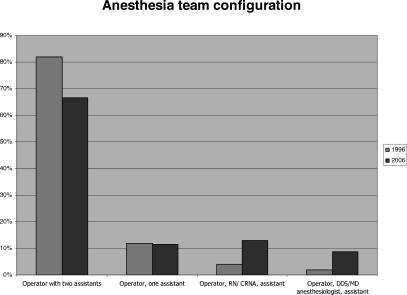
Several of the questions looked at staffing and use of anesthesiologists or nurse anesthetists. The office anesthesia team configuration most frequently used the following patterns: operator with 1 assistant 11.5% (12% in 1996), operator with 2 assistants 66.5% (82% in 1996), operator with a certified registered nurse anesthetist (CRNA) or RN and an additional assistant 13% (4% in 1996), operator with MD/DDS anesthesiologist and an additional assistant 8.8% (2% in 1996) (Figure 5). For clarification, in Illinois, a dentist wishing to utilize the services of a nurse anesthetist must possess a sedation/anesthesia permit equivalent to the level of sedation being administered. On the other hand the dentist does not need to have a sedation/anesthesia permit if the services of an MD/DDS anesthesiologist are utilized. An additional question attempted to further define the picture by asking if the practitioner ever utilized the services of a CRNA, MD anesthesiologist, or DDS anesthesiologist. The results were as follows: CRNA 10%, MD anesthesiologist 9%, and DDS anesthesiologist 15%.
Figure 5.
Most commonly utilized anesthesia team configuration as a percentage of respondents reporting.
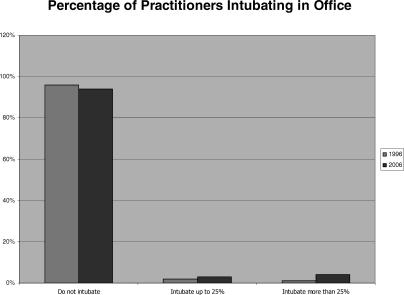
Elective intubation in the office setting is always under close scrutiny. Responses to this procedure were as follows: do not intubate 94% (96% in 1996), intubate less than 25% of cases 3% (2% in 1996), intubate more than 25% but less than 75% of cases 2% (1% in 1996), and intubate more than 75% of cases only 2% (0% in 1996) (Figure 6).
Figure 6.
Percentage of practitioners intubating in office remains low.
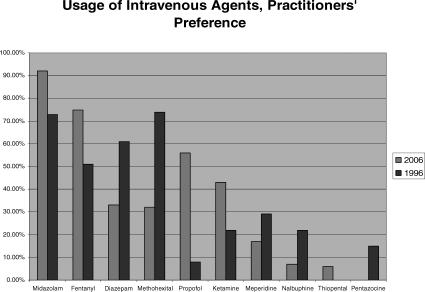
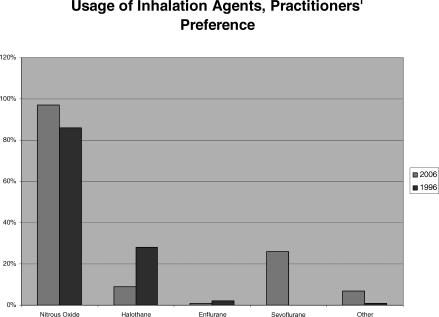
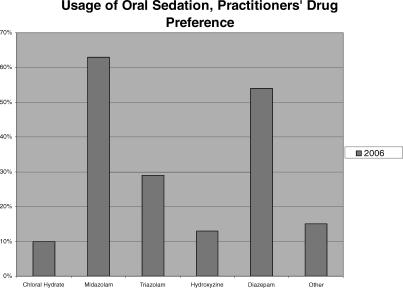
The questionnaire also investigated the practitioner's preference for drugs used in the dental office setting. These included inhalation agents, intravenous agents, and orally administered drugs. There was an increased use of midazolam, propofol, fentanyl, and ketamine, and decrease in diazepam (Valium), methohexital, meperidine (Demerol), nalbuphine (Nubain), and pentazocine (Talwin) (Figure 7). Also, sevoflurane was the most common inhalation anesthetic after nitrous oxide (Figure 8). Midazolam and diazepam remain the most common orally administered drugs (Figure 9).
Figure 7.
Comparison of practitioners' preference for intravenous agents.
Figure 8.
Comparison of practitioners' preference for inhalation agents.
Figure 9.
Comparison of practitioners' preference for oral sedative agents.
To determine the frequency of utilization of anesthesia services in the dental office setting, the respondents were asked to report the number of patients they had treated between January 1, 2005 and December 31, 2005. The results indicated that a total of 109,121 intravenous sedation and general anesthesia cases by all dental practitioners were completed, with 100,269 (92%) cases having been treated by oral and maxillofacial surgeons. The utilization of oral sedation by all dentists for the same time period totaled 6819 cases, of which 2959 (43%) were treated by oral surgeons. Thus, a total of 115,940 patients were treated under some form of sedation, not including the use of nitrous oxide analgesia, in the 1-year period. This would indicate that approximately 1% of the people in Illinois received some form of dental anesthesia/sedation that year if there were no repeat procedures done during that time.
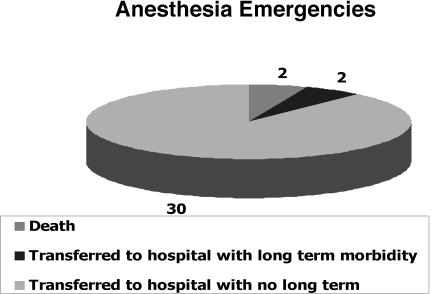
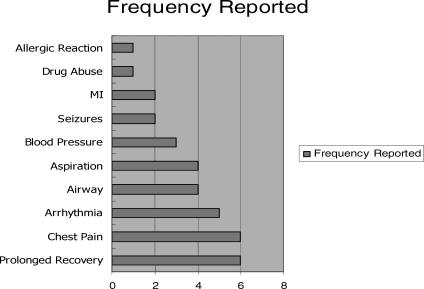
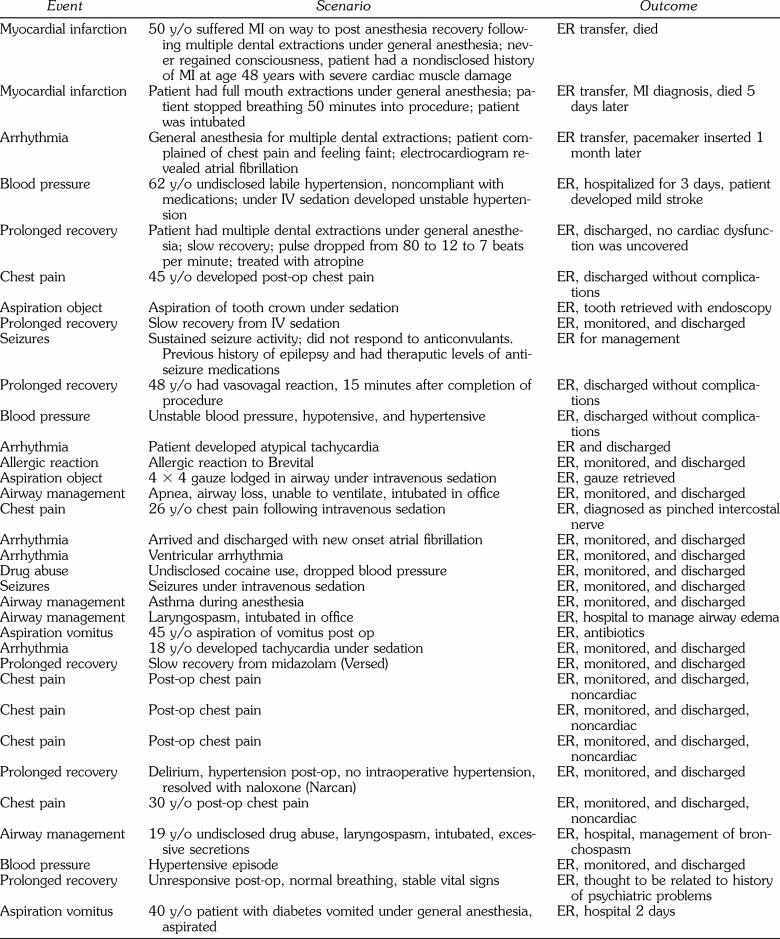
The morbidity and mortality questions covered the same 10-year period of January 1, 1996 through December 31, 2005. Two patient deaths were reported during this period. Two additional patients were transported to the emergency room and suffered long-term morbidities. Thirty additional patients were transported to the emergency room for treatment but were discharged with no long-term morbidities (Figures 10 and 11 and Table).
Figure 10.
The number of reported anesthesia related morbidities and mortalities requiring hospital transfer for the 10-year period.
Figure 11.
Reported anesthesia emergencies categorized by type.
10-Year Morbidity and Mortality
Several questions regarding controversial issues of the standards of care were also included. The use of capnography was reported by 9.0% of practitioners; 63% of practitioners utilized an automated external defibrillator. Dantrolene was stocked in emergency kits by 21% of practitioners.
CONCLUSIONS
Several important practice trends were identified in these data. Over the 10-year period, the proportion of nonoral surgeons providing sedation services has increased. However, based upon the number of patients treated, oral and maxillofacial surgeons provide the vast majority of sedation and anesthesia services in the dental setting. The utilization of CRNAs, DDS, and MD anesthesiologists, although relatively low, is increasing. Although not mandated in Illinois, ACLS training was obtained by 90% of the practitioners and 80% reported that the training was current (within 2 years). This is a significant improvement over the 10-year period and is due in part to the increased availability of ACLS courses and the deliberate commitment by the ISOMS to offer this training on a regular basis every 2 years.
The number of practitioners intubating patients in the office setting remains very low. Although capnograph technology has improved significantly over the last few years, making the devices less expensive and easier to use, the reported utilization is low and corresponds mainly to those practitioners using inhalation agents.
Although office accreditation is now provided by the JCAHO and AAAHC, only 4% of practitioners report that their offices have been accredited. On the other hand 84% of oral and maxillofacial surgeons participate in the ISOMS office anesthesia evaluation program. Since the program is mandatory for all AAOMS members, one must assume that the 16% nonparticipating oral and maxillofacial surgeons are not AAOMS members or are not obligated to participate if they participate with one of the accrediting agencies. An area of possible concern is that 43% of practitioners do not participate in any peer review process.
A significant number of providers (11%) may not be staffing their offices according to the Illinois Dental Practice Act Rules and Regulations which require a minimum of 2 assistants for each operator. This provision applies to the administration of conscious sedation as well as deep sedation/general anesthesia.
Midazolam and fentanyl have become the favored intravenous sedative agents and propofol has replaced methohexital. Midazolam stands out as the most popular oral sedative agent. Sevoflurane has become the primary inhalation anesthetic agent other than nitrous oxide.
Two mortalities were reported over the 10-year period and seem to both have been related to undisclosed medical conditions. This would translate to a mortality rate of approximately 1 death for every 500,000 patients who received anesthetics. Unfortunately, our confidence in the validity of this prediction is low since anecdotal reports of deaths have been higher. There were 2 long-term morbidities reported during the same period. Thirty additional events required transporting patients to the emergency room for management but resulted in no long-term morbidities. Analysis of these events reflects the full range of possible emergency scenarios including myocardial infarction, arrhythmias, blood pressure management, chest pain, aspiration, allergic reaction, airway problems, and prolonged recovery.
Acknowledgments
This survey was endorsed and sponsored by the Illinois Dental Society of Anesthesiology and The Illinois Society of Oral and Maxillofacial Surgeons.
REFERENCES
- Flick WG, Green J, Perkins D. Illinois Dental Anesthesia and Sedation Survey for 1996. Anesth Prog. 1998;45:51–56. [PMC free article] [PubMed] [Google Scholar]
- Lytle JJ. The 1988 anesthesia survey of the Southern California Society of Oral and Maxillofacial Surgeons. J Oral Surg. 1980;38:814–819. [PubMed] [Google Scholar]
- Lytle JJ, Stamper EP. The 1988 anesthesia survey of the Southern California Society of Oral and Maxillofacial Surgeons. J Oral Maxillofac Surg. 1989;47:834–842. doi: 10.1016/s0278-2391(89)80043-6. [DOI] [PubMed] [Google Scholar]
- D'Eramo EM. Morbidity and mortality with outpatient anesthesia: the Massachusetts experience. J Oral Maxillofac Surg. 1992;50:700–704. doi: 10.1016/0278-2391(92)90101-5. [DOI] [PubMed] [Google Scholar]
- Springfield; Illinois: Illinois Dental Practice Acts and Administrative Codes (Part 1220, Section 1220.510 and 1220.520. Last amended December 13, 2002), Illinois Department of Professional Regulation. [Google Scholar]
- American Association of Oral and Maxillofacial Surgeons. Office Anesthesia Manual. 7th Edition. Rosemont, Ill: 2006. [Google Scholar]