Abstract
Introduction
Information Technology (IT) has the potential to significantly support skill-mix change and, thereby, to improve the efficiency and effectiveness of integrated care.
Theory and methods
IT and skill-mix change share an important precondition: the standardisation of work processes. Standardisation plays a crucial role in IT-supported skill-mix change. It is not a matter of more or less standardisation than in the ‘old’ situation, but about creating an optimal fit. We used qualitative data from our evaluation of two integrated-care projects in Dutch eyecare to identify domains where this fit is important.
Results
While standardisation was needed to delegate screening tasks from physicians to non-physicians, and to assure the quality of the integrated-care process as a whole, tensions arose in three domains: the performance of clinical tasks, the documentation, and the communication between professionals. Unfunctional standardisation led to dissatisfaction and distrust between the professionals involved in screening.
Discussion and conclusion
Although the integration seems promising, much work is needed to ensure a synergistic relationship between skill-mix change and IT. Developing IT-supported skill-mix change by means of standardisation is a matter of tailoring standardisation to fit the situation at hand, while dealing with the local constraints of available technology and organisational context.
Keywords: skill-mix, information technology, standardisation, integrated care, eyecare
Introduction
Health care is faced with a number of challenges such as an ageing population, the rise of costs and shortages of skilled health care workers. Skill-mix change of the healthcare workforce is presented as one of the solutions for the problems healthcare is facing [1]: by reallocating tasks among professionals, scarce resources could be used more efficiently, without compromising quality. Several developments have attributed to the current interest in skill-mix: the professionalisation of nurses and paramedics in the 1970s [2,3], periods in which the efficient use of resources was needed, such as that of the lack of doctors in the 1980s [4], a transformation from supply-driven to demand-driven patient centred health care of the 1990s [5], and the breakthroughs in medical technology [6,7]. A well-known example of the latter is the development of X-ray technology, which resulted in radiology as a new specialty in medicine [8]. The potential for substitution is increased if new technologies make tasks simpler than the old technologies [9].
Skill-mix change can be brought about through, for example, task substitution (across professional divides, e.g. from physician to nurse), task delegation (from more qualified to less qualified staff within the same professional group), or task innovation (new tasks for new professionals). On a service level skill-mix change can be brought about through transfer of tasks from a hospital to the community [1]. Therefore, it is closely related to the development of integrated care. Skill-mix change, the focus of this paper, is now one of the key elements of (integrated) care programmes and pathways for groups of patients with a particular disease [10].
In this context, the rise of information technology (IT) may also contribute to skill-mix change. The integration of skill-mix change and use of information technology seems, at least in theory, very effective. For example, information systems could be used to organise all types of data collected during the course of a patient's trajectory and could add structure to it, thereby enhancing its information content. Information systems, like shared electronic records, could also sequence and structure activities, and so facilitate coordination among more professionals and/or in more locations [11]. However, little is known about the promises and problems of IT-supported skill-mix change in everyday practice [10]. In many instances, skill-mix change and IT can do without each other. However, we suggest that for the system's change that is needed to take health care to a next level—as proven in several reports of the American Institute of Medicine [12], IT-supported skill-mix change is a concept that needs serious exploration and research. Despite all attention for information technology and skill-mix change, the two domains are hardly ever connected in the literature.
Standardisation seems to be the core binding concept in discussions about the problems and promises of IT-supported skill-mix change. Both information technology and skill-mix change require standardisation of work processes, decision criteria and terminology to be effective. However, standardisation can also stand in the way of high-quality health care work, when the wrong processes are focused on, or when standardisation is pursued too rigidly. Thus, although their complementary values seem obvious at first glance, in practice a happy marriage between IT and skill-mix change might not be self-evident at all [13].
In this article we will explore the possibilities of creating an optimal fit between skill-mix change and IT through standardisation. We evaluated two well-known screening projects in eyecare in the Netherlands on behalf of the Dutch Society of Ophthalmology (NOG). In both projects, aimed at retinopathy and glaucoma, respectively, tasks were reallocated among professionals, and integrated-care was introduced. IT was used to facilitate the care process. Eyecare is one of the aspects of health care in which the rise of new technologies and new professionals has led to discussion about substitution of tasks [14]. In eyecare, substitution of tasks is related to the development of new imaging techniques that require less specialised skills than traditional instruments like the slit lamp and lenses [15,16]. These developments led to new professionals in Dutch eyecare: the technician as an assistant to the ophthalmologist, and the optometrist with a bachelor's degree in optometry, practicing in optician stores or hospitals [14]. They were also the grounds for delegating tasks outside the ophthalmologic domain, for example, to nurses of diabetic patients.
The structure of this paper is as follows. First, we will briefly describe the two skill-mix projects in eyecare, and the methodology of our evaluation study. In section three, we will explicate our theoretical assumptions about the relationship between skill-mix change, information technology and standardisation. After that, we will present our findings when studying standardisation in the two screening projects, and thereby show the tensions that exist between the design of an optimal match of IT and skill-mix change. In the discussion portion of this article we will answer the question, what is needed for an optimal co-operation of skill-mix change and information technology?
Methods
The setting
The main characteristics of the two integrated care projects for retinopathy and glaucoma are briefly described in Box 1.
Box 1. Two local IT-supported skill-mix change projects in eyecare in The Netherlands.
The Retinopathy project
Setting. Isala Clinics, Zwolle
Aim. Regular screening of all patients with Diabetes Mellitus (DM) for retinopathy, a complication of DM related to micro vascular damage of the eye.
Prior to task substitution. The ophthalmologist was responsible for screening diabetes patients every 1–2 years.
Professionals involved. Ophthalmologists, diabetes nurses. Diabetes nurses perform routine tests every year and educate their patients.
Technologies used. Non-mydriatic retina camera, local hospital network, and electronic patient record.
The New process. Trained diabetes nurses make digital images of the back of the eyes of their patients with a non-mydriatic retina camera. The images are saved in the hospital's network, which is also accessible to the ophthalmologist. The ophthalmologist examines the blood vessel pattern and decides whether a consultation is necessary.
The Glaucoma project
Setting. The Rotterdam Eye Hospital and 10 optician's stores in the Rotterdam area.
Aim. Detecting cases of glaucoma in the population at risk. Glaucoma is an eye disease related to high intraocular pressure.
Before task substitution. People at risk for glaucoma were referred by the primary care physician to the ophthalmologist for tests and a physical examination.
Professionals involved. Ophthalmologists, technicians, and optometrists. Optometrists have a bachelor's degree in optometry, and are specialised in eye health. Technicians assist the ophthalmologist; they perform several visual tests under supervision of the ophthalmologist.
Technologies used. Nerve Fibre Analyser, Internet server.
The New process. Trained optometrists use a Nerve Fibre Analyser to test the condition of the eyes. This camera produces an image and estimates the thickness of the nerve fibre layer using polarised laser light. The images are saved on the Internet in a database that is also accessible to the ophthalmologists and their trained technicians at the hospital. After the assessment, they decide whether a referral to the hospital for ophthalmic evaluation is necessary. This glaucoma screening service has become part of regular care in 2003.
The participants and data collection
Our evaluation of the two screening projects had a multi-method design, combining quantitative and qualitative methods. We used a sociotechnical approach to collect our data, which implied that both the health care professionals and the technologies (cameras, recording forms, protocols) were the objects of our study and analysis.
Unfortunately, the projects had already begun when we commenced the evaluation. Therefore, a before and after design was not possible. Instead, we analysed administrative and patient data to assess the quality of care realised in these projects. These findings were published in the Journal of Telemedicine and Telecare in 2004 [17]. Parallel to this quantitative evaluation, we conducted 37 formal, semi-structured or informal interviews with all ophthalmologists, optometrists, nurses and ICT-experts involved in the two projects. Data collection took place between April 2001 and November 2003. Key informants were interviewed several times. For the retinopathy project, the key informants were the internist, the ophthalmologist and one of the diabetes nurses. In the glaucoma project the key informants were the ophthalmologist, one of the technicians and two optometrists. For the interviews topic lists were used, including the themes cooperation between the professionals, communication patterns, satisfaction with the IT used, and perceived effectiveness and efficiency of the care programme. The interviews were audio taped and transcribed.
In addition, we had email contact with our informants, attended project meetings, joined meetings for (re)training and visited the key informants at their workplace several times to observe their work. All research activities are summarised in Table 1.
Table 1.
Research activities
| Time frame | Research activity | Subjects in Retinopathy project | Subjects in Glaucoma project |
|---|---|---|---|
| July–October 2001 | Observation and unstructured interview | 3 Optometrists | |
| 1 Technician | |||
| 1 Ophthalmologist | |||
| November 2001 | Semi-structured interview | 1 Ophthalmologist | |
| December 2001 | Observation and group interview | 1 Ophthalmologist | |
| 1 Internist | |||
| 1 Diabetes nurse | |||
| 1 Researcher | |||
| March–June 2002 | Semi-structured interview | 1 Ophthalmologist | 1 Project manager |
| 1 IT-developer | 10 Optometrists | ||
| 1 Diabetes nurse | 1 Technician | ||
| 3 Ophthalmologists | |||
| March–April 2003 | Observation and unstructured interview | 4 Optometrists | |
| 1 Technician | |||
| 1 Ophthalmologist | |||
| August 2003 | Semi-structured interview | 1 Ophthalmologist | |
| 1 Internist | |||
| 1 IT-developer | |||
| July 2001–October 2003 | Email and telephone contact | All professionals involved | Project manager |
| July 2001–October 2003 | Attending project meetings | Project team | Project team |
| July 2001–October 2003 | Attending training sessions | Project team and attending optometrists |
We analysed our empirical data for instances of standardisation, and the interaction of the professionals and the technologies in these situations. The data were clustered by emerging themes to answer our research question: “What is needed in these projects for an optimal match of IT and skill-mix change?”
Skill-mix change, information technology and standardisation
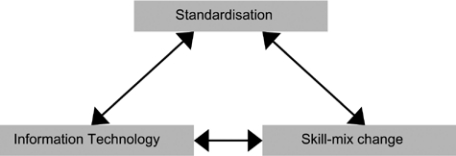
IT and skill-mix change share an important precondition: standardisation of work processes. The relationship between these three concepts is presented in Figure 1.
Figure 1.
Relationship between skill-mix change, information technology and standardisation.
The use of information technology is valuable in redesigned clinical work processes, because it fulfils two roles. First, information systems can be used to organise all types of data collected during the course of a patient trajectory and can add structure to it, thereby enhancing its information content. Second, information systems, like shared electronic records, can sequence and structure activities; it can make synchronous coordination possible; and it can facilitate coordination between more locations [11,18]. Because of these features, IT has the potential to significantly support task delegation and reallocation in skill-mix change projects.
At the same time, redistribution of tasks is often necessary for information systems to optimise their potential impact. For example, structured, detailed recording forms are a prerequisite for electronic patient records that allow support of the decision-making process, or plan all activities in a care trajectory. Yet physicians are often not the best candidate for such detailed and structured data entry tasks: their (relatively expensive) time is better used for tasks that require their clinical expertise. A specialised nurse or clerk, with specific time allotted for such a task, is often both more efficient and more disciplined in the data entry than a physician [10,19].
Standardisation refers to the ‘process of rendering things uniform’. Guidelines, protocols or other procedural standards are both the means and the outcome of standardisation [20]. Therefore, we have to look at the process of standardisation in practice (and not only to a specific procedural standard) to fully understand its impact on the care process.
From the skill-mix perspective, standardisation is often used to assure the quality of the work of the ‘new professionals’ who take over from the physicians. In protocols and practice guidelines, the physicians set down (in detail) what should be done. And conversely, if it is possible to standardise certain (clinical) tasks, it is easier to delegate these tasks from physician to non-physician. In many care programmes efficiency and quality benefits can be realised by delegating tasks to nurses, secretaries, receptionists, etc. [10]. These ‘new’ professionals have to develop the skills to actively use the standards, which implies that they have to know when to discard or adjust the standards according to the individual patient. This proficiency required for a standard to be effective, is at odds with the notion expressed in the literature that standardisation leads to “cookbook” medicine. The professionals involved have to submit themselves to the standards, which is not equivalent to passively following the rules, but to actively allowing the standards to affect their work [20].
In addition, IT requires standardisation as well. The roles of coordination and accumulation [11] can only be fulfilled if professionals align themselves with the standards of the system. For example, these standards can relate to the terminology used in the system (e.g. diagnosis codes), and the procedures incorporated in the system (e.g. sequence of documentation). This property of IT—that it requires standardised use—can be optimally utilised in situations where standardised work is required. It can be a deliberate choice to use IT instead of paper records and forms in skill-mix change.
Standardisation plays an important role in IT-supported skill-mix change. It is not a matter of more or less standardisation than in the ‘old’ situation, but about creating an optimal fit. Unfortunately, this fit is not fully modifiable. Sometimes there are conflicts of interest between or within the professional, clinical, technical and organisational domains. In those situations, tensions can arise when designing standardisation and this often results in standards that are experienced as ‘too strict’ or ‘unpractical’ from the perspective of the ‘new’ professional. For example, the extent to which standards allow flexibility and diversion often depends on the amount of trust non-physicians (nurses, optometrists) have gained from the physicians that delegated their tasks. However, there can also be clinical considerations leading to a choice for strict standards. For example, protocols for chemotherapy have to be meticulously followed by oncology nurse practitioners, not because the oncologists question their proficiency, but because otherwise the therapy will be ineffective or perhaps even harmful.
Results
Both eyecare screening projects can be seen as examples of task innovation and task delegation. “Screening” was split up into “gathering information and examination” and “assessment”. The new diagnostic techniques facilitate skill-mix change, because they replace physical examinations of a specialised ophthalmologist. The (non-mydriatic retina) camera allows the nurse, or whoever is using the camera, to make images of the back of the eye, where changes in the blood vessel pattern (which can be caused by the diabetes) can be detected. The software in the nerve fibre analyser, the camera used in the glaucoma project, estimates the thickness of the nerve fibre layer and calculates the probability of glaucoma. The results of the measurements, the digital images, are accompanied by an anamnesis performed by the optometrist or nurse. The ophthalmologist and the technician use these data to assess the images and to recommend follow-up. In the retinopathy project, the local hospital network is used for data exchange between nurse and physician. In the glaucoma project, a secure Internet connection is used to facilitate data exchange to and from a password-protected server.
These screening processes with delegated tasks could only be designed with the use of (information) technology. In our analysis we focus on three parts of the care process, where (standardised) use of IT plays an important role: performing clinical tasks, documentation, and communication between the professionals. In these areas tensions arose during the course of these projects with regard to standardisation.
Standardisation of clinical tasks
In both projects paper-based protocols were created that stated which tasks had to be performed by the nurse and the optometrist, and how this had to be done. The most important clinical task was the production of high-quality images with a digital camera. The protocols explained the use of this camera both for the process (how to prepare for the measurement, how many images to make) and the outcome (what is a high quality image and how many of these images are requested). That way the images produced by different optometrists and nurses with different cameras would be comparable.
In the glaucoma project the standard stated that six images of each eye had to be made by the optometrist, which would take about 10 minutes. In practice, the optometrists could not always follow this standard. In several interviews the optometrists explained why the standard did not work in practice and their strategy to deal with this. If a patient had difficulty in keeping his eyes still, or if he had an eye disease, such as cataracts, it was impossible to produce six high quality images within a reasonable time and with reasonable amount of effort. Either, the optometrists made many more images than six per eye (which was even more time-consuming), and then chose the best, or the optometrists decided to make fewer images, because they knew from experience that six images would be impossible within the time limits or because of the patient's condition. The optometrists would then send in fewer images, or images of lower quality. However, if the technician strictly followed the standard, she would have to reject these images and request new ones. In some instances this actually happened, which created extra work for the optometrists. Some optometrists resigned to the situation:
they [the technicians, MM] will know, they have more experience (interview optometrist B, March 2002).
Other optometrists, however, were very uncomfortable with this situation:
If they [the hospital, MM] respond that the image has to be made again, I have my doubts. I don't see added value in asking my client to come again. There just cannot be a better image (Interview optometrist G, March 2002).
In the data we analysed, we found only a few cases in which images were sent back, so quantitatively the problem seemed small. However, in the experience of the optometrists it was a significant problem that caused dissatisfaction. They regarded it as unfair criticism of their work. The optometrists discussed this with the ophthalmologist and the project team decided to set a new standard: at least one image per eye had to be sent to the hospital, provided that it was of high quality.
In the retinopathy project, the use of the retina camera was standardised, but along the way, new standards were introduced that caused resistance with the diabetes nurses. The camera that was purchased for the project was a so-called non-mydriatic camera, which meant that, in principal, the camera did not need dilated pupils to produce well-exposed images. This type of camera was chosen because it would be easy to use and no extra work was involved. According to the standard, dilation with medication was only necessary if the first series of images were too dark, for example because the patient had small pupils. Because dilation of the eyes leads to temporary blurred vision, the diabetes nurses were hesitant to dilate their patients' eyes:
if we have a reason not to dilate our patient's eyes, then we don't…the ophthalmologist knows why we don't use dilation, but he disagrees with our arguments, that's the issue here (Interview diabetes nurse, May 2002).
According to the ophthalmologist, the nurses did not conform to the standard. Too many images could not be assessed, because they were too dark, and according to the ophthalmologist this could have been prevented if more patients' pupils had been dilated. The nurses disputed this, as the large majority of images could be assessed without problems. They wanted dilation to be an exception, not a rule.
Still, the ophthalmologist wanted to change the standard: as a precaution, all patients with small pupils and all patients that previously had dark images would require dilation. The nurses protested; they wanted to dispose of the eye examination altogether. In their opinion, the eye examination should be easy and should not produce a great deal of work for them or too much discomfort for the patient. Their work with the patient involved more than the eye examination: they also needed time for discussing blood glucose levels, the patients' life styles and time for examination of the feet. If the ophthalmologist knows best, then why doesn't he make the images himself, or have someone do it at the ophthalmic department, they argued. The ophthalmologist was not sensitive to the arguments of the diabetes nurses. He did not understand why these nurses were so reluctant to dilate their patient's pupils, and approached the ‘problem’ from a different perspective:
That stuff is not dangerous, I would drink it myself! Maybe they are afraid that something goes wrong, and that they are responsible, but that is nonsense. If I ask them to do this, it is my responsibility, not theirs (Interview ophthalmologist, September 2001).
In both projects, the diagnostic instruments are easy to use, according to the ophthalmologists:
“I could teach you [the interviewer, MM] to make and interpret the retina images in two days” (Interview ophthalmologist retinopathy project, September 2001) and “Anyone can learn to make images in two weeks” (Interview ophthalmologist glaucoma project, May 2002).
Standards were designed to prescribe the use of the nerve fibre analyser and the retina camera. In practice, however, tensions arose among the physicians who made the protocol and the optometrists and nurses who had to use it. These tensions were due to poor or unfunctional standardisation. In the glaucoma project the standard was updated to allow for more flexibility. This improved the workability of the standard. In the retinopathy project the standard was changed in an unexpected way as the technology now had to be used differently than intended (i.e. for dilated pupils only, while it was designed for non-dilated pupils). While this flexible approach in the glaucoma project resulted in more satisfaction for the optometrists and technicians, the strict approach in the retinopathy project caused dissatisfaction and even discussions about the skill-mix change itself.
Standardisation of data recording
In both eyecare projects, the transfer of information between the professionals about their separate tasks was important for the screening process as a whole. For this, the recording of data had to be standardised; the protocols codified which information was expected from which professional, in which format and at what time. In the glaucoma project, the patient file was a structured recording form on the Internet, which had to be filled out completely, before the data could be saved in the database. This mandatory character was beneficial for the hospital, since availability of all the data they needed for reviewing a patient's status was guaranteed.
For the optometrists, however, these structured procedures had some disadvantages, and they had to find alternatives to manage them.
Firstly, since the structured recording form was derived from the clinical protocol, diversion from the protocol (as we saw in the previous paragraph) could lead to problems with the data recording. For example, behind the protocol lied the assumption that a patient has two eyes, and that both eyes needed to be tested by the optometrist. Therefore, the form requested two files per patient. However, there could be several reasons for an optometrist to confine him- or herself to examining only one eye: a patient may have been blind in one eye; or have one-sided cataract or another eye disease that made it impossible to analyse the nerve fibre layer with the camera. The most common reason, though, might be that the hospital requested that, for a particular eye, new images were made because of low quality. From our observations, we know that the optometrists found an alternative when dealing with this situation. They either attached the file with images from the one eye two times, or they used old images or false images and added an explanatory note to the form.
Secondly, the optometrists were not satisfied with the pre-structured forms, from which they had to choose from a limited list of options, for example regarding the perceived quality of the images.
The options are very black-and-white. Often, an image is neither bad nor average. It's somewhere in between. How should I record that? (Interview optometrist C, March 2002).
They also lacked the option best image possible. The system's feature to attach notes in free text was not used very often. As one of the optometrists confessed:
I often forget to add a note that this image was the best image possible (Interview optometrist E, March 2002).
The third disadvantage was related to the technology used in the glaucoma project. The recording form on the Internet only allowed for complete entries. In the interviews, optometrists affirmed that this feature was useful, knowing that they were likely to forget things if the form did not guide them. However, they also experienced a downside: if one or more items were missing, the electronic form could not be saved, and the data would not be stored in the database. In fact, all data would be lost and the optometrist had to fill out the form once again. It is not practical to fill out the form during the patient examination, as not all data are available at that moment. Most optometrists wanted to review the images thoroughly after the patient had left, so they usually filled out the electronic form at quieter times, or after their store had been closed. We observed that, as a workaround, they used a paper form during the examination, or made notes on a piece of paper. Although this meant double work, the optometrists expressed to us that it was more efficient than using the Internet server only.
These three examples from the glaucoma project show that a structured recording method required by the information technology can be a barrier for the users and for the care process. The required completeness and the inaccuracy are examples of technological design failures that can, at least partly, be solved by building in more flexibility. If the optometrist can save incomplete recording forms in the database or send in only one set of images, he does not need the workaround. And if the list of choices for image quality matches the definitions of the users (good, average, moderate, bad) they will be more satisfied. However, for the project team, complete and structured patient records might be preferred to allow for continuous quality assessment by calculation of indicators like ‘% images of high quality’. The managerial or quality domain might conflict with the interest of the optometrists, who want an easy-to-use recording form that is tailored to their specific needs.
Standardisation of communication
In both projects, the professionals who performed part of the eye screening were situated in geographically separated places. In the retinopathy project, the diabetes nurses worked at the outpatient diabetes clinic and in a few remote nursing homes, while the ophthalmologist was situated in the outpatient clinic of the ophthalmology department. In the glaucoma project, the optometrists were situated in optician shops throughout the extended Rotterdam area. As the professionals did not normally come into contact with each other, formal communication had to be arranged. In both projects, the communication was mainly the transfer of clinical and administrative data like the images, the visual parameters and the advice for follow up. For this, they used the Internet and the hospital network, and thereby standardised the communication. Oral communication with the hospital seemed to be unnecessary: when the ophthalmologists or technicians saw a new case in the database, they knew that their assessment was expected.
However, there are also drawbacks to standardised communication. Firstly, as explained in a previous paragraph, there is the risk that the context of the data collection will be lost from view. There is a risk of jumping to conclusions, especially if the images are of low quality. For example, in the glaucoma project one of the optometrists received feedback from the hospital stating “Low quality! Send us new images”. Because the person who assessed the images (the technician) was not there when the image was made, he or she interpreted the image from a different perspective: "the image is too dark” or “the image is blurred" and, therefore, the optometrist had to do his work again. The optometrist, in turn, gave another interpretation:
We always try to make the best image. ‘Better’ is not possible, under those circumstances… it is not realistic that the hospital asks us to make that image again (Interview optometrist G, March 2002).
A second risk follows naturally from the de-contextualisation of data: the tone of the communication. Feedback from the technician in short notes like “Low quality! Send us new images”, can be (mis) understood by the optometrist as a negative or critical remark:
The last few months, we noticed that the feedback from the hospital is sometimes very unfriendly… they use terms that are not always appropriate (Interview optometrist A, March 2002).
The lack of other ways of communication (outside the standardised form) can lead to deterioration of the communication and dissatisfaction with each other's work. For example, some of the optometrists did not feel appreciated for their work of making a good image with the nerve fibre analyser, when they received ‘negative’ feedback.
When is an image good enough? There are no agreements on this… we often doubt whether the image is good enough, but we decide to send it because it is the best result we can get (Interview optometrist A, March 2002).
It is striking that at the inception of the project, the ophthalmologist and technician expected that the optometrists would call if they were unsatisfied, or if they had questions regarding the feedback from the hospital. In practice only a few of the optometrists used the telephone as a regular communication tool alongside the Internet system. Those optometrists who called frequently, were satisfied with the communication. However, most optometrists said in the interviews that they hardly ever had telephone contact with the hospital. They confessed that this was due to lack of time or interest:
we don't contact the hospital, especially if a client is assessed as normal, while we thought he was suspect (Interview optometrist D, March 2002).
Others had a negative experience:
“I got the feeling that my calls were not appreciated, because of the tone used by the technician.” (Interview optometrist F, March 2002).
Thus, for most optometrists, the main contact between the hospital and the optician stores was through the electronic recording form.
In the glaucoma project, the electronic recording form was used as a standardised communication tool between the optometrists, the technicians and the ophthalmologists in the Rotterdam area. However, not only geographical, but also professional boundaries had to be crossed. This ‘social distance’ between the professionals was one of the causes of dissatisfaction about the communication. This was also one of the main reasons why the communication problems in this project could not be solved with technical adjustments.
Discussion
In this paper the role of IT in skill-mix change has been explored. IT can be used to accumulate information and to coordinate tasks. However, we demonstrated that it is more than a tool, because IT also standardises and transforms data and tasks. To understand what IT does in skill-mix change, we examined the way IT transformed skill-mix, while at the same time we showed that IT was highly dependent on the health care professionals to become embedded in daily practice. In both eyecare projects, for example, data recording had to be standardised to transfer information among the professionals about their separate tasks. Protocols codified which information was expected from which professional, in which format and at what time. As the patient file was a structured recording form on the Internet, which had to be filled out completely, before the data could be saved in the database, all data the hospital needed to review a patient's status were guaranteed.
The way standards are designed and used highly influences the ‘success’ of IT-supported skill-mix change. Firstly, we demonstrated that standardisation of clinical tasks can interfere with the work practices of optometrists and diabetes nurses, and can lead to tensions in daily practice. A more flexible approach to the use of protocols seemed to be a solution for this dissatisfaction [20,21], but then the physicians should support this development. In one of the projects this was not the case. Secondly, we showed that structured recording, although desirable for skill-mix change, needs workarounds. Professionals have to play an active role in matching the technology to their work [20]. Thirdly, we showed a change in communication patterns in these projects, when recording forms replaced informal, personal contact. Unintentionally, this affected teamwork [22,23]. Especially for the glaucoma project it seems important to restore the ‘old’ communication patterns.
Strategies for standardisation can only be recognised and valued if the ‘whole picture’ is taken into account; that is, if we look at IT and people (the professionals and users of the technology) together. Moreover, standardisation was a valuable concept to show the co-construction of IT and skill-mix change. Both in research and practice, focusing on only one aspect of skill-mix change has many shortcomings. By isolating technology and focusing on IT-solutions, it is hard to circumvent technologically determinist accounts. The “embeddedness” of IT in and dependence upon work practices and the professionals that use IT, is easily lost from view. By looking at the processes ‘behind the tools’, for example the standardisation process, the interrelation of the technical and the social becomes visible. Similarly, if the only focus is on the professionals involved in skill-mix change, there is the risk of overlooking IT as an essential element of the process. In many skill-mix change projects, discussions about standards can be rephrased as discussions about proficiency and trust, as we saw in these two cases as well, regarding the administering of dilation medication and the complete recording forms. Only if we consider IT as well, we see that trust is redefined in these projects. Trust is not (only) a matter of knowing each other and recognising each other's skills, but it is shaped by and incorporated in the technology; the standardised cameras, the recording forms, and the data exchange that were crucial in these skill-mix change projects [24].
Recognising the interdependency of skill-mix change and information technology is not only relevant for research into skill-mix change [25], but also for those who are actively involved in (developing) skill-mix change projects and integrated care programmes. They should be interested in more than functional, technical and implementation issues of IT. IT can highly influence and transform work practices. Hence, it is important to know the possibilities and pitfalls of IT in advance, as well as the organisational context in which IT is going to be used.
Conclusion
IT is not only a tool that can be used in skill-mix change projects to accumulate information and to coordinate tasks of the various professionals involved in the care process. IT also standardises and transforms data and tasks. Therefore, it has to be carefully integrated with the work of the healthcare professionals involved in skill-mix change. Developing IT-supported skill-mix change by means of standardisation, is a matter of tailoring standardisation to fit the situation at hand, while dealing with the local constraints of available technology and clinical and organisational context. It is a challenge to combine the best of both worlds.
Contributor Information
Marleen de Mul, Institute of Health Policy and Management, Erasmus Medical Centre, Rotterdam, The Netherlands.
Antoinette de Bont, Institute of Health Policy and Management, Erasmus Medical Centre, Rotterdam, The Netherlands.
Marc Berg, Institute of Health Policy and Management, Erasmus Medical Centre, Rotterdam, The Netherlands.
Reviewers
Guus ten Asbroek, MSc, PhD, Department of Social Medicine, Academic Medical Centre, University of Amsterdam, The Netherlands.
Henry Potts, PhD, Lecturer, Centre for Health Informatics and Multiprofessional Education (CHIME), University College London, UK.
Jeannette Pols, Dr., Department of General Practice, Medical Ethics, Amsterdam Medical Centre, University of Amsterdam, The Netherlands.
References
- 1.Sibbald B, Shen J, McBride A. Changing the skill-mix of the health care workforce. Journal of Health Services Research and Policy. 2004 Jan;9(Suppl 1):28–38. doi: 10.1258/135581904322724112. [DOI] [PubMed] [Google Scholar]
- 2.Fay JK, Jones A, Ram FS. Primary care based clinics for asthma. Cochrane Database Systematic Review. 2002;1 doi: 10.1002/14651858.CD003533. CD003533. [DOI] [PubMed] [Google Scholar]
- 3.Smith B, Appleton S, Adams R, Southcott A, Ruffin R. Home care by outreach nursing for chronic obstructive pulmonary disease. Cochrane Database Systematic Review. 2001;3 doi: 10.1002/14651858.CD000994. CD000994. [DOI] [PubMed] [Google Scholar]
- 4.Richardson G, Maynard A, Cullum N, Kindig D. Skill mix changes: substitution or service development? Health Policy. 1998 Aug;45(2):119–32. doi: 10.1016/s0168-8510(98)00038-4. [DOI] [PubMed] [Google Scholar]
- 5.Griffin S, Kinmonth A. Diabetes care: the effectiveness of systems for routine surveillance for people with diabetes. Cochrane Database Systematic Review. 2000;2 doi: 10.1002/14651858.CD000541. CD000541. [DOI] [PubMed] [Google Scholar]
- 6.Buchan J, Dal Poz MR. Skill mix in the health care workforce: reviewing the evidence. Bulletin of the World Health Organisation. 2002;80(7):575–80. [PMC free article] [PubMed] [Google Scholar]
- 7.Detmer DE. Information technology for quality health care: a summary of United Kingdom and United States experiences. Quality in Health Care. 2000 Sep;9(3):181–9. doi: 10.1136/qhc.9.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blume S. Insight and industry: on the dynamics of technological change in medicine. London, Cambridge MA: MIT Press; 1991. [Google Scholar]
- 9.Richardson G. Identifying, evaluating and implementing cost-effective skill mix. Journal of Nursing Management. 1999 Sep;7(5):265–70. doi: 10.1046/j.1365-2834.1999.00137.x. [DOI] [PubMed] [Google Scholar]
- 10.Berg M, Schellekens W, Bergen C. Bridging the quality chasm: integrating professional and organisational approaches to quality. International Journal for Quality in Health Care. 2005 Feb;17(1):75–82. doi: 10.1093/intqhc/mzi008. [DOI] [PubMed] [Google Scholar]
- 11.Berg M. Accumulating and coordinating: occasions for information technologies in medical work. Computer Supported Cooperative Work. 1999;4:373–401. [Google Scholar]
- 12.Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academy Press; 2001. [Google Scholar]
- 13.Oudshoorn N, Pinch T, editors. How users matter. The co-construction of users and technology. London/Cambridge MA: MIT Press; 2003. [Google Scholar]
- 14.Stevens FC, Horst van der F, Hendrikse F. The gatekeeper in vision care. An analysis of the co-ordination of professional services in The Netherlands. Health Policy. 2002 Jun;60(3):285–97. doi: 10.1016/s0168-8510(01)00199-3. [DOI] [PubMed] [Google Scholar]
- 15.Sharp PF, Olson J, Stachan F, Hipwell J, Ludbrook A, O'Donnell M, et al. The value of digital imaging in diabetic retinopathy. Health Technology Assessment. 2003;7(30):1–119. doi: 10.3310/hta7300. [DOI] [PubMed] [Google Scholar]
- 16.Greenfield DS. Optic nerve and retinal nerve fiber layer analyzers in glaucoma. Current Opinion in Ophthalmology. 2002 Apr;13(2):68–76. doi: 10.1097/00055735-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Mul de M, Bont de AA, Reus NJ, Lemij HG, Berg M. Improving the quality of eye care with tele-ophthalmology: shared-care glaucoma screening. Journal of Telemedicine and Telecare. 2004;10(6):331–6. doi: 10.1258/1357633042602107. [DOI] [PubMed] [Google Scholar]
- 18.Osterlund C. Mapping medical work: documenting practices across multiple medical settings. Journal of the Centre for Information Studies. 2004;5(3):35–43. [Google Scholar]
- 19.Massaro TA. Introducing physician order entry at a major academic medical centre: I. Impact on organisational culture and behaviour. Academic Medicine. 1993 Jan;68(1):20–5. doi: 10.1097/00001888-199301000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Timmermans S, Berg M. The gold standard: the challenge of evidence-based medicine and standardisation in health care. Philadelphia: Temple University Press; 2003. [Google Scholar]
- 21.Quaglini S, Stefanelli M, Lanzola G, Carporuzzo V, Panzarasa S. Flexible guideline-based patient careflow systems. Artificial Intelligence in Medicine. 2001 Apr;22(1):65–80. doi: 10.1016/s0933-3657(00)00100-7. [DOI] [PubMed] [Google Scholar]
- 22.Strauss A, Fagerhaugh S, Suczek B, Wieder C. Social organisation of medical work. Chicago: University of Chicago Press; 1985. [Google Scholar]
- 23.Gold N. Teamwork, multidisciplinary perspectives. New York: Palgrave Macmillan; 2005. [Google Scholar]
- 24.Kumar K, Van Dissel HG, Bielli P. The merchant of Prato—Revisited. Toward a third rationality of information systems. MIS Quarterly. 1998;22(2):199–226. [Google Scholar]
- 25.Stoop AP, Heathfield H, Mul de M, Berg M. Evaluation of patient care information systems. Theory and practice. In: Berg M, editor. Health information management: Integrating ICT in health care work. London: Routledge; 2004. pp. 206–29. [Google Scholar]