Abstract
The study was designed to evaluate the prognostic value of the 6-minute walk test in stable outpatients with heart failure.
We prospectively studied 43 patients (6 women and 37 men) who had chronic heart failure secondary to ischemic heart disease or idiopathic cardiomyopathy. All patients had left ventricular systolic dysfunction (ejection fraction, ≤0.40), and they were in stable New York Heart Association functional class II or III heart failure. All patients were evaluated by M-mode and 2-dimensional echocardiography. At the outset, walking distances of all the patients were evaluated by the 6-minute walk test. The patients were divided into 2 groups: Group I, patients with a 6-minute walk test distance of ≤300 m; and Group II, patients with a 6-minute walk test distance of >300 m. The patients were then monitored for a period of 2 years in regard to cardiac death.
The mortality rate was significantly higher in patients with a 6-minute walk test distance of ≤300 m than in patients with a 6-minute walk test distance of >300 m (79% vs 7%; P <0.001). The death risk was found to be significantly higher in patients with a distance of ≤300 m (P=0.005). The death risk was also higher in patients whose left ventricular ejection fraction was ≤0.30 (P=0.02).
We conclude that a 6-minute walk test distance of ≤300 m is a simple and useful prognostic marker of subsequent cardiac death in patients with mild-to-moderate heart failure. (Tex Heart Inst J 2007;34:166–9)
Key words: Exercise test; heart failure, congestive/mortality; 6-minute walk test; predictive value of tests; prognosis; risk factors; stroke volume
Functional capacity provides strong independent insight into the prognosis of patients with heart failure.1,2 Information on peak oxygen consumption (PvO2) during cardiopulmonary exercise testing is used extensively to evaluate cardiovascular performance. Several studies have supported PvO2 as an independent prognostic index of survival in patients with heart failure.3,4 Similarly, a PvO2 of <10 to 12 mL/kg per min is considered a reliable indicator for heart transplantation.5,6 However, cardiopulmonary exercise testing is both expensive and time-consuming. In addition, approximately 30% of patients with heart failure are unable to perform a maximal symptom-limited exercise test or to tolerate the tight mask used for breath-by-breath gas analysis. The 6-minute walk test (6MWT) has been suggested as a simple, safe, and inexpensive alternative to cardiopulmonary exercise testing.7
The aim of the present study was to prospectively evaluate the prognostic value of the 6MWT in patients with mild-to-moderate congestive heart failure.
Patients and Methods
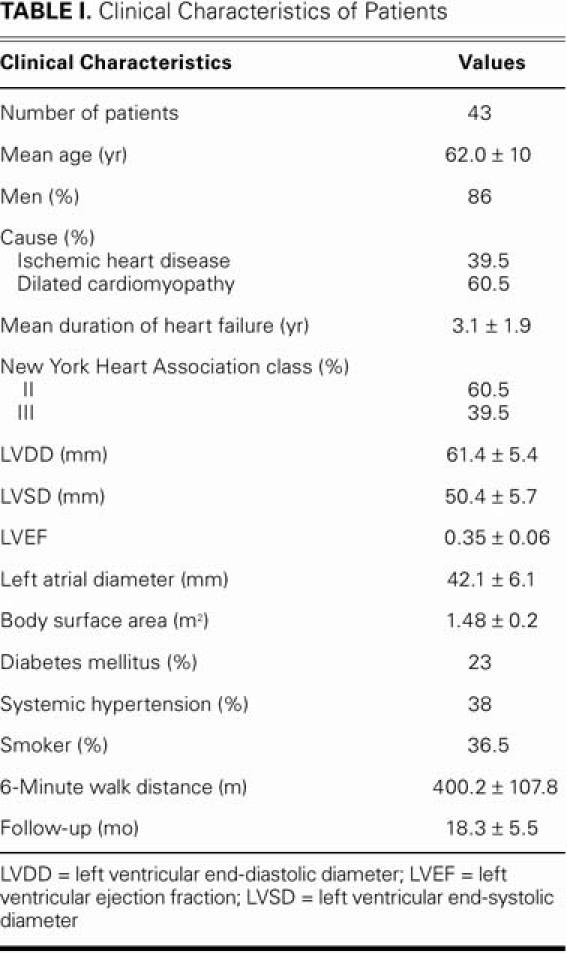
From January 2003 through October 2003, we studied 43 patients (6 women and 37 men) who had stable chronic heart failure secondary to ischemic heart disease or idiopathic cardiomyopathy. All patients underwent treatment for stable heart failure with angiotensin-converting enzyme (ACE) inhibitors for at least 4 weeks and with diuretics for at least 2 weeks. The mean age was 62 ± 10 years. The cause of heart failure was idiopathic dilated cardiomyopathy in 26 patients and ischemic cardiomyopathy in 17 patients. All patients had left ventricular (LV) systolic dysfunction (left ventricular ejection fraction [LVEF], ≤0.40), and all were in stable New York Heart Association (NYHA) functional class II or III heart failure. The functional capacity of 26 patients was class II and that of the remaining 17 was class III. Table I summarizes the patients' clinical characteristics.
TABLE I. Clinical Characteristics of Patients
We excluded from the study patients who had decompensated heart failure, limitation of physical activity due to factors other than exertional dyspnea and fatigue (such as arthritis), psychiatric disorders that could keep the patients from understanding the examination, anemia, and any febrile condition or infectious disease. We also excluded patients who had experienced unstable angina, myocardial infarction, coronary revascularization, or stroke within the previous 2 months. Patients with ischemic heart failure received anti-ischemic treatment (a nitrate) and anti-aggregation treatment (aspirin), in addition to ACE inhibitors and diuretics. None of the patients received β-blocker ther-apy. After the walk test was performed, the patients were given 6.25 mg/day of carvedilol or 25 mg/day of metoprolol succinate, and this was increased to the maximal dose tolerated.
The study conformed to good clinical practice guidelines and followed the recommendations of the Declaration of Helsinki. The protocol was approved by our local ethics committee. Informed written consent was obtained from all patients before enrollment.
We used a GE VingMed® Vivid FiVe® echocardiographic system (GE Ultrasound; Horten, Norway) with a 2.5-MHz probe. All echocardiography was performed by the same investigator. The echocardiographic study was performed in the left lateral decubitus in the parasternal long-axis and 4-chamber views. The LVEF was obtained using Simpson's biplane methods in 2-dimensional echocardiography.8 Left ventricular end-diastolic diameter, LV end-systolic diameter, and left atrial diameter were measured with M-mode echocardiography, using a parasternal window.
The walk test was performed in an indoor corridor 25 m long, according to the recommendations of Guyattand colleagues.7 Patients were instructed to walk the corridor from 1 end to the other, as many times as possible within the permitted time. The test was performed under the control of a physician, who encouraged the patients with remarks such as “you are doing well.” At the end of the 6 min, the physician measured the total distance walked by the patient. On the basis of the distance walked, patients were grouped into 2 different performance levels: Group I, ≤300 m; and Group II, >300 m. The patients were monitored for 2 years in regard to cardiovascular death.
Statistical Analysis
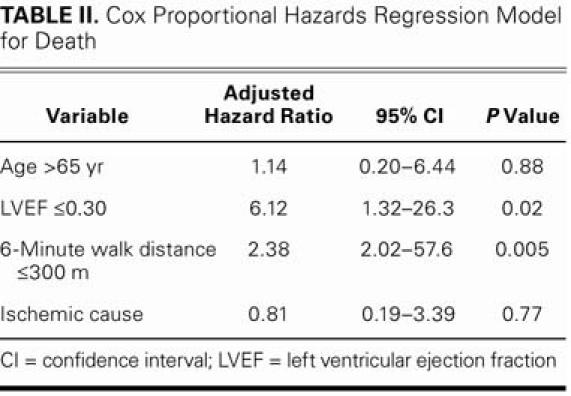
The SPSS version 11.5 statistical program (SPSS Inc.; Chicago, Ill) was used for statistical study. Continuous variables are given as mean ± standard deviation, and categorical variables are given as percentages. The χ2 test was used for the comparison of categorical values. The Cox proportional hazards regression model was used to estimate the relative risk of cardiovascular death. Other variables used to determine basic risk were LVEF ≤0.30, age over 65 years, and ischemic cause of heart failure. Risk ratios were determined with 95% confidence intervals, according to the Cox regression model (Table II). Cardiac death curves were obtained by the Kaplan-Meier method. The log-rank test was used for comparison of the 2 curves. A value of P <0.05 was considered statistically significant.
TABLE II. Cox Proportional Hazards Regression Model for Death
Results
Of the 43 patients studied, 13 (30%) were lost to follow-up. The average follow-up period was 18 ± 6 months.
All patients completed the 6MWT. No clinical complication was recorded during the tests or within the 5-hour period after the tests. The mortality rate in patients whose 6MWT distance was ≤300 m was significantly higher than in patients whose 6MWT distance was >300 m (79% vs 7%; P <0.001, log-rank test). When subgroup analyses were considered, the mortality rate in patients with heart failure due to ischemia was higher (41%) than that in patients with idiopathic cardiomyopathy (23%); however, this difference was not statistically significant.
Risk of death was significantly higher in patients whose 6MWT distance was ≤300 than in patients whose 6MWT distance was >300 m (P=0.005, Cox regression model). In addition, the risk of death was higher in patients with LVEF ≤0.30 than in those with LVEF >0.30 (P=0.02). Old age and ischemic cause of heart failure were not statistically significant in regard to risk of death (P >0.05).
At the end of follow-up (18 months on average), the mortality rate was 11.5% for patients in NYHA classII and 58.8% for patients in NYHA class III; this difference was statistically significant (P=0.001). The Kaplan-Meier curve indicating death rates during follow-up is shown in Figure 1.
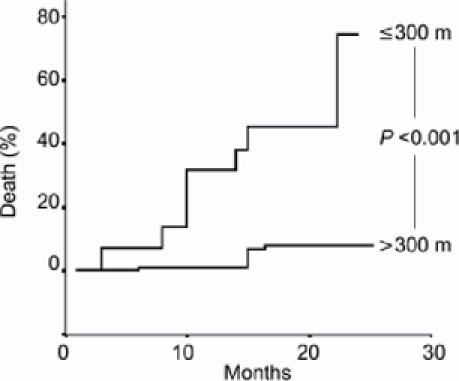
Fig. 1 Kaplan-Meier curves for the 6-minute walk test, according to the distance walked.
Discussion
Studies of Left Ventricular Dysfunction (SOLVD)9 was the 1st large investigation (898 patients) to show a strong connection between distances walked during the 6MWT and death, in cases of NYHA class II and class III heart failure. This prognostic value, however, remains controversial. In a study of 315 moderate-to-severe heart failure patients, Opasich and colleagues10 reported that the distance walked during the 6MWT does not provide prognostic information that can complement or replace oxygen consumption (VO2) or the classic clinical functional class grading system. However, patients in Opasich's study did not receive the recom-mended “encouraging remarks,” despite their having undergone two 6MWTs each, one of which was preparatory. If Opasich's patients did not approach their anaerobic thresholds during the walking exercise, such results might have been influenced by lack of encouragement.
In the study by Rostagno and associates11 of 214 patients with mild-to-moderate heart failure, the mortality rate for patients whose 6MWT distance was <300 m was significantly higher than that for patients whose 6MWT distance was ≥300 m. They concluded that a 6MWT distance of <300 m is a “simple and useful prognostic marker of subsequent cardiac death in unselected patients with mild-to-moderate congestive heart failure.” Cahalin and coworkers12 studied 45 patients referred for heart-transplantation evaluation. A 6MWT distance of <300 m predicted an increased likelihood of death or of hospitalization for inotropic or mechanical support within 6 months, but it failed to predict overall or event-free survival at a follow-up of 62 weeks. Conversely, our results suggest that a walking distance of <300 m during the 6MWT is an independent predictor of death over the long term (18 months on average) in unselected patients with mild-to-moderate heart failure.
Rubim and co-authors13 found that, according to the receiver operating characteristics (ROC) curve, the optimal cut-off value for the distance walked was 520 m in 179 patients with mild-to-moderate heart failure. However, most of the patients in that study were in NYHA class II. Only 6 patients (3%) were in class III. In our study, 40% of the patients were in NYHA class III.
The LVEF is one of the strongest indicators of death in patients with heart failure.13–16 The findings of our study confirm that a lower LVEF is an independent predictor of death.
While Rubim's group13 found no difference between NYHA class I and II in 179 patients with mild or moderate heart failure, they showed that survival for patients in NYHA classes III and IV was <50%, which was significantly different when compared with patients in NYHA class I and class II. Similarly, in our study, the death rate in NYHA class III patients was significantly higher.
In 2,711 patients, Andersson and colleagues17 showed that the mortality rate in heart failure that developed due to ischemia was higher than the mortality rate in heart failure due to other reasons. The mortality rate was also higher among our patients with ischemic heart failure, but the difference was not statistically significant. This may be attributable to the small number of patients in our study.
Recently, there have been reports of several prognostic indicators in heart failure. Anand and associates18 reported their thesis on the value of C-reactive protein as an independent predictor of survival in patients with heart failure. In 2004, de Groote's group19 reported that, for patients with stable heart failure, type-B natriuretic peptide plasma levels and maximal VO2 provide independent information for prognostic risk stratification. Despite the recent appearance of such laboratory prognostic indicators for heart failure, the distance walked in the 6MWT remains a low-cost indicator that is easy to perform and apply.
Cardiopulmonary exercise tests and the 6MWT may induce arrhythmias. When the arrhythmogenic potential of both tests was analyzed for the population studied, both methods showed a high tendency to induce arrhythmias (84.4% and 86.4%, respectively). Therefore, arrhythmias may compromise the safety of both methods—mainly that of the 6MWT, because the patient is not under continuous cardiac monitoring.13 However, during the SOLVD study,9 no complications were recorded for the 833 6MWTs performed. In the present study, no clinical complication was recorded within the 5-hour period after each test. We conclude that the 6MWT was a safe method for evaluating our patients.
The present study has several limitations. The major limitations are the small size of the patient group and the fact that 30% of that population was lost to follow-up. Another significant limitation is that the short duration of the study may have lowered the statistical power of the prognostic findings.
Despite these limitations, this study appears to con-firm that the distance walked during the 6MWT is a highly reliable and independent predictor of cardiac death.
Footnotes
Address for reprints: Sakir Arslan, MD, Ataturk Universitesi Tip Fakultesi, Kardiyoloji Anabilim Dali, 25070 Erzurum, Turkey. E-mail: sarslan@atauni.edu.tr
References
- 1.Cohn JN, Rector TS. Prognosis of congestive heart failure and predictors of mortality. Am J Cardiol 1988;62:25A–30A. [DOI] [PubMed]
- 2.Pilote L, Silberberg J, Lisbona R, Sniderman A. Prognosis in patients with low left ventricular ejection fraction after myocardial infarction. Importance of exercise capacity. Circulation 1989;80:1636–41. [DOI] [PubMed]
- 3.Szlachcic J, Massie BM, Kramer BL, Topic N, Tubau J. Correlates and prognostic implication of exercise capacity in chronic congestive heart failure. Am J Cardiol 1985;55:1037–42. [DOI] [PubMed]
- 4.Myers J, Gullestad L, Vagelos R, Do D, Bellin D, Ross H, Fowler MB. Clinical, hemodynamic, and cardiopulmonary exercise test determinants of survival in patients referred for evaluation of heart failure. Ann Intern Med 1998;129:286–93. [DOI] [PubMed]
- 5.Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH Jr, Wilson JR. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation 1991;83:778–86. [DOI] [PubMed]
- 6.Stevenson LW. Role of exercise testing in the evaluation of candidates for cardiac transplantation. In: Wasserman K, editor. Exercise gas exchange in heart disease. Armonk (NY): Futura Publishing Company, Inc.; 1996. p. 271–86.
- 7.Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985;132:919–23. [PMC free article] [PubMed]
- 8.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989;2:358–67. [DOI] [PubMed]
- 9.Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, et al. Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. JAMA 1993;270:1702–7. [PubMed]
- 10.Opasich C, Pinna GD, Mazza A, Febo O, Riccardi R, Riccardi PG, et al. Six-minute walking performance in patients with moderate-to-severe heart failure; is it a useful indicator in clinical practice? Eur Heart J 2001;22:488–96. [DOI] [PubMed]
- 11.Rostagno C, Olivo G, Comeglio M, Boddi V, Banchelli M, Galanti G, Gensini GF. Prognostic value of 6-minute walk corridor test in patients with mild to moderate heart failure: comparison with other methods of functional evaluation. Eur J Heart Fail 2003;5:247–52. [DOI] [PubMed]
- 12.Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest 1996;110:325–32. [DOI] [PubMed]
- 13.Rubim VS, Drumond Neto C, Romeo JL, Montera MW. Prognostic value of the six-minute walk test in heart failure [in Portuguese]. Arq Bras Cardiol 2006;86:120–5. [DOI] [PubMed]
- 14.Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med 1991;325:293–302. [DOI] [PubMed]
- 15.Cohn JN, Johnson GR, Shabetai R, Loeb H, Tristani F, Rector T, et al. Ejection fraction, peak exercise oxygen consumption, cardiothoracic ratio, ventricular arrhythmias, and plasma norepinephrine as determinants of prognosis in heart failure. The V-HeFT VA Cooperative Studies Group. Circulation 1993;87(6 Suppl):VI5–16. [PubMed]
- 16.Gradman A, Deedwania P, Cody R, Massie B, Packer M, Pitt B, Goldstein S. Predictors of total mortality and sudden death in mild to moderate heart failure. Captopril-Digoxin Study Group. J Am Coll Cardiol 1989;14:564–72. [DOI] [PubMed]
- 17.Andersson B, Waagstein F. Spectrum and outcome of congestive heart failure in a hospitalized population. Am Heart J 1993;126(3 Pt 1):632–40. [DOI] [PubMed]
- 18.Anand IS, Latini R, Florea VG, Kuskowski MA, Rector T, Masson S, et al. C-reactive protein in heart failure: prognostic value and the effect of valsartan. Circulation 2005;112:1428–34. [DOI] [PubMed]
- 19.de Groote P, Dagorn J, Soudan B, Lamblin N, McFadden E, Bauters C. B-type natriuretic peptide and peak exercise oxygen consumption provide independent information for risk stratification in patients with stable congestive heart failure. J Am Coll Cardiol 2004;43:1584–9. [DOI] [PubMed]


