A 36-year-old immigrant from El Salvador, who had had a heart murmur since childhood, presented after recent-onset dyspnea on exertion and several episodes of “turning blue.” A physical examination revealed a resting oxygen saturation of 98% on room air, blood pressure of 114/70 mmHg, and a regular heart rate of 76 beats/min. There was a normal S1, an absent P2, and a grade 4/6 systolic ejection murmur with a palpable thrill along the left mid-sternal border. There was no evidence of peripheral or central cyanosis, but clubbing was present. The patient's hemoglobin concentration was 20 g/dL (hematocrit, 58%). An electrocardiogram showed sinus rhythm, right-axis deviation, right atrial enlargement, and the Katz-Wachtel phenomenon (a large, equiphasic voltage in midprecordial leads), indicating biventricular hypertrophy (Fig. 1).
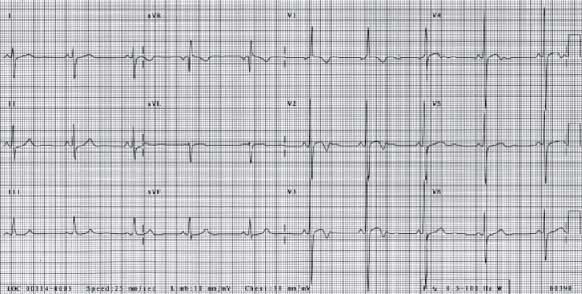
Fig. 1 An electrocardiogram illustrates the Katz-Wachtel phenomenon (a large, equiphasic QRS voltage in midprecordial leads), indicating biventricular hypertrophy.
Transthoracic echocardiography was consistent with a diagnosis of tetralogy of Fallot: there was an overriding aorta, right ventricular hypertrophy, pulmonic stenosis (peak gradient of at least 72 mmHg), and a perimembranous ventricular septal defect (Fig. 2) with a minimal bidirectional shunt on color-flow Doppler. Cardiac catheterization revealed a 90-mmHg gradient in the infundibulum below the pulmonic valve. Aortography showed a right-sided aortic arch and the anomalous origin of the right pulmonary artery from the ascending aorta (right hemitruncus; Fig. 3). The left pulmonary artery was the sole branch of the main pulmonary trunk (Fig. 4).
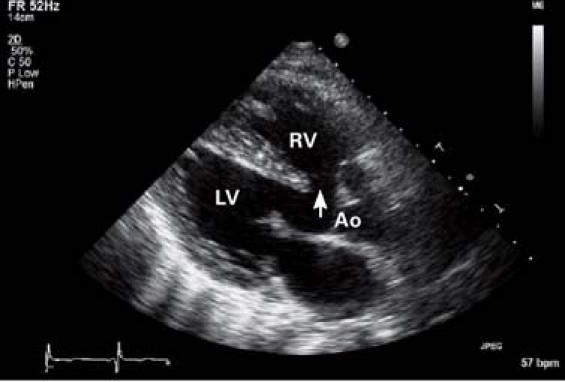
Fig. 2 Transthoracic echocardiography shows tetralogy of Fallot: a perimembranous ventricular septal defect (arrow), an overriding aorta (Ao), and right ventricular (RV) hypertrophy.
LV = left ventricle
Real-time motion image is available at texasheart.org/journal.
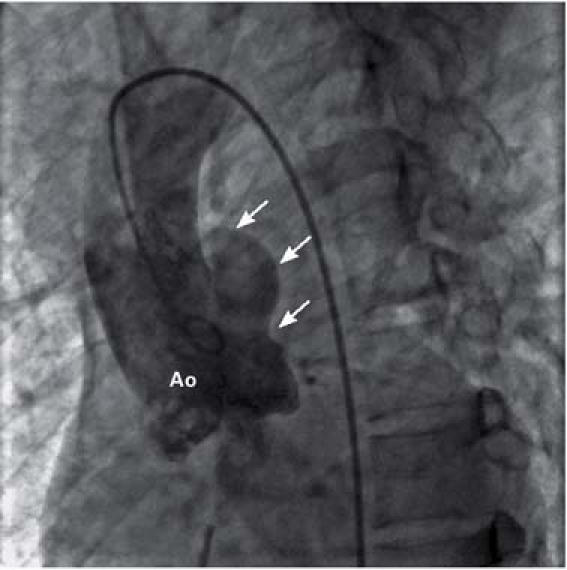
Fig. 3 Iodine contrast injection into the aortic root (Ao) reveals the anomalous origin of the right pulmonary artery (arrows) from the proximal ascending aorta.
Real-time motion image is available at texasheart.org/journal.
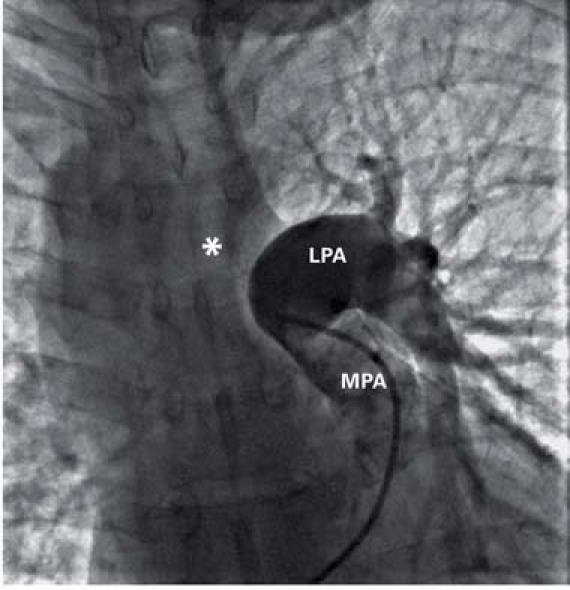
Fig. 4 Iodine contrast injection into the main pulmonary artery (MPA) shows only the left pulmonary artery (LPA) with its branches. The right pulmonary artery (asterisk) is not opacified.
Real-time motion image is available at texasheart.org/journal.
The patient underwent repair of the ventricular septal defect and resection of the infundibular obstruction; the right hemitruncus was left in place. Six months later, he was acyanotic, with normal right ventricular pressures and markedly improved overall functional capacity.
Comment
The anomalous origin of 1 pulmonary artery from the aorta is known as hemitruncus. A combination of hemitruncus and tetralogy of Fallot is a congenital syndrome rarely seen in adults, because most patients do not survive infancy without surgical treatment.1 The incidence of hemitruncus is estimated at 0.1% of all congenital cardiac anomalies. Left hemitruncus is seen much more often with tetralogy of Fallot than is right hemitruncus (75% vs 3% of cases).2 To the best of our knowledge, our patient is the oldest living person to have been diagnosed with unrepaired tetralogy of Fallot and right hemitruncus.
Supplementary Material
Footnotes
Address for reprints: Muhamed Saric, MD, PhD, Department of Medicine, New Jersey Medical School, 185 South Orange Avenue I-538, University Heights, Newark, NJ 07103. E-mail: saricmu@umdnj.edu
References
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


