Have you ever wondered what types of conditions can cause cognitive and perceptual disturbances in a patient without a psychiatric history? Have you been uncertain about what type of evaluation should be initiated? If you have, then the following case vignette (of a young man with cognitive and perceptual disturbances) should serve to provide the forum for answers to these and other questions related to strategies for the workup and treatment of such a patient.
CASE PRESENTATION: PART 1
Mr. A, a 23-year-old college graduate (with a major in computer science) came to the emergency department (ED) and requested treatment for self-diagnosed schizophrenia. He had never seen a psychiatrist before, and he had no known medical or psychiatric conditions. However, his family history was notable for bipolar disorder and schizophrenia. Although he had been an athlete and an academic star during most of high school, his grades began to slip around the time he started college, and he also became increasingly withdrawn. He spent most of his time by himself or with roommates (e.g., playing video games). Mr. A's hygiene declined; although he still showered daily, he wore the same clothes for days at a time, and he brushed his teeth only once a week. He was interested in girls, but never dated. By the time he graduated from college (mostly with grades of Bs and Cs), he had made no plans for securing a job. He stayed in his fraternity house and eventually worked as a systems administrator on campus. He started experimenting with recreational drugs for the first time in his life and quickly moved from marijuana to a vast array of hallucinogens and designer drugs. Around this time, Mr. A developed visual illusions and “confused smells” (e.g., he thought his food smelled like cat litter). He felt anxious and apathetic and worried that people were talking about him and laughing at him behind his back. At times, he “spaced out” and “lost time,” which he attributed to his drug use. After 9 months of heavy drug use, he stopped using illicit substances. However, his symptoms persisted; this prompted him to come to the ED.
How Should One Approach the Workup of a Patient With Social and/or Academic Decline?
The most important first step in the evaluation is to take a thorough medical and psychiatric history. Close attention should be paid to family history, prenatal and developmental history, and social history, as these variables may provide important clues to the presence of heritable mental illness (e.g., bipolar disorder, alcohol dependence, or schizophrenia), to prodromal symptoms predating the presenting complaints, and to unfavorable sociocultural or psychodynamic factors. It is also important to determine the rate of decline, as well as the presence or absence of associated symptoms that could help to narrow the differential diagnosis.1
Next, a thorough physical examination and neurologic testing (including tests of vision and hearing) should be carried out; other laboratory tests (e.g., for potential auto-immune, metabolic, or infection etiologies), neuroimaging, and a workup for partial complex seizures should be considered if clinically warranted. Fatigue (e.g., a variety of chronic or subacute medical illnesses, such as mononucleosis or early autoimmune disease) can also cause academic problems; it, too, should be considered in the differential diagnosis.2,3
When medical or neurologic conditions have been ruled out, psychiatric etiologies (e.g., depression, psychosis, learning disability, attention-deficit disorder, anxiety, substance abuse, tic disorder, conduct disorder, attachment problems, and child abuse) should be considered.4 Although a careful psychiatric interview may establish a tentative diagnosis, neuropsychological testing may be necessary to assess cognitive and emotional function as well as to detect subtle signs of a thought disorder or an emerging psychosis.
How Should One Approach the Evaluation and Management of Disordered or Tangential Thought?
Evaluation of disordered or tangential thinking, a delirium, or a dementing process should be broad-based, as the diagnosis may reflect a disorder of affect, behavior, or cognition. Reversible and life-threatening causes must be addressed first. The initial workup should include a physical examination, an electrocardiogram, a complete blood count, a comprehensive metabolic panel, and a toxicology screen, as well as measurement of levels of B12, ammonia, and thyroid-stimulating hormone, a microbiological assay of spirochetes, a radiological examination for intracranial lesions via computerized tomography or magnetic resonance imaging (MRI), a chest x-ray, and a urinalysis. Further diagnostic tests (e.g., electroencephalography), neuropsychological testing, and close outpatient follow-up (to observe the course of the symptoms) may also be necessary.5
The differential diagnosis of life-threatening causes of mental status changes can be recalled by use of the mnemonic “rule out the WHIMPS,” with each letter of “WHIMPS” standing for 1 or more conditions: Wernicke's encephalopathy and withdrawal; hypoglycemia, hypoxia, hypoperfusion of the central nervous system, and hypertensive encephalopathy; infections and intracranial processes; metabolic derangements (such as hyponatremia/ hypernatremia, hypocalcemia/hypercalcemia, hyperammonemia, uremia, hypercortisolemia, and B12 and thiamine deficiency); poisons (e.g., anticholinergic excess); and seizures.6
Management of tangentiality and disorganization should include treatment of the underlying cause, as well as any related symptoms (such as psychomotor agitation or autonomic hyperarousal).7
How Should Perceptual Disturbances (with or without concomitant drug use) Be Evaluated?
Perceptual disturbances (e.g., illusions and hallucinations) may reflect impairment of the entire sensory pathway mediating the modality in question. Therefore, a thorough examination of the sensory organ should be considered. If the perceptual disturbance is in the visual system, for instance, the evaluation may include a complete ophthalmologic examination with a slit lamp and an MRI of the brain to assess the entire optic nerve, the brain stem, the thalamus, and the cortical visual areas. Presenting signs or symptoms should guide further testing.
Even if there is low suspicion for prescription medications as causes of perceptual disturbance, assessment of the serum levels of the patient's medications and their active metabolites can impart useful knowledge regarding the workup.
What Are Some Specific Disorders Associated With Perceptual Disturbances?
Perceptual disturbances were predominantly visual in the case of Mr. A. The differential diagnosis of visual disturbances includes ophthalmic conditions (e.g., enucleation, cataract formation, retinal disease, choroidal disorder, macular abnormalities, and glaucoma), neurologic conditions (e.g., optic nerve disorders, brain stem lesions [peduncular hallucinosis], hemispheric lesions, epilepsy, migraine, and narcolepsy), toxic-metabolic conditions (toxic-metabolic encephalopathy, drug and alcohol withdrawal syndromes, and use of hallucinogenic agents), psychiatric states (e.g., schizophrenia, affective disorders, and conversion reactions), and miscellaneous causes (e.g., dreams, hypnagogic hallucinations, imaginary companions of childhood, eidetic images, sensory deprivation, sleep deprivation, hypnosis, and intense emotional experiences).8
What Is Involved in Neuropsychological Testing?
Neuropsychological testing consists of a flexible battery of standardized tests of written, verbal, and psychomotor performance tailored to each patient and most often administered by a psychologist. The battery usually includes an IQ test (e.g., Wechsler Adult Intelligence Scale-III9) in addition to a number of other tests selected to target the patient's symptoms. Commonly tested areas of neurocognitive functioning are attention and memory (e.g., Trail Making Test Parts A and B), language ability (such as word recognition, reading comprehension, and object naming), immediate and delayed recall (e.g., Wechsler Memory Scale-III), visuospatial skills (e.g., Rey-Osterreith Complex Figure Test), and executive functioning (e.g., Wisconsin Card Sorting Test and Stroop Color Word Test).10 Psychological tests are also sometimes included in the battery. For example, the Minnesota Multiphasic Personality Inventory-II can help detect malingering, the Personality Assessment Inventory can alert the clinician to a personality disorder, and the Rorschach Inkblot Test can reveal evidence of psychosis or other disordered thinking.10
CASE PRESENTATION: PART 2
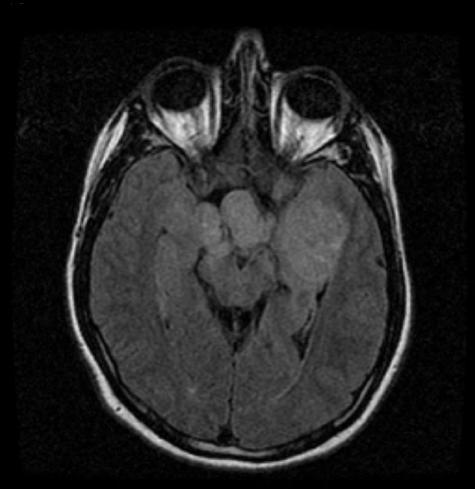
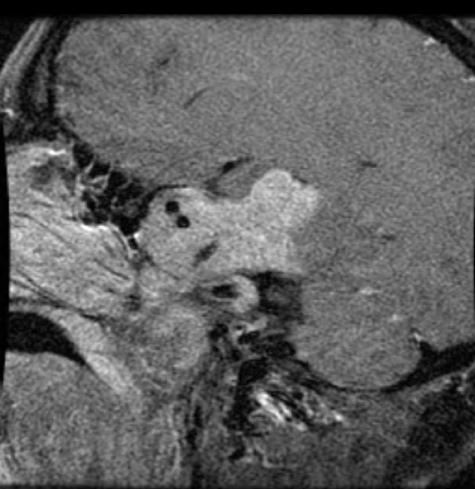
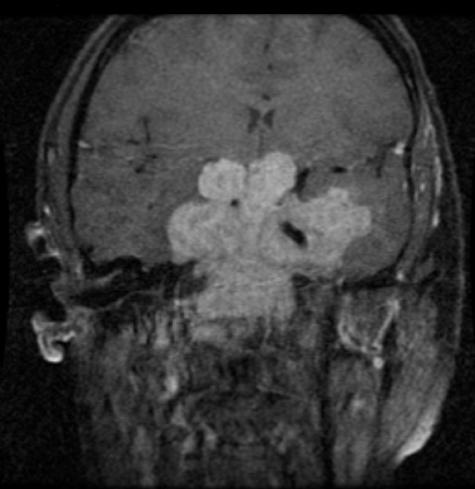
Mr. A's screening laboratory testing was unremarkable; moreover, serum toxicology was negative, and urine toxicology was positive only for cannabinoids. Given the patient's visual and olfactory disturbances, neuroimaging was also obtained in the ED. Testing revealed an 8-cm × 7.5-cm × 8-cm mass centered in the sella turcica and clivus with extension into the suprasellar cistern, the bilateral cavernous sinuses, the sphenoid sinuses, the occipital condyles, and the middle cranial fossa and through the foramen rotundum and superior orbital fissures. It encased both internal carotid arteries and produced a mass effect on the adjacent temporal lobes, the inferior frontal lobe, the brain stem, and the optic chiasm (see Figures 1–3). A neuroendocrine workup revealed an isolated prolactin elevation of 16,348 ng/mL (reference range, 0–15 ng/mL), confirming a diagnosis of pituitary macroadenoma (macroprolactinoma). Mr. A appeared unconcerned about his tumor; he maintained a stable, though constricted, affect throughout the workup. He was admitted to the Neurosurgery Service, with consultations from Neurology, Neuroendocrinology, and Psychiatry.
Figure 1.
MRI (axial view) of the 8-cm × 7.5-cm × 8-cm Mass in the Sella Turcica and Clivus With Extension Into the Suprasellar Cistern, the Bilateral Cavernous Sinuses, the Sphenoid Sinuses, the Occipital Condyles, and the Middle Cranial Fossa
Figure 3.
Pretreatment Magnetic Resonance Imaging (sagittal view) Revealing a Large Tumor
What Are the Common Manifestations of Prolactin-Secreting Tumors?
Not surprisingly, one of the most common consequences of prolactin-secreting tumors is hyperprolactinemia. This is most conspicuous in premenopausal women, who often develop amenorrhea, galactorrhea, and infertility. Although hyperprolactinemia is often detected after discontinuation of the use of an oral contraceptive, there is no apparent relationship between the use of oral contraceptives and the formation of prolactinomas. Because hyperprolactinemia-associated hormonal symptoms are more pronounced in women, prolactinomas are usually diagnosed at an earlier stage in women than in men. Thus, they are more likely to be small at the time of diagnosis, and headache and neurologic deficits are often absent.
In contrast, prolactinomas in men typically tend to be large at the time of diagnosis; they may cause cranial nerve dysfunction, visual loss, and hypopituitarism. In men, hyperprolactinemia leads to impotence, infertility, gynecomastia, and decreased libido, but these are rarely the initial symptoms. Galactorrhea may also be present, but less frequently than in women. In both sexes, longstanding hyperprolactinemia also leads to osteoporosis, especially in the spine.11
Were Mr. A's Symptoms Fully Explained by the Presence of His Tumor?
Based on its size, Mr. A's tumor had been growing for years; its presence and location likely account for his sensory disturbances. His optic chiasm had been displaced by the tumor, leading to his visual deficits; his olfactory nerves were also likely affected due to their anatomic location, leading to his description of “confused smells.” These olfactory illusions, as well as his episodes of “spacing out” and “losing time,” could also have been manifestations of partial complex seizures caused by the tumor's mass effect and by impingement on the temporal lobes.
Mr. A's constricted affect and subjective apathy may have been linked to a disturbance of the hypothalamic-pituitary tract by his tumor; this type of disruption in patients with pituitary tumors has been proposed as a cause of an “apathy syndrome” that is usually refractory to antidepressant treatment but responds well to stimulants.12
Although hyperprolactinemia has been associated with major depression in several studies,13 it is hard to account for Mr. A's social dysfunction and declining academic performance in high school, since these symptoms started 5 years earlier, when the tumor was likely small or nonexistent. Recreational drug use cannot account for these symptoms, either, since Mr. A did not start using drugs until close to the time of his graduation from college. Thus, an underlying affective or cognitive disorder cannot be ruled out, especially given Mr. A's family history of schizophrenia and a mood disorder. He will be monitored for the potential emergence of a primary psychiatric disorder, such as depression or schizophrenia, during and after treatment of his tumor. Since treatment of his prolactinoma involves the use of dopaminergic agents, he is at an increased risk for development of a psychotic state. If he were to develop psychotic symptoms, he would not be a good candidate for dopamine-blocking antipsychotic agents that would interfere with his neuroendocrine treatment. Were he to require antipsychotics, clozapine might be the best choice (because of its weak effect on the lactotrophs in the pituitary).14
What Treatments Should Mr. A Consider at This Point, and What Is His Prognosis?
Although over 90% of untreated microadenomas (measuring < 1 cm) do not enlarge over 4 to 6 years,15 treatment is usually initiated for masses that are large enough at the time of discovery to extend outside the sella and/or to cause symptoms. Medical treatment of prolactinomas involves use of a dopamine agonist (such as bromocriptine, cabergoline, or pergolide). Although bromocriptine causes tumor shrinkage in 80% of macroprolactinomas, the other dopamine agonists appear to have comparable efficacy, with cabergoline favored for its less severe side effect profile and twice-weekly dosing schedule.16,17 For this class of medications, common side effects include nausea, orthostatic hypotension, and unmasking or exacerbation of depression or psychosis (which is rare).
In cases of nonresponse or only partial response to medication, surgery is the next treatment of choice. A transsphenoidal approach is used more frequently, as it is associated with lower morbidity and mortality than with a transcranial approach. In patients with macroprolactinomas (> 1 cm), long-term normalization of prolactin occurs in about 25% of surgical cases, with the cure rate decreasing as tumor size increases.17 Radiation treatment or radiosurgery is even less effective, as a recent review found that only 1 in 4 cases yielded normalization of prolactin levels in adenomas of all sizes at a corrected median follow-up time of 29 months.18
Other treatments include monitoring for, and treatment of, medication side effects and, in the case of large macroadenomas, addressing the results of mass effect (e.g., seizures, hydrocephalus, and visual field deficits).
Microadenomas have a better prognosis than macroadenomas, with up to 95% of cases remaining stable with medical suppressive treatment for more than 4 to 6 years. Although rates vary widely, macroadenomas are more likely to continue to grow and to eventually require surgical intervention.
Figure 2.
Pretreatment Magnetic Resonance Imaging (coronal view) Revealing a Large Tumora
Footnotes
Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital (MGH) sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. Such consultations require the integration of medical and psychiatric knowledge. During their thrice-weekly rounds, Dr. Stern and other members of the Psychiatric Consultation Service discuss the diagnosis and management of conditions confronted. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Drs. Zahajszky and Quinn are residents in the Departments of Psychiatry at MGH and McLean Hospitals. Dr. Smith is an attending physician on the Psychiatric Consultation Service at MGH. Dr. Stern is Chief of the Psychiatric Consultation Service at MGH and a Professor of Psychiatry at Harvard Medical School.
REFERENCES CITED
- Querques J, Stern TA. Approach to consultation psychiatry: assessment strategies. In: Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 5th ed. Philadelphia, Pa: Mosby. 2004 9–19. [Google Scholar]
- Sadock CJ, Sadock VA. eds. Kaplan and Sadock's Synopsis of Psychiatry. 9th ed. New York, NY: Lippincott Williams and Wilkins. 2003 229–274. [Google Scholar]
- Roffman JL, Stern TA. Diagnostic rating scales and laboratory tests. In: Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 5th ed. Philadelphia, Pa: Mosby. 2004 37–48. [Google Scholar]
- Parry TS.. Assessment of developmental learning and behavioural problems in children and young people. Med J Aust. 2005;183:43–48. doi: 10.5694/j.1326-5377.2005.tb06892.x. [DOI] [PubMed] [Google Scholar]
- Falk WE. The patient with memory problems or dementia. In: Stern TA, Herman JB, Slavin PL, eds. Massachusetts General Hospital Guide to Primary Care Psychiatry. 2nd ed. New York, NY: McGraw-Hill. 2004 197–212. [Google Scholar]
- Wise MG. Delirium. In: Hales RE, Yudofsky SC, eds. Textbook of Neuropsychiatry. Washington, DC: American Psychiatric Press. 1987 89–103. [Google Scholar]
- Freudenreich O, Stern TA.. Clinical experience with the management of schizophrenia in the general hospital. Psychosomatics. 2003;44:12–23. doi: 10.1176/appi.psy.44.1.12. [DOI] [PubMed] [Google Scholar]
- Cummings J, Miller BL.. Visual hallucinations: clinical occurrence and use in differential diagnosis. West J Med. 1987;146:46–51. [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Manual for the Wechsler Adult Intelligence Scale. 3rd ed. New York, NY: Psychological Corporation. 1997 [Google Scholar]
- Blais MA, O'Keefe SM, and Norman DK. Psychological and neuropsychological assessment. In: Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 5th ed. Philadelphia, Pa: Mosby. 2004 49–59. [Google Scholar]
- Schlechte JA.. Prolactinoma. N Engl J Med. 2003;349:2035–2041. doi: 10.1056/NEJMcp025334. [DOI] [PubMed] [Google Scholar]
- Weitzner MA, Kanfer S, Booth-Jones M.. Apathy and pituitary disease: it has nothing to do with depression. J Neuropsychiatry Clin Neurosci. 2005;17:159–166. doi: 10.1176/jnp.17.2.159. [DOI] [PubMed] [Google Scholar]
- Sonino N, Fava GA.. Psychological aspects of endocrine disease. Clin Endocrinol (Oxf) 1998;49:1–7. doi: 10.1046/j.1365-2265.1998.00528.x. [DOI] [PubMed] [Google Scholar]
- Melkersson K, Hulting AL.. Prolactin-secreting pituitary adenoma in neuroleptic treated patients with psychotic disorder. Eur Arch Psychiatry Clin Neurosci. 2000;250:6–10. doi: 10.1007/pl00007539. [DOI] [PubMed] [Google Scholar]
- Sisam DA, Sheehan JP, Sheeler LR.. The natural history of untreated microprolactinomas. Fertil Steril. 1987;48:67–71. doi: 10.1016/s0015-0282(16)59292-9. [DOI] [PubMed] [Google Scholar]
- Levy A. Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry. 2004 75suppl 3. 47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molitch ME.. Medical management of prolactin-secreting pituitary adenomas. Pituitary. 2002;5:55–65. doi: 10.1023/a:1022375429083. [DOI] [PubMed] [Google Scholar]
- Brada M, Ajithkumar TV, Minniti G.. Radiosurgery for pituitary adenomas. Clin Endocrinol (Oxf) 2004;61:531–543. doi: 10.1111/j.1365-2265.2004.02138.x. [DOI] [PubMed] [Google Scholar]
ANNOTATED BIBLIOGRAPHY
- Brada M, Ajithkumar TV, and Minniti G. Radiosurgery for pituitary adenomas. Clin Endocrinol (Oxf). 2004 61:531–543.–The authors outline the technological advances that have improved delivery of radiation to intracranial tumors (with significant reduction in radiation dose to normal brain). There is little evidence to recommend certain methods of radiation delivery over others; fractionated conventional, stereotactic, gamma knife, and single fraction radiation options are discussed. [DOI] [PubMed] [Google Scholar]
- Cummings J, Miller BL. Visual hallucinations: clinical occurrence and use in differential diagnosis. West J Med. 1987 146:46–51.–The authors discuss the diverse clinical circumstances (including ophthalmologic diseases, neurologic disorders, toxic/metabolic disorders, and psychiatric illness) in which visual hallucinations arise. The content, duration, and timing of the symptoms relate to their cause and provide useful diagnostic information. Hallucinations must be distinguished from delusions and from confabulation for diagnostic accuracy. [PMC free article] [PubMed] [Google Scholar]
- Levy A. Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry. 2004 75suppl 3. 47–52.–In this brief yet comprehensive overview, the presentation, classification, and general investigation of pituitary lesions are followed by a discussion of the diagnosis and management of specific secretory subtypes. Important general diagnostic maneuvers include use of magnetic resonance imaging, visual field examination, and assessment of hormone levels. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melkersson K, Hulting AL. Prolactin-secreting pituitary adenoma in neuroleptic treated patients with psychotic disorder. Eur Arch Psychiatry Clin Neurosci. 2000 250:6–10.–Three patients with psychoses and concomitant prolactin-secreting pituitary tumors are described. These case reports support the view that neuroleptics (being dopamine antagonists) and dopamine agonist agents, used as a primary treatment for prolactinomas, can cancel out the other's effects. The combination of clozapine and quinagolide is recommended as the treatment of choice for patients with psychosis and a prolactin-secreting tumor. [DOI] [PubMed] [Google Scholar]
- Molitch ME. Medical management of prolactin-secreting pituitary adenomas. Pituitary. 2002 5:55–65.–Medical therapy is the initial treatment of choice for patients with prolactinomas. When infertility is the primary indication for treatment, bromocriptine use has an extensive safety experience and is preferred. However, for other indications, cabergoline appears to be more efficacious and better tolerated. Transsphenoidal surgery remains an option, especially for patients with microadenomas, when medical therapy is ineffective. [DOI] [PubMed] [Google Scholar]
- Parry TS. Assessment of developmental learning and behavioural problems in children and young people. Med J Aust. 2005 183:43–48.–This article outlines the clinical approach to the assessment of pediatric patients with behavioral problems for developmental and learning disorders. Observation, careful history, and assessment of cognitive function provide most of the diagnostic information. A multidisciplinary team approach is recommended. [DOI] [PubMed] [Google Scholar]
- Schlechte JA. Prolactinoma. N Engl J Med. 2003 349:2035–2041.–A comprehensive review article on the clinical etiologies, diagnosis, and treatment of prolactinomas. Using a case report of a 22-year-old woman with amenorrhea, galactorrhea, and an elevated prolactin level as an example, the article explains the rationale behind the clinical workup and describes the various options for the management of microadenomas and macroadenomas. [DOI] [PubMed] [Google Scholar]
- Sisam DA, Sheehan JP, and Sheeler LR. The natural history of untreated microprolactinomas. Fertil Steril. 1987 48:67–71.–To characterize the rate and prevalence of microprolactinoma growth, the authors performed serial computerized tomography scans (an average of about 32 months apart) in 38 untreated patients with microprolactinomas. In no patient was there any evidence of tumor growth. The authors conclude that the majority of patients with microprolactinomas have a benign course, with tumor growth occurring, if at all, over a period of years. [DOI] [PubMed] [Google Scholar]
- Sonino N, Fava GA. Psychological aspects of endocrine disease. Clin Endocrinol (Oxf). 1998 49:1–7.–This article highlights some ways that the psychosocial aspects of endocrine illness may have important clinical and research implications. Areas discussed include the role of life stress in the pathogenesis of some endocrine conditions, the association of psychosocial variables with affective disorders, and the presence of residual symptoms after treatment. Evidence points to the need for an updated psychosocial awareness of endocrine disease. [DOI] [PubMed] [Google Scholar]
- Weitzner MA, Kanfer S, and Booth-Jones M. Apathy and pituitary disease: it has nothing to do with depression. J Neuropsychiatry Clin Neurosci. 2005 17:159–166.–The authors present a series of cases in which patients with pituitary disease were diagnosed and treated for depression with little response to conventional antidepressants. They note that there is a growing understanding that patients with pituitary disease may experience depressed mood and emotional withdrawal as a result of the long-term effects of the pituitary tumor itself, its treatment, and/or the hormonal changes that occur on the hypothalamic-pituitary-end–organ axis. When the diagnosis of apathy syndrome was considered and treatment implemented, the patients' condition improved. A review of the literature on apathy, hypothalamic-pituitary-end–organ axis dysfunction, and treatment for apathy syndrome is included. [DOI] [PubMed] [Google Scholar]