Abstract
Objective: To characterize the extent and impact of bipolar I and II disorders and rapid cycling in a managed care population using both coded diagnostic claims and clinical screening.
Method: The Mood Disorder Questionnaire (MDQ) was used to identify bipolar disorder among patients attending the psychiatry service of a large Midwestern health system. Suicidal ideation screening questions were also asked, along with a brief set of relevant history and medication questions. Patients scoring positive on the MDQ or identified as bipolar-positive according to DSM-IV criteria by the screening clinician were administered the Work and Social Adjustment Scale and an Employment questionnaire. Descriptive statistics were used to summarize results. The study was conducted from July 2004 to November 2004.
Results: Seventy (6.4%) of 1087 patients had bipolar disorder, 59 of whom completed the entire study. For these patients, the mean time with bipolar disorder was 9.3 (SD 10.2) years. The mean length of the current episode was 10.4 (SD 14.4) weeks, with 22% of patients experiencing a mixed episode, 5% manic-predominant, 12% hypomanic-predominant, and 46% a depressive-predominant episode. Twenty-four percent of patients with bipolar disorder were rapid cycling at the time of their visit; for 5 of these patients, rapid cycling was thought to be related to antidepressant use. Sixty-one percent of patients with bipolar disorder were taking an antidepressant; 69.5% were taking a mood stabilizer. Of these patients with bipolar disorder, 19% were evaluated as high suicidality risk, while 47% were considered moderate risk. Bipolar disorder patients reported problems with employment/employability and social adjustment. About one quarter of these patients ranked problems with family and relationships as marked or severe. Fifty percent of these bipolar disorder patients reported missing at least 1 week of work during the past month; 41% reported fearing the loss of their current job due to their emotional state; and 20% reported being fired/laid off during the past 5 years due to their emotional state.
Conclusions: This research documents some of the clinical features and social and labor-force impact of bipolar disorder in a managed care population and adds several dimensions to data published to date. Fully two thirds of our study subjects with bipolar disorder were found to be at substantial risk of suicide, and bipolar disorder patients in this study reported substantial problems with employment/employability and social functioning.
Bipolar disorder is one of the world's 10 most disabling conditions, and it affects people across nationality, race, and socioeconomic status.1 While traditionally defined bipolar disorder (bipolar I) has a prevalence of approximately 1% across all populations, the prevalence of bipolar II disorder, involving episodes of less severe hypomania and major depression, along with bipolar spectrum subtypes, brings the estimated prevalence of all bipolar disorders to over 3% of people in the United States.1
A 2005 primary care practice–based study2 reported that the prevalence of positive screening results for lifetime bipolar disorder was 9.8%, and it did not differ significantly by age, sex, or race/ethnicity. Of those who screened positive for bipolar disorder, 72.3% sought professional help for their symptoms, but only 8.4% reported receiving a diagnosis of bipolar disorder. Similarly, among those who screened positive for bipolar disorder, 68.2% had a current major depressive episode or an anxiety or substance use disorder, and only 6.5% reported taking a mood-stabilizing agent in the past month. In that study, primary care physicians recorded evidence of current depression in 49.0% of those screening positive for bipolar disorder, but did not record a bipolar disorder diagnosis in either administrative billing or the medical record of any of these patients. Health-related quality of life was worse among those with bipolar disorder compared with those who screened negative, as was social and family impact.2
A recent clinic-based study3 of patients taking an anti-depressant for depression found that 21.3% screened positive for bipolar disorder symptoms on the Mood Disorder Questionnaire (MDQ). Those screening positive for bipolar disorder symptoms were younger, more likely to be white, more likely to be living alone, much less likely to be married, and less likely to be employed than those who screened negative. Almost two thirds of patients screening positive for bipolar disorder had never received that diagnosis. These findings indicate that bipolar disorder is underdiagnosed and undertreated in primary care, and they suggest some of the serious problems and impairments faced by patients with bipolar disorder.3
In addition to the substantial burden of the symptoms of bipolar disorder itself, a wide range of associated medical problems have been reported in the few studies focused on medical illness in this population, the most common being cardiovascular disease, diabetes mellitus, obesity, and thyroid disease.1 The coexistence of key medical risk factors related to excessive nicotine use, use of alcohol and other drugs, and co-occurring anxiety disorders and eating disorders may lead to the early onset of medical diseases with poor long-term outcomes.1
Economic costs of bipolar disorder are also high: a 2001 study4 estimated the present value of the lifetime cost of persons with onset of bipolar disorder (in 1998) to be 24 billion U.S. dollars. In that study, average cost per case ranged from $11,720 for those with a single manic episode to $624,785 for those with nonresponsive/chronic episodes.4
The present study focused on systematically screening attendees of a psychiatry clinic for bipolar disorder and documenting the clinical features and impact that bipolar disorder has on their social and labor-force participation.
METHOD
Study Site
We conducted this study in a large, vertically integrated health system serving the primary and specialty health care needs of Midwestern residents. This system is affiliated with a multispecialty salaried physician group that provides most of the care for health system patients. The health system owns a large, nonprofit, mixed-model health maintenance organization (HMO). In order to optimize the data available for this study, the population was limited to HMO members. The institutional review board reviewed and approved this research. The study was conducted from July 2004 to November 2004.
Assessment Tools
The MDQ5 was utilized as an initial screening tool to identify bipolar disorder among each patient attending the health system psychiatry service. Our target was to screen 1000 consecutive clinic attendees. An MDQ screening score of 7 or more is reported to yield good sensitivity (0.73) and very good specificity (0.90) in the diagnosis of bipolar disorder.5 The MDQ was immediately scored by a mental health professional, and, regardless of score, patients were immediately evaluated for bipolar disorder using the DSM-IV bipolar disorder criteria. Those meeting the criteria were further evaluated for their rapid-cycling status in addition to any other relevant clinical/mental health disorders. In addition to the MDQ, suicidal ideation screening questions (developed and implemented by the health system with a working group using data culled from key literature sources6,7; please contact author C.F. for further information) were asked by the psychiatric clinician, and a brief set of relevant history and medication questions were completed. Patients scoring positive on the MDQ or found to be bipolar-positive by the clinician were solicited to provide informed consent. For those who consented, the Work and Social Adjustment Scale,8 a 9-point Likert scale from 0 (not at all affected) to 8 (very severely affected), and Employment questionnaire (13 questions about employment history, nature of employment, and impact of depressive and/or manic symptoms on employment history; a copy is available on request from author P.S.) were administered.
Data Analysis
Statistical analyses were performed using SAS statistical software (SAS Institute Inc; Cary, N.C.). Descriptive statistics were used to summarize the results of the MDQ screening, the clinician diagnosis, and the findings on the questionnaires.
RESULTS
Screening
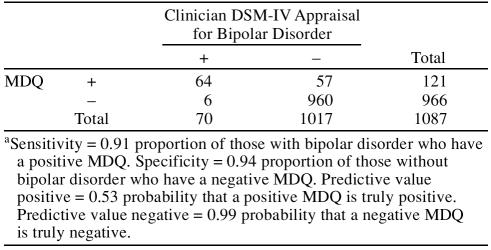
There were 1087 MDQs completed by patients attending the psychiatry service. Of these, 121 patients had MDQ-positive results, 64 of whom were found to be bipolar positive by clinician assessment (Table 1). There were 966 patients with MDQ-negative results, of whom 6 were found by the clinician to be bipolar positive. The MDQ did well at identifying those without bipolar disorder (negative predictive value 0.99); however, the MDQ had a relatively high proportion of false-positives, which reduced its positive predictive value to 0.53. Overall, the MDQ identified 91% of those with bipolar disorder (sensitivity) and 94% of those without (specificity).
Table 1.
Number of Patients Meeting Bipolar Disorder Criteria According to the Mood Disorder Questionnaire (MDQ) Versus Clinical DSM-IV Assessmenta
Therefore, 70 (6.4%) of 1087 patients attending the psychiatry service were found to have bipolar disorder, 59 of whom provided informed consent and completed the entire questionnaire load. The remainder of the results will focus on these 59 patients.
Patient characteristics
Among those patients who were confirmed by the psychiatrist as having bipolar disorder, the mean time with bipolar disorder was 9.3 years (SD 10.2 years). The mean length of their current episode was 10.4 weeks (SD 14.4 weeks), with 22% experiencing a mixed episode, 5% a manic predominant episode, 12% a hypomanic predominant episode, and 46% a depressive predominant episode. Almost 1 in 4 (24%) were thought to be rapid cycling at the time of their visit.
Treatments received
Of the 59 patients with bipolar disorder who completed all of the surveys, 61% were found to be taking an antidepressant; almost half of whom (42%) were taking selective serotonin reuptake inhibitors (SSRIs). Among these 59 patients, 69.5% were taking a mood stabilizer.
The psychiatry clinician felt that in 5 (36%) of the 14 rapid-cycling patients their rapid cycling was related to antidepressant use. Antidepressant monotherapy was more common among non-rapid cyclers (22.7% vs. 7.4%) as was mood stabilizer monotherapy (27.3% vs. 21%). Co-therapy with both a mood stabilizer and an anti-depressant was similar in both non–rapid-cycling patients and their rapid-cycling counterparts (41% vs. 43%).
Suicidality Risk
When the bipolar disorder patients who completed all the study surveys were assessed using the health system suicidality risk guideline, 19% of the respondents were evaluated as high risk, while 47% were considered moderate risk.
Work and Social Adjustment Scale
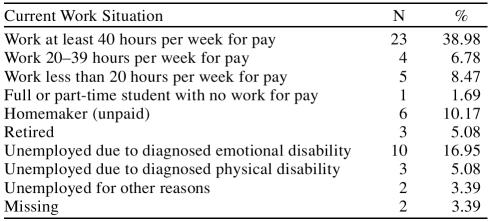
Almost 40% of the subjects worked at least 40 hours per week for pay (Table 2), while 17% reported being unemployed due to their emotional disability. A substantial proportion of bipolar disorder patients reported problems with work and social adjustment. While 42% reported that their work is at least markedly affected by their symptoms, over 50% reported experiencing difficulties with home management. Social activities were at least markedly affected in 37% of subjects, and 58% reported definite problems with private activities. Notably, about one quarter of these patients ranked problems with family and relationships as marked or severe.
Table 2.
Employment Status Among Surveyed Bipolar Disorder Patients
When these respondents were asked, “How often did depressive symptoms affect activities/work?” 12% of these patients said all of the time, 35% said most of the time, and 29% said some of the time. Manic symptoms seemed to be less impactful, as only 14% of patients felt that their manic symptoms affected their activities/work all or most of the time and 35% said some of the time.
Fifty percent of these bipolar disorder patients reported missing at least 1 week of work (paid work/nonpaid work activities) during the past month. Even though 42% of respondents reported missing no days from work/school in the past 30 days due to depressive symptoms, approximately 1 in 5 (21%) reported having missed 10 days or more. Similarly, over half (57%) of respondents reported missing no days from work/school in the past 30 days due to manic symptoms, but 17% missed from 2 to 10 days. Overall, our work finds that subjects reported missing a mean of 7 days in the past month (absenteeism alone). When absenteeism was subdivided by depressive and manic symptoms, the cohort reported a mean of 6.6 days in the past month lost from work or school due to depressive symptoms versus 3.9 days for manic symptoms.
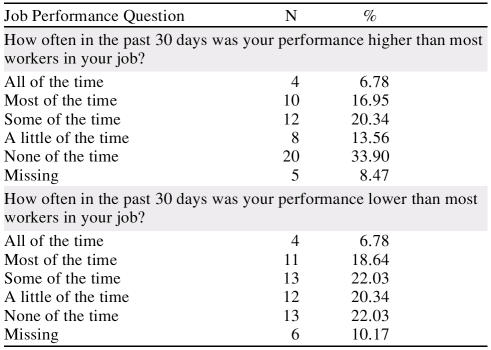
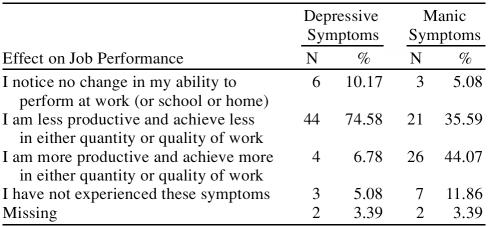
This absenteeism appears to have had other effects as well, since 41% of these patients reported fearing the loss of their current job due to their emotional state, while 20% of subjects report being fired/laid off during the past 5 years due to their emotional state. Interestingly, when asked about higher and lower performance on the job relative to other workers in their position (Table 3), 47% felt that their performance was sometimes to all of the time lower than that of their peers. Similarly, in the past 30 days, 22% of the cohort reported not working as carefully as they should all or most of the time, and 17% felt that the quality of their work in the past 30 days was lower than it should have been most or all of the time. Work performance seems to vary by depressive and manic symptoms, as 75% of patients reported being less productive and achieving less in quantity or quality of work when experiencing depressive symptoms (vs. 36% during manic symptoms), while 44% report being more productive while experiencing manic symptoms (vs. 7% during depressive symptoms; Table 4).
Table 3.
Self-Reported Job Performance of Bipolar Disorder Patients Relative to Other Workers in Their Position
Table 4.
Self-Reported Effect of Depressive and Manic Symptoms on Job Performance
DISCUSSION
Others have reported substantial underdetection of bipolar disorder in screened samples of primary care patients,1,2 which has brought to light the number of people who are misdiagnosed or overlooked. Our current work has sought to highlight more directly some of the key clinical (medication use, rapid cycling, suicidality) and social (labor force participation and social impact) features among those found to have bipolar disorder, which have not been adequately addressed in previous studies.
One issue that has been suggested in the literature is the risk of rapid cycling and suicidality among those taking antidepressants, particularly SSRIs. Almost 1 in 4 subjects in our study (24%) were thought to be rapid cycling at the time of their visit; the psychiatry clinician felt that in 5 (36%) of the 14 rapid-cycling patients their rapid cycling was related to antidepressant use (7 were taking anti-depressants). These findings are consistent with reports from the Stanley Foundation Bipolar German cohort, in which 40% of “rapid cyclers” suffered a recurrent rapid-cycling course during a 2.5-year follow-up period.9 A Veterans Affairs study cohort found that 14% of bipolar patients had experienced rapid cycling in the 12 months prior to intake (and 33% during the follow-up period),10 while Schneck and colleagues11 report a rapid-cycling rate of 20% in their cohort of 500 bipolar patients.
The move to more aggressive recognition and treatment of depression, coupled with the underdetection of bipolar disorder among those presenting with depression, is probably a major explanatory factor in the rise of antidepressant use among bipolar patients.12 Given that most patients with bipolar disorder present for treatment during the depressive phase rather than during manic or hypomanic phases, there is an increased likelihood of a unipolar depression diagnosis and treatment with antidepressants. The overuse of antidepressants has been associated with increased risk of antidepressant-induced mania, as 30% to 70% of patients with bipolar disorder are treated with antidepressants alone.13 However, Altshuler and colleagues14 found that bipolar patients who respond to anti-depressants and do not switch into an episode of mania in the first 6 weeks are not at risk for switching over the ensuing year.
There are trials supporting the efficacy of antidepressants in bipolar disorder, along with evidence that they may induce rapid cycling, switching, and mania.15 Anti-depressant-induced mania is often mixed, and since increased suicide risk is a particular feature of mixed states, this may explain why suicidal ideation can emerge with antidepressant treatment.15 The sentiment that antidepressants are “probably overused” and mood stabilizers “underused” has been expressed after critical review of the studies in the nosology of bipolar disorder and the effects of antidepressant agents.16 About 1 in 5 members of our cohort (22%) experienced a mixed bipolar episode at the time of the screening. Furthermore, 61% of the cohort was found to be taking an antidepressant, almost half of whom (42%) were taking SSRIs, while 69.5% were also on treatment with a mood stabilizer.
Patients with bipolar disorder have been reported to have a higher risk of suicide than patients with any other psychiatric or medical illness,17–19 with rates of suicidal ideation and attempts between 35% and 50%.17,20,21 The completed suicide rate has been reported to be approximately 20%.22 Shi and colleagues,23 in their study of recognized and unrecognized bipolar disorder in 25,460 California Medicaid (Medi-Cal) patients, found that unrecognized bipolar patients were nearly 4 times more likely to attempt suicide and 50% more likely to be hospitalized than nonbipolar patients. We found that 19% of bipolar patients in our study were considered to be at high risk of suicide and 47% at moderate risk, meaning that two thirds of our cohort was at substantial risk for suicide. Estimates of lifetime risk of suicide in patients with bipolar disorder range from 8% to 20% or 10 to 20 times that of the U.S. general population24–29 and may account for between 9% and 60% of all deaths among those with bipolar disorder.30 Decreased suicide attempts have been documented among users of mood stabilizers, especially lithium and valproex.30
Labor Force Participation
In the current study, 17% of bipolar subjects reported that they were unemployed due to their “emotional disability,” while another 8.5% were unemployed for other reasons. This is consistent with reports from other studies. Zwerling and colleagues,31 using the National Health Interview Survey Disability Supplement of 1994 to 1995, found that only 56% of persons with bipolar disorder participated in the workforce, and the likelihood of workforce participation among bipolar subjects was substantially lower than among those without these disorders (OR 0.60, 95% CI 0.48 to 0.75) in multivariate models controlling for major demographics, education, race, and marital status. This would also seem to support the findings of Abood et al.,32 which refuted the commonly held notion that bipolar disorder does not necessarily confer social disadvantage (and is overrepresented in higher socioeconomic strata). Kupfer and colleagues20 reported that 64% of those in the Stanley Center Bipolar Disorder Registry population of 2839 patients were unemployed, which is about 4 times the rate that we found. The difference is probably attributable to differences in the populations studied: the Stanley Registry recruits from those actively in treatment and those active in support groups, while our study population consists of those currently in treatment and insured for health care services, which likely reflects positive employment status.
Kessler and colleagues,33 citing findings from the National Comorbidity Survey, found that patients with bipolar I experienced a mean 8.1 impairment days in the past month (bipolar II 3.8 days), which accounts for both absenteeism and presenteeism at work and at home; our research finds that subjects reported missing a mean of 7 days in the past month (absenteeism alone). When absenteeism was subdivided by depressive and manic symptoms, the cohort on average reported 6.6 days in the past month lost due to depressive symptoms versus 3.9 days for manic symptoms.
Results from the National Depressive and Manic-Depressive Association surveys suggest that 88% of those with bipolar disorder felt that their illness affected their ability to perform on their job, with only 40% reporting that they were employed at the time of the survey.34 The current study provides additional data about the impact of depressive and manic symptom features separately, which adds a dimension to the data published to date.
The current study and its value must be viewed in the context of its potential limitations. First, the cohort was obtained from a series of patients with appointments in a psychiatry clinic that is part of a large managed care organization. This suggests that the subjects in this study may not be representative of the broad spectrum of all patients since they have access to health care through a managed care organization. Thus, it is possible that the impairment in this group is less than among those who may be unable to attain access to a managed care organization. Similarly, the coordination of care and the ease of referral from medical practitioners within a managed care setting probably increase likelihood of detection. Our protocol was explained to the staff and clinicians, and, as such, they were not blinded to the objectives of the study or the MDQ results of the patients, which may have biased our results and shown more favorable screening characteristics for the MDQ. Our validity calculations for the MDQ are higher than those reported by Hirschfeld5 in his original work; however, it is possible that the MDQ identifies lifetime experience versus a clinical diagnosis, which reflects current active disease. This may have led to a higher number of MDQ-positive but clinical diagnosis–negative patients in our study. Finally, a number of the patients in our study had been seen in this clinic before, which also increases the likelihood of detection and chronicity of disease. Although we had relatively high participation rates, we do not have comparator data.
This research documents some of the clinical features and social and labor-force impact of bipolar disorder in a managed care population and adds several dimensions to data published to date. More research is needed to continue the pursuit of better detection and treatment of bipolar disorder, which is extremely costly in individual, economic, and public-health terms.
Acknowledgments
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside U.S. Food and Drug Administration–approved labeling has been presented in this article.
Take-Home Points
♦ Increased screening for bipolar disorder with a diagnostic tool (like the Mood Disorder Questionnaire) is an important step in identifying those patients in need of intervention
♦ Two thirds of the patients with bipolar disorder were at substantial risk for suicide
♦ Among patients with bipolar disorder, 42% reported that their work was at least markedly affected by their symptoms, and social activities were at least markedly affected in 37%
Pretest and Objectives
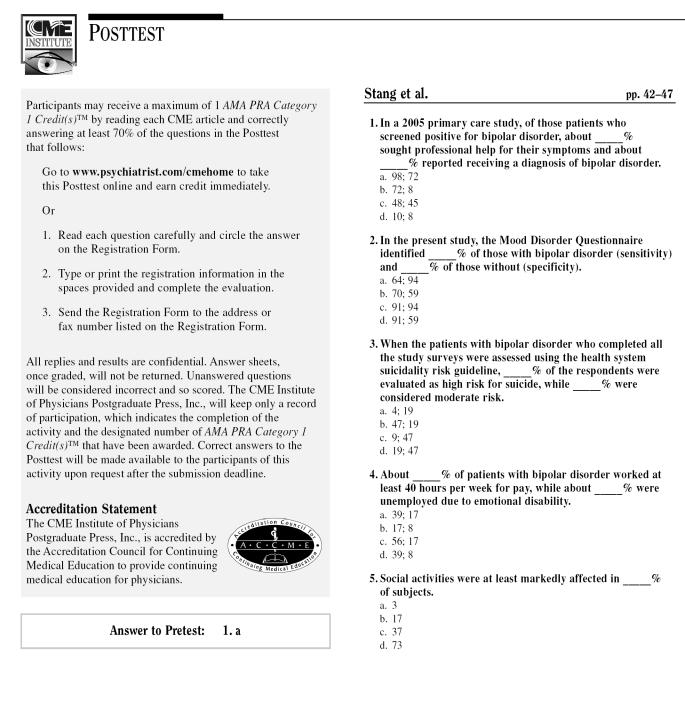
Posttest
Registration Form
Footnotes
This research was funded by GlaxoSmithKline.
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME article were asked to complete a statement regarding all relevant financial relationships between themselves or their spouse/partner and any commercial interest (i.e., any proprietary entity producing health care goods or services consumed by, or used on, patients) occurring within at least 12 months prior to joining this activity. The CME Institute has resolved any conflicts of interest that were identified. The disclosures are as follows: Dr. Stang has been a consultant to and received grant/research support from GlaxoSmithKline and other pharmaceutical companies. Dr. Burch is an employee of GlaxoSmithKline. Drs. Frank and Yood and Ms. Wells have no personal affiliations or financial relationships with any proprietary entity producing health care goods or services consumed by, or used on, patients to disclose relative to the article.
REFERENCES CITED
- Kupfer DJ.. Commentary: the increasing medical burden in bipolar disorder. JAMA. 2005;293:2528–2530. doi: 10.1001/jama.293.20.2528. [DOI] [PubMed] [Google Scholar]
- Das AK, Olfson M, and Gameroff MJ. et al. Screening for bipolar disorder in a primary care practice. JAMA. 2005 293:956–963. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Cass AR, and Holt DCL. et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005 18:233–239. [DOI] [PubMed] [Google Scholar]
- Begley CE, Annegers JF, and Swann AC. et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. 2001 19:483–495. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Williams JBW, and Spitzer RL. et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000 157:1873–1875. [DOI] [PubMed] [Google Scholar]
- Busch KA, Fawcett J, Jacobs DG.. Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003;64:14–19. doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- Jacobs DG, Brewer M, and Klein-Benheim M. Suicide assessment: an overview of recommended protocol. In: Jacobs DG, ed. The Harvard Medical School Guide to Suicide Assessment and Intervention. San Francisco, Calif: Jossey-Bass. 1998 3–39. [Google Scholar]
- Mundt JC, Marks IM, and Shear MK. et al. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002 180:461–464. [DOI] [PubMed] [Google Scholar]
- Dittmann S, Biedermann NC, and Grunze H. et al. The Stanley Foundation Bipolar Network: results of the naturalistic follow-up study after 2.5 years of follow-up in the German centres. Neuropsychobiology. 2002 46suppl 1. 2–9. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Kirk GF, and Gavin C. et al. Determinants of functional outcome and healthcare costs in bipolar disorder: a high-intensity follow-up study. J Affect Disord. 2001 65:231–241. [DOI] [PubMed] [Google Scholar]
- Schneck CD, Miklowitz DJ, and Calabrese JR. et al. Phenomenology of rapid-cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry. 2004 161:1902–1908. [DOI] [PubMed] [Google Scholar]
- Sachs GS.. Bipolar mood disorder: practical strategies for acute and maintenance phase treatment. J Clin Psychopharmacol. 1996;16(2 suppl 1):32S–47S. doi: 10.1097/00004714-199604001-00005. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Manic Depressive Illness. New York, NY: Oxford University Press. 1990 [Google Scholar]
- Altshuler L, Suppes T, and Black D. et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry. 2003 160:1252–1262. [DOI] [PubMed] [Google Scholar]
- Berk M, Dodd S.. Are treatment emergent suicidality and decreased response to antidepressants in younger patients due to bipolar disorder being misdiagnosed as unipolar depression? Med Hypotheses. 2005;65:39–43. doi: 10.1016/j.mehy.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Ghaemi N, Sachs GS, Goodwin FK.. What is to be done? controversies in the diagnosis and treatment of manic-depressive illness. World J Biol Psychiatry. 2000;1:65–74. doi: 10.3109/15622970009150569. [DOI] [PubMed] [Google Scholar]
- Woods SW. The economic burden of bipolar disease. J Clin Psychiatry. 2000 61suppl 13. 38–41. [PubMed] [Google Scholar]
- Chen YW, Dilsaver SC.. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other axis I disorders. Biol Psychiatry. 1996;39:896–899. doi: 10.1016/0006-3223(95)00295-2. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE.. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, and Grochocinski VJ. et al. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry. 2002 63:120–125. [DOI] [PubMed] [Google Scholar]
- Suppes T, Leverich GS, and Keck PE. et al. The Stanley Foundation Bipolar Treatment Outcome Network II: demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001 67:45–59. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Harrow M.. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. J Affect Disord. 2004;81:123–131. doi: 10.1016/S0165-0327(03)00161-7. [DOI] [PubMed] [Google Scholar]
- Shi L, Thiebaud P, McCombs JS.. The impact of unrecognized bipolar disorders for patients treated for depression with antidepressants in the fee-for-services California Medicaid (Medi-Cal) program. J Affect Disord. 2004;82:373–383. doi: 10.1016/j.jad.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Bostwick JM, Pankratz VS.. Affective disorders and suicide risk. Am J Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- Sharma R, Markar HR.. Mortality in affective disorder. J Affect Disord. 1994;31:91–96. doi: 10.1016/0165-0327(94)90112-0. [DOI] [PubMed] [Google Scholar]
- Guze SB, Robins E.. Suicide and primary affective disorders. Br J Psychiatry. 1970;117:437–438. doi: 10.1192/bjp.117.539.437. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B.. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Brodersen A, Licht RW, and Vestergaard P. et al. Sixteen-year mortality in patients with affective disorder commenced on lithium. Br J Psychiatry. 2000 176:429–433. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Kupfer DJ, Rucci P.. Suicide attempts and ideation in patients with bipolar I disorder. J Clin Psychiatry. 2004;65:509–514. doi: 10.4088/jcp.v65n0409. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Fireman B, and Simon GE. et al. Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA. 2003 290:1467–1473. [DOI] [PubMed] [Google Scholar]
- Zwerling C, Whitten PS, and Sprince NL. et al. Workforce participation by persons with disabilities: the National Health Interview Survey Disability Supplement, 1994 to 1995. J Occup Environ Med. 2002 44:358–364. [DOI] [PubMed] [Google Scholar]
- Abood Z, Sharkey A, and Webb M. et al. Are patients with bipolar affective disorder socially disadvantaged? a comparison with a control group. Bipolar Disord. 2002 4:243–248. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, and Barber CB. et al. The association between chronic medical conditions and work impairment. In: Rossi AS, ed. Caring and Doing for Others: Social Responsibility in the Domains of Family, Work, and Community. Chicago, Ill: University of Chicago Press. 2001 403–426. [Google Scholar]
- Hirschfeld RM, Lewis L, Vornik LA.. Perceptions and impact of bipolar disorder: how far have we really come? results of the National Depressive and Manic-Depressive Association 2000 Survey of Individuals With Bipolar Disorder. J Clin Psychiatry. 2003;64:161–174. [PubMed] [Google Scholar]