Abstract
Chronic pain has adverse effects on individuals with chronic pain (ICPs) as well as their family members. Borrowing from an empathy model described by Goubert et al. (2005), we examined top-down and bottom-up factors that may be related to psychological well-being in the spouses of ICPs. A diverse community sample of 113 middle-aged spouses of individuals with chronic pain (ICPs) completed measures on pain severity and spouse pain catastrophizing (PCS-S; Cano et al., 2005). Results showed that almost half (48.7%) of spouses reported chronic pain themselves and that pain in the spouse accounted for within-couple differences on psychological distress. That is, in couples where only the ICP reported pain, ICP psychological distress was greater than their spouses. However, when both partners reported chronic pain, there was no significant difference in psychological distress between partners. Hierarchical regression analyses showed that spouse magnification catastrophizing was associated with depressive and anxiety symptoms, and that helplessness catastrophizing was associated with depressive symptoms for spouses of ICPs who also reported chronic pain but not for spouses of ICPs without chronic pain. The results are discussed in light of interpersonal processes that may affect spouses’ distress.
Keywords: Chronic pain, Couples, Depression, Anxiety, Catastrophizing, Spouses
1. Introduction
Pain has an adverse impact on the significant others of individuals with chronic pain (ICPs). For example, spouses of ICPs report elevated psychological distress when compared to spouses of diabetic patients and healthy individuals (Shanfield et al., 1979;Rowat and Knafl, 1985;Flor et al., 1987a;Subramanian, 1991;Smith et al., 1999;Bigatti and Cronan, 2002). An understanding of how pain impacts the psychological distress of spouses requires a conceptual framework that accounts for characteristics of both partners. One such framework, developed by Goubert et al. (2005), suggests that both top-down (i.e., observer characteristics) and bottom-up influ-ences (i.e., ICP pain cues) provide pain observers (e.g., spouses of ICPs) with knowledge about ICPs’ experiences. This knowledge then contributes to a variety of spouse affective responses including psychological distress. The purpose of this study is test the extent to which top-down and bottom-up characteristics directly relate to psychological distress in spouses of ICPs.
Two top-down influences mentioned by Goubert et al. (2005)are spouses’ pain catastrophizing (i.e., an exaggerated and negative focus on pain) about ICPs’ pain and spouses’ personal experiences with pain. Both variables might impact spouse distress because they provide the observer spouse with information and knowledge about the ICPs’ pain. While the literature has focused on pain catastrophizing as a correlate of psychological distress in ICPs (Keefe et al., 1989;Sullivan and D’Eon, 1990;Geisser et al., 1994;Turner et al., 2000,2002), research also demonstrates that spouses catastrophize about ICPs’ pain (Cano et al., 2005). As a top-down influence, spouse pain catastrophizing contributes to spouses’ sense of knowing about the ICPs’ pain. Therefore, spouse pain catastrophizing may create a sense of exaggerated or heightened concern about ICPs’ pain that contributes to spouse psychological distress.
As indicated earlier, spouses’ own personal experiences with pain may also be considered a top-down variable. Although personal experience with pain appears to affect accuracy of pain judgments (Robinson and Wise, 2004), no published studies of which we are aware have examined the association between spouses’ personal experiences of pain with their own elevated psychological distress. Chronic pain in the spouse may intensify the negative impact of catastrophizing because the knowledge about ICP pain is enhanced with first-hand experience.
Finally, bottom-up variables such as ICP pain severity provide additional information and cues about the ICP that may heighten distress in spouses. Previous studies have demonstrated the importance of pain severity in spouse distress (Schwartz et al., 1991); however, no studies to date have examined the top-down and bottom-up influences simultaneously. As the model suggests, these influences may contribute uniquely and jointly to spouse distress.
In sum, we expected that spouses’ psychological distress would be a function of these top-down and bottom-up influences. Specifically, we expected that spouses’ pain catastrophizing and personal experiences with chronic pain as well as ICP pain severity would be related to spouses’ psychological distress. Such findings would support the validity of models accounting for characteristics of observers and ICPs, and suggest that spouse distress is deserving of research and clinical attention.
2. Method
2.1. Participants
The participants were 139 married couples, which included one couple member who had a chronic musculoskeletal pain condition (ICP) and his/her spouse. A subset of these participants participated in Cano (2004,2005). The spouses of the ICPs were predominately male (58.4%, n= 66) and the sample was diverse (53.1% Caucasian, 38.9% African American, 8.0% other [Hispanic/Latino, Native American, Asian, multiracial]). On average, spouses were 54 years old (SD = 13.6), had 14.4 years of education (SD = 2.7), and had been married 20.6 years (SD = 16.7).
To clarify terminology, the current study consisted of ICPs and their spouses. The individual with the chronic musculoskel-etal condition was deemed the “ICP” and their partner as the “spouse.” Throughout the rest of the paper, the term “spouses” is used to identify the spouses of ICPs as a group. A distinction was made between “healthy spouses” and “spouses with chronic pain (SCPs).” When both partners in a couple reported chronic pain, the couple member with the musculoskeletal pain condition (e.g., osteoarthritis) as opposed to other chronic pain conditions was chosen as the ICP. If, however, both partners reported a chronic musculoskeletal pain condition, the ICP was identified as the individual who had the most severe or debilitating pain as indicated by reports from each partner during the telephone screening interview. General pain information obtained from both partners revealed that ICPs had more severe pain on a 5-point Likert scale question on pain severity (M = 4.0, SE = .12) than SCPs (M = 3.32, SE = .13), t(68) = 4.02, p < .01, consistent with the study design.
Almost half of the spouses reported chronic pain themselves (48.7%, n = 55). The most common location for SCPs to have pain was in their lower back or knees (49.1%, n = 27 for both locations). Of the spouses who reported pain, 58.2% (n = 32) had received a diagnosis for their pain, the most common being osteoarthritis (41.6%, n = 22). See Table 1 for additional information on spouses who reported pain.
Table 1.
Pain ratings and duration for spouses with chronic pain
| Scale | Mean (SD) |
|---|---|
| Pain severity (scale from 1–5) | 3.3 (1.11) |
| Average visual analogue rating scale | 44.3 (28.8) |
| Average length of pain (in months) | 130.85 (113.21) |
Note. N = 55.
2.2. Measures
2.2.1. Psychological distress
The Mood and Anxiety Questionnaire (MASQ; Watson and Clark, 1991) provides five subscales to assess symptoms of anxiety, depression, and general distress. The MASQ has a stable factor structure in adult samples (Watson et al., 1995) and in community and clinic pain samples (Geisser et al., 2006). The non-specific depression subscale (12 items, α = .90) and the anhedonic depression subscale (22 items, α = .94) measure depressive symptoms whereas the non-spe-cific anxiety (11 items α = .84) and anxious arousal (17 items, α = .85) assess anxiety symptoms. The inclusion of anxiety symptoms in the current study is important to note as this type of psychological distress has not yet been explored in spouses of ICPs in the current literature. Means for the non-specific depression scale, anhedonic depression scale, non-specific anxiety scale, and the anxious arousal scale were 22.2 (SD = 8.6), 57.2 (SD = 15.6), 19.7 (SD = 6.5), 27.3 (SD = 8.1) for patients and 20.3 (SD = 7.8), 51.3 (SD = 15.1), 17.0 (SD = 5.9), 23.9 (SD = 7.5) for spouses, respectively. These means were very similar to the means for community men and women reported by Watson et al., (1995 ). Spouses’ non-specific depressive symptoms and anhe-donic depressive symptoms were highly correlated with one another (r[113] = .77, p < .001), as were non-specific anxiety and anxious arousal symptoms (r[113] = .77, p < .001). Therefore, a composite depressive and anxiety symptom score was calculated to protect against Type I error and redundant results in later analyses. The inter-item reliabilities for both depression (34 items) and anxiety (28 items) composite scores were excellent (αs = .95 and .91, respectively).
Comparisons between SCPs and ICPs were conducted to further understand spouses’ psychological distress, particularly in light of the within couple differences that have been reported in the literature (e.g., Ahern and Follick, 1985;Flor et al., 1987b). A repeated measures ANOVA was conducted separately for each composite score to determine if spouse pain status was an important correlate of within-couple differences. These analyses showed that the ICP-spouse differences in depressive symptoms were moderated by the pain status of the spouse (F[1] = 7.72, p < .01). Post hoc paired t-tests were conducted and revealed that within-couple differences in depressive symptoms were found only for couples in which only one partner suffered from chronic pain (t[111] = 4.53 p < .001; ICP M = 79.79, SE = 3.01 and spouse M = 65.32, SE = 2.28, respectively). ICPs and SCPs did not report significantly different mean scores on symptoms of depression (t[111] = 0.69, p > .05; ICP M = 81.11, SE = 3.31 and SCP M = 78.55, SE = 3.40, respectively). Similar results for symptoms of anxiety were found for both spouses who denied a pain condition (t[111] = 5.22, p < .001; ICP M = 44.81, SE = 1.50 and spouse M = 35.49, SE = 0.94) and SCPs (t[111] = 1.15, p > .05; ICP M = 49.69, SE = 2.17 and SCP M = 46.47, SE = 2.05). These differences suggest that spouses’ personal experiences of pain are an important top-down influ-ence that should be examined as a correlate of spouse distress.
2.2.2. Pain catastrophizing
The Pain Catastrophizing Scale-Significant Other Version (PCS-S) (Cano et al., 2005) was adapted from Sullivan et al.’s (1995)Pain Catastrophizing Scale (PCS) for use with significant others by rewording the questions so that spouses indicated the degree of their catastrophizing about ICPs’ pain. The PCS-S consists of 13 items and assesses three components of catastrophizing: magnification (3 items; e.g., “I wonder whether something serious may happen”), helplessness (6 items; e.g., “There is nothing I can do to reduce the intensity of the pain”), and rumination (4 items; e.g., “I keep thinking about how much it hurts”). The PCS-S has a stable factor structure that is invariant across gender and racial groups (Cano et al., 2005). In the current study, each of the three components of catastrophizing was analyzed individually. This is particularly important as there are no studies of which we are aware that explore each dimension separately as a correlate of distress. Inter-item reliabilities for the PCS-S subscales in the current sample were acceptable (magnification α = .77, helplessness α = .78, and rumination α = .84). There were no differences between SCPs and healthy spouses on dimensions of pain catastrophizing (p > .05).
2.2.3. Pain severity
Pain severity is an important correlate of spouse psychological distress in clinical samples (e.g., Geisser et al., 2005); therefore, it is also included in this community study. Because the current literature has been somewhat inconsistent about which couple member’s (ICP or spouse) report of pain severity is used, we used ratings from both ICPs and spouses. Pain severity was assessed with the pain severity subscales (3 items) of the Multidimensional Pain Inventory (MPI) (Kerns et al., 1985) and Multidimensional Pain Inventory-Spouse Version (MPI-S) (Flor et al., 1987a). This subscale assesses affective, sensory, and evaluative pain dimensions. The items ask for a rating of the ICP’s pain at the current moment, average severity, and amount of suffering experienced by the ICP. The reliability for the current sample was adequate for ICPs and excellent for spouses (αs = .77 and .85, respectively). ICPs’ ratings of pain severity and spouses’ ratings were significantly related to one another (r[137] = .45, p < .001). Therefore, a composite pain severity score was computed by adding the two pain severity ratings. This composite was used in further analyses. The reliability of the pain composite was excellent (α = .82).
2.2.4. Marital satisfaction
The Dyadic Adjustment Scale (DAS) (Spainer, 1976) measures overall marital satisfaction and discord. The DAS consists of 32 items that measure agreement on a variety of topics (e.g., finances and world views), degree of affection, and general marital happiness. The range of the scale is from 0 to 151 with higher scores indicating greater marital satisfaction. Marital satisfaction was included as a covariate in the hierarchical regression analyses because marital satisfaction is consistently related to depressive symptoms in pain samples (see Leonard et al., 2006) and marital satisfaction is important aspect of the spouse’s experience of pain (Maruta et al., 1981;Ahern and Follick, 1985;Flor et al., 1987a;Geisser et al., 2005). The alpha for the spouses was .93, indicating excellent inter-item reliability. Scores on the DAS were not significantly different for SCPs and healthy spouses (p > .05).
2.3. Procedure
Couples were recruited from newspaper advertisements as part of a larger study of marriage and chronic pain. Upon responding to these advertisements, participants were screened over the telephone to ensure eligibility prior to the completion of any study related materials. Couples were eligible if they met all of the following criteria: (1) married or living together for a minimum of two years, (2) at least one spouse experienced a chronic musculoskeletal pain condition, (3) the pain condition lasted at least six months, (4) neither couple member had been diagnosed with a terminal illness, (5) both couple members were able to demonstrate adequate cognitive ability as assessed by a telephone version of the Mini-Mental Status Exam (MMSE) (Folstein et al., 1975). Once a couple was deemed eligible, an appointment was made for the couple to come to the laboratory where research assistants described the protocol to the couples and obtained written consent. Each partner then completed questionnaires independently and participated in the larger study protocol. Upon completion of the study, participants were debriefed and compensated $100 for their effort.
2.4. Analysis plan
Of the 139 couples recruited, 25 of the spouses who initially participated did not complete the PCS-S and consequently were excluded from analyses. Additionally, two individuals did not provide complete data for the MASQ and were excluded. There were no significant differences on pain catastrophizing, ICP pain severity, or their own likelihood of reporting pain (p > .05) between participants who did and did not complete the questionnaires. There was a significant difference, however, on marital satisfaction (t[137] = –2.60, p < .05), where spouses who provided complete data had higher mean scores on the DAS (M = 111.59, SE = 1.67) than those who did not (M = 102.13, SE = 4.26). The final sample consisted of 113 spouses when non-completers were excluded from the analyses.
Pearson product–moment correlations were conducted to examine the bivariate relationships of the top-down variable of pain catastrophizing, bottom-up variable of ICP pain severity, and potential covariate of marital satisfaction with depressive and anxiety symptoms. We also examined the extent to which the top-down variable of personal experiences with pain would be related to spouse distress through t-tests.
Next, hierarchical regressions were conducted to examine the overall relationship between pain in the spouse and catastrophizing to spouses’ depressive and anxiety symptoms as well as any interactions. Each of the catastrophizing subscales was tested separately. Before completing the regression analyses, however, all variables were centered as recommended by Cohen (1988)andHolmbeck (2002)to reduce multicollinearity among the variables. Each of the regressions included marital satisfaction and gender as covariates entered in the first step. Marital satisfaction was included in light of the significant correlation between marital satisfaction with spouse depressive (r = –.42, p < .001) and anxiety symptoms (r = –.28, p < .01), as well as the consistent relationship between marital satisfaction and psychological distress in the existing literature (e.g., Kerns and Turk, 1984 ; Kerns et al., 1990 ; Cano et al., 2000 , 2004 ). Gender was also included as a covariate because analyses revealed significant gender differences on depressive symptoms (t[112] = –2.44, p < .05), with female spouses reporting more symptoms of depression than their male counterparts (M = 78.36 [SE = 3.68] and M = 67.65 [SE = 2.39], respectively). The gender difference for symptoms of anxiety was in the same direction and approached significance (t[112] = –1.86, p < .07). Therefore, gender was included as a covariate in analyses predicting depressive and anxiety symptoms. The second step for the regression of depressive symptoms included the main effects for one of the catastrophizing subscales, pain in the spouse, and ICP pain severity, while for anxiety symptoms ICP pain severity was excluded as it was not significantly correlated with symptoms of anxiety (r = .12, p > .05). The third step of the regressions included the two-way interaction terms between the variables entered in step 2. The depressive symptom regression included a fourth step consisting of a three-way interaction between ICP pain severity, pain catastrophizing, and pain in the spouse. There were six regressions calculated in total: one for each subscale of the catastrophizing measure (magnification, helplessness, and rumination) predicting either depressive or anxiety symptoms. Any significant interactions in the regressions were then subjected to post hoc analysis as per Holmbeck (2002) , where multiple regression analysis is used to estimate the expected value of the dependent variable at high (+1SD) and low (–1SD) levels of the independent variable.
3. Results
3.1. Correlations and t-tests
Bivariate correlations are shown in Table 2. As one would expect, depressive and anxiety symptoms were strongly related to each other and the three pain catastrophizing subscales were also significantly related to each other. As hypothesized, the bottom-up influence of ICP pain severity was significantly and positively related to spouses’ depressive symptoms. ICP pain severity was also related to each of the three catastrophizing subscales. The top-down factors of magnifica-tion and helplessness catastrophizing were also correlated significantly with depressive symptoms, with moderate effect sizes. However, rumination was not sig-nificantly related to either depressive or anxiety symptoms. In addition, magnification and helplessness were not significantly related to anxiety symptoms. The potential covariate of marital satisfaction was signifi-cantly and negatively related to depressive symptoms and magnification and helplessness catastrophizing.
Table 2.
Correlations among catastrophizing subscales, pain severity, and psychological distress
| Depressive symptoms | Anxiety symptoms | ICP pain severity | Marital satisfaction | Magnification | Helplessness | Rumination | |
|---|---|---|---|---|---|---|---|
| Depressive symptoms | – | .72* | .20a | −.42** | .23a | .28* | .16 |
| Anxiety symptoms | – | .12 | −.28* | .17 | .16 | .11 | |
| ICP pain severity | – | −.13 | .36** | .38** | .23a | ||
| Marital satisfaction | – | −.21a | −.30* | −.12 | |||
| Magnification | – | .70** | .56** | ||||
| Helplessness | – | .49** | |||||
| Rumination | – |
Note. (n = 113).
p < .05.
p < .01.
p < .001.
Independent samples t-tests were conducted to examine the association between the top-down variable of personal experience with chronic pain and symptoms of depression and anxiety. Results showed significant differences between SCPs and healthy spouses on reports of depressive symptoms (t[112] = –3.07, p < .01) and anxiety symptoms (t[112] = –4.75, p < .001). SCPs reported more depressive symptoms (M = 78.55 [SE = 3.40]) than spouses without pain (M = 66.00 [SE = 2.35]). Likewise, SCPs reported more anxiety symptoms (M = 46.47 [SE = 2.05]) than spouses without pain (M = 35.83 [SE = .98]).
3.2. Hierarchical regressions
Hierarchical regressions were conducted for both symptoms of depression and anxiety to determine the extent to which top-down and bottom-up variables are associated with psychological distress in spouses. Of particular interest were the interactions since earlier analyses demonstrated the bivariate relationships between variables.
For depressive symptoms, the interaction between spouses’ personal experiences with chronic pain and helplessness catastrophizing was significant (see Table 3). Post hoc examination showed that helplessness was positively related to depressive symptoms in SCPs (β = .55, t = 4.17, p < .001); however, helplessness was not significant in predicting symptoms of depression in spouses without chronic pain (β = .12, t = 1.10, p = .27) (see Fig. 1). Likewise, there was a significant interaction between magnification catastrophizing and the presence of chronic pain in the spouse, superceding the interpretation of the significant main effects of these variables (see Table 4). Post hoc examination showed that magnification was positively correlated with depressive symptoms for SCPs (β = .52, t = 3.73, p < .001); however, magnification was not significant in predicting depression in spouses without pain (β = .08, t = .75, p = .46). This interaction produced a similar pattern to that of helplessness and pain in the spouse, subsequently only one figure is displayed. All other interactions were not significant in these two regression analyses. Results from the regression with rumination showed main effects for gender (β = .25, t = 3.09, p < .01), marital satisfaction (β = –.33, t = –4.00, p < .001), and personal experience with chronic pain in the spouse (β = .31, t = 3.79, p < .001), however there were no significant interactions between these variables in relating to depressive symptoms.
Table 3.
Hierarchical regression predicting depressive symptoms from helplessness, ICP pain severity, and spouses’ personal experiences with chronic pain
| Variable | B | SE B | β | t | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
| Step 1 | .47 | ||||||
| Gender of spouse | 8.72 | 3.63 | .19 | 2.41* | |||
| Marital satisfaction | −.39 | .11 | −.31 | −3.73*** | |||
| Step 2 | .58 | .11*** | |||||
| Helplessness | −.11 | .63 | −.02 | −.17 | |||
| Spouse pain | 11.69 | 3.72 | .26 | 3.14** | |||
| ICP pain severity | .50 | .43 | .14 | 1.15 | |||
| Step 3 | .62 | .04a | |||||
| Helplessness × spouse pain | 2.01 | .88 | .26 | 2.27* | |||
| ICP pain severity × spouse pain | .13 | .62 | .03 | .22 | |||
| ICP pain severity × helplessness | .04 | .08 | .05 | .48 | |||
| Step 4 | .62 | .00 | |||||
| ICP pain severity × spouse pain × helplessness | .17 | .13 | .15 | 1.31 |
Note. ICP, individual with chronic pain.
p = .05.
p < .05.
p < .01.
p < .001.
Fig. 1.
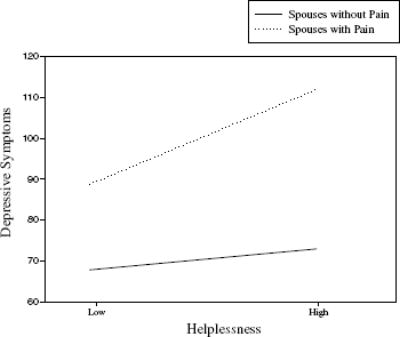
Interaction of helplessness and spouses’ personal experiences with chronic pain on depressive symptoms.
Table 4.
Hierarchical regression predicting depressive symptoms from magnification, ICP pain severity, and spouses’ personal experiences with chronic pain
| Variable | B | SE B | β | t | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
| Step 1 | .47 | ||||||
| Gender of spouse | 9.08 | 3.64 | .20 | 2.50* | |||
| Marital satisfaction | −.44 | .10 | −.34 | −4.26*** | |||
| Step 2 | .58 | .11** | |||||
| Magnification | −.30 | .81 | −.04 | −.37 | |||
| Spouse pain | 12.98 | 3.79 | .29 | 3.43*** | |||
| ICP pain severity | .47 | .43 | .14 | 1.11 | |||
| Step 3 | .62 | .04* | |||||
| Magnification × spouse pain | 2.71 | 1.28 | .24 | 2.11* | |||
| ICP pain severity × spouse pain | −.08 | .59 | −.02 | −.14 | |||
| ICP pain severity × magnification | .15 | .11 | .12 | 1.30 | |||
| Step 4 | .62 | .00 | |||||
| ICP pain severity × spouse pain × magnification | .04 | .22 | .02 | .20 |
Note. ICP, individual with chronic pain.
p < .05.
p < .01.
p < .001.
Similar regressions were conducted for anxiety symptoms. As for depressive symptoms, the interaction between magnification catastrophizing and chronic pain in the spouse was significant (see Table 5). A similar pattern to depressive symptoms was noted as post hoc examination results showed magnification was a signifi-cant predictor of anxiety symptoms for spouses in pain (β = .44, t = 3.24, p < .01); however, catastrophizing was not significant in predicting anxiety in spouses without pain (β = .05, t = .46, p = .65). Because this pattern of association was similar to the depressive symptom results above, we do not present a separate figure for anxiety symptoms. Regression analyses for helplessness and rumination catastrophizing showed main effects for gender (β = .17, t = 2.04, p < .05 and β = .21, t = 2.56, p < .05, respectively), marital satisfaction (β = 3.19, t = –2.26, p < .05 and β = –.20, t = –2.34, p < .05, respectively), and pain in the spouse (β = .42, t = 5.18, p < .001 and β = .44, t = 5.37, p < .001). Neither the main effects for helplessness and rumination nor the interaction terms were significant, ps > .05.
Table 5.
Hierarchical regression predicting anxiety symptoms from magnification and spouses’ personal experiences with chronic pain
| Variable | B | SE B | β | t | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
| Step 1 | .32 | ||||||
| Gender of spouse | 4.67 | 2.12 | .18 | 2.20* | |||
| Marital satisfaction | −.15 | .06 | −.20 | −2.45* | |||
| Step 2 | .54 | .22** | |||||
| Magnification | .15 | .42 | .03 | .27 | |||
| Spouse pain | 10.93 | 2.08 | .42 | 5.26** | |||
| Step 3 | .57 | .03* | |||||
| Magnification × spouse pain | 1.41 | .67 | .21 | 2.09* |
p < .05.
p < .001.
4. Discussion
Research has demonstrated that the interpersonal nature of chronic pain inevitably leads to negative consequences for both ICPs and others that are close to them. Borrowing from an empathy model of pain (Goubert et al., 2005), we examined both observer (i.e., top-down influences) and ICP (i.e., bottom-up influences) characteristics that may be important in affecting observers’ psychological distress.
ICP pain severity, a bottom-up variable, was related to spouse depressive symptoms as was expected. ICP pain severity may result in pain behaviors or other observable signs that cue the spouse as to how the ICP is feeling. Interestingly, ICP pain severity was not significantly associated with spouse anxiety symptoms in contrast to studies showing that pain severity is associated with anxiety in ICPs (Cano et al., 2004). Perhaps for spouses, witnessing a partner in pain is not associated with a high arousal state including fear or tension.
One top-down influence examined in the current study was spouses’ personal experiences with chronic pain. Spouses who experience pain themselves may have a greater appreciation for the diffculties ICPs may face (i.e., a greater sense of knowing; Goubert et al., 2005). Indeed, we found that spouses’ personal experience with chronic pain was associated with greater distress. In fact,almost half of the spouses reported a chronic pain problem. While this number may not be surprising because of the high prevalence of chronic pain (Bonica, 1990;Smith et al., 1999), few studies have investigated this matter. Past research that has examined spouses’ general health has shown that spouses of ICPs are more likely to have pain symptoms than spouses of patients with diabetes (Flor et al., 1987a). Additionally, spouses of depressed pain patients have more pain symptoms than spouses of depressed patients without pain (Mohamed et al., 1978). Mohamed et al. (1978) further noted that the location of the pain symptoms among spouses was more similar to patient’s pain location for this group compared to the depressed group without pain. Although that study lacked a group of participants who were not depressed but still had pain, the findings suggest some similarity within couples with pain. It is possible that some spouses of ICPs experience more physical wear and tear on their bodies due to additional responsibilities (e.g., household chores). Clearly, researchers should fully examine such top-down variables and not assume that all spouses of ICPs are physically healthy.
Spouses’ pain catastrophizing was also investigated as a top-down influence that relates to psychological distress because it could enhance or alter spouses’ knowledge about ICPs’ pain. Helplessness and magnification catastrophizing were correlated with depressive symptoms; however, several significant interactions suggested that more complex relationships existed when also accounting for the spouses’ personal experiences with pain. That is, magnification and helplessness catastrophizing were significant correlates of depressive symptoms in SCPs but not in spouses without chronic pain, despite the absence of significant differences in the mean levels of pain catastrophizing for SCPs compared to spouses without chronic pain. The magnification results were also found for anxiety symptoms. These interactions are consistent with the framework presented earlier, and suggest that multiple top-down characteristics work together in influencing affective response to chronic pain. For instance, spouses who have personal experience with pain and magnify the ICPs’ pain may feel more depressed and anxious because it is diffcult for them to pull their attention away from pain cues. Spouses who have pain and also engage in helplessness catastrophizing may have increased feelings of hopelessness and perceptions of caregiver burden. Not only is their sense of knowing about their partners’ pain increased but that sense of knowing might also contribute to catastrophizing about their own pain. Unfortunately, we did not assess spouses’ catastrophizing directed toward their own pain experience. Future research may be able to address the relative contributions of ICP-directed and self-directed pain catastrophizing in spouses. Such research could address the possibility that the negative effects of spouse catastrophizing are activated only when spouses experience pain. In addition, it is possible that psychological distress primes spouses to focus on negative aspects of their own and the ICPs’ pain problems. Additional longitudinal or experimental studies must be conducted to further explore the mechanisms and directions between the relationship of catastrophizing and psychological distress.
Helplessness catastrophizing did not interact with spouses’ personal experiences with chronic pain in associating with anxiety symptoms. Helplessness catastrophizing may not be a factor in anxiety symptoms because of the high arousal nature of these symptoms. Alternatively, helplessness catastrophizing may tap feelings of hopelessness and “giving up” rather than helplessness or feelings of threat, which might explain why this type of catastrophizing is related to depressive but not anxiety symptoms in spouses. In addition, rumination catastrophizing was not associated with depressive or anxiety symptoms. The content of the rumination items (i.e., “I keep thinking about how much it hurts my partner”) may reflect persistent thoughts about ICP pain as well as spouses’ care and concern for ICPs’ welfare. While creating sustained attention on the negative impact of the pain and increasing spouses’ sense of knowing about ICPs’ pain, rumination may result in a feeling of understanding of ICPs’ experiences. Therefore, while rumination catastrophizing may be experienced as unpleasant, it may not correlate with spouse distress. Perhaps, ruminative catastrophizing is associated with other spouse outcomes such as spouse solicitous responses to pain. Additional research is needed to further clarify this hypothesis.
Although the current study has contributed to the knowledge of the impact of pain on spouses, there are several limitations. First, the data used in the current study were cross-sectional in nature. Therefore, these data cannot be used to provide causal or temporal explanations. Additionally, data regarding the pain status of the spouse were based solely on the self-report and verification of pain by physician reports of medical information was not conducted. Spouses of ICPs may be primed to interpret physical sensations as pain because they are confronted with ICP pain almost daily. The current study asked spouses to report on their pain catastrophizing about pain in the ICPs. The extent to which SCPs catastrophize about their own pain is unknown. Finally, although we discuss the findings in the context of an empathy framework, empathy was not directly measured in the current study. To provide a complete test of the Goubert et al. (2005) model, researchers must examine empathy and how it relates to top-down and bottom-up characteristics as well as observers’ psychological distress and behavioral reactions.
In sum, the current findings provide support for the further exploration of top-down and bottom-up factors that contribute to observers’ experiences (Goubert et al. 2005). The current study also emphasizes the need to include both partners in the assessment of chronic pain for research and treatment purposes. It is recommended that researchers interested in spouses of ICPs differentiate between SCPs and spouses without chronic pain to identify important processes that may account for psychological distress. Additionally, the interaction between top-down and bottom-up factors within couples and other close dyads (e.g., parents and children) should be explored as chronic pain clearly has interpersonal consequences.
Footnotes
The first author was supported by Grant T32 AG00275 and the second author was supported by Grant K01 MH066975 while working on this paper.
References
- Ahern D, Follick M. Distress in spouses of chronic pain patients. Int J Fam Ther. 1985;7:247–57. [Google Scholar]
- Bigatti S, Cronan T. An examination of the physical health, health care use, and psychological well-being of spouses of people with fibromyalgia syndrome. Health Psychol. 2002;21:157–66. [PubMed] [Google Scholar]
- Bonica J., 2nd . The management of pain. 1 . London: Lea and Febiger; 1990. [Google Scholar]
- Cano A. Pain catastrophizing and social support in married individuals with chronic pain: the moderating role of pain duration. Pain. 2004;110:656–64. doi: 10.1016/j.pain.2004.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano A, Gillis M, Heinz W, Geisser M, Foran H. Marital functioning, chronic pain, and psychological distress. Pain. 2004;107:99–106. doi: 10.1016/j.pain.2003.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano A, Leonard M, Franz A. The significant other version of the pain catastrophizing scale (PCS-S): preliminary validation. Pain. 2005;119:26–37. doi: 10.1016/j.pain.2005.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano A, Weisberg J, Gallagher R. Marital satisfaction and pain severity mediate the association between negative responses to pain and depressive symptoms in a chronic pain patient sample. Pain Med. 2000;1:35–43. doi: 10.1046/j.1526-4637.2000.99100.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hills-dale, NJ; Lawrence Erlbaum: 1988. [Google Scholar]
- Flor H, Turk D, Scholz O. Impact of chronic pain on the spouse: marital, emotional and psychical consequences. J Psychosom Res. 1987a;31:63–71. doi: 10.1016/0022-3999(87)90099-7. [DOI] [PubMed] [Google Scholar]
- Flor H, Kerns R, Turk D. The role of spouse reinforcement, perceived pain, and activity levels of chronic pain patients. J Psychosom Res. 1987b;31:251–9. doi: 10.1016/0022-3999(87)90082-1. [DOI] [PubMed] [Google Scholar]
- Folstein M, Folstein S, McHugh P. Mini-mental state: a practical method for grading the state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Geisser M, Cano A, Foran H. Psychometric properties of the MASQ in two sample of chronic pain patients. Clin J Pain. 2006;22:1–9. doi: 10.1097/01.ajp.0000146180.55778.4d. [DOI] [PubMed] [Google Scholar]
- Geisser M, Cano A, Leonard M. Factors associated with marital satisfaction and mood among spouses of persons with chronic back pain. J Pain. 2005;6:518–25. doi: 10.1016/j.jpain.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Geisser M, Robinson M, Keefe F, Weiner M. Catastrophizing depression and the sensory, affective and evaluative aspects of chronic pain. Pain. 1994;59:79–83. doi: 10.1016/0304-3959(94)90050-7. [DOI] [PubMed] [Google Scholar]
- Goubert L, Craig K, Vervoort T, Morley S, Sullivan M, de C Williams A, et al. Facing others in pain: the effects of empathy. Pain. 2005;118:285–8. doi: 10.1016/j.pain.2005.10.025. [DOI] [PubMed] [Google Scholar]
- Holmbeck G. Post hoc probing of significant moderational and mediational effects in studies of pediatric populations. J Pediatr Psychol. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Keefe F, Brown G, Wallston K, Caldwell D. Coping with rheumatoid arthritis pain: Catastrophizing as a maladaptive strategy. Pain. 1989;37:51–6. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- Kerns R, Haythornthwaite J, Southwick S, Giller E. The role of marital interaction in chronic pain and depressive symptom severity. J Psychosom Res. 1990;34:401–8. doi: 10.1016/0022-3999(90)90063-a. [DOI] [PubMed] [Google Scholar]
- Kerns R, Turk D. Depression and chronic pain: the mediating role of the spouse. J Marriage Fam. 1984;46:845–52. [Google Scholar]
- Kerns R, Turk D, Rudy T. The west haven-yale multidimensional pain inventory (Whympi) Pain. 1985;23:345–56. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Leonard M, Johansen A, Cano A. Chronic pain in a couples context: a review and integration of theoretical models and empirical evidence. J Pain. 2006;7:377–90. doi: 10.1016/j.jpain.2006.01.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruta T, Osborne D, Swanson D, Halling J. Chronic pain patients and spouses marital and sexual adjustment. Mayo Clin Proc. 1981;56:307–10. [PubMed] [Google Scholar]
- Mohamed S, Weisz G, Waring E. The relationship of chronic pain to depression, marital adjustment, and family dynamics. Pain. 1978;5:285–92. doi: 10.1016/0304-3959(78)90015-5. [DOI] [PubMed] [Google Scholar]
- Robinson ME, Wise EA. Prior pain experience: influence on the observation of experimental pain in men and women. Pain. 2004;5:264–9. doi: 10.1016/j.jpain.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Rowat K, Knafl K. Living with chronic pain: the spouse’s perspective. Pain. 1985;23:259–71. doi: 10.1016/0304-3959(85)90104-6. [DOI] [PubMed] [Google Scholar]
- Schwartz L, Slater M, Birchler G, Atkinson J. Depression in spouses of chronic pain patients: the role of patient pain and anger, and marital satisfaction. Pain. 1991;44:61–7. doi: 10.1016/0304-3959(91)90148-Q. [DOI] [PubMed] [Google Scholar]
- Shanfield S, Heiman E, Cope D, Jones J. Pain and the marital relationship: psychiatric distress. Pain. 1979;7:343–51. doi: 10.1016/0304-3959(79)90090-3. [DOI] [PubMed] [Google Scholar]
- Smith B, Hopton J, Chambers W. Chronic pain in primary care. Fam Pract. 1999;16:475–82. doi: 10.1093/fampra/16.5.475. [DOI] [PubMed] [Google Scholar]
- Spainer G. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–28. [Google Scholar]
- Subramanian K. The multidimensional impact of chronic pain on the spouse: a pilot study. Soc Work Health Care. 1991;15:47–62. doi: 10.1300/j010v15n03_03. [DOI] [PubMed] [Google Scholar]
- Sullivan M, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Asses. 1995;7:524–32. [Google Scholar]
- Sullivan M, D’Eon J. Relation between catastrophizing and depression in chronic pain patients. J Abnorm Psychol. 1990;99:260–3. doi: 10.1037//0021-843x.99.3.260. [DOI] [PubMed] [Google Scholar]
- Turner J, Jensen M, Romano J. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85:115–25. doi: 10.1016/s0304-3959(99)00259-6. [DOI] [PubMed] [Google Scholar]
- Turner J, Jensen M, Warms C, Cardenas D. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain. 2002;98:127–34. doi: 10.1016/s0304-3959(02)00045-3. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark L. Mood and anxiety symptom questionnaire, unpublished manuscript. University of Iowa, Department of Psychology; Iowa City, IA: 1991. [Google Scholar]
- Watson D, Weber K, Assenheimer J, Clark L, Strauss M, McCormick R. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. J Abnorm Psychol. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]


