Abstract
Comprehensive intervention for homeless, street living youth that addresses substance use, social stability, physical and mental health issues has received very little attention. In this study, street living youth aged 14 to 22 were recruited from a drop-in center and randomly assigned the Community Reinforcement Approach (CRA) or treatment as usual (TAU) through a drop-in center. Findings showed that youth assigned to CRA, compared to TAU, reported significantly reduced substance use (37% v. 17% reduction), depression (40% v. 23%) and increased social stability (58% v. 13%). Youth in both conditions improved in many other behavioral domains including substance use, internalizing and externalizing problems, and emotion and task oriented coping. This study indicates that homeless youth can be engaged into treatment and respond favorably to intervention efforts. However, more treatment development research is needed to address the barriers associated with serving these youth.
Keywords: homelessness, adolescents, substance abuse, treatment, community reinforcement approach (CRA)
Treatment Outcome for Street-Living, Homeless Youth
Although research focusing on chronic runaways and homeless youth is increasing, there is a void of treatment evaluation studies with this group. Clements, Gleghorn, Garcia, Katz, and Marx (1997) note the importance of examining street based youth as separate from more stable, shelter residing youth given the higher levels of risk behaviors among street living youth. Street living youth often do not access other institutional settings (shelters, foster care, treatment centers) or family for assistance because these systems are not perceived to meet their needs (Marshall & Bhugra, 1996). In sum, differences among street living and shelter residing youth suggest the need for different intervention foci. Different challenges are posed and different treatment strategies are needed when addressing substance use and motivation for change in a youth whose basic needs are met (shelter-residing youth) than for a youth who has trouble finding enough food to eat, a place to sleep and receiving needed medical care.
Scope of the Problem
Although estimates are crude given that these youth do not make it into standard school or population surveys, estimates of the number of youth who leave home prematurely each year is estimated to reach nearly to two million (Shane, 1996). Substance abuse, mental and physical health problems among street living youth are significant issues for those that serve this population. Compared to non-homeless counterparts, researchers have found higher rates of suicide (Molnar, Shade, Kral, Booth, & Watters, 1998) physical and sexual abuse (Rew, Taylor-Seehafer, & Fitzgerald, 2001), high risk behaviors (Ennett, Federman, Bailey, Ringwalt, & Hubbard, 1999) and psychiatric disorders (Cauce et al., 2000). Also, Kipke, Montgomery, Simon and Iverson (1997) reported that 71% of their sample (N = 432) of homeless youth were classified as having an alcohol and/or illicit drug abuse disorder, while Baer, Ginzler and Peterson (2003) found that 69% of their homeless sample met criteria for dependence for at least one substance.
Treatment Findings
Most of the research on the adult homeless has focused on ‘captive’ shelter samples that are easy to approach and identify, although findings from these populations cannot be generalized to homeless individuals who live on the streets and do not access social services (Marshall & Bhugra, 1996). Chamberlain and MacKenzie (2004) argue that intervention and prevention should consider that youth go through various stages before they self-identify as a homeless person, with different interventions needed at different points in the homeless trajectory. The first stage being when youth are “at risk” as determined by school counselors. The second stage is when youth begin to break from the home and family (runaway), with the next stage being when the youth no longer considers him or herself as belonging to the family. The final stage is “transition to chronicity” when the youth experiences sustained periods of homelessness. Chamberlain and MacKenzie (2004) propose that at the early stages, intervention to support family reconciliation is important while a community placement program for later stages is needed. Only two randomized clinical trials addressing the multiple needs of this population were identified in the literature, and each study generally reflects the stage-based intervention strategies described by Chamberlain and McKenzie (2004).
Cauce et al. (1994) compared an intensive case management intervention with a less intensive, service as usual case management intervention through a drop-in center for street living youth. Few differences were found between the case management provided by drop-in center staff and the project’s intensive case management along the Child Behavior Checklist subscales, depression, problem behaviors and substance use. The authors concluded that the greater cost of the intensive case management makes it difficult to justify given the few differences in outcomes detected. Slesnick and Prestopnik (2005) evaluated an Ecologically-Based Family Therapy (EBFT) intervention with shelter-residing youth as compared to treatment as usual through a runaway shelter. Findings showed that youth assigned to EBFT reported greater reductions in overall substance abuse compared to youth assigned to treatment as usual through the shelter while many other problem areas including internalizing, externalizing, family relations, and communication improved in both conditions up to 15 months post-baseline.
An Ecological Approach to the Problems of Homeless Youth
The intervention highlighted in this study is informed by the social ecological/systems model outlined by the developmental theorist Urie Bronfenbrenner (1979). At the core of this model is the idea that behavioral trajectories and outcomes (such as homelessness) are the result of activities within defined settings and/or in response to the demands of specific social systems. The primary goal of any intervention needs to be – at least from an ecological perspective – removing the adolescent from dangerous settings, making sure they make better decisions about their activities in difficult settings, and replacing settings that promote deviant behavior (e.g. the street, a flop house) with more positive settings that promote healthy and safe behavior.
The ecological/systems approach suggests that all important (life defining) activities takes place within defined, delineated settings (Bronfenbrenner referred to these primary activity settings as micro-systems). The critical factor in micro-system analyses is the web of relationships between people in a specific ecological context. These relationships are defined by the ecological context (the same people would have different relationships in different contexts) and serve as both guide and context for individual activities. For example, some activities homeless youth engage in are influenced by relationships they develop in a street setting. Relationships in micro-systems are not unidirectional – individuals have choices in how they respond to influences and whether to even remain within a sphere of influence (an individual can exit a micro-system at any time, though circumstances can sometimes make this difficult).
A micro-system setting never exists within a vacuum and this is what makes attempting to change the dynamics of a particular micro-system so difficult. An individual’s relationships in every setting are impacted by relationships in other settings in that individual’s life. There is, in a sense, a chain of activity that individuals drag with them across micro-systems. For instance an individual’s choices of activity in a street setting might be highly impacted by relationships in their family setting or their school setting. Bronfenbrenner referred to this system of interlocking micro-systems as the meso-system (1979). It is the meso-system that truly sets the trajectory of individual activity. In the case of troubled adolescents, activities in various settings can take on a momentum creating a downward spiral leading not only to homelessness, but settings that create or perpetuate ancillary problems such as drug abuse and survival sex.
The critical question in the ecological/systems approach we have adopted is how to stop and somehow reverse the downward spiral of a troubled adolescent’s meso-system. How can we change the momentum of activity so it leads an individual to healthy and positive relationships and settings? There are two possibilities for changing the momentum of an individual’s activity: 1) change the settings in which individuals engage in everyday activities, and 2) change the way individuals respond to influences in particular settings (e.g., decision making).
Settings impact each other and have salience in an individual’s larger meso-system because of what Bronfenbrenner called linkages (1979). These linkages tie different microsystems together, providing the individual both the information and the motivation to move between settings, and apply the residue of activity in one setting to relationships in another setting. Linkages can also lead to new micro-systems (and micro-system activities) providing different impacts on ongoing relationships. The difficulty in dealing with a population such as homeless youth is the momentum of their activities creates linkages to deviant settings (McCarthy & Hagan, 1995). The introduction of these new deviant settings is more likely to increase the downward spiral of the over-all meso-system. An intervention needs to not only provide supportive, positive settings, but also through the activity it generates also create linkages – that both change the dynamics of relationships in existing settings and creates entry points in to new more positive settings.
One of the most efficient ways to create new types of activities that have impacts across settings is operant conditioning (Skinner, 1963). Reinforcements can, and should, not only change behavior but also – from an ecological perspective – offer linkages to new/different healthier, more positive settings. The linkages build on each other. What is important is that the activities of the individual take a new momentum so that the individual slowly pushes the meso-system in a more positive direction.
The focus of this treatment evaluation project is on homeless, street living youth who are not currently residing in runaway shelters. Substance abusing homeless youth were randomly assigned to either the operant-based Community Reinforcement Approach (CRA, Meyers & Smith, 1995) or treatment as usual (TAU) through a drop-in center (where youth can rest, receive food, and access showers, a washer/dryer and case management) and were evaluated at post-treatment. This research is a step towards identifying effective interventions designed specifically for homeless youth.
Hypotheses
Our primary hypothesis was that alcohol and drug use would show a statistically significant greater decrease for youth at post-treatment in CRA compared to treatment as usual. Our secondary hypotheses were that ancillary drug use measures and individual difference measures would show greater positive change for youth in CRA as compared to TAU.
Methods
Participants
All youth (N = 180) were engaged through the only drop-in center for homeless youth in Albuquerque. In order to be eligible for participation, youth were between the ages of 14–22, had been living in the metropolitan area for at least 3 months, with plans to remain for at least 6 months, met DSM-IV criteria for Alcohol or other Psychoactive Substance Use Disorders, as assessed by the computerized diagnostic interview schedule for children (CDISC, Shaffer, 1992), and met criteria for homelessness as defined by DHHS as “a situation in which a youth has no place of shelter and is in need of services and shelter where he or she can receive supervision and care” (Runaway and Homeless Youth Program/Title 45, 1999, p. 300).
Procedure
Recruitment
An RA engaged and screened youth at the drop-in center to determine basic eligibility for the study. Those eligible signed the consent statement, which was approved by our local IRB. The interviewer proceeded to administer the CDISC (Shaffer, 1992), sections on drugs, alcohol, and psychosis to determine formal eligibility. Those not passing inclusion criteria for the project during the diagnostic screening were not included in the project but continued to receive services provided through the drop-in center. Those meeting the criteria for participation in the study, continued with the assessment battery. Recruitment began on 11/2/01 and ended on 2/21/05. Youth were randomly assigned to either (1) CRA (N = 96) or (2) TAU, (N = 84), see below for randomization details. Youth assigned to the project intervention were offered 12 CRA therapy sessions and 4 HIV education/skills practice sessions. Intervention began following completion of the baseline assessment battery and randomization. No blinding of condition was used.
All adolescents were evaluated at 3 and 6 months after the baseline assessment. Although treatment was planned to be completed in 3 months, due to unstable life situations of youth, no-shows were common, making 6 months a more realistic timeframe to enable the most clients to complete therapy. Since the 3 month follow-up assessment became a mid-treatment evaluation, and this paper evaluates the impact of treatment on outcome, 6 month data was examined in the outcome analyses. Six month assessments were conducted from 5/30/02 to 9/26/05, and were typically completed in the drop-in center, although some follow-up assessments were completed in other locations (restaurants, parks, etc.) or by phone to facilitate completion. Research assistants (RAs), trained by the PI in all the assessment instruments, conducted all of the screening, intake and follow-up assessments.
The baseline and follow-up assessments, including the diagnostic battery, required approximately 2 hours to complete. Youth received a care package including blankets, toiletries and food items at the completion of the pre-treatment assessment and $50 at the completion of the follow-up assessment. Assistance in completing forms was provided as needed.
Intervention
Community Reinforcement Approach (CRA)
CRA procedures and session guidelines are detailed in Meyers and Smith (1995) and Godley et al.’s (2001) ACRA manual for the treatment of adolescent marijuana abusers. CRA uses an operant perspective that is based on the belief that environmental contingencies can play a powerful role in encouraging or discouraging behavior. Although CRA is based upon an operant theoretical perspective, it also integrates and conceptually links behavioral and cognitive intervention strategies to the ecological, multi-causal formulation of youth problem behaviors. CRA is multisystemic in that it directs intervention to intra- and interpersonal change as well as to social contexts that influence behavior. The following provides a brief description of the sequence/timing of the intervention and the session topics.
Session 1 was used to establish rapport and to provide a clear rationale for the CRA approach. Session 2 focused on a tentative treatment plan developed in active collaboration between the therapist and youth, using the Happiness Scales (Meyers & Smith, 1995) to help the youth identify areas of their life they want to examine more closely. Thus, the plan targeted areas of greatest need for the client: housing, medical care, job finding, social relations, psychiatric issues (depression, anxiety), and/or legal problems. For sessions 3-12, therapists followed CRA treatment strategies using both a standard set of core procedures and a menu of optional treatment modules matched to clients’ needs (Meyers & Smith, 1995). Role plays and homework assignments were incorporated into the sessions in order to generalize and practice newly learned skills. In addition, 4 sessions were offered that covered AIDS education and assessment of risk, risk reduction and skills practice. These sessions used strategies drawn from those used successfully by St. Lawrence, Kelly and their colleagues, Becoming a Responsible Teen (B.A.R.T.; Kelly, St. Lawrence, Hood, & Brasfield, 1989; St. Lawrence, Jefferson, O’Bannon, & Shirley, 1995).
Treatment sessions
For the CRA group, mean number of treatment sessions completed was 6.8 (SD = 5.5). Eighteen youth did not attend any treatment sessions.
Treatment as Usual
Youth who were not randomly assigned to CRA were assigned to the treatment as usual control condition through the drop-in center. The drop-in center offered a place to rest during the day, food, showers, clothing and case management that linked youth with community resources at the youth’s request. On average, youth in TAU reported attending 3.4 case management sessions offered by the drop-in center.
Materials
Demographic Measures
A demographic questionnaire designed to characterize and compare participants was administered.
Substance Use
The Form 90, developed for NIAAA funded Project Match (Miller & Del Boca, 1994), was the primary measure of quantity and frequency of drug and alcohol use. It has shown adequate test-retest reliability in major drug categories for adults (Tonigan, Miller & Brown, 1997) and runaway adolescents (Slesnick & Tonigan, 2004). Percent days of alcohol and drug use was the primary dependent measure used in this study. To address problem consequences associated with drug use, the Problem Oriented Screening Instrument for Teenagers (POSIT; Rahdert, 1991) was utilized.
Individual Problem Behaviors
The National Youth Survey Delinquency Scale (NYSDS) is a structured interview used as a measure of delinquent behavior which has displayed adequate test-retest and criterion validity (Elliot, Huizinga, & Ageton, 1985). The Youth Self-Report (YSR) of the parent-reported Child Behavior Checklist (CBCL; Achenbach & Edelbrock, 1982) is a 120-item scale which provides factor scores for internalizing, externalizing as well as total behavior problems. The measure is highly reliable and effectively discriminates between children referred to clinics for problem behavior and non-clinic children.
The adolescent version of the Coping Inventory for Stressful Situations (CISS; Endler & Parker, 1990) was used to measure youths’ coping. The CISS consists of 48 items and has been shown to be a valid multidimensional coping measure, and to have adequate construct validity with adolescent and clinical populations (Endler & Parker, 1990). The three factor analytically derived subscales were included as dependent measures: (1) task-oriented coping, (2) emotion-oriented coping, (2) avoidance-oriented coping.
Depressive symptoms were measured using the Beck Depression Inventory (BDI-II; Beck, Steer & Brown, 1996). The BDI-II is a 21-item self-report instrument for measuring depressive symptoms in adults and adolescents age 13 and above. Shaffer’s Computerized Diagnostic Interview Schedule for Children (CDISC, 1992) is a computerized instrument consisting of 263 items measuring the criteria for DSM IV diagnoses. It has demonstrated excellent interrater reliability of 97% with clinicians agreeing with the diagnosis of CDISC (Wolfe, Toro, & McCaskill, 1999).
The Health Risk Questionnaire incorporated items from the Health Risk Survey (Kann Nelson, Jones, & Kolbe, 1989) and the Homeless Youth Questionnaire (Johnson, Aschkenasy, Herbers, & Gillenwater 1996) which, together, address a wide range of HIV-attitudes, knowledge and risk behaviors.
Statistical Analyses
Initial analyses were conducted to examine the distributional characteristics of the variables of interest. Delinquency (from the NYSDS) was skewed due to some extremely high scores. To compensate for these scores, log transformations were conducted.1
To test for treatment differences, pre- to post-treatment analyses were conducted on all clients on the main variables of interest in two categories: substance use and individual functioning (see Table 2 for specific variables). Repeated measures ANOVAs were conducted for the two follow-up points (baseline and 6 month follow-up) with treatment modality as the between-subjects factor. RMANOVAs were chosen as statistical tests in order to test for both change over time, and the effect of modality, as well as the interaction between time and modality. Linear modeling was considered and discarded as using two time points would result in exactly the same analyses as RMANOVAs. The key effect sought was a statistical interaction between time and treatment. All analyses are intent to treat.
Table 2.
Means and Standard Deviations for Main Variables by Treatment Modality
| Baseline | 6 month follow-up | Time effect | Interaction effect | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | CRA | TAU | CRA | TAU | F | p | d | F | p | d |
| Substance Use: | ||||||||||
| % days alcohol and drug use § | 67 (33) | 60 (34) | 43 (37) | 50 (36) | 37.42 | < .001 | 1.00 | 5.39 | < .05 | .35 |
| # of categories of drugs used | 4.30 (1.83) | 4.04 (1.57) | 3.16 (1.99) | 3.19 (1.92) | 40.50 | < .001 | 1.03 | 0.83 | >.20 | .20 |
| Problem Consequences(POSIT) | 7.31 (5.01) | 6.66 (3.94) | 4.98 (4.88) | 4.92 (4.43) | 43.63 | < .001 | 1.06 | 0.94 | >.20 | .20 |
|
| ||||||||||
| Individual Functioning | ||||||||||
| Social Stability § | 40 (42) | 50 (51) | 68 (60) | 57 (52) | 10.98 | < .01 | 0.55 | 3.86 | = .05 | .35 |
| High-risk behaviors last 3 months (out of 7) | 0.77 (1.00) | 1.04 (0.94) | 0.73 (1.05) | 0.86 (0.76) | 1.92 | > .05 | 0.20 | 0.82 | >.20 | .20 |
| Depression (BDI ) § | 20.40 (10.68) | 16.80 (10.63) | 12.15 (11.10) | 13.00 (11.42) | 34.20 | < .001 | 0.94 | 4.67 | < .05 | .35 |
| CISS Task Scale | 54.22 (14.73) | 52.11 (13.68) | 56.63 (14.02) | 53.68 (12.65) | 2.89 | = .09 | 0.29 | 0.13 | >.20 | .00 |
| CISS Emotion Scale | 49.64 (13.93) | 46.07 (13.64) | 42.12 (14.29) | 42.11 (12.13) | 25.35 | < .001 | 0.81 | 2.44 | >.10 | .29 |
| CISS Avoidance Scale | 52.03 (11.81) | 49.61 (11.52) | 50.48 (10.82) | 47.35 (13.00) | 3.48 | = .06 | 0.29 | 0.12 | >.20 | .00 |
| Internalizing (YSR) § | 22.93 (10.53) | 20.19 (9.23) | 15.89 (10.25) | 16.78 (8.72) | 47.48 | < .001 | 1.12 | 5.99 | < .05 | .41 |
| Externalizing (YSR) | 22.94 (10.01) | 23.32 (8.54) | 17.85 (9.26) | 19.06 (7.99) | 30.12 | < .001 | 0.91 | 0.32 | >.20 | .00 |
| Delinquent behaviors (NYSDS total) 1 | 88.63 (161.49) | 88.68 (97.65) | 99.19 (219.83) | 58.71 (99.94) | 24.40 | < .001 | 0.81 | 3.02 | =.08 | .29 |
Note. Time by Modality interactions; see text for statistics for significant interactions, based on N = 155, CRA: N = 81, TAU: N = 74
Transformed scores for delinquency were used in the analyses and are: CRA pretx: 2.87 (2.06); TAU pretx: 3.54 (1.78); CRA 6mfu: 2.27 (2.34); TAU 6mfu: 2.26 (2.16).
Primary and Secondary Measures
Our primary measure was the percent days of use (drugs and alcohol combined). Our secondary measures included other measures of drug use and individual difference measures that we believed would also be important in a homeless youth’s life (see Table 2 for a list of these measures).
Results
Youth were 19.21 years (SD = 2.14), with 118 (66%) males and 62 (34%) females recruited. Self-identified ethnicity of the youth was Native American (24, 13%), Asian (1, 1%), African American (6, 3%), Hispanic (54, 30%), Anglo (73, 41%), and mixed ethnicity/race (22, 12%). At baseline, only 39% reported accessing any type of shelter or mission for services within the prior 3 months. Please see Table 1 for a summary of sample characteristics. T-tests or χ-square analyses (as appropriate) were used to test for potential baseline differences between modality groups. Treatment groups did not differ in any demographic characteristics except for number of other substance use diagnoses (see Table 1). No differences were found for any of the other main variables (substance use, individual differences), indicating that the treatment groups were relatively equal in baseline performance (all p’s > .10).
Table 1.
Demographic characteristics by treatment modality at baseline.
| Variable | CRA (N = 96) | TAU (N = 84) | Total (N = 180) | Statistical test | |
|---|---|---|---|---|---|
| Age | 19.03 (2.45) | 19.40 (1.73) | 19.21 (2.15) | t (178) = 1.17 | |
| Gender (#, % Male) | 61, 64% | 57, 68% | 118, 66% | χ2 (1) = 0.37 | |
| Ethnicity (#,%) | Anglo | 43, 45% | 30, 36% | 73, 41% | χ2 (5) = 6.23 |
| Hispanic | 29, 30% | 25, 30% | 54, 30% | ||
| Native Am | 8, 8% | 16, 19% | 24, 13% | ||
| African Am | 3, 3% | 3, 4% | 6, 3% | ||
| Asian | 0, 0% | 1, 1% | 1, 1% | ||
| Other | 13, 14% | 9, 11% | 22, 12% | ||
| Percent days housed | 19 (32) | 20 (30) | 19 (31) | t (178) = -0.17 | |
| Percent days use of alcohol or drugs | 67 (32) | 60 (34) | 64 (33) | t (178) = 1.25 | |
| IV drug Use (#, %) | 25, 26% | 17, 20% | 42, 23% | χ2 (1) = 0.84 | |
| Alcohol Diagnosis 1 | 66 (71%) | 55 (70%) | 121 (70%) | χ2 (1) = 0.04 | |
| Marijuana Diagnosis 1 | 83 (89%) | 64 (81%) | 147 (85%) | χ2 (1) = 2.33 | |
| Other Substance Use Diagnosis 1 | 38 (41%) | 46 (58%) | 84 (49%) | χ2 (1) = 5.16 | |
| # Arrests | 6.09 (10.43) | 9.10 (18.60) | 7.49 (14.84) | t (178) = -1.36 | |
| Currently enrolled in school (#, %) | 13, 14% | 8, 10% | 21, 12% | χ2 (1) = 0.70 | |
Note. Means (Standard deviations) unless otherwise specified
Number (percent) positive diagnoses of Abuse or Dependence from CDISC (Shaffer, 1992)
Randomization procedures
Participants were randomized using a computerized urn randomization procedure, which has been used successfully in prior clinical studies to ensure baseline group equivalence (e.g., Project MATCH, 1993). Non-equivalent groups can emerge by chance especially given small samples. The urn procedure retains random allocation and balances groups on a priori continuous and categorical variables. The relative probabilities of assignment to treatment groups (urns) are computer adjusted based on previous randomizations to reduce the risk of nonequivalent groups and removes potential experimenter biases by completely computerizing the randomization process. The variables included in the urn were: gender, age, ethnicity, number of days homeless, number of days substance abuse, and IV drug use. None of the urn variables differed between treatment groups (all p’s > .20; see Table 1). Randomization was done following the completion of the intake assessment by the project PI and the youth’s group assignment was then communicated to the project staff (RAs and therapists).
Therapist Training and Supervision
Therapist training included reading Meyers and Smith (1995) and Godley et al.’s (2001) ACRA manual for the treatment of adolescent marijuana abusers, a two-day didactic and role-play seminar, and on-going weekly supervision done in groups with all therapists in attendance. Audiotape recordings of therapy sessions were used for treatment adherence checks, fidelity monitoring, and supervision. Selected portions of audiotapes were reviewed, feedback was provided and problems were discussed. Problems included further instruction on how and when to apply CRA techniques and how to find and use the clients’ “reinforcers” to increase positive behavior change.
Four therapists conducted the majority (77%) of the CRA therapy intervention. These therapists were master’s level female licensed professional counselors ranging in age from 26 to 47 with 2-12 years experience in the field. Therapist differences were investigated among these four therapists. Two therapists completed more therapy sessions than the other two therapists (completing 7.05 and 7.58 sessions on average as compared to 3.00 and 4.58 sessions on average), although the difference only showed a statistical trend toward significance (F (3, 71) = 2.37, p = .078). Further, an interaction between therapist and time was found for percentage of days of substance use, with two therapists showing an overall decrease in substance use in their clients, while one therapist showed no decrease and one therapist showed a trend towards a decrease (overall F (3, 59) = 3.59, p < .05; using repeated measures ANOVAs).
Treatment Fidelity
Two coders rated a portion (10%) of the audiotapes. Codes were of two parts for 9 different treatment procedures: the occurrence (yes/no) of the procedure during the session, then how well it was done by the therapist (1 “very poorly” to 7 “exceptional” scale). Coder reliability for procedure occurrence was Kappa = .71, while the coder reliability of the procedure rating was ICC = .78. We had good therapist adherence with an average procedure rating of 4.5 which was in the “average” to “well” range. The average number of procedures used during a session was 4.5 (range 1 to 7 out of a possible 9 procedures).
Intent to Treat Outcome Analyses
For outcome analyses, repeated measures analyses were conducted with treatment modality as the between-subjects factor. The key effect sought was an interaction between time and modality, which would show support for our hypothesis. Eighty-one (84%) subjects assigned to CRA completed the baseline and 6 month follow-up assessment, and 74 (88%) TAU subjects completed the baseline and 6 month follow-up assessments.
One-hundred and fifty-five youth completed both the baseline and 6 month follow-up assessment. However, 25 youth missed one or more assessments. It was of some concern that these youth that did not complete all assessments differed in some fundamental way from those youth who did complete all the assessments. We found that these two groups of youth did differ at baseline for alcohol abuse, marijuana dependence, and HIV risk for the past three months. Those youth who completed all assessments had a greater prevalence of marijuana dependence (not completed: 33%, completed: 68%; χ2 (1) = 10.36, p < .01) and lower prevalence of alcohol abuse (not completed: 33%, completed: 15%; χ2 (1) = 4.89, p < .05). Those who completed all assessments had a lower HIV risk score for the past 3 month period than those who did not complete each assessment interview (not completed: 1.42 (1.21) completed: 0.89 (0.98), F (1, 178) = 5.59, p < .05).
Interaction Effects
Substance Use
An interaction was found between percent days of drug use (excluding tobacco) and treatment condition, which showed a differential impact for the two groups (F (1, 153) = 5.39, p < .05; d = .35; see Figure 1; Table 2). Testing simple main effects (SME) as follow-up analyses, youth in CRA had a greater decrease (F (1, 153) = 37.29, p < .001; d = 1.00) in drug use than youth in TAU (F (1, 153) = 6.89, p < .05; d = .41).
Figure 1.
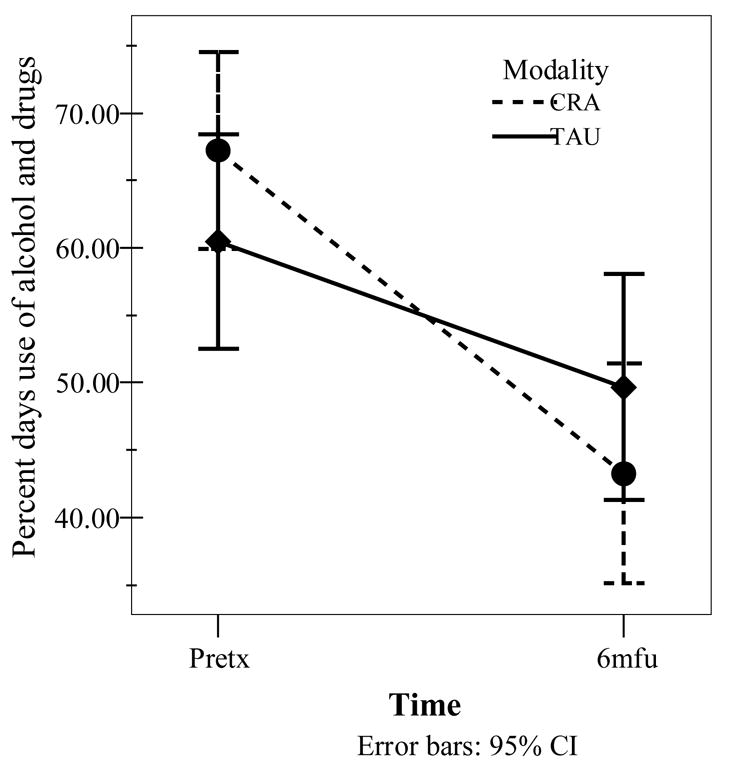
Significant interaction between time and modality for percent days of alcohol and drug use (all classes excluding tobacco).
Individual Functioning
An interaction was found between depression (as measured by the BDI) and treatment condition, which showed a differential impact for the two groups (F (1, 153) = 4.67, p < .05; d = .35). SME tests showed that youth in CRA had a greater decrease (F (1, 153) = 33.58, p < .001; d = .94) than youth in TAU (F (1, 153) = 6.51, p < .05; d = .41). Further, an interaction was found between internalizing behaviors (YSR) and treatment condition (F (1, 153) = 5.73, p < .05; d = .41). SME tests showed that youth in CRA showed a greater decrease (F (1, 153) = 45.67, p < .001; d = 1.09) than youth in TAU (F (1, 153) = 9.69, p < .01; d = .51).
Social stability was measured by the percent days in the period of work, education, being housed, and seen for medical care, as assessed on the Form 90. The social stability score had an interaction between time and treatment condition (F (1, 153) = 3.86, p = .05; d = .35), with follow-up analyses showing that youth in CRA had a greater increase in social stability (F (1, 153) = 14.59, p < .001; d = .63) than did youth in TAU (F (1, 153) = 0.87, p > .20; d = .20). See Table 2 for details.
Time Effects
Overall, both groups got better on many different areas of functioning (main effect of time), including drug use measures (percent days use (except tobacco), percent days illegal drug use, percent days hard drug use, number of categories of drugs used, number of problem consequences) and individual functioning measures (BDI and YSR), coping skills (emotion and task-oriented), internalizing and externalizing problems, and delinquent behaviors. See Table 2 for more details.
Moderational Analyses
To examine differences in treatment, moderational analyses were conducted using repeated measures ANOVAs, with age, gender and ethnicity used as an additional between subject variable (Baron & Kenny, 1986).
Age was submitted to a median split to enable repeated measures analyses. Ages through 19 were one group while ages 20 and older were a second group. The younger group’s mean age was 17.61 (SD = 1.59), while the older group’s mean age was 21.02 (SD = 0.86). Age moderated treatment outcome, but only for depression (F (1, 151) = 3.80, p = .05; d = .35; see Figure 2). Both CRA age groups showed a significant decrease in depression over time (younger: F (1, 151) = 11.53, p = .001, d = .59; older: F (1, 151) = 24.48, p < .001, d = .81). For the TAU group, only younger youth showed a decrease in depression (F (1, 151) = 7.91, p < .01, d = .46), while older youth in TAU did not (F (1, 151) = 0.46, p > .20, d = .00).
Figure 2.
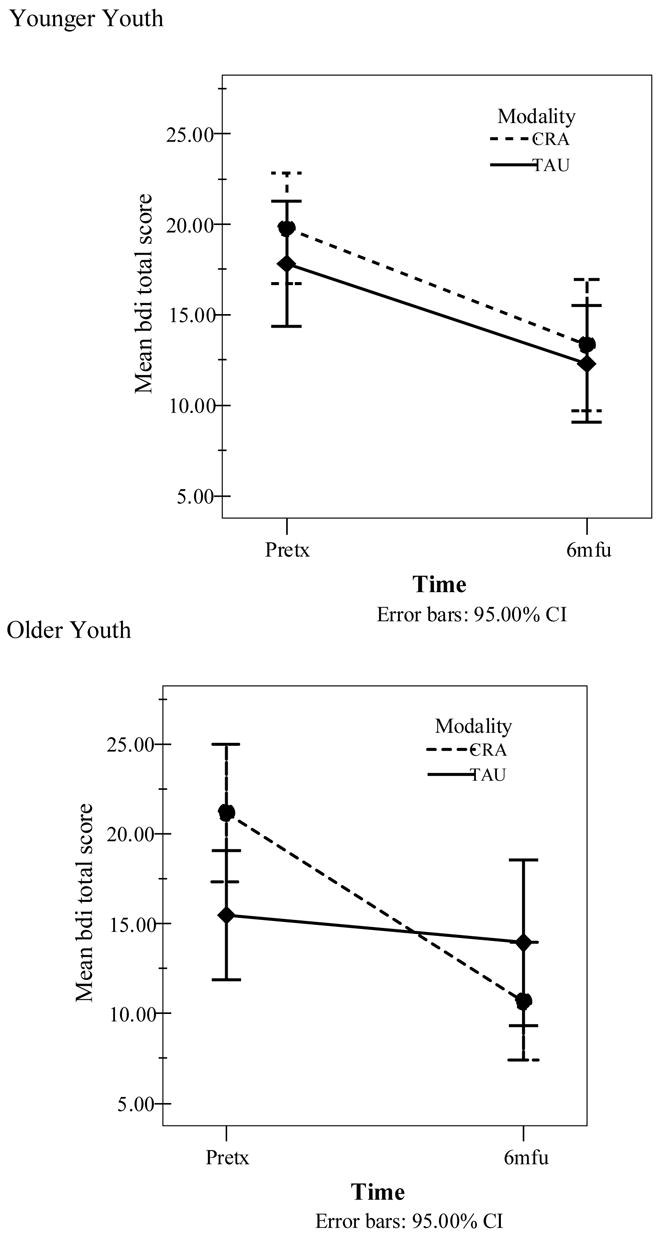
Moderational effect of age on depression (BDI).
Discussion
Few empirically supported treatments for street living youth are available. Many logistical, treatment and research barriers impede evaluation. For example, participant barriers include transportation and accessibility to the treatment research site, engagement, development of trust, and tracking for follow-up. Social barriers in treating youth include the provision of housing and psychiatric services for minors who refuse to have parents contacted or social service system involvement. In the current study, the Community Reinforcement Approach was evaluated and compared to treatment as usual through a homeless youth drop-in center.
Results showed that CRA is an efficacious intervention, as youth improved in many domains. As hypothesized, street living youth assigned to CRA showed statistically significant greater improvement in substance use, social stability and depression/internalizing problems compared to those assigned to TAU. Treatment findings did not differ depending upon age, gender or ethnicity with the exception that older youth assigned to TAU did not report reductions in BDI depression while younger youth reported improvement in depression. Possibly, older youth, who may have a longer history of homelessness and depressive symptoms, require a greater focus on coping, mood management, and others skills development as offered in CRA. Overall, many youth were engaged into treatment and responded positively to the intervention. This is significant in that engagement and maintenance of homeless youth in ongoing treatment efforts can be difficult (Smart & Ogborne, 1994). Our findings suggest that an open door policy, engagement of youth slowly and without pressure through a drop-in center, and employing charismatic, informed therapists can contribute to effective engagement and maintenance of these youth in treatment.
In regard to clinical significance, youth who received CRA were improved but not recovered. For example, youth in CRA showed a 37% reduction in substance use (from 67% days use to 43% days use), while those receiving TAU showed a 17% reduction in substance use (60% to 50% days use). Given the reduction in BDI depression (40% v. 23%) and increase in social stability (58% v. 13%) among those in CRA relative to TAU, the potential for intervention and improving outcomes among these youth is promising. However, this study provides a very small step towards understanding the treatment needs and responses of these youth to treatment; much more treatment development research is needed to address the difficult life situation of these youth.
In summary, youth assigned to CRA showed greater improvement in some areas compared to TAU, but those receiving TAU also improved in several domains. All youth received assistance in meeting basic needs, and this could account for some of the observed improvements. Involvement of youth with a system in which adults provide positive, reinforcing experiences (received in both CRA and TAU) is likely integral to change. Both CRA and TAU provide youth with experiences consistent with the underlying theoretical assumptions of the developmental systems approach (Bronfenbrenner, 1979). CRA and TAU provide one of the first times in the youth’s life that they are being reinforced for positive behavior. This fundamentally changes the youth’s relationship with a social system. The positive reinforcement for positive behavior places the homeless youth on a positive developmental trajectory that breaks negative interactional continuity and can be built upon, allowing for the possibility of further linkages to positive micro-systems. For example, if a youth requests assistance with obtaining a job and the therapist assists the youth in achieving this goal, the youth will see this as a positive linkage. The experience not only offers the opportunity of making the drop-in a part of the youth’s meso-system but increases the possibilities of the youth making similar linkages to other positive micro-systems such as one that offers medical assistance.
Thus, we believe that the Community Reinforcement Approach (CRA) therapy has the potential to impact homeless youth over the long term. This method of intervention attempts to change the relationship between homeless youth and their micro-systems and meso-systems. It is important to point out that the second intervention, the treatment as usual, also offers weak linkages to healthier settings. But because it is not focused on the larger ecological circumstances of the individual youth, this type of intervention is held hostage to influences in other parts of the youth’s meso-system. The TAU intervention’s effects are haphazard rather than purposeful and focused.
The research design is limited in that youth were only assessed at post-treatment. A longer follow-up is needed to determine stability of treatment effects. The design does not allow determination of whether CRA is more or less effective than other intervention approaches for treating substance abusing homeless youth. Also, all youth were recruited as a sample of convenience through a drop-in center. These youth might be more amenable to change, have greater trust or respond differently to treatment efforts than youth who do not access drop-in centers. Also, youth in other parts of the country who experience different stressors or community supports might respond differently to the treatment efforts examined in this project. The drop-in center from which youth were recruited was the only drop-in center designed to serve homeless youth in the state, and features of this center may have affected the findings. The drop-in center likely included activities, staff attributes and other features that were particular only to that drop-in center, and may not be representative of other drop-in centers. Since RA’s were not blinded to the treatment condition that youth were assigned, knowledge of the youth’s treatment condition may have affected the administration of the follow-up assessments and thus the data. However, without such blinding and assistance from the therapists or case managers in tracking youth, the follow-up rate would likely have suffered significantly. Moreover, youth were aware of the possible treatment conditions, and youth who were unhappy with their treatment condition may have biased the outcomes. Youth who did not complete each assessment interview reported significantly higher HIV risk behaviors and higher alcohol use frequency compared to those who completed each assessment interview. Thus, given that some of these higher risk youth were missed, the findings might over or underestimate the impact of CRA overall.
While development of psychosocial interventions is important, and much more research in this area is needed, substance use, health risks and associated mental health problems will likely continue until the youth is removed from the streets. Our goal in this treatment was to remove youth from the streets, but we were limited in achieving this goal. These youth, and especially minors, are unable to sign for housing without a guardian’s consent and refuse foster care. Older youth are often unable to acquire housing because of other barriers including financial, behavioral/emotional and social prejudice. It is difficult for youth to maintain housing and employment with an active drug addiction and mental health problem, and it is difficult for youth to address substance use and related problems without social stability. Future research will need to consider social barriers when designing and evaluating treatments for this population.
Footnotes
Using a log transform for the NYSDS scores adjusted the skewed scores to be within more normal distribution. The untransformed scores had a skewness of 3.22 and 3.59 and kurtosis of 14.68 and 14.34 for each of the assessment points (intake, 6mfu). The transformed scores skewness was -0.30 and 0.45 and kurtosis was -1.11 and -1.30 for each of the assessment points (intake, 6mfu).
Using an inverse transformation of the use of hard drugs variables made the scores more normally distributed. The untransformed scores had a skewness of 1.82 and 3.02 and kurtosis of 2.49 and 8.65 for each of the assessment points (intake, 6mfu). The transformed scores skewness was 0.42 and 0.42 and kurtosis was -1.51 and -1.78 for each of the assessment points (intake, 6mfu).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Child Behavior Profile. Burlington, VT: Child Psychiatry, University of Vermont; 1982. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Arlington, VA: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Baer JS, Ginzler JA, Peterson PL. DSM-IV alcohol and substance abuse and dependence in homeless youth. Journal of Studies on Alcohol. 2003;64(1):5–15. doi: 10.15288/jsa.2003.64.5. [DOI] [PubMed] [Google Scholar]
- Bailey SL, Camlin CS, Ennett ST. Substance use and risky sexual behavior among homeless and runaway youth. Journal of Adolescent Health. 1998;23:378–388. doi: 10.1016/s1054-139x(98)00033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory of moral thought and action. In: Kurtines WM, Gewirtz JL, editors. Handbook of moral behavior and development. Vol. 1. Hillsdale, NJ: Lawrence Erlbaum; 1991. pp. 45–103. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II, Beck Depression Inventory: Manual. 2. Boston, MA: Harcourt Brace; 1996. [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Cauce AM, Morgan CJ, Wagner V, Moore E, Sy J, Wurzbacher K, et al. Effectiveness of intensive case management for homeless adolescents: Results of a 3-month follow-up. Journal of Emotional and Behavioral Disorders. 1994;2:219–227. [Google Scholar]
- Cauce AM, Paradise M, Ginzler JA, Embry L, Morgan CJ, Lohr Y, et al. The characteristics and mental health of homeless adolescents: Age and gender differences. Journal of Emotion and Behavioral Disorders. 2000;8(4):230–239. [Google Scholar]
- Chamberlain C, MacKenzie D. Australian Housing and Urban Research Institute. 2004. Youth homelessness: Four policy proposals. Final Report. [Google Scholar]
- Clements K, Gleghorn A, Garcia D, Katz M, Marx R. A risk profile of street youth in northern California: Implications for gender-specific human immunodeficiency virus prevention. Journal of Adolescent Health. 1997;20:343–353. doi: 10.1016/S1054-139X(97)00033-5. [DOI] [PubMed] [Google Scholar]
- Elliot DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills, CA: Sage; 1985. [Google Scholar]
- Endler NS, Parker JDA. Coping Inventory for Stressful Situations (CISS): Manual. Toronto: Multi-Health Systems; 1990. [Google Scholar]
- Ennett ST, Federman EB, Bailey SL, Ringwalt CL, Hubbard ML. HIV-risk behaviors associated with homelessness characteristics in youth. Journal of Adolescent Health. 1999;25(5):344–53. doi: 10.1016/s1054-139x(99)00043-9. [DOI] [PubMed] [Google Scholar]
- Godley SH, Meyers RJ, Smith JE, Karvinen T, Titus JC, Godley MD, et al. The Adolescent Community Reinforcement Approach for Adolescent Cannabis Users. DHHS Publication No. (SMA) 01–3489 2001 [Google Scholar]
- Johnson TP, Aschkenasy JR, Herbers MR, Gillenwater SA. Self-reported risk factors for AIDS among homeless youth. AIDS Education and Prevention. 1996;8:308–322. [PubMed] [Google Scholar]
- Kann L, Nelson GD, Jones JT, Kolbe LJ. Establishing a system of complementary school-based surveys to annually assess HIV-related knowledge, beliefs, and behaviors among adolescents. Journal of School Health. 1989;59:55–58. doi: 10.1111/j.1746-1561.1989.tb05392.x. [DOI] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Hood HV, Brasfield TL. Behavioral intervention to reduce AIDS risk activities. Journal of Consulting and Clinical Psychology. 1989;57:60–67. doi: 10.1037//0022-006x.57.1.60. [DOI] [PubMed] [Google Scholar]
- Kipke MD, Montgomery SB, Simon TR, Iverson EF. Substance abuse disorders among runaways and homeless youth. Substance Use and Misuse. 1997;32:969–986. doi: 10.3109/10826089709055866. [DOI] [PubMed] [Google Scholar]
- Marshall EJ, Bhugra D. Services for the mentally ill homeless. In: Bhugra D, editor. Studies in social and community psychiatry. Cambridge: Cambridge Univ. Press; 1996. pp. 99–109. [Google Scholar]
- McCarthy B, Hagan J. Getting into street crime: The structure and process of criminal embeddedness. Social Science Research. 1995;24:63–95. [Google Scholar]
- Meyers RJ, Smith JE. Clinical guide to alcohol treatment: The Community Reinforcement Approach. New York: Guilford Press; 1995. [Google Scholar]
- Miller WR, DelBoca FK. Measurement of drinking behavior using the Form-90 family of instruments. Journal of Studies on Alcohol. 1994;2(Supplement No 1):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Shade SB, Kral AH, Booth RE, Watters JK. Suicidal behavior and sexual/physical abuse among street youth. Child Abuse & Neglect. 1998;22:213–222. doi: 10.1016/s0145-2134(97)00137-3. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group; National Institute on Alcohol Abuse and Alcoholism. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical and Experimental Research. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Rahdert E, editor. DHHS Publication No. (ADM) 91–1735. Rockville, MD: National Institute on Drug Abuse; 1991. The Adolescent Assessment and Referral System Manual. [Google Scholar]
- Rew L, Taylor-Seehafer M, Fitzgerald ML. Sexual abuse, alcohol and other drug use, and suicidal behaviors in homeless adolescents. Issues in Comprehensive Pediatric Nursing. 2001;24(4):225–40. doi: 10.1080/014608601753260326. [DOI] [PubMed] [Google Scholar]
- Runaway and Homeless Youth Program (Title 45), 4 C.F.R. pt. 1351 (1999).
- Shaffer D. The Diagnostic Interview Schedule for Children – 2.3 Version. New York: Columbia University; 1992. [Google Scholar]
- Shane PG. What about America’s homeless children? Hide and seek. Thousand Oaks, CA: Sage Publications, Inc; 1996. [Google Scholar]
- Skinner BF. Operant Behavior. American Psychologist. 1963;18(7):503–515. [Google Scholar]
- Slesnick N, Prestopnik JL. Ecologically-based family therapy outcome with substance abusing runaway adolescents. The Journal of Adolescence. 2005;28:277–298. doi: 10.1016/j.adolescence.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of alcohol and other drugs used by runaway youths: A test-retest study of the Form 90. Alcoholism Treatment Quarterly. 2004;22(2):21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart RG, Ogborne AC. Street youth in substance abuse treatment: Characteristics and treatment compliance. Adolescence. 1994;29:733–745. [PubMed] [Google Scholar]
- Smith JE, Meyers RJ, Delaney HD. The community reinforcement approach with homeless alcohol dependant individuals. Journal of Consulting and Clinical Psychology. 1998;66:541–548. doi: 10.1037//0022-006x.66.3.541. [DOI] [PubMed] [Google Scholar]
- St Lawrence JS, Jefferson KW, O’Bannon RE, Shirley A. Cognitive-behavioral intervention to reduce African American adolescents’ risk for HIV infection. Journal of Consulting and Clinical Psychology. 1995;63:221–237. doi: 10.1037//0022-006x.63.2.221. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Wolfe SM, Toro PA, McCaskill PA. A comparison of homeless and matched housed adolescents on family environment variables. Journal of Research on Adolescence. 1999;9:53–66. [Google Scholar]


