Abstract
An activating 1849G>T mutation of JAK2 (Janus kinase 2) tyrosine kinase was recently described in chronic myeloproliferative disorders (MPDs). Its role in other hematologic neoplasms is unclear. We developed a quantitative pyrosequencing assay and analyzed 374 samples of hematologic neoplasms. The mutation was frequent in polycythemia vera (PV) (86%) and myelofibrosis (95%) but less prevalent in acute myeloid leukemia (AML) with an antecedent PV or myelofibrosis (5 [36%] of 14 patients). JAK2 mutation was also detected in 3 (19%) of 16 patients with Philadelphia-chromosome (Ph)–negative chronic myelogenous leukemia (CML), 2 (18%) of 11 patients with megakaryocytic AML, 7 (13%) of 52 patients with chronic myelomonocytic leukemia, and 1 (1%) of 68 patients with myelodysplastic syndromes. No mutation was found in Ph+CML (99 patients), AML M0-M6 (28 patients), or acute lymphoblastic leukemia (20 patients). We conclude that the JAK2 1849G>T mutation is common in Ph– MPD but not critical for transformation to the acute phase of these diseases and that it is generally rare in aggressive leukemias.
Introduction
Janus kinase 2 (JAK2) is a tyrosine kinase involved in the transduction of cellular growth stimuli.1,2 Chromosomal translocations resulting in fusions deregulating JAK2 activity are implicated in leukemias.3-5 A somatic activating mutation, 1849G>T (Val617Phe), in the JAK2 gene was recently described in most patients with polycythemia vera (PV) and in approximately half those with essential thrombocythemia (ET) and myelofibrosis (MF).6-10 Mutation of both JAK2 alleles has been reported in approximately 30% of the patients.6-10 It has been proposed that wild-type JAK2 suppresses the transformation properties of mutant JAK2, providing a selective advantage to loss of heterozygosity at this locus.6 PV can progress to MF and to acute myelogenous leukemia (AML),11 and MF can also progress to AML.12 The role of JAK2 mutations in the transformation of myeloproliferative disorders to acute leukemia and in de novo acute leukemias, as well as in other hematologic malignancies, remains unclear. Infrequent occurrence of this unique JAK2 mutation has been reported recently in chronic myelomonocytic leukemia (CMML), atypical or unclassified myeloproliferative disorder (MPD), myelodysplastic syndrome (MDS), systemic mastocytosis, and chronic neutrophilic leukemia.13,14
Pyrosequencing is a rapid and quantitative technique suitable for detecting single nucleotide polymorphisms.15 We developed a pyrosequencing assay for the detection of the JAK2 1849G>T mutation in leukocyte genomic DNA and studied its prevalence in MPD and other hematologic malignancies.
Study design
Patient samples
Samples were obtained from peripheral blood (n = 330) or bone marrow cells (n = 9) stored in a tissue bank in the Leukemia Department at M.D. Anderson Cancer Center and from Baylor College of Medicine. All patients gave consent for donation of samples to the tissue bank, in accordance with policies at the M.D. Anderson Cancer Center and Baylor College of Medicine. In 35 samples, DNA was extracted from paraffin-embedded diagnostic bone marrow biopsy specimens by heating paraffin slices at 100°C for 20 minutes in the solution containing 2% sodium dodecyl sulfate and 25 mM EDTA (ethylenediaminetetraacetic acid), followed by digestion at 50°C with proteinase K. Protein was removed by precipitation with 0.33 vol of 10 M ammonium acetate and centrifugation. DNA was recovered from the supernatant by alcohol precipitation.
Pyrosequencing
We developed 2 independent assays to detect the 1849G>T JAK2 mutation on the sense and antisense DNA strands. Exon 12 of JAK2 was amplified by polymerase chain reaction (PCR) from genomic DNA by primers JAK200F 5′-GCAGAGAGAATTTTCTGAACTAT and JAK200Rbio 5′biotin-CTCTGAGAAAGGCATTAGAAAG for the sense assay and JAK115Fbio 5′biotin-GCAGCAAGTATGATGAGCA and JAK115R 5′-CTCTGAGAAAGGCATTAGAAAG for the antisense assay. After PCR, the biotinylated strand was captured on streptavidin Sepharose beads (Amersham Biosciences, Uppsala, Sweden) and annealed with the sequencing primers JAK200S 5′-GGTTTTAAATTATGGAGTATGT for the sense strand and JAK115S 5′-TCTCGTCTCCACAGA for the antisense strand. Pyrosequencing was performed separately for the sense and antisense strands using PSQ HS 96 Gold SNP Reagents and the PSQ HS 96 pyrosequencing machine (Biotage, Uppsala, Sweden). The protocol for sample preparation and pyrosequencing is described in detail by Jones et al.14
Statistical analysis
The correlation between the pyrosequencing assays detecting the 1849G>T mutation on the sense and antisense strands and the linearity of the assays were assessed by linear regression analysis. Differences in clinical parameters between the groups of patients with or without the mutation were analyzed by parametric or nonparametric t tests.
Results and discussion
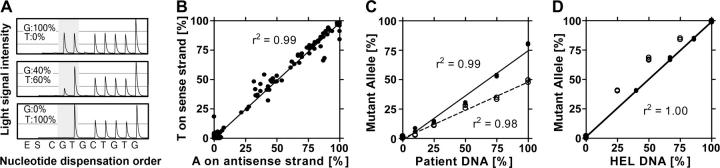
JAK2 1849G>T mutation status was analyzed by 2 independent pyrosequencing assays in 374 samples of patients with hematologic neoplasms, 21 leukemic cell lines, and 40 healthy controls. Examples of pyrograms are shown in Figure 1A. We observed a nearly perfect correlation of the results from the pyrosequencing assays on the sense and antisense DNA strands (Figure 1B), confirming the accuracy and reproducibility (r2 = 0.99; P < .001) of the method. To examine the linearity of the assay, we performed titrations by mixing DNA from healthy controls with DNA from patients with 50% or 80% of mutant allele, respectively. DNA mixes containing different ratios of healthy control and patient DNA were amplified by PCR and analyzed by pyrosequencing. Figure 1C demonstrates a linear relationship between the content of patient DNA and the quantity of mutant allele detected by pyrosequencing (r2 = 0.99). The experiments suggested the lower detection limit of 5% to 10% mutant allele.
Figure 1.
Pyrosequencing assay for detection of 1849G>T JAK2 mutation. (A) Examples of pyrosequencing results. The sequence read is (G/T)TCTGTGG. The mutation site with the adjacent T nucleotide is shaded. Peak heights are proportional to the amount of nucleotide present in the sequenced DNA. (top panel) Results from healthy control showing equal heights of the 1849G and the following T peak. The last peak is of double height, reflecting 2 adjacent G nucleotides. (middle panel) Ph–CML, with the normal G allele constituting 40% and the mutant T allele 60% of the total amplified DNA. (bottom panel) HEL cell line showing 0% of normal G allele and 100% of mutant T allele. The height of the T peak is 200% (100% from the mutant allele and 100% from the adjacent T allele). (B) Reproducibility of quantitative analysis of the JAK2 mutation. Two independent PCR and pyrosequencing reactions were performed to quantify the presence of A on the antisense strand (x-axis) and T on the sense strand (y-axis). Correlation between the assays was nearly perfect (r2 = 0.99). (C) Titration experiments showed linearity of the pyrosequencing assay. Healthy control DNA was mixed with 10%, 25%, 50%, and 75% DNA from a patient with MF carrying 50% of the mutant allele (○, broken line) or from a patient with PV whose DNA contained 80% of the mutant allele (•, solid line). Linear regression showed slopes of 0.47 and 0.77 and correlation coefficients (r2) of 0.98 and 0.99, respectively. (D) JAK2 gene is amplified in HEL erythroleukemic cell line. Healthy control DNA mixed with 25%, 50%, and 75% HEL DNA showed 40%, 67%, and 85% of mutant allele (○), indicating that the HEL cell line carries 4 mutant alleles and no normal allele. After correction for copy number, the dilution experiment showed a straight line (•, solid line).
Our analysis of various hematologic malignancies confirmed the high prevalence of JAK2 mutation in PV (25 [86%] of 29 patients), MF (18 [95%] of 19 patients), and ET (3 [30%] of 10 patients). We next analyzed the role of the JAK2 mutation in the progression of these disorders to AML. In 22 AML patients with preexisting PV, ET, or MF, 12 (55%) had the JAK2 mutation. This prevalence of the JAK2 mutation was lower compared with that in all ET/PV/MF patients studied in whom the JAK2 mutation was present (46 [79%] of 58 patients). This difference was significant by the Fisher exact test (2-sided; P = .047). When broken into individual MPD diagnoses, the prevalence of the JAK2 mutation in 9 AML patients with antecedent PV was lower (5 [56%] of 9 patients) than in the total group of PV patients studied (25 [86%] of 29; P = .07). This difference was even more striking in patients with myelofibrosis. None of 5 AML patients with preceding myelofibrosis had the JAK2 mutation, whereas the mutation was present in 18 (95%) of 19 of our patients with myelofibrosis (P < .001). Interestingly, a reverse pattern was seen in patients with ET. A higher prevalence of the JAK2 mutation was observed in AML patients than in those with antecedent ET (7 [88%] of 8), whereas we found the mutation in only 3 of 10 ET patients studied. Remarkably, the age at diagnosis of AML with antecedent PV/ET/MF was significantly lower (P = .04; t test) in patients lacking the JAK2 mutation (median, 58 years; range, 40-73 years) than in patients carrying the mutation (median, 68 years; range, 57-82 years), suggesting a more aggressive disease in MF and PV patients without the JAK2 mutation. In these patients, there also was an 8-year difference in the median age at PV, ET, or MF diagnosis in patients without the JAK2 mutation (age, 50 years; range, 24-71 years) than in those with the mutation (age, 58 years; range, 41-68 years), but this difference was not significant (P = .15).
In 4 patients, we had access to samples at MPD and progression from the same patients. The mutation was present in PV and progression samples at approximately the same proportions as in mutant allele (32% and 71% at PV, compared with 49% and 74% at MF, and 0% and 85% at PV, compared with 0% and 85% in AML). These data suggest the deviation from the expected 50% and 100% results from contamination of the clonal cells by polyclonal cells not bearing the somatic JAK2 mutation (eg, T cells, stromal cells)16 and that the mutation occurs early in disease development. Overall, the data suggest the JAK2 1849G>T mutation is common in MPD but not critical for transformation to the acute phase of these diseases. Further studies in larger sets of patients and multivariate analysis for confounding factors are needed to confirm this observation.
No mutations were found in 99 patients with Philadelphia chromosome (Ph)–positive CML (including 55 patients with imatinib-resistant disease), AML M0-M5 (20 patients), erythroleukemia (8 patients), or ALL (20 patients), but 2 of 11 patients with megakaryocytic leukemia (AML M7) were positive for the 1849G>T JAK2 mutation. In Ph– CML, we found the mutation in 3 (19%) of 16 patients. In CMML, 7 (13%) of 52 patients had the mutation. In MDS, the mutation was found in only 1 of 68 patients. None of these patients had an antecedent history of PV or MF. Individual characteristics of the non–PV/ET/MF patients carrying the 1849G>T JAK2 mutation are summarized in Table 1.17,18 In 4 patients, the proportion of mutant allele was lower than 20%, suggesting the presence of minor populations of cells carrying the mutation. We confirmed the presence of the mutant allele in all these patients by cloning PCR products in a plasmid vector and pyrosequencing 50 clones for each patient. In 9 of 13 patients, the sample studied was obtained within 6 months of diagnosis, indicating that the abnormality was acquired early rather than at disease progression. Mutation status for N-RAS and K-RAS was available in 79 patients studied here. JAK2 mutation was found in none of 9 patients positive for RAS mutations, compared with 7 of 70 patients free of RAS mutations. This difference was not statistically significant.
Table 1.
Characteristics of patients with JAK2 mutations (other than PV/MF/ET)
| Diagnosis,*sex, and age, y | WBCs, × 109/L | Monocytes, × 109/L | Bone marrow megakaryocytes | Splenomegaly | Cytogenetics | Time from diagnosis, mo. | Quantity of JAK2 mutant allele, % | RAS mutations |
|---|---|---|---|---|---|---|---|---|
| CML Ph- | ||||||||
| M, 67 | 16.3 | 0.8 | Normal | No | 46XY | 0 | 5 | Negative |
| M, 70 | 12.4 | 0.2 | Hyperplasia | Yes | 46XY | 6 | 44 | ND |
| M, 70 | 29.7 | 1.1 | Hyperplasia | Yes | 46XY | 20 | 59 | Negative |
| CMML | ||||||||
| M, 73 | 39.1 | 7.4 | Hyperplasia | Yes | 46XY | 18 | 9 | Negative |
| M, 55 | 9.5 | 1.5 | Hyperdysplasia | No | 46XY | 0 | 36 | Negative |
| M, 70 | 61.3 | 9.2 | Hyperplasia | Yes | 46XY | 1 | 83 | ND |
| M, 73 | 16.1 | 2.4 | Hyperplasia | No | 46XY | 16 | 40 | ND |
| F, 73 | 22.1 | 5.3 | Hypoplasia | No | 46XX | 0 | 17 | ND |
| F, 68 | 26.6 | 4.5 | Normal | No | 46XX,-7,t(13;21)(q12;q22) | 0 | 48 | Developed later |
| F, 63 | 4.9 | 0.9 | Hyperplasia | Yes | 46,XX,i(X)(p10) | 1 | 47 | ND |
| AML M7 | ||||||||
| M, 52 | 4.0 | 0.1 | Blasts | No | 46XY,del(9)(q22) | 5 | 7 | Negative |
| F, 51 | 0.6 | 0.1 | Hyperdysplasia | Yes | Complex, includes +add(9)(p24) | 3 | 57 | ND |
| MDS-RAEB | ||||||||
| M, 63 | 65.8 | 3.9 | Hyperdysplasia | Yes | 46XY | 10 | 51 | Negative |
Finally, we analyzed 21 leukemia cell lines. We detected the mutation in only the HEL erythroleukemic cell line, as reported,8 and showed amplification of the mutant allele (Figure 1D). No mutation was found in 12 other myeloid (BV173, HL60, K562, K5MBR, KG1, KG1a, ML1, MV4:11, NB4, OCI-AML3, TF1, U937), 4 T-cell (CEM, Jurkat, MOLT4, TALL), or 3 B-cell lines (BJAB, Raji, RS4:11).
In summary, our results confirm previous reports on the prevalence of JAK2 mutations in PV, MF, ET, CMML, and MDS.6-10,13,14 Our data suggest that the JAK2 mutation is acquired early, indicating that other molecular events are required for progression. JAK2 mutation was found in a lower proportion of patients whose MF or PV progressed to AML, and the age of AML onset was 10 years lower in patients lacking the JAK2 mutation. This may indicate that patients with MF and PV but without the JAK2 mutation represent a subgroup with more aggressive disease or that AML developed from a different subpopulation of stem cells than did PV. JAK2 mutation is rare in other hematologic malignancies except CMML, Ph– CML, and megakaryocytic leukemia. Further studies of the clinical significance of the JAK2 mutation in these diseases will be of interest.
Prepublished online as Blood First Edition Paper, July 21, 2005; DOI 10.1182/blood-2005-05-1800.
Supported in part by the Leukemia SPORE grant P50CA100632 from the National Institutes of Health and by funds from the Physicians Referral Service at the University of Texas M.D. Anderson Cancer Center.
J.J. designed the study and performed research and data analysis and wrote the manuscript. Y.O. substantially participated in the research, analyzed clinical data, and participated in writing and editing the manuscript. V.G. performed JAK2 mutation analysis in CML patients. C.B.R. critically evaluated and provided bone marrow biopsy specimens. J.T. Prchal contributed to the manuscript concept, referred some patients, critically evaluated data, and participated in composing and editing the manuscript. S.V. contributed to the manuscript concept, referred patients, and critically evaluated data. M.B., E.E., and H.K. referred patients and critically evaluated data and the manuscript. J.P.J.I. designed the study, provided blood and bone marrow samples, analyzed and critically evaluated data, and wrote the manuscript.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
- 1.Witthuhn BA, Quelle FW, Silvennoinen O, et al. JAK2 associates with the erythropoietin receptor and is tyrosine phosphorylated and activated following stimulation with erythropoietin. Cell. 1993; 74: 227-236. [DOI] [PubMed] [Google Scholar]
- 2.Parganas E, Wang D, Stravopodis D, et al. Jak2 is essential for signaling through a variety of cytokine receptors. Cell. 1998;93: 385-395. [DOI] [PubMed] [Google Scholar]
- 3.Peeters P, Raynaud SD, Cools J, et al. Fusion of TEL, the ETS-variant gene 6 (ETV6), to the receptor-associated kinase JAK2 as a result of t(9; 12) in a lymphoid and t(9;15;12) in a myeloid leukemia. Blood. 1997;90: 2535-2540. [PubMed] [Google Scholar]
- 4.Nunez CA, Zipf TF, Roberts WM, Medeiros LJ, Hayes K, Bueso-Ramos CE. Molecular monitoring of cerebrospinal fluid can predict clinical relapse in acute lymphoblastic leukemia with eosinophilia. Arch Pathol Lab Med. 2003;127: 601-605. [DOI] [PubMed] [Google Scholar]
- 5.Reiter A, Walz C, Watmore A, et al. The t(8; 9)(p22;p24) is a recurrent abnormality in chronic and acute leukemia that fuses PCM1 to JAK2. Cancer Res. 2005;65: 2662-2667. [DOI] [PubMed] [Google Scholar]
- 6.James C, Ugo V, Le Couedic JP, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005; 434: 1144-1148. [DOI] [PubMed] [Google Scholar]
- 7.Baxter EJ, Scott LM, Campbell PJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365: 1054-1061. [DOI] [PubMed] [Google Scholar]
- 8.Levine RL, Wadleigh M, Cools J, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7: 387-397. [DOI] [PubMed] [Google Scholar]
- 9.Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352: 1779-1790. [DOI] [PubMed] [Google Scholar]
- 10.Zhao R, Xing S, Li Z, et al. Identification of an acquired JAK2 mutation in polycythemia vera. J Biol Chem. 2005;280: 22788-22792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchioli R, Finazzi G, Landolfi R, et al. Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol. 2005;23: 2224-2232. [DOI] [PubMed] [Google Scholar]
- 12.Mesa RA, Li CY, Ketterling RP, Schroeder GS, Knudson RA, Tefferi A. Leukemic transformation in myelofibrosis with myeloid metaplasia: a single-institution experience with 91 cases. Blood. 2005;105: 973-977. [DOI] [PubMed] [Google Scholar]
- 13.Steensma DP, Dewald GW, Lasho TL, et al. The JAK2 V617F activating tyrosine kinase mutation is an infrequent event in both “atypical” myeloproliferative disorders and the myelodysplastic syndrome. Blood. 2005;106: 1207-1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones AV, Kreil S, Zoi K, et al. Widespread occurrence of the JAK2 V617F mutation in chronic myeloproliferative disorders. Blood. Prepublished on May 26, 2005, as DOI 10.1182/blood-2005-03-1320. [DOI] [PubMed]
- 15.Ahmadian A, Gharizadeh B, Gustafsson AC, et al. Single-nucleotide polymorphism analysis by pyrosequencing. Anal Biochem. 2000;280: 103-110. [DOI] [PubMed] [Google Scholar]
- 16.Prchal JT. Polycythemia vera and other primary polycythemias. Curr Opin Hematol. 2005;12: 112-116. [DOI] [PubMed] [Google Scholar]
- 17.Onida F, Ball G, Kantarjian HM, et al. Characteristics and outcome of patients with Philadelphia chromosome negative, bcr/abl negative chronic myelogenous leukemia. Cancer. 2002;95: 1673-1684. [DOI] [PubMed] [Google Scholar]
- 18.Onida F, Kantarjian HM, Smith TL, et al. Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood. 2002;99: 840-849. [DOI] [PubMed] [Google Scholar]