Abstract
Lipoteichoic acid (LTA), a glycerol phosphate surface polymer, is a component of the envelope of Gram-positive bacteria. However, the molecular basis for its synthesis or function is not known. Here we report that Staphylococcus aureus LtaS synthesizes glycerol phosphate LTA. Construction of a mutant S. aureus strain with inducible ltaS expression revealed that LTA synthesis is required for bacterial growth and cell division. An ltaS homologue of Bacillus subtilis restored LTA synthesis and the growth of ltaS mutant staphylococci. Thus, LtaS inhibition can be used as a target to treat human infections caused by antibiotic-resistant S. aureus or other bacterial pathogens.
Keywords: cell division, ltaS, polyglycerol phosphate
Staphylococcus aureus is the leading cause of hospital- and community-acquired soft tissue infections, the therapy for which frequently fails because staphylococcal strains acquire resistance mechanisms for all known antibiotics (1–3). The development of novel antibiotics is urgently needed and will require the identification of new target genes that are required for bacterial growth (4). Cell wall teichoic acid (WTA) and lipoteichoic acid (LTA) are characteristic envelope components of Gram-positive bacteria (5–7). Several decades of research on WTA and LTA has revealed their chemical structure and modifications in many different Gram-positive microbes (8–10). Earlier work presumed that synthesis of these secondary wall polymers might be essential for bacterial growth and might therefore serve as a target for antibiotic development (11), similar to peptidoglycan, the primary wall polymer and target of penicillin (12). More recent work showed that, although WTA is dispensable for growth under laboratory conditions (13–15), staphylococcal mutants unable to synthesize WTA display colonization and virulence defects in animal models of infection (15, 16). S. aureus LTA, a 1,3-linked glycerol phosphate polymer, is retained by a glycolipid anchor, diglucosyl diacylglycerol (Glc2-DAG), in bacterial membranes (Fig. 1A) (17, 18). Staphylococci produce polyglycerol phosphate polymers even in the absence of glycolipids, because mutant strains that cannot synthesize Glc2-DAG can still anchor LTA via diacylglycerol (19, 20). Mutations in the dlt operon abolish d-alanyl esterification of LTA without affecting the synthesis of polyglycerol phosphate (21–24). Both dlt and glycolipid anchor mutants continue to multiply, thereby revealing that these nonessential genes are not ideal targets for antibiotic development (20, 23).
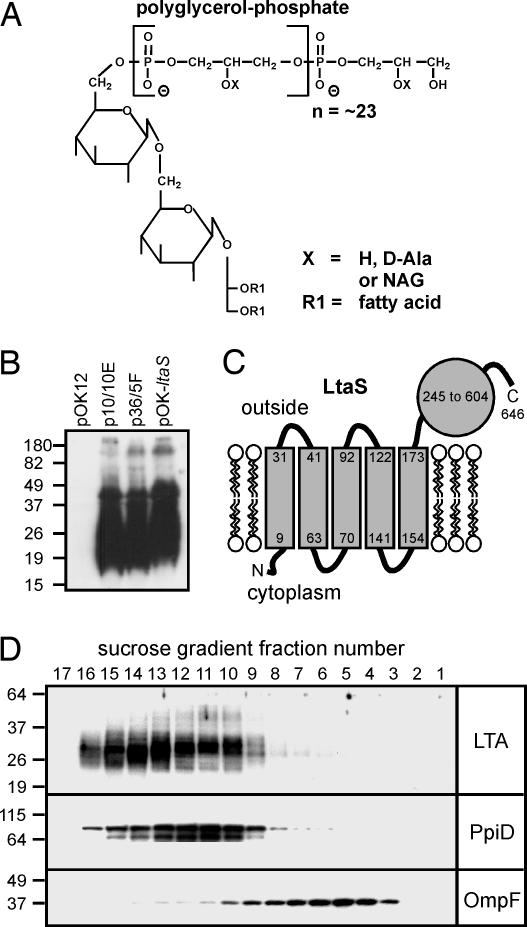
Fig. 1.
Expression of S. aureus LtaS in E. coli promotes synthesis of glycerol phosphate LTA. (A) Chemical structure of S. aureus LTA (26). NAG, N-acetylglucosamine (GlcNAc). (B) Analysis of LTA with polyglycerol phosphate-specific monoclonal antibody. Extracts obtained from E. coli strains ANG490 (pOK12, empty vector), ANG492 (p10/10E), ANG493 (p36/5F), and ANG491 (pOK–ltaS) were separated by SDS/PAGE, electrotransferred to PVDF membrane, and subjected to immunoblotting with LTA-specific antibody. (C) Predicted membrane topology of LtaS. (D) Separation of E. coli inner and outer membranes by sucrose density centrifugation. Isolated fractions were immunoblotted for LTA as well as PpiD (an inner membrane protein) and OmpF (an outer membrane protein). The migration of protein size standards on SDS/PAGE gels is indicated in kilodaltons.
Here we report the identification of a polyglycerol phosphate synthase, LtaS, in S. aureus and demonstrate its requirement for LTA synthesis using staphylococcal and Bacillus subtilis ltaS homologues. Upon ltaS depletion, staphylococci were unable to synthesize LTA and ceased to grow, while displaying defects in cell division. These findings suggest that inhibition of LtaS can be explored as a target for antibiotic therapy of S. aureus infections.
Results
Identification of S. aureus ltaS Encoding Polyglycerol Phosphate LTA Synthase.
Although models proposed for the mechanism of LTA synthesis differ, it is commonly accepted that phosphatidyl glycerol (PG) is used as substrate for polyglycerol phosphate LTA synthesis (25–27). Werner Fischer proposed a model whereby LTA is polymerized on the outer surface of bacterial membranes (26). If LTA synthesis were required for the envelope assembly and growth of Gram-positive bacteria, it would not be possible to isolate mutants with irreversibly inactivated LTA synthesis. We therefore asked whether expression of the presumed LTA synthase in Escherichia coli, a Gram-negative microbe that lacks polyglycerol phosphate but harbors PG membrane lipids, could promote LTA synthesis. A plasmid library of staphylococcal genomic DNA fragments was constructed in pOK12 (28). Plasmids were introduced into E. coli strain ANG471, and clones producing LTA were identified by SDS/PAGE and immunoblotting with monoclonal antibody specific for polyglycerol phosphate. Two plasmid clones, p10/10E and p36/5F, each conferred onto E. coli the ability to produce immune-reactive LTA. As a control, LTA was absent in samples from E. coli harboring only the empty vector pOK12 (Fig. 1B).
LtaS-Mediated Synthesis of LTA Occurs in the Inner Membrane of E. coli.
The identity of the S. aureus DNA fragments contained within plasmids p10/10E and p36/5F was determined by DNA sequencing. A single ORF encoding a previously uncharacterized protein (locus tag SAV0719 in S. aureus Mu50), was present in both clones. This gene was named ltaS for LTA synthase. ltaS was cloned with its native promoter into pOK12, generating plasmid pOK–ltaS. E. coli strains harboring pOK–ltaS produced glycerol phosphate polymers, demonstrating that expression of a single staphylococcal gene in E. coli, which encodes LtaS, is indeed sufficient for LTA synthesis (Fig. 1B).
In agreement with the Fischer model for polyglycerol phosphate synthesis on bacterial surfaces (26), LtaS is predicted to assemble as a polytopic membrane protein with a large C-terminal domain located on the outer surface of the bacterial membrane. The C-terminal domain (LtaS amino acids 245–604) presumably functions as a catalytic domain and is annotated in the Pfam database (www.sanger.ac.uk/Software/Pfam) as a sulfatase domain (Fig. 1C). Initial fractionation experiments suggested that a large fraction of glycerol phosphate polymer was present in the membranes of E. coli strains expressing ltaS (data not shown). Sucrose gradient centrifugation was used to separate bacterial inner and outer membranes (Fig. 1D). LTA floated to the same sucrose density as the inner membrane protein PpiD, but not to that of OmpF, an outer membrane protein (Fig. 1D). The glycerol phosphate polymer therefore seems to be located in the cytoplasmic (inner) membrane of E. coli ANG490 (pOK–ltaS).
ltaS Is Required for LTA Synthesis and Growth of S. aureus.
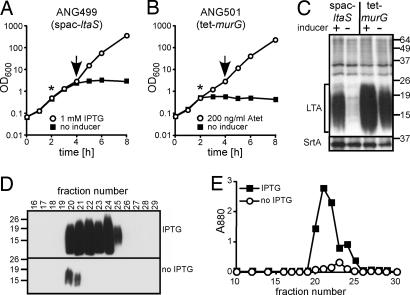
To test whether ltaS is also required for LTA glycerol phosphate synthesis in staphylococci, S. aureus ANG499, a strain with isopropyl β-d-thiogalactopyranoside (IPTG)-inducible expression of ltaS, was constructed. Strain ANG499 ceased to grow within 4 h of removing the ltaS inducer IPTG (Fig. 2A). Moreover, within 2 h of IPTG removal, immunoblot analysis failed to detect LTA in crude bacterial extracts of ltaS-depleted staphylococci (Fig. 2C). To examine whether the disappearance of LTA was caused by an arrest in bacterial growth or by a specific blockade in ltaS expression, we analyzed S. aureus ANG501, a strain that expresses murG, an essential gene in the peptidoglycan biosynthesis pathway (29), under control of a tetracycline-inducible promoter. Similar to strain ANG499, S. aureus strain ANG501 ceased to grow upon removal of the inducer anhydrotetracycline (Fig. 2B). In contrast to that in strain ANG499, anhydrotetracycline removal and depletion of murG in strain ANG501 did not abolish staphylococcal LTA synthesis (Fig. 2C). Thus, the observed block in LTA synthesis of strain ANG499 is likely caused by the depletion of ltaS.
Fig. 2.
S. aureus ltaS is required for LTA synthesis and bacterial growth. (A and B) S. aureus ANG499, with IPTG-inducible ltaS (A), and S. aureus ANG501, with anhydrotetracycline-inducible murG (B). Bacterial strains were grown overnight in the presence of appropriate antibiotics and inducer. The following day, cultures were washed, back-diluted, and grown in the presence or absence of inducer. Bacterial growth was monitored by OD measurements of staphylococcal cultures (OD600). Asterisks indicate time of sample withdrawal for immunoblot analysis. Arrows indicate time of culture dilution (100-fold into fresh media) to sustain logarithmic growth. Atet, anhydrotetracycline. (C) Immunoblot analysis of membrane extracts isolated from ltaS (ANG499) and murG (ANG501) strains by using antibodies specific for LTA and sortase A (SrtA, loading control). The migration of protein size standards on SDS/PAGE gels is indicated in kilodaltons. (D and E) S. aureus ANG513 (ANG499 pitet) was grown in the presence or absence of IPTG (ltaS expression), and LTA was extracted from bacterial membranes. LTA was subjected to hydrophobic interaction chromatography and eluted with a linear gradient of 1-propanol (15–65%). Isolated fractions were subjected to immunoblotting with LTA-specific monoclonal antibody (D) and to hydrolysis and phosphate analysis (E). Phosphate content was measured by A at 880 nm.
To examine further whether polyglycerol phosphate synthesis ceased upon ltaS depletion, LTA was purified from the ltaS-inducible S. aureus strain ANG513, which had been grown in the presence or absence of IPTG. Briefly, LTA was extracted from bacterial lysates, subjected to octyl Sepharose chromatography, and eluted with a linear gradient of 1-propanol [15–65% (vol/vol)] in 50 mM sodium citrate (pH 4.7) (30–32). Large quantities of LTA could only be purified from S. aureus ANG513 cultures that had been grown in the presence of IPTG, but not from cultures grown without IPTG, as judged by immunoblot and phosphate determinations (Fig. 2 D and E). Together these data demonstrate that ltaS is not only required for staphylococcal growth but also for the synthesis of glycerol phosphate LTA.
Depletion of ltaS and LTA Results in Staphylococcal Envelope and Cell Division Defects.
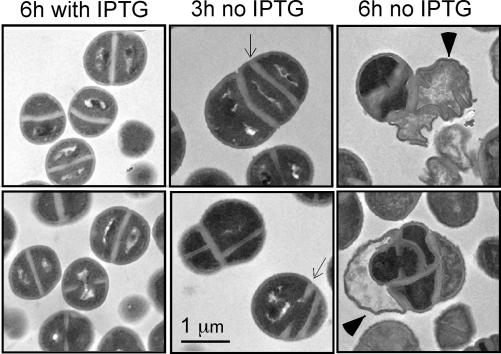
To examine the physiological role of LTA during staphylococcal growth, S. aureus ANG499 cultures that had been grown in the presence or absence of IPTG were subjected to electron microscopy. Briefly, bacterial cells were sedimented by centrifugation, glutaraldehyde- and paraformaldehyde-fixed, stained, embedded, and thin-sectioned. When viewed at 300 kV through an electron microscope, S. aureus ANG499 grown in the presence of IPTG displayed the expected morphology of staphylococci: round cells with a thick cell wall envelope, central division septa, and perpendicularly positioned septa in adjacent cells that displayed subsequent division events (33, 34) (Fig. 3). Within 3 h of IPTG removal, S. aureus ANG499 that had been depleted of LTA displayed aberrant positioning of division septa, which were spaced very closely to the previous division plane (Fig. 3). Further, cells harbored parallel, but not perpendicular, division septa. Upon 6 h of LTA depletion, large numbers of aberrantly shaped cells with empty envelopes, lacking both cytoplasm and nucleic acid, could be observed. These results suggest that LTA synthesis and deposition of this secondary wall polymer within the envelope are essential for the proper positioning of cell wall septa and for cell division processes. Taken together, these experiments identify staphylococcal ltaS as being required for LTA synthesis, cell division, and staphylococcal growth.
Fig. 3.
LTA is required for proper cell envelope assembly. Electron microscopy of fixed and thin-sectioned samples of S. aureus ANG499 were grown in the presence or absence of IPTG (inducer of ltaS expression) for 3 and 6 h. Arrows indicate cell wall septa, whereas arrowheads point to empty cell wall envelopes without cytoplasm and nucleic acid. (Scale bar, 1 μm size standard.)
LtaS Function Is Conserved in Gram-Positive Bacteria.
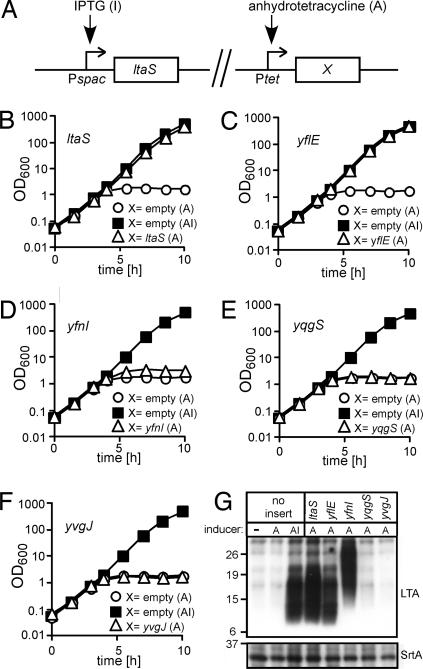
Glycerol phosphate LTA has been isolated from the cell wall envelope of many Gram-positive bacteria including B. subtilis, Bacillus anthracis, Bacillus cereus, Listeria monocytogenes, Streptococcus pyogenes (group A streptococci), and Streptococcus agalactiae (group B streptococci) (10, 18). By using BLAST database (www.ncbi.nlm.nih.gov/BLAST) searches of microbial genomes, one or more ltaS homologues were identified in the genome sequences of any one of the aforementioned bacterial species. For example, whereas S. aureus has one ltaS gene, B. subtilis 168 contains four ltaS homologues (yfnI, yflE, yqgS, and yvgJ with E (expectation) P values of <1e-100 and >40% identity) (35). In previous work, each of these genes could be deleted without abolishing the growth of bacilli (36), prompting the conclusion that any one of the four ltaS homologues of B. subtilis might not be required for bacterial replication. Nevertheless, the multiple, different ltaS homologues of B. subtilis may fulfill redundant or overlapping functions similar to those of S. aureus LtaS in synthesizing polyglycerol phosphate LTA. To address this question, B. subtilis yfnI, yflE, yqgS, and yvgJ or S. aureus ltaS was cloned under control of the tetracycline-inducible promoter in the integration vector pitet (20). Plasmids were integrated into the chromosome of S. aureus ANG499. Functional complementation of ltaS depletion was examined after removal of IPTG by adding anhydrotetracycline to the culture medium (Fig. 4). Anhydrotetracycline-inducible expression of staphylococcal ltaS or B. subtilis yflE restored both LTA glycerol phosphate synthesis and bacterial growth in medium lacking IPTG (Fig. 4 B, C, and G). B. subtilis yqgS or yvgJ did not restore staphylococcal growth and/or LTA synthesis (Fig. 4 E–G). In contrast, anhydrotetracycline-inducible expression of yfnI promoted LTA synthesis, although its polyglycerol phosphate product migrated with a different mobility on SDS/PAGE than LTA synthesized in ltaS- or yflE-expressing strains (Fig. 4G). Unlike that of yflE, expression of yfnI could not restore staphylococcal growth after ltaS depletion (Fig. 4D). These results suggest that B. subtilis yflE and yfnI both encode glycerol phosphate LTA synthases with at least partially overlapping functions, which may explain why these genes can be deleted without loss of viability in bacilli.
Fig. 4.
Functional complementation of ltaS depletion in S. aureus ANG499 with B. subtilis ltaS homologues. (A) Schematic representation of chromosomal organization in ltaS complementation strains. (B–F) Bacterial cultures were grown overnight in the presence of IPTG. The following day, cultures were washed and diluted in fresh medium containing anhydrotetracycline (A), the ltaS homologue inducer, or both anhydrotetracycline and IPTG (AI), the ltaS inducer. Bacterial growth was monitored by OD measurements of staphylococcal cultures (OD600). (B) As a control, anhydrotetracycline induction of staphylococcal ltaS restored bacterial growth upon IPTG removal (depletion of ltaS in strain ANG514). (C–F) Anhydrotetracycline-mediated induction of B. subtilis yflE (ANG516) (C), yfnI (ANG515) (D), yqgS (ANG517) (E), or yvgJ (ANG518) (F) was analyzed for restoration of staphylococcal growth upon IPTG removal. (G) Samples of ltaS-depleted cultures that had been induced with anhydrotetracycline were subjected to immunoblotting by using antibodies specific for LTA and sortase A (SrtA, loading control). The migration of protein size standards on SDS/PAGE gels is indicated in kilodaltons.
Discussion
S. aureus LTA is a polymer of 1,3-linked glycerol phosphate subunits that are tethered to Glc2-DAG (Fig. 1A) (17, 18). This glycerol phosphate structure is conserved in many different Gram-positive bacteria including the human pathogens B. anthracis, Enterococcus faecalis, L. monocytogenes, S. agalactiae, and S. pyogenes (18, 37). Biosynthesis of LTA has been studied with in vitro experiments using isolated bacterial membranes or toluene-treated cells (38, 39). PG was demonstrated to function as substrate for LTA synthesis (39), whereas CDP glycerol, a sn-glycerol-3-phosphate and substrate for WTA assembly, cannot substitute during LTA synthesis (40). PG is comprised of sn-glycerol-1-phosphate linked to diacylated sn-3-glycerol isomer. Although sn-glycerol-1-phosphate is incorporated into LTA, its diacylglycerol byproduct is successively converted to phosphatidic acid, CDP diacylglycerol, phosphatidyl glycerophosphate, and PG, thereby completing the LTA biosynthetic cycle (41).
Pulse-labeling of staphylococci with [14C]acetate revealed that the label appeared successively in glucosyl diacylglycerol (Glc-DAG), Glc2-DAG, and eventually LTA (25). Pulse-labeling with [2-3H]glycerol demonstrated incorporation into PG and glycolipid-anchored LTA (25). Stepwise degradation of pulse-labeled LTA from the glycerol terminus with phosphodiesterase and phosphomonoesterase revealed that the polymer chain grew distal to the lipid anchor (42, 43). These observations were incorporated into a unifying hypothesis whereby transfer of glycerol-1-phosphate from PG to Glc2-DAG and subsequent stepwise addition of glycerol phosphate at the distal end of a polymerizing chain would lead to LTA assembly. If so, LTA synthesis would require an enzyme for polyglycerol phosphate synthesis and perhaps a second activity for transfer of glycerol-1-phosphate from PG to Glc2-DAG (26). Two other proteins are known to be involved in LTA biosynthesis: YpfP synthesizes Glc2-DAG, and LtaA is required for the attachment of glycolipid to LTA (19, 20). However, ltaA mutants continue to assemble LTA with DAG lipid anchor moieties, and there is yet no evidence that LtaA, in addition to its presumed role in glycolipid transport across the membrane, is also involved in transfer of glycerol-1-phosphate to Glc2-DAG (20). Herein we show that LTA synthase (LtaS) is necessary and sufficient for the polymerization of LTA polyglycerol phosphate, a reaction that presumably uses PG substrate and proceeds in the presence or absence of Glc2-DAG. Further studies are needed to unravel whether purified LtaS can indeed synthesize polyglycerol phosphate from PG precursor and/or assemble LTA on its Glc2-DAG membrane anchor.
We report here the identification of S. aureus LTA synthase (locus tag SAV0719 in the genome of the Mu50 strain), where ltaS is required for polyglycerol phosphate LTA synthesis and other cell envelope functions. Expression of ltaS in E. coli led to the formation of polyglycerol phosphate polymer (Fig. 1). After depletion of ltaS in staphylococci, only minimal amounts of the phosphate-containing LTA could be detected by either immunoblot or phosphate determination (Fig. 2 C–E). ltaS depletion also caused growth arrest of staphylococci (Fig. 3). Microscopic examination of ltaS-depleted cells revealed an increase in cell size, partially thickened cell walls, and aberrant placement of cell division sites (Fig. 3). A precise mechanism for the observed defects in envelope and cell division functions cannot yet be deduced from these data. Nevertheless, the proposed functions of LTA, which include scavenging of the Mg2+ ions required for enzyme function and the proper targeting of autolysins to the bacterial envelope (44–46), are in agreement with the observed phenotype of ltaS depletion. A single ltaS gene was identified in the genome sequences of S. aureus, S. pyogenes, and S. agalactiae (data not shown). In contrast, multiple ltaS homologues were found in other Gram-positive bacteria, including four homologues (YfnI, YflE, YqgS, and YvgJ) in B. subtilis. Each of these genes apparently can be deleted without abolishing the growth of mutant bacilli (36), suggesting that any one ltaS homologue of B. subtilis may not be required for bacterial replication. Presumably, the different ltaS homologues fulfill redundant or overlapping functions in synthesizing polyglycerol phosphate LTA. In agreement with this conjecture, we observed that two homologues, yflE and yfnI, encode glycerol phosphate LTA synthases with at least partially overlapping function (Fig. 4).
The finding that ltaS depletion leads to bacterial growth arrest opens the possibility that targeted inhibition of LtaS may be used as an antibiotic therapy for S. aureus infections. LtaS displays the appropriate features of drug targets, because polyglycerol phosphate LTA is not present in eukaryotic cells, and specific inhibitors may abolish bacterial growth. The enzymatic domain of LtaS is thought to be displayed outside of bacterial membranes, obviating the need for inhibitory compounds to cross bacterial membranes. Previous work hypothesized that daptomycin, a compound in clinical use for treatment of drug-resistant S. aureus infections, may inhibit LTA synthesis (47), a claim that has been challenged by the finding of resistance mutations in staphylococcal genes that are not involved in LTA synthesis (48, 49). Identification of LTA synthase now permits further testing of this hypothesis as well as screening for inhibitors with therapeutic properties.
Materials and Methods
Bacterial Strains and Identification of Staphylococcal ltaS.
The strains used in this study are listed in Table 1. Chromosomal DNA of S. aureus SEJ1 (20) was digested with Sau3A, and 3- to 8-kb fragments were cloned into pOK12 cut with BamHI. Plasmids were electroporated into E. coli ANG471 (DH5α harboring pCL55–ypfP/ltaA), transformants were plated on X-Gal indicator agar, and white or light blue colonies were picked. E. coli cultures were grown in 96-well plates, aliquots of four cultures were pooled, and bacterial sediments were extracted with 2% (wt/vol) SDS containing protein sample buffer. Samples were separated on 15% (wt/vol) SDS/PAGE and subjected to immunoblotting with polyglycerol phosphate-specific monoclonal antibody (clone 55, HyCult Biotechnology, Uden, The Netherlands), and LTA expression was detected via chemiluminescence.
Table 1.
Bacterial strains used in this study
| Strains | Relevant features | Source or ref. |
|---|---|---|
| E. coli | ||
| XL1-Blue | Cloning strain, Tetr | Stratagene |
| DH5α | Cloning strain | 53 |
| DY330 | Strain for λ-red cloning | 54 |
| ECE148 | pMutin–HA in E. coli, Ampr | Bacillus Genetic Stock Center |
| ANG243 | pCL55 in XL1–Blue, S. aureus single-site integration vector, Ampr | 55 |
| ANG284 | pitet in XL1–Blue, pCL55 containing tetracycline-inducible promoter, Ampr | 20 |
| ANG343 | pLTV1 in XL1–Blue, Ampr | 51 |
| ANG344 | pLTV1–iTET in DY330, Kanr | This study |
| ANG375 | pDL276 in DH5α, Gram-negative/Gram-positive shuttle vector, Kanr | 50 |
| ANG471 | pCL55–ypfP/ltaA in DH5α, expression of YpfP (SAV1017) and LtaA (SAV1016) under native promoter control, Ampr | 20 |
| ANG490 | pOK12 in DH5α, Kanr | 28 |
| ANG491 | pOK–ltaS in DH5α, Kanr | This study |
| ANG492 | p10/10E in DH5α, Kanr | This study |
| ANG493 | p36/5F in DH5α, Kanr | This study |
| ANG498 | pMutin–HA–ltaS in XL1–Blue, Ampr | This study |
| ANG508 | pitet–ltaS in XL1–Blue, Ampr | This study |
| ANG509 | pitet–yfnI in XL1–Blue, Ampr | This study |
| ANG510 | pitet–yflE in XL1–Blue, Ampr | This study |
| ANG511 | pitet–yqgS in XL1–Blue, Ampr | This study |
| ANG512 | pitet–yvgJ in XL1–Blue, Ampr | This study |
| ANG526 | pLTV1 in DY330, Ampr | This study |
| S. aureus | ||
| RN4220 | Transformable laboratory strain | 56 |
| SEJ1 | spa mutant of RN4220 | 20 |
| ANG499 | RN4220 with IPTG-inducible ltaS expression, Ermr | This study |
| ANG501 | RN4220 with tetracycline-inducible murG expression, Kanr | This study |
| ANG513 | ANG499 with integrated pitet (ANG284); Ermr, Camr, IPTG | This study |
| ANG514 | ANG499 with integrated pitet–ltaS (ANG508); Ermr, Camr, IPTG | This study |
| ANG515 | ANG499 with integrated pitet–yfnI (ANG509); Ermr, Camr IPTG | This study |
| ANG516 | ANG499 with integrated pitet–yflE (ANG510); Ermr, Camr, IPTG | This study |
| ANG517 | ANG499 with integrated pitet–yqgS (ANG511); Ermr, Camr, IPTG | This study |
| ANG518 | ANG499 with integrated pitet–yvgJ (ANG512); Ermr, Camr, IPTG | This study |
| Other | ||
| ANG196 | B. subtilis 168 | Laboratory strain collection |
Tetr, Ampr, Kanr, Ermr, and Camr are resistance markers for tetracycline, ampicillin, kanamycin, erythromycin, and chloramphenicol, respectively.
Inducible Expression of ltaS in Staphylococci.
To construct S. aureus ANG499 with IPTG-inducible ltaS expression, the first 471 bases of ltaS and its preceding ribosome binding site were PCR-amplified with the primers CCCAAGCTTCTAAATAACGGGGGAAAGAATCATGAGTTC and GGGGTACCGACAGGAACAAATTTCTTACTAAATGCTTTTG. The PCR product was cut with HindIII and KpnI and cloned under the IPTG-inducible spac promoter control in pMutin–HA (Bacillus Genetic Stock Center, Columbus, OH). pMutin–HA–ltaS was electroporated into S. aureus RN4220, and transformants were selected on tryptic soy agar supplemented with 10 μg/ml erythromycin and 0.5 mM IPTG. S. aureus ANG501 (murG under tetracycline-inducible promoter control) was obtained by transposon mutagenesis with pLTV1–iTET. Plasmid pLTV1–iTET was constructed by recombining the tetracycline-inducible promoter amplified from plasmid pitet (20), and the Gram-positive and Gram-negative kanamycin-resistance gene was amplified from plasmid pDL276 (50) onto plasmid pLTV1 (51) by using λ-red recombination technology. pLTV1–iTET was electroporated into S. aureus RN4220, and transposon mutants were selected at 44°C on tryptic soy agar plates supplemented with 100 μg/ml kanamycin and 150 ng/ml anhydrotetracycline. The transposon insertion site was 30 nucleotides upstream of murG. PCR and specifically designed primers were used to amplify ltaS from S. aureus RN4220 or yfnI, yflE, yqgS, and yvgJ from B. subtilis 168 DNA. PCR products were digested with AvrII and BglII and ligated with vector pitet that had been cut with the same enzymes. Recombinant plasmids were inserted into the staphylococcal chromosome (20), yielding S. aureus strains ANG513 (ANG499 pitet), ANG514 (ANG499 pitet–ltaS), ANG515 (ANG499 pitet–yfnI), ANG516 (ANG499 pitet–yflE), ANG517 (ANG499 pitet–yqgS), and ANG518 (ANG499 pitet–yvgJ).
Phosphate Determination.
Phosphate determinations were performed essentially as described by Schnitger et al. (52) with some modifications. Briefly, 140 μl of collected FPLC fractions was transferred to 7-ml glass vials and dried for 3 h at 98°C. Compounds were hydrolyzed at 160°C in 400 μl of acid solution [139 ml of concentrated H2SO4 and 37.5 ml of 70% (vol/vol) HClO4 per liter] and subsequently cooled to room temperature. Samples were then cooled on ice, and 2 ml of a freshly prepared reduction solution (3.75 g of ammonium molybdate, 20.4 g of sodium acetate, and 10 g of ascorbic acid per liter) were added. After a 2-h incubation period at 37°C, A880 values were determined. For 5 mM glycerol phosphate and 1.25 mM standard solution, A880 readings of 3.04 ± 0.13 and 0.93 ± 0.06 were measured.
Electron Microscopy.
S. aureus ANG499 was grown overnight at 37°C in tryptic soy broth containing 10 μg/ml erythromycin and 1 mM IPTG. Staphylococci were sedimented by centrifugation (8,000 × g for 5 min), washed twice, and diluted 200-fold into prewarmed medium without or with 1 mM IPTG and appropriate antibiotic. Culture aliquots were removed 3 or 6 h after dilution, and bacteria (OD600 equivalent of ≈90) were sedimented by centrifugation (8,000 × g for 5 min), washed three times with 0.8 ml of 0.1 M sodium cacodylate (pH 7.4), and subsequently fixed for 15 min at room temperature and 2 h at 4°C with 2% (vol/vol) glutaraldehyde/4% (vol/vol) paraformaldehyde in 0.1 M sodium cacodylate. After fixation, bacteria were washed with 0.1 M sodium cacodylate, stained, dehydrated, and embedded for electron microscopy. Thin sections (90 nm) were examined at 300 kV by using a FEI (Hillsboro, OR) Tecnai F30 microscope, and images were captured with a Gatan (Pleasanton, CA) CCD digital camera.
Bacterial Strains, LTA Purification, and Analysis.
Detailed methods are described in the supporting information (SI) Materials and Methods.
Supplementary Material
Acknowledgments
We thank Dominique Missiakas (University of Chicago) for antibody reagents; Taeok Bae (Indiana University School of Medicine Northwest, Gary, IN) for the murG mutant; members of our laboratory for discussion; and the University of Chicago electron microscopy facility for experimental assistance. This work was supported by United States Public Health Service Grant AI38897 (to O.S.) from the Division of Microbiology and Infectious Diseases of the National Institute of Allergy and Infectious Diseases. O.S. is supported by the Great Lakes Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research under National Institute of Allergy and Infectious Diseases Award 1-U54-AI-057153.
Abbreviations
- LTA
lipoteichoic acid
- WTA
wall teichoic acid
- Glc2-DAG
diglucosyl diacylglycerol
- PG
phosphatidyl glycerol
- IPTG
isopropyl β-d-thiogalactopyranoside.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/cgi/content/full/0701821104/DC1.
References
- 1.Kaplan SL, Hulten KG, Gonzalez BE, Hammerman WA, Lamberth L, Versalovic J, Mason EO., Jr Clin Infect Dis. 2005;40:1785–1791. doi: 10.1086/430312. [DOI] [PubMed] [Google Scholar]
- 2.Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, Beach M. Clin Infect Dis. 2001;32:S114–S132. doi: 10.1086/320184. [DOI] [PubMed] [Google Scholar]
- 3.Weigel LM, Clewell DB, Gill SR, Clark NC, McDougal LK, Flannagan SE, Kolonay JF, Shetty J, Killgore GE, Tenover FC. Science. 2003;302:1569–1571. doi: 10.1126/science.1090956. [DOI] [PubMed] [Google Scholar]
- 4.Projan SJ, Shlaes DM. Clin Microbiol Infect. 2004;10:18–22. doi: 10.1111/j.1465-0691.2004.1006.x. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong JJ, Baddiley J, Buchanan JG, Davison AL, Kelemen MV, Neuhaus FC. Nature. 1959;184:247–249. doi: 10.1038/184247a0. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong JJ, Baddiley J, Buchanan JG, Carss B, Greenberg GR. J Chem Soc. 1958:4344–4354. [Google Scholar]
- 7.Archibald AR, Armstrong JJ, Baddiley J, Hay JB. Nature. 1961;191:570–572. doi: 10.1038/191570a0. [DOI] [PubMed] [Google Scholar]
- 8.McCarty M. J Exp Med. 1959;109:361–378. doi: 10.1084/jem.109.4.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neuhaus FC, Baddiley J. Microbiol Mol Biol Rev. 2003;67:686–723. doi: 10.1128/MMBR.67.4.686-723.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fischer W. In: Handbook of Lipid Research. Hanahan DJ, editor. Vol 6. New York: Plenum; 1990. pp. 123–234. [Google Scholar]
- 11.Mauel C, Young M, Margot P, Karamata D. Mol Gen Genet. 1989;215:388–394. doi: 10.1007/BF00427034. [DOI] [PubMed] [Google Scholar]
- 12.Tipper DJ, Strominger JL. Proc Natl Acad Sci USA. 1965;54:1133–1141. doi: 10.1073/pnas.54.4.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D'Elia MA, Pereira MP, Chung YS, Zhao W, Chau A, Kenney TJ, Sulavik MC, Black TA, Brown ED. J Bacteriol. 2006;188:4183–4189. doi: 10.1128/JB.00197-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D'Elia MA, Millar KE, Beveridge TJ, Brown ED. J Bacteriol. 2006;188:8313–8316. doi: 10.1128/JB.01336-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weidenmaier C, Kokai-Kun JF, Kristian SA, Chanturiya T, Kalbacher H, Gross M, Nicholson G, Neumeister B, Mond JJ, Peschel A. Nat Med. 2004;10:243–245. doi: 10.1038/nm991. [DOI] [PubMed] [Google Scholar]
- 16.Weidenmaier C, Peschel A, Xiong YQ, Kristian SA, Dietz K, Yeaman MR, Bayer AS. J Infect Dis. 2005;191:1771–1777. doi: 10.1086/429692. [DOI] [PubMed] [Google Scholar]
- 17.Duckworth M, Archibald AR, Baddiley J. FEBS Lett. 1975;53:176–179. doi: 10.1016/0014-5793(75)80013-5. [DOI] [PubMed] [Google Scholar]
- 18.Fischer W, Mannsfeld T, Hagen G. Biochem Cell Biol. 1990;68:33–43. doi: 10.1139/o90-005. [DOI] [PubMed] [Google Scholar]
- 19.Kiriukhin MY, Debabov DV, Shinabarger DL, Neuhaus FC. J Bacteriol. 2001;183:3506–3514. doi: 10.1128/JB.183.11.3506-3514.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gründling A, Schneewind O. J Bacteriol. 2007;189:2521–2530. doi: 10.1128/JB.01683-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heaton MP, Neuhaus FC. J Bacteriol. 1992;174:4707–4717. doi: 10.1128/jb.174.14.4707-4717.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heaton MP, Neuhaus FC. J Bacteriol. 1994;176:681–690. doi: 10.1128/jb.176.3.681-690.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peschel A, Otto M, Jack RW, Kalbacher H, Jung G, Götz F. J Biol Chem. 1999;274:8405–8410. doi: 10.1074/jbc.274.13.8405. [DOI] [PubMed] [Google Scholar]
- 24.Peschel A, Vuong C, Otto M, Götz F. Antimicrob Agents Chemother. 2000;44:2845–2847. doi: 10.1128/aac.44.10.2845-2847.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koch HU, Haas R, Fischer W. Eur J Biochem. 1984;138:357–363. doi: 10.1111/j.1432-1033.1984.tb07923.x. [DOI] [PubMed] [Google Scholar]
- 26.Fischer W. Med Microbiol Immunol. 1994;183:61–76. doi: 10.1007/BF00277157. [DOI] [PubMed] [Google Scholar]
- 27.Chiu TH, Morimoto H, Baker JJ. Biochim Biophys Acta. 1993;1166:222–228. doi: 10.1016/0005-2760(93)90101-e. [DOI] [PubMed] [Google Scholar]
- 28.Vieira J, Messing J. Gene. 1991;100:189–194. doi: 10.1016/0378-1119(91)90365-i. [DOI] [PubMed] [Google Scholar]
- 29.Mengin-Lecreulx D, Texier L, Rousseau M, van Heijenoort J. J Bacteriol. 1991;173:4625–4636. doi: 10.1128/jb.173.15.4625-4636.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morath S, von Aulock S, Hartung T. J Endotoxin Res. 2005;11:348–356. doi: 10.1179/096805105X67328. [DOI] [PubMed] [Google Scholar]
- 31.Hashimoto M, Tawaratsumida K, Kariya H, Kiyohara A, Suda Y, Krikae F, Kirikae T, Götz F. J Immunol. 2006;177:3162–3169. doi: 10.4049/jimmunol.177.5.3162. [DOI] [PubMed] [Google Scholar]
- 32.Fischer W, Koch HU, Haas R. Eur J Biochem. 1983;133:523–530. doi: 10.1111/j.1432-1033.1983.tb07495.x. [DOI] [PubMed] [Google Scholar]
- 33.Giesbrecht P, Kersten T, Maidhof H, Wecke J. Microbiol Mol Biol Rev. 1998;62:1371–1414. doi: 10.1128/mmbr.62.4.1371-1414.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tzagoloff H, Novick R. J Bacteriol. 1977;129:343–350. doi: 10.1128/jb.129.1.343-350.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kunst F, Ogasawara N, Moszer I, Albertini AM, Alloni G, Azevedo V, Bertero MG, Bessieres P, Bolotin A, Borchert S, et al. Nature. 1997;390:249–256. doi: 10.1038/36786. [DOI] [PubMed] [Google Scholar]
- 36.Kobayashi K, Ehrlich SD, Albertini A, Amati G, Andersen KK, Arnaud M, Asai K, Ashikaga S, Aymerich S, Bessieres P, et al. Proc Natl Acad Sci USA. 2003;100:4678–4683. doi: 10.1073/pnas.0730515100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCarty M, Morse SI. Adv Immunol. 1964;4:249–286. doi: 10.1016/s0065-2776(08)60709-9. [DOI] [PubMed] [Google Scholar]
- 38.Emdur L, Chiu T. FEBS Lett. 1975;55:216–219. doi: 10.1016/0014-5793(75)80995-1. [DOI] [PubMed] [Google Scholar]
- 39.Childs WC, III, Neuhaus FC. J Bacteriol. 1980;143:293–301. doi: 10.1128/jb.143.1.293-301.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ganfield MC, Pieringer RA. J Biol Chem. 1980;255:5164–5169. [PubMed] [Google Scholar]
- 41.Fischer W. Adv Microb Physiol. 1988;29:233–302. doi: 10.1016/s0065-2911(08)60349-5. [DOI] [PubMed] [Google Scholar]
- 42.Cabacungan E, Pieringer RA. J Bacteriol. 1981;147:75–79. doi: 10.1128/jb.147.1.75-79.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taron DJ, Childs WC, III, Neuhaus FC. J Bacteriol. 1983;154:1110–1116. doi: 10.1128/jb.154.3.1110-1116.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fischer W, Rösel P, Koch HU. J Bacteriol. 1981;146:467–475. doi: 10.1128/jb.146.2.467-475.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cleveland RF, Höltje JV, Wicken AJ, Tomasz A, Daneo-Moore L, Shockman GD. Biochem Biophys Res Commun. 1975;67:1128–1135. doi: 10.1016/0006-291x(75)90791-3. [DOI] [PubMed] [Google Scholar]
- 46.Lambert PA, Hancock IC, Baddiley J. Biochim Biophys Acta. 1977;472:1–12. doi: 10.1016/0304-4157(77)90012-0. [DOI] [PubMed] [Google Scholar]
- 47.Canepari P, Boaretti M, Lleo MM, Satta G. Antimicrob Agents Chemother. 1990;34:1220–1226. doi: 10.1128/aac.34.6.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Laganas V, Alder J, Silverman JA. Antimicrob Agents Chemother. 2003;47:2682–2684. doi: 10.1128/AAC.47.8.2682-2684.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Friedman L, Alder JD, Silverman JA. Antimicrob Agents Chemother. 2006;50:2137–2145. doi: 10.1128/AAC.00039-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dunny GM, Lee LN, LeBlanc D. Appl Environ Microbiol. 1991;57:1194–1201. doi: 10.1128/aem.57.4.1194-1201.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Camilli A, Portnoy A, Youngman P. J Bacteriol. 1990;172:3738–3744. doi: 10.1128/jb.172.7.3738-3744.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schnitger H, Papenberg K, Ganse E, Czok R, Buecher T, Adam H. Biochem Z. 1959;332:167–185. [PubMed] [Google Scholar]
- 53.Hanahan D. J Mol Biol. 1983;166:557–572. doi: 10.1016/s0022-2836(83)80284-8. [DOI] [PubMed] [Google Scholar]
- 54.Yu D, Ellis HM, Lee EC, Jenkins NA, Copeland NG, Court DL. Proc Natl Acad Sci USA. 2000;97:5978–5983. doi: 10.1073/pnas.100127597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee CY, Buranen SL, Ye Z-H. Gene. 1991;103:101–105. doi: 10.1016/0378-1119(91)90399-v. [DOI] [PubMed] [Google Scholar]
- 56.Kreiswirth BN, Lofdahl S, Betley MJ, O'Reilly M, Schlievert PM, Bergdoll MS, Novick RP. Nature. 1983;305:709–712. doi: 10.1038/305709a0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.