Abstract
Background
Cardiac arrest due to ventricular arrhythmia in the absence of a reversible cause or contraindication has been a class I indication for insertion of an implantable cardioverter defibrillator since 1998. We compared and contrasted the use of implantable cardioverter defibrillator therapy in Canada and the United States among adults who survived a cardiac arrest.
Method
Data on hospital separations from April 1, 1994 through March 31, 2003 were obtained from the Health Person-Oriented Information Database maintained by Statistics Canada and from the US National Hospital Discharge Survey on all patients with a primary diagnosis of cardiac arrest, ventricular fibrillation or ventricular flutter for the same 9-year period. We excluded all records of patients with a secondary diagnosis of acute myocardial infarction.
Results
In Canada, 3793 patients survived to discharge after a cardiac arrest; 628 (16.6%) of these were implanted with a cardioverter defibrillator before discharge. The implant rate rose steadily from 5.4% in 1994/95 to 26.7% in 2002/03. In the United States, 23 688 (30.2%) of 78 538 such survivors received an implantable cardioverter defibrillator before discharge. Logistic regression analysis indicated that sex, age, fiscal year, the hospital's teaching status, hospital size and patient history of heart failure were positive predictors of implantable cardioverter defibrillator implantation. Age, renal failure, liver failure and cancer were negative predictors of receiving an implantable cardioverter defibrillator.
Interpretation
The rate of use of implantable cardioverter defibrillator therapy for cardiac arrest survivors in Canada is increasing, but still is lower than the rate in the United States.
Sudden cardiac death is the second-leading cause of death in the United States, with over 400 000 deaths annually1,2 (comparable data for Canada are unavailable). Most such sudden deaths are from ventricular fibrillation secondary to coronary artery disease;3 primary ventricular arrhythmias, bradycardia, asystole and pulseless electrical activity are the other broad mechanisms. Studies4–6 published prior to the major trials7–9 of implantable cardioverter defibrillators showed that survivors of sudden cardiac arrest are at high risk of another episode within a few years; over half of the deaths that result are due to recurrences.
There have been 3 large randomized studies that compared cardioverter defibrillator implantation with the best known medical therapy, in patients surviving sudden cardiac death.7–9 The largest of these was the Antiarrhythmics Versus Implantable Defibrillators (AVID) trial, reported in 1997,7 which at 1 year found a relative reduction in deaths of 39%; the other studies8,9 showed similar results. A meta-analysis10 of all 3 studies indicated that implantable cardioverter defibrillators reduced the relative risk of recurrent sudden cardiac death by 50% (95% confidence interval [CI] 0.37%–0.67%) and death from any cause by 28% (95% CI 0.60%–0.87%). Since 1998, the guidelines of the American College of Cardiology and the American Heart Association have recommended that a “cardiac arrest due to ventricular fibrillation or ventricular tachycardia not due to a transient or reversible cause is a class 1 indication for an implantable cardioverter defibrillator.”11 The Canadian guidelines, first published in 2000, are similar.12 Previous data from Ontario have revealed a low rate of cardioverter defibrillator implantation (12.8%) after an out-of-hospital cardiac arrest.13 The aims of our study were 3-fold: to examine temporal trends of cardioverter defibrillator implantation in Canada during periods before and after publication of the related trials and guidelines; to compare implant rates in Canada with those in the United States; and to examine in detail the factors influencing implantation in Canada.
Methods
Study population
We obtained data on all Canadian and US patients with a primary diagnosis of cardiac arrest, ventricular fibrillation or ventricular flutter and not also having a diagnosis of myocardial infarction who survived to be discharged from hospital for the period April 1, 1994 through March 31, 2003. Data from patients with a primary diagnosis of ventricular tachycardia were not included for analysis because the data sources do not contain detail sufficient to adequately assess each patient's suitability for cardioverter defibrillator implantation.
Medical data were coded according to the International Classification of Diseases (ICD).14–16 All diagnostic and procedure codes examined in this article were unchanged over the 9-year study period; they are listed, respectively, in Appendix 1 and Appendix 2 (available at www.cmaj.ca/cgi/content/full/177/1/41/DC1).
Canadian data source
Data on hospital separations for the study period were obtained from the Health Person-Oriented Information database maintained by Statistics Canada. This database tracks patients from admission until in-hospital death or final discharge (including transfers between acute-care hospitals). For each patient, a primary diagnosis and up to 16 secondary diagnoses were abstracted. Medical data were coded according to the ICD's 9th revision (ICD-9)14 or the 10th revision enhanced for Canada (ICD-10-CA).15 Health Person-Oriented Information data are derived from the Discharge Abstracts Data set maintained by the Canadian Institute for Health Information. In 2002/03, the discrepancy rates17 between initial abstraction and subsequent audit for demographic data was 0.2%; for intervention codes, less than 1.0%; and for major clinical category, 4.2%. Since the database does not track interprovincial transfers, data were not extracted for provinces and territories that lacked implanting capacity for the device during any part of the study period. Thus, data from Yukon, Nunavut, the Northwest Territories, Newfoundland, New Brunswick and Prince Edward Island were excluded.
The database tracks patients between hospitals until in-hospital death or final discharge; data on patients' disposition at discharge were unavailable for some years within the study period. We examined overall survival and the implantation rates of cardioverter defibrillators among survivors. Unlike other provinces, British Columbia records preadmission deaths as admissions to hospital; BC was therefore excluded from the initial analysis of survival until hospital discharge. Data from surviving BC patients were then included in all subsequent analyses.
US data source
The National Hospital Discharge Survey has been conducted continuously by the National Center for Health Statistics since 1965.18 This survey continues to be the principal source for national data on the characteristics of patients discharged from nonfederal short-stay hospitals in the United States. Its 3-stage probability design involves sampling within geographic areas, then hospitals within these areas and, finally, the discharges at individual hospitals. Available data relating to the personal characteristics of a patient include birth date (converted to age), sex, race, ethnicity, marital status, US Postal Service zip code and expected sources of payment of patients' medical expenses, as well as administrative items such as admission and discharge dates, type and source of admission, and status at discharge. Medical information about each patient (up to 7 diagnoses and up to 4 procedures) is coded according to ICD-9-CM (clinical modification).16
Because of the complex multistage design of the National Hospital Discharge Survey, the data must be weighted to produce national estimates; the estimation procedure produces national estimates that are unbiased.19 Estimates of the sampling variability that occurs by chance are provided by approximate relative standard errors. Details of the calculation of the estimates are provided elsewhere.18
The US National Center for Health Statistics produces a multiyear file of the survey's discharge and weight data, relative standard error tables and census population estimates. An ongoing quality-control program recodes 5%–10% of the data independently, with discrepancies resolved by the chief survey coder. In 2002, for example, overall error rates for medical coding and other data entry were less than 0.1%.18 Moreover, the quality of the National Hospital Discharge Survey has been shown to be very good in independent validation studies20,21 and its data have been used in multiple publications.22–24 In its files for public use, however, information on the sampling variability of the survey's complex multistage design is insufficient to permit logistic regression modelling.
Statistical analysis and ethics approval
The Z-test was used to test simple relationships between continuous measures and receipt of a cardioverter defibrillator implant, and the population proportions test for categorical measures (presented as percentages). Logistic regression was used to create a multivariable model with odds ratios and confidence intervals by sex, admitting hospital size (≥ 100 v. < 100 beds), teaching status of the admitting hospital (teaching or nonteaching), patient residence (rural or nonrural, decided via patients' postal codes) and comorbidities (Appendix 2, available at www.cmaj.ca/cgi/content/full/177/1/41/DC1). Stepwise selection methods were used to identify the statistically significant independent predictors of cardioverter defibrillator implantation. All 2-way interactions in the main effects model were considered and included in the model by means of stepwise selection. The Hosmer and Lemeshow goodness-of-fit test was used to evaluate the model. All tests used p ≤ 0.05 to indicate statistical significance.
The study was approved by the ethics board of the University of Ottawa Heart Institute.
Results
Canadian outcomes
In the year 2000, the total estimated population of the 7 provinces included in our analysis was 29 260 050; that of the excluded provinces and territories was 1 530 784. There were 9699 hospital admissions with a primary diagnosis of cardiac arrest, ventricular fibrillation or ventricular flutter in the 6 provinces (i.e., excluding BC as well). Hence, the prevalence in 2000 of patients who experienced an out-of-hospital cardiac arrest and survived to hospital admission was 3.8 per 100 000 population. Of these 9699 patients, 1537 (15.8%) had a secondary diagnosis of myocardial infarction and were excluded from further analysis. There was no significant change in the annual percentage of patients excluded because of a secondary diagnosis of myocardial infarction; for example, 14.6% of patients were excluded in 1993/94, compared with 15.8% in 2002/03.
Of the 8162 eligible patients, 3256 (39.9%) survived to be discharged from hospital, a survival rate that varied little over the study period. Corresponding data from British Columbia (i.e., on 537 patients who survived until discharge) were then added, making a total of 3793 patients who survived until discharge. Of these survivors, 628 (16.6%) received an implantable cardioverter defibrillator before hospital discharge. Patients' demographics at baseline are shown, stratified by sex, in Table 1; device implantation rates, stratified by year and age group, are shown in Appendix 3 (available at www.cmaj.ca/cgi/content/full/177/1/41/DC2). Implantation rates were relatively similar across age groups less than 70 years (20%–29%), but declined to 12.0% in the 70–79 year age group and even less (2.7%) in patients aged over 80 years. Figure 1, which graphs the annual rates in Canada and the United States, reveals that cardioverter defibrillator implant rates have progressively increased in both countries, and that the US rate, recently, was at least twice that in Canada. Univariate predictors of device implantation in Canada are shown in Figure 2, along with details of logistic regression analysis to show the independent predictors of receiving an implantable cardioverter defibrillator. Independent predictors were age, sex, teaching status and size of the admitting hospital, year and comorbidity. Figure 3 shows Canadian implant rates by year, stratified by sex.
Table 1
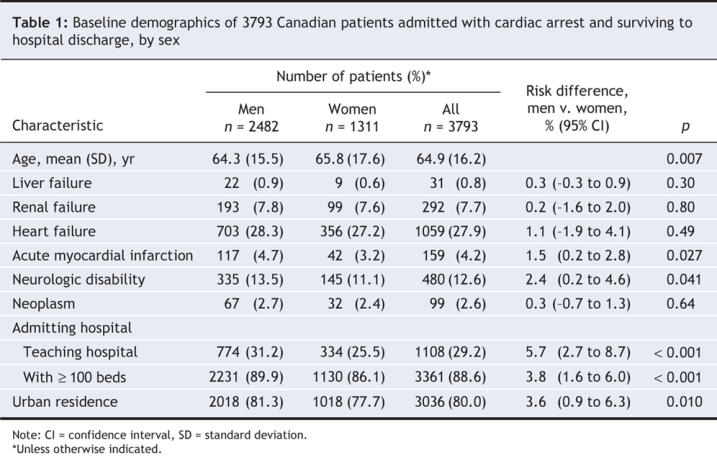
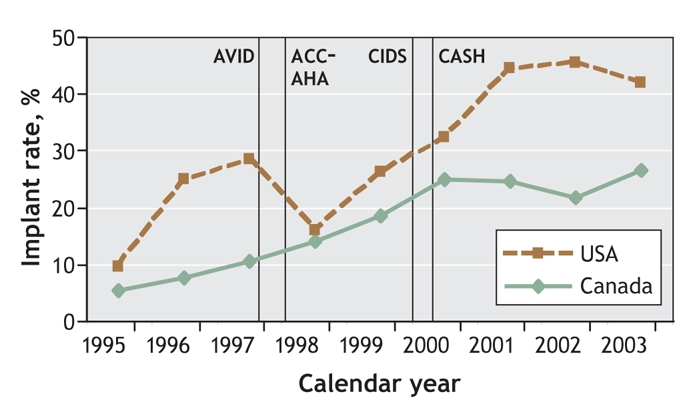
Figure 1: Cardioverter defibrillator implant rates in survivors of out-of-hospital cardiac arrest in the United States and Canada. Data points centre on fiscal years, which end on March 31. Vertical lines indicate the publication of major secondary-prevention trials and guidelines, as follows. AVID = Antiarrhythmics Versus Implantable Defibrillators trial,7 published November 1997: N Engl J Med 1997;337:1576. ACC–AHA = American College of Cardiology–American Heart Association guidelines,11 April 1998: J Am Coll Cardiol 1998;31:1175. CIDS = Canadian Implantable Defibrillator Study,8 March 2000: Circulation 2000;101:1297. CASH = Cardiac Arrest Hamburg Study,9 August 2000: Circulation 2000;102:748.
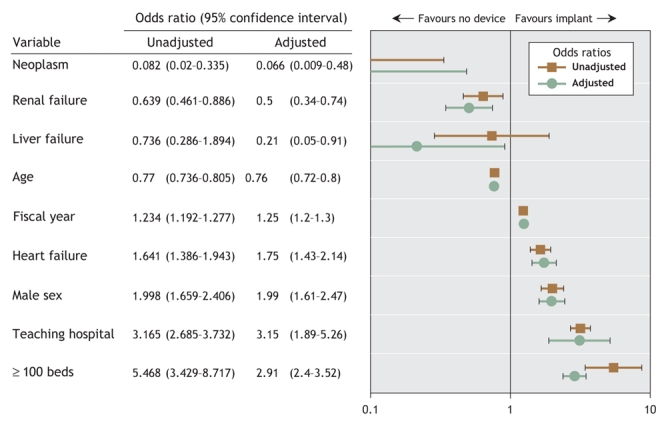
Figure 2: Odds ratios, both unadjusted and adjusted for all variables in the model, for predictors of cardioverter defibrillator implantation in Canadian survivors of out-of-hospital cardiac arrest. All other variables considered for the model, including presence of acute myocardial ischemia, were not predictive for use of this therapy.
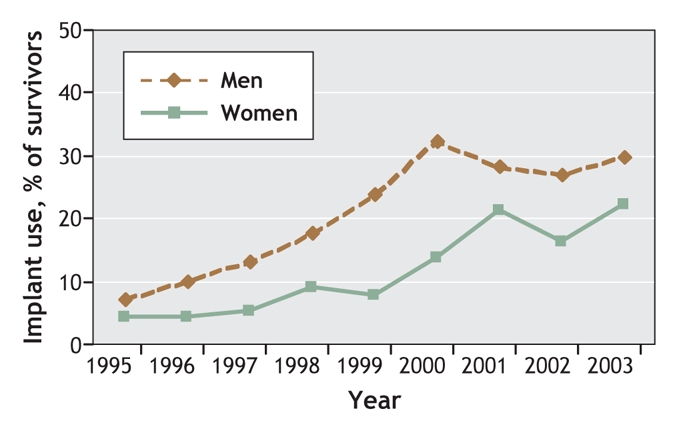
Figure 3: Cardioverter defibrillator implant rates in male and female survivors of out-of-hospital cardiac arrest in Canada by year, 1994–2003. (Data points centre on fiscal years, which end on March 31.)
When we repeated the entire analysis after excluding an additional 414 patients with concomitant diagnoses of another potentially reversible cause of cardiac arrest (acute myocardial ischemia, hypokalemia, hyperkalemia or drug reaction), the results were similar to those presented (data not shown).
US outcomes
Data were drawn from the entire US population, estimated at 274 634 000 from census data gathered in 2000.25 Between April 1994 and March 2003, an estimated 182 058 patients without myocardial infarction were admitted with cardiac arrest; 78 538 (43.1%) survived until discharge. Among 75 538 survivors discharged home, 23 688 (30.2%) received an implantable cardioverter defibrillator during their stay. Figure 1 compares the temporal pattern of device implantation with that of Canada.
Interpretation
The main findings of the study are that implantation rates for implantable cardioverter defibrillators after out-of-hospital cardiac arrests in Canada are increasing (26.7% in 2002/03) but are still behind those in the United States (42.0% in the same fiscal year). However, we also found a significant sex disparity in implantation rates (male patients were twice as likely as female patients to receive an implantable cardioverter defibrillator) and evidence of issues with care access, knowledge translation and guideline penetration: patients initially admitted to a teaching hospital were almost 3 times as likely to receive an implantable cardioverter defibrillator as those admitted to a nonteaching hospital (Figure 2).
The appropriate rate of cardioverter defibrillator implantation after surviving a cardiac arrest is unclear. Some patients will have had a cardiac arrest unrelated to ventricular arrhythmia. About 5% of patients will have major neurologic impairment after their arrest;26 some patients will have clinically important comorbidity or terminal illness; and in some patients, the ventricular arrhythmia causing the arrest will be clearly related to a reversible cause. (For example, patients with acute myocardial infarction causing their cardiac arrest do not require an implanted cardioverter defibrillator. Therefore, we excluded such patients in our study.) Perhaps the best available contemporary data are from a study26 involving 200 patients in a single US county who experienced an out-of-hospital cardiac arrest between 1990 and 2001. Of these, 84 patients survived until hospital discharge, of whom 35 (42%) received an implantable cardioverter defibrillator. Even this implant rate may be an underestimate, because many of the patients in this study had their arrest before publication of the large trials of implantable cardioverter defibrillators.7–9 Our data showed that US implantation rates of cardioverter defibrillators are consistently higher than in Canada (lately, more than double our rate: Figure 1); data for revascularization procedures have shown a similar trend.27,28 Although it is possible that the gap between the countries in part reflects overuse of implantable cardioverter defibrillators in the United States, an analysis29 of the US Medicare database suggested that they were actually underutilized.
Differences in cardiac care according to sex have been described for 20 years; most of the previous data related to the management of coronary artery disease.30–32 We show clear evidence of a sex differential in access to implantable cardioverter defibrillator therapy for the secondary prevention of sudden cardiac death. Two previous studies13,26 were underpowered to detect a sex difference. A third22 did find evidence of a sex gap in the United States but suggested that the gap had closed by 2000. A number of explanations for our findings are possible: perhaps there are some additional confounding factors that make male survivors of sudden cardiac death different from female survivors; perhaps women decline cardioverter defibrillator implantation more often than men do; and perhaps a sex bias exists in referrals. However, it is clear that male and female patients with implants have similar rates of appropriate therapy from the device.33,34
We also found evidence of a major gap in the use of these devices depending on the status of the admitting hospital: patients initially admitted to a teaching hospital were 2.91 times likelier to receive an implantable cardioverter defibrillator as those admitted to a nonteaching hospital. There is probably more than 1 reason for this. Knowledge translation is likely to be a key factor.35 Availability of electrophysiologists and implanting centres may be an issue, since countries with more electrophysiologists and cardioverter defibrillator implanting centres (such as the United States and Germany) have higher implantation rates than countries with lower levels of service (e.g., the United Kingdom, Canada and France).29 Some physicians may also be concerned about the cost of the technology, although implantable cardioverter defibrillators have been shown to be moderately cost-effective for secondary prevention of death (US$67 000 per life-year gained).36
This study has several limitations. The validity of the data depends on the appropriate use of codes at the time of hospital discharge. In the United States, internal audits of the National Hospital Discharge Survey and previous studies20,21 have indicated that the validity of its data is acceptable. The discrepancy rate for the Canadian database is higher than that reported for the US discharge survey. No data exist on the discrepancy rates of the medical codes used in our study (we speculate that the discrepancy rates for the relatively unequivocal primary codes in our study would be less). Because clinical information from administrative databases may be incomplete, we may not have controlled for all confounders. Finally, it is not possible to check for consistency of coding between the Canadian and US databases. Since the coding processes are very similar, however, we do not anticipate that this would lead to a bias of any consequence to the results.
Despite the limitations noted, we believe that this is the most comprehensive population-based study of implantable cardioverter defibrillator utilization in survivors of out-of-hospital cardiac arrest. We found that implant rates in Canada are increasing but are still substantially behind those in the United States. There was evidence of a significant sex disparity in cardioverter defibrillator implantation as well as a major issue in care access, knowledge translation and guideline penetration. Further investigation is required to identify reasons for these several gaps in care and to devise and implement strategies to address them.
@ See related article page 49
Supplementary Material
Acknowledgments
Thanks to Ann Guo for assistance with the extraction and analysis of National Hospital Discharge Survey data.
Footnotes
This article has been peer reviewed.
Contributors: David Birnie developed the concept, design and direction of the project and wrote the manuscript. David Birnie, Christie Sambell, Helen Johansen, Kathryn Williams and Douglas Lee coordinated the project. David Birnie and Kathryn Williams selected the International Classification of Diseases codes that were used. Extraction and all analyses of the Canadian data from the Health Person Oriented Information initiative were performed by Christie Sambell, supervised by Helen Johansen. All authors were involved in the critical revision of the manuscript and approved the final version for publication.
Competing interests: None declared by Christie Sambell, Helen Johansen, Kathryn Williams, Robert Lemery, Michael Gollob and Douglas Lee. David Birnie and Martin Green have received speaker's fees and honoraria from Medtronic Inc. Medtronic Canada contributes to a university–industry research grant from the Canadian Institutes of Health Research to Anthony Tang.
Correspondence to: Dr. David Birnie, Ottawa Heart Institute, 40 Ruskin Rd., Ottawa ON K1Y 4W7; fax 613 761-4407; dbirnie@ottawaheart.ca
REFERENCES
- 1.Zheng ZJ, Croft JB, Giles WH, et al. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001;104:2158-63. [DOI] [PubMed]
- 2.Hoyert DL, Heron MP, Murphy SL, et al. Deaths: final data for 2003. Natl Vital Stat Rep 2006;54:1-120. [PubMed]
- 3.Myerburg RJ, Castellanos A. Cardiac arrest and sudden cardiac death. In: Braunwald E, Zipes DP, Libby P, editors. Heart disease: a textbook of cardiovascular medicine. Philadelphia: WB Saunders; 2001. p. 890–931.
- 4.Cobbe SM, Dalziel K, Ford I, et al. Survival of 1476 patients initially resuscitated from out of hospital cardiac arrest. BMJ 1996;312:1633-7. [DOI] [PMC free article] [PubMed]
- 5.Liberthson RR, Nagel EL, Hirschman JC, et al. Prehospital ventricular defibrillation: prognosis and follow-up course. N Engl J Med 1974;291:317-21. [DOI] [PubMed]
- 6.Schaffer WA, Cobb LA. Recurrent ventricular fibrillation and modes of death in survivors of out-of-hospital ventricular fibrillation. N Engl J Med 1975;293:259-62. [DOI] [PubMed]
- 7.The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med 1997;337:1576-83. [DOI] [PubMed]
- 8.Connolly SJ, Gent M, Roberts RS, et al. Canadian Implantable Defibrillator Study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 2000;101:1297-302. [DOI] [PubMed]
- 9.Kuck KH, Cappato R, Siebels J, et al. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg (CASH). Circulation 2000;102:748-54. [DOI] [PubMed]
- 10.Connolly SJ, Hallstrom AP, Cappato R, et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials: AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study; Cardiac Arrest Study Hamburg; Canadian Implantable Defibrillator Study. Eur Heart J 2000;21:2071-8. [DOI] [PubMed]
- 11.Gregoratos G, Cheitlin MD, Conill A, et al. ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). J Am Coll Cardiol 1998;31:1175-209. [DOI] [PubMed]
- 12.Connolly SJ, Krahn A, Klein G. Long term management of the survivor of ventricular fibrillation or sustained ventricular tachycardia. Can J Cardiol 2000;16(Suppl C):20C-2C. [PubMed]
- 13.Parkash R, Tang A, Wells G, et al. Use of implantable cardioverter defibrillators after out-of-hospital cardiac arrest: a prospective follow-up study. CMAJ 2004;171:1053-6. [DOI] [PMC free article] [PubMed]
- 14.Manual of the international statistical classification of diseases. Based on recommendation of the Ninth Revision Conference, 1975, and adapted by the Twenty-ninth World Health Assembly. Volume 1. Geneva, Switzerland: World Health Organization; 1977.
- 15.Canadian Institute of Health Information. International statistical classification of diseases and related health problems. ICD-10-CA/CCI. Ottawa: The Institute; 2003.
- 16.Commission on Professional and Hospital Activities. Annotated ICD-9-CM international classification of diseases, 9th revision, clinical modification. Ann Arbor (MI): Edward Brothers, Inc.; 1986.
- 17.Health Results Team for Information Management. Reabstraction study of the Ontario case costing facilities for fiscal years 2002/2003 and 2003/2004. November 2005. Available: www.health.gov.on.ca/transformation/providers/information/data_quality/reabstraction_study.pdf (accessed 2007 May 3).
- 18.National Center for Health Statistics. National hospital discharge survey description. Available: www.cdc.gov/nchs/about/major/hdasd/nhdsdes.htm (accessed 2007 May 3).
- 19.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Series 1: Programs and collection procedures. No. 39. Hyattsville (MD): US Department of Health and Human Services; 2000. Available: www.cdc.gov/nchs/data/series/sr_01/sr01_039.pdf (accessed 2007 May 3). [PubMed]
- 20.Hsia DC, Krushat WM, Fagan AB, et al. Accuracy of diagnostic coding for Medicare patients under the prospective-payment system. N Engl J Med 1988;318:352-5. [DOI] [PubMed]
- 21.Romano PS, Mark DH. Bias in the coding of hospital discharge data and its implications for quality assessment. Med Care 1994;32:81-90. [DOI] [PubMed]
- 22.Voigt A, Ezzeddine R, Barrington W, et al. Utilization of implantable cardioverter–defibrillators in survivors of cardiac arrest in the United States from 1996 to 2001. J Am Coll Cardiol 2004;44:855-8. [DOI] [PubMed]
- 23.Koelling TM, Chen RS, Lubwama RN, et al. The expanding national burden of heart failure in the United States: the influence of heart failure in women. Am Heart J 2004;147:74-8. [DOI] [PubMed]
- 24.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA 2004;292:1333-40. [DOI] [PubMed]
- 25.National Center for Health Statistics. Age adjustment. Available: www.cdc.gov/nchs/datawh/nchsdefs/ageadjustment.htm (accessed 2007 May 3).
- 26.Bunch TJ, White RD, Gersh BJ, et al. Long-term outcomes of out-of-hospital cardiac arrest after successful early defibrillation. N Engl J Med 2003;348:2626-33. [DOI] [PubMed]
- 27.Rouleau JL, Moye LA, Pfeffer MA, et al; the SAVE investigators. A comparison of management patterns after acute myocardial infarction in Canada and the United States. N Engl J Med 1993;328:779-84. [DOI] [PubMed]
- 28.Tu JV, Pashos CL, Naylor CD, et al. Use of cardiac procedures and outcomes in elderly patients with myocardial infarction in the United States and Canada. N Engl J Med 1997;336:1500-5. [DOI] [PubMed]
- 29.Ruskin JN, Camm AJ, Zipes DP, et al. Implantable cardioverter defibrillator utilization based on discharge diagnoses from Medicare and managed care patients. J Cardiovasc Electrophysiol 2002;13:38-43. [DOI] [PubMed]
- 30.Daly C, Clemens F, Lopez Sendon JL, et al. Gender differences in the management and clinical outcome of stable angina. Circulation 2006;113:490-8. [DOI] [PubMed]
- 31.Gan SC, Beaver SK, Houck PM, et al. Treatment of acute myocardial infarction and 30-day mortality among women and men. N Engl J Med 2000;343:8-15. [DOI] [PubMed]
- 32.Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med 2005;353:671-82. [DOI] [PMC free article] [PubMed]
- 33.Davis DR, Tang AS, Lemery R, et al. Influence of gender on ICD implantation for primary and secondary prevention of sudden cardiac death. Europace 2006;8:1054-6. [DOI] [PubMed]
- 34.Pires LA, Sethuraman B, Guduguntla VD, et al. Outcome of women versus men with ventricular tachyarrhythmias treated with the implantable cardioverter defibrillator. J Cardiovasc Electrophysiol 2002;13:563-8. [DOI] [PubMed]
- 35.Oxman AD, Thomson MA, Davis DA, et al. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ 1995;153:1423-31. [PMC free article] [PubMed]
- 36.Larsen G, Hallstrom A, McAnulty J, et al. Cost-effectiveness of the implantable cardioverter–defibrillator versus antiarrhythmic drugs in survivors of serious ventricular tachyarrhythmias: results of the Antiarrhythmics Versus Implantable Defibrillators (AVID) economic analysis substudy. Circulation 2002;105:2049-57. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


