Abstract
Context: The sensorimotor system controls the balance between upper extremity stability and mobility during athletic performance. Research indicates that fatigue hampers sensorimotor system function; however, few investigators have studied functional fatigue or multijoint, multiplanar measures.
Objective: To examine the effect of functional fatigue on upper extremity position reproduction in overhead throwing athletes.
Design: Single-session, repeated-measures design.
Setting: University musculoskeletal laboratory.
Patients or Other Participants: Sixteen healthy collegiate baseball players (age = 21.0 ± 1.6 years, height = 175.8 ± 10.2 cm, mass = 82.8 ± 4.3 kg).
Intervention(s): Subjects threw a baseball from a single knee with maximum velocity (every 5 seconds) and rated their level of upper extremity exertion after every 20 throws. Subjects stopped after reporting above level 14 on the Borg scale and began posttests immediately.
Main Outcome Measure(s): We measured active multijoint reproduction of 2 positions: arm cock and ball release. Dependent variables were absolute and variable error for 10 joint motions: scapulothoracic internal-external rotation, upward rotation, and posterior tilt; glenohumeral internal-external rotation, horizontal abduction-adduction, and flexion-extension; elbow pronation-supination and flexion-extension; and wrist ulnar-radial deviation and flexion-extension. We calculated acuity for each joint and the entire upper extremity using 3-dimensional variable error.
Results: Fatigue occurred after an average of 62 ± 28 throws and increased 3-dimensional variable error scores (ie, decreased acuity) of the entire upper extremity and all joints in both positions (P < .05) except for the wrist in arm cock. Fatigue increased errors (ranging from 0.6° to 2.3°) at arm cock for scapulothoracic internal-external rotation, upward rotation, and posterior tilt; glenohumeral internal-external rotation and flexion-extension; elbow flexion-extension; and wrist ulnar-radial deviation and at ball release for scapulothoracic internal-external rotation and upward rotation, glenohumeral horizontal abduction-adduction, elbow pronation-supination, and wrist ulnar-radial deviation and flexion-extension (P < .05).
Conclusions: Functional fatigue affects the acuity of the entire upper extremity, each individual joint, and multiple joint motions in overhead throwers. Clinicians should consider the deleterious effects of upper extremity fatigue when designing injury prevention and rehabilitation programs and should incorporate multijoint and multiplanar endurance exercises. Compromised neuromuscular control of the scapulohumeral relationship may hold pathologic implications for this population as well.
Keywords: proprioception, multijoint position reproduction, overhead throwing athletes
Key Points
After a bout of repeated throws, fatigue decreased sensorimotor system acuity over the upper extremity and at the scapulothoracic, glenohumeral, elbow, and wrist joints.
Fatigue diminished position sense at the scapulothoracic and glenohumeral joints in planes of motion that may have implications for the labral, subacromial, and internal impingement conditions common in throwers.
Rehabilitation and conditioning programs for throwers should include multijoint, multiplanar exercises that address sensorimotor system control and endurance.
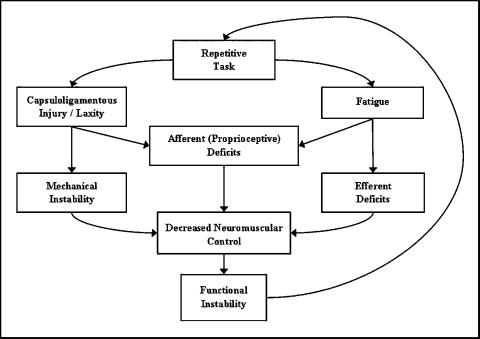
The overhead throw is a complex sequence of proximal to distal force and moment interrelations, with the goal of transferring energy from the lower extremity and trunk up and through the upper extremity.1 Competitive throwers experience forces approaching 100% body weight at the elbow and even greater force at the shoulder.2,3 The upper extremity must effectively control and transfer these forces to sustain performance and avoid injury. Maintaining proper throwing form helps to efficiently disperse such forces.3 The sensorimotor system (SMS) is responsible for providing the awareness, coordination, and feedback to maintain such form and stability, thereby serving as a major component of injury-free athletic performance.4 Evidence indicates that joint injury compromises SMS function.5,6 The compromised structural and dynamic stability seen with such injuries may render the involved joint even more unstable.7 These events are described in the cyclic paradigm of functional stability,8 which indicates that joint injury or laxity leads to proprioceptive deficits, functional instability, further injury, and compromised structural stability. Fatigue seems to hamper upper extremity SMS function in ways similar to joint injury.6,9–13 In overhead throwing athletes, SMS deficits may result in the inability to appreciate and maintain the ideal mechanics that should accompany prolonged throwing.14 Such breakdowns in throwing mechanics result in undue stress to the upper extremity2,3,14 and may contribute to the high rates of upper extremity injuries suffered by National Collegiate Athletic Association baseball players.15
The relationships among injuries, fatigue, and the SMS are illustrated in a model of functional stability (Figure 1) derived from the current literature.8 This model indicates that injury or fatigue may affect the SMS both directly and indirectly, hampering neuromuscular control and leading to functional instability. Through this model, researchers and clinicians can appreciate the effects of fatigue and can begin to identify areas in which interventions may be appropriate. However, this model is derived from the results of research that may not apply to overhead athletes. To validate a model that applies to overhead throwers, we must use more functional research methods. To do so, we must address several variables in commonly used measures that may threaten external validity and significantly alter results, including body support, movement restrictions during testing, and the nature of the fatigue protocol.
Figure 1. Model of functional stability, integrating the role of fatigue into the paradigm.
The external body support and movement restrictions required by some testing instruments may affect SMS acuity. Subjects are often tested while strapped to the equipment, in either a seated10 or a supine5,6,16 position, with motion restricted at both adjacent joints.5,10,16 Such measures, while isolating specific joints and single motions for observation, may not represent SMS function during complex multijoint, multidimensional tasks. Three-dimensional, multijoint measures may provide additional insights.
A functional measure of SMS acuity in overhead throwers should include an unsupported body, unconstrained multijoint motion, and actively identified and reproduced practical test positions. We chose to use previously described methods employing active, unconstrained, functional methods.13,17,18 Additionally, to gain a more comprehensive representation of SMS function over the entire upper extremity, we measured reposition acuity simultaneously in multiple planes of motion at the scapulothoracic, glenohumeral, elbow, and wrist joints.
Traditional observations of the effects of fatigue on SMS function isolate single-plane and single-joint motions to induce fatigue and measure acuity.6,11 Such methods do not allow the natural strategy of reorganizing muscle activity to prolong performance.9,19 We chose to use a previously described unconstrained functional throwing fatigue protocol.13
Research investigating the specific effects of fatigue induced using a functional multijoint activity is lacking. Therefore, the purposes of our investigation were to observe the effects of functional fatigue in overhead throwers on active position reproduction acuity of the following: (1) the overall upper extremity, (2) each joint (scapulothoracic, glenohumeral, elbow, and wrist), and (3) each plane of motion within the individual joints. We believed that fatigue would decrease SMS acuity in multiple joints and planes. Measuring the effects on acuity of the upper extremity as a functional unit as well as on individual joints allows us to observe whether overall acuity is maintained despite deficits at one or more joints. This model will also afford comparisons among the individual joints and planes of motion, indicating which joints were more affected by fatigue. These observations may provide insight into pathomechanics and may hold implications for rehabilitation strategies in overhead throwing athletes.
METHODS
Subjects
Subjects were 16 male, overhead-throwing athletes (age = 21.0 ± 1.6 years, height = 175.8 ± 10.2 cm, mass = 82.8 ± 4.3 kg). All subjects volunteered and participated in the study within 1 year of competing in National Collegiate Athletic Association baseball. Subjects reported 2.3 ± 1.2 years of experience in National Collegiate Athletic Association baseball and 15 ± 1.4 total years of baseball experience. Subjects were 14 right-handed and 2 left-handed throwers, including 6 pitchers, 5 infielders, and 5 outfielders. All testing took place during the November-December off-season. All participants were healthy and presented with no history of upper extremity injury or surgery or central nervous system disorder. We explained the test protocol, and each participant signed an informed consent form. The university's Institutional Review Board for the Social and Behavioral Sciences approved this study.
Procedures
All subjects reported to the University Musculoskeletal Research Laboratory for testing. We used a single-session repeated-measures design. The dependent variables were 50 measures of position sense acuity. For each test position (2), we calculated 25 acuity scores, including absolute and variable error for each joint motion (10) and 3-dimensional variable error (3DVE) for each upper extremity joint (4) and for the entire extremity (1). The independent variable was condition at 2 levels (prefatigue and postfatigue). We used a Flock of Birds electromagnetic tracking device (Ascension Technology, Burlington, VT) with MotionMonitor software (Innovative Sports Training, Chicago, IL) to test active multijoint position reproduction acuity. We collected data at 100 Hz and used a fourth-order zero-phase-shift Butterworth filter (20-Hz cutoff) to smooth positional and angular data. To assure accuracy of sensor data, we tested subjects within the validated (metal-mapped) collection field. Using double-backed and Coverroll tape (Beiersdorf Inc, Norwalk, CT), we applied 3 sensors to each subject at the sternal notch, at the dominant side at the posterior acromial angle of the scapula, and at the dorsal aspect of the third metacarpal. Elastic rubber cuffs (2 in [5.08 cm] in width) sprayed with Tuf-Skin (Cramer Products Inc, Gardner, KS) held additional sensors to the distal lateral humerus and the distal posterior aspect of the radius. We used the elastic cuffs to stabilize cords from distal sensors to help limit sensory feedback from the cords.
After the instrumentation process, we asked subjects to warm up normally, including throwing and stretching until they were comfortable throwing at their maximum velocity. Using a wooden stylus to identify landmarks, we then digitized subjects, creating local and then anatomically relevant coordinate systems for the thorax and each involved segment. We followed the International Society of Biomechanics' standard protocol20 for identifying and determining upper extremity coordinate systems and Euler rotation sequences. This method is a valid21 and reliable17 measure of scapular and humeral motion.
Active Multijoint Position Reproduction Measure
We used the previously described active multijoint position reproduction test17 to assess subjects' ability to recreate 2 upper extremity positions. Subjects knelt in a single-knee stance for the test as well as for the throwing protocol to assure a standard and appropriate distance (within the collection field) between subjects and the transmitter and continuity between the test and throwing position. We defined the positions as follows: kneeling with the nondominant hip flexed to 90°, foot placed flat on the ground in front of the subject, and the knee on the side of the throwing shoulder on the ground.17 We instructed subjects to maintain 90° angles at both knees.
We tested subjects' ability to reproduce their arm cocked (Figure 2) and ball release positions (Figure 3) individually. We chose these 2 specific positions because they are critical to the throwing motion, with large-magnitude forces experienced by the shoulder and elbow.3 Neuromuscular control and stability is, therefore, critical at these 2 vulnerable positions in order to avoid injury. We described the arm cocked position as “the position at which forward acceleration of your arm would begin” and the ball release position as “the position at which you release the ball, your release point.” To control for any biasing of test sequence, we counterbalanced the order of the 2 test positions. During this identification of the initial target trial, investigators instructed subjects that they were to “recreate this position” during the 3 trials to follow. We gave these specific instructions to avoid creating bias toward any one segment or joint angle and to ensure each subject's conscious appreciation of the target position. We blindfolded subjects and prompted them to actively go through the throwing motion, to pause for approximately 1 second, and then to press the trigger in the nonthrowing hand when they believed they had recreated the position. We used the trigger (a single frame) during this initial trial to identify the target position of each upper extremity joint and angle for each axis of rotation for the 3 repositioning trials to follow. Subjects identified each position 4 times (a target and 3 repositioning trials). They remained blindfolded between trials, each of which began within 5 seconds of the previous trial. The time between identification of a target position and completion of all repositioning trials did not exceed 20 seconds. We did not provide results or any feedback regarding acuity of individual trials at any time.
Figure 2. An overhead throwing athlete reproducing his arm cocked position during the active multijoint position reproduction test.
Figure 3. An overhead throwing athlete reproducing his ball release position during the active multijoint position reproduction test.
Functional Fatigue Protocol
Before beginning the fatigue protocol, we provided subjects with written and verbal instructions for using the Borg Rating of Perceived Exertion scale.22 Subjects used the scale ratings of 6 to 20 to indicate the level of “local” exertion or fatigue in the throwing arm during the throwing protocol. This scale is a valid measure of local upper extremity exertion.23,24
The functional fatigue protocol consisted of a single bout of throwing baseballs (Rawlings Sporting Goods Co, Inc, St Louis, MO; circumference = 9 in [22.86 cm], mass = 5 oz [0.14 kg]) at a 17-in [43.18-cm] target located 20 feet (6.10 m) away. To expedite fatigue of the upper extremity and to maintain continuity between the test and throwing positions, subjects threw from the single-knee stance position. We asked subjects to throw with maximum velocity and accuracy when prompted by the tester (every 5 seconds). Investigators used a radar gun (JUGS Pitching Machine Company, Tualatin, OR), following the manufacturer's guidelines, to measure ball velocity. The radar gun has a manufacturer-reported accuracy of ±0.5 mph (±0.22 m/s). We allowed subjects 3 to 5 throws to become familiar with the procedures and to establish a goal velocity. We considered the maximum of these throws to be the subject's goal velocity. To encourage continuous effort during the throwing program, we warned participants if the velocity fell below 90% of the goal. After every 20 throws, we asked subjects to rate their fatigue level. We considered subjects fatigued, ending the throwing protocol, when they reported an exertion level exceeding 14 or after 160 throws. A rating of 15 on the Rating of Perceived Exertion scale corresponds with “hard/heavy work or strain and fatigue on muscles.”22 We did not inform subjects of the level of fatigue used as a threshold.
Immediately after the throwing protocol, we retested participants in the same manner as for the prefatigue measures. We began testing within 1 minute after the fatigue protocol and completed the posttest for both positions within 3 minutes.
Data Reduction and Statistical Analysis
We exported angular and position data from the MotionMonitor into Microsoft Excel (version 2000; Microsoft Corp, Redmond, WA) to calculate error scores. We calculated variable error and absolute error differences (in degrees) between the target and repositioned joint angles in each plane of motion available within each joint.25,26 Variable error represents consistency or variability in repositioning trials, and absolute error represents overall accuracy. We calculated error in 3 planes at the scapulothoracic (internal-external rotation, upward-downward rotation, anterior-posterior tilt) and glenohumeral joints (internal-external rotation, horizontal abduction-adduction [ie, plane of elevation], flexion-extension) and in 2 planes at the elbow (pronation-supination, flexion-extension) and wrist joints (ulnar-radial deviation, flexion-extension).
We calculated separate 3DVE13,27 to represent acuity of the entire upper extremity for each test position (arm cock and ball release) and acuity at each joint. We used hand position (ie, dispersion of endpoint position) in relation to the thorax to measure overall upper extremity acuity (in millimeters) for each position (arm cock and ball release).13,27 Errors in 3-dimensional angular orientation were calculated for each joint (scapulothoracic, glenohumeral, elbow, and wrist) using 3DVE. These scores assess deviation of end-position dispersions, with overall acuity 3DVE reflecting how well the entire upper extremity achieved its goal and individual joint 3DVE reflecting acuity at each joint.13,27
We performed statistical analyses using SPSS software (version 10.0; SPSS Inc, Chicago, IL). Because 56% of the variables violated the assumption of normality and 22% violated the assumption of homogeneity of variances, nonparametric tests were appropriate. For each measure of acuity (variable error, absolute error, and 3DVE) and each test position, we used a Wilcoxon matched-pairs signed-rank test (nonparametric repeated-measures analysis of variance) to obtain Z scores and the Dunn correction for multiple comparisons to observe differences between prefatigue and postfatigue error scores. We set the statistical significance for all comparisons at P < .05 a priori. We calculated the effect size for fatigue using standard calculations.28
RESULTS
Subjects reported a rating of upper extremity exertion exceeding 14 (the predetermined threshold) after an average of 62 ± 28 throws. Subjects' average target velocity was 60 ± 5 miles/h (27.7 ± 2.2 m/s). No subjects reached the 160-throw limit, nor did any fail to maintain a throwing velocity within 90% of their target when prompted. Subjects were fatigued after 140 (n = 1), 100 (n = 1), 80 (n = 2), 60 (n = 7), 40 (n = 4), and 20 (n = 1) throws.
The Effect of Fatigue on Overall Upper Extremity Acuity
The first purpose of this study was to observe the effects of fatigue on overall position reproduction of the upper extremity. Fatigue significantly increased 3DVE error scores (decreased endpoint reproduction acuity) of the arm cocked position (12.4 mm prefatigue to 24.1 mm postfatigue) (Z = 3.31, P < .001, effect size = 1.71) and ball release position (20.8 mm prefatigue to 41.7 mm postfatigue) (Z = 3.52, P < .001, effect size = 2.79).
The Effect of Fatigue on Joint Acuity
The second purpose of this study was to observe the effects of fatigue on joint position sense acuity of upper extremity joints. Fatigue significantly increased 3DVE (decreased acuity) in the arm cocked position for the scapulothoracic, glenohumeral, and elbow joints (P < .05) (Figures 4 and 5). The only joint not significantly affected by fatigue was the wrist (Z = 1.03, P = .15, β = .15). For reproduction of the ball release position, fatigue significantly increased 3DVE for each joint (P < .05).
Figure 4. Prefatigue and postfatigue 3-dimensional variable error score means (degrees) for the scapulothoracic, glenohumeral, elbow, and wrist joints in the arm cock position. *Indicates significant difference between scapulothoracic prefatigue and postfatigue error scores (P < .05); †, significant difference between glenohumeral prefatigue and postfatigue error scores (P < .05); and ‡, significant difference between elbow prefatigue and postfatigue error scores (P < .05).
Figure 5. Prefatigue and postfatigue 3-dimensional variable error score means (degrees) for the scapulothoracic, glenohumeral, elbow, and wrist joints in the ball release position. *Indicates significant difference between scapulothoracic prefatigue and postfatigue error scores (P < .05); †, significant difference between glenohumeral prefatigue and postfatigue error scores (P < .05); ‡, significant difference between elbow prefatigue and postfatigue error scores (P < .05); and §, significant difference between wrist prefatigue and postfatigue error scores (P < .05).
The Effect of Fatigue on Acuity for Individual Planes of Motion
To observe the effects of fatigue on acuity in each individual plane of motion within the 4 joints, we compared prefatigue and postfatigue acuity error scores (Tables 1 and 2). Fatigue significantly increased variability for the arm cocked position in all planes of scapulothoracic motion, glenohumeral internal-external rotation, elbow flexion-extension, and wrist deviation (P < .05) (Table 1). For the ball release position, fatigue significantly increased variability in scapulothoracic upward-downward rotation and wrist deviation (P < .05) (Table 2). Fatigue significantly decreased accuracy for the arm cocked position in scapulothoracic internal-external rotation and anterior-posterior tilt and glenohumeral flexion-extension and internal-external rotation (P < .05) (Table 3). For the ball release position, fatigue significantly decreased accuracy in scapulothoracic internal-external rotation, glenohumeral horizontal abduction-adduction, elbow pronation-supination, and wrist flexion-extension (P < .05) (Table 4).
Table 1. Prefatigue and Postfatigue Variable Error Scores in the Arm Cocked Position (Mean ± SD).
Table 2. Prefatigue and Postfatigue Variable Error Scores in the Ball Release Position (Mean ± SD).
Table 3. Prefatigue and Postfatigue Absolute Error Scores in the Arm Cocked Position (Mean ± SD).
Table 4. Prefatigue and Postfatigue Absolute Error Scores in the Ball Release Position (Mean ± SD).
DISCUSSION
The first purpose of this study was to observe the effects of functional fatigue on overall acuity of the upper extremity in reproducing the arm cocked and ball release positions. Fatigue decreased overall endpoint acuity and had a large effect on replication of both positions, which may support the theory that muscle mechanoreceptors contribute to position sense toward the end range of motion.26,29 The endpoint error scores we observed are similar to those previously reported17 and indicate that errors accrued over multiple joints and planes. The magnitude of such errors indicates that any interactions among joints or planes of motion could not compensate for deficits elsewhere to maintain overall acuity. Testing methods that focus on single-joint motions do not allow such observations. Unless the bulk of errors arise from a single upper extremity joint, such myopic measures may not represent the entire upper extremity.
To enhance our appreciation, we must assess all joint(s) contributing to the task. Therefore, the second purpose of our study was to examine the effects of fatigue on acuity for the scapulothoracic, glenohumeral, elbow, and wrist joints simultaneously. Our observation that fatigue affected endpoint acuity leads us to question whether fatigue affected each joint similarly. In the arm cocked position, fatigue decreased acuity of the scapulothoracic, glenohumeral, and elbow joints. Although fatigue had a greater effect on the glenohumeral joint than the scapulothoracic and elbow joints, we observed large effect sizes for all 3 joints (effect sizes = 7.42, 3.08, and 2.64, respectively). In the ball release position, fatigue had a large effect on each of the 4 joints. Because this position is in the midrange of motion for multiple glenohumeral and wrist motions, this observation supports the theory that positions in the midrange of joint motion rely heavily on afferent information arising from muscle mechanoreceptors.26 Fatigue may have affected the acuity of all 4 joints by desensitizing the muscular receptors on which they rely. Our observation that fatigue decreased the acuity of multiple upper extremity joints indicates that endurance and SMS control exercises should not focus exclusively on single joints. Clinicians designing rehabilitation and prevention programs should therefore address the upper extremity as a functional unit.
Although our observations that fatigue diminished position sense over multiple joints are unique, we can investigate further and identify the planes of motion affected within each joint. By comparing the effects among planes of motion, we may gain further insight into some common conditions. Of particular interest in this regard are the deficits we observed in the arm cocked position. In overhead throwers, this position is implicated as a factor contributing to injuries, including subacromial30,31 and posterior30–32 impingement, as well as to tears of the glenoid labrum.31,33 In the arm cocked position, throwers experience 250 N of superior shear force,3 which attempts to drive the humerus into the acromial arch. Failure to maintain sufficient space between the acromial arch and humeral head leads to subacromial impingement.34 This space is maintained by controlling humeral orientation in relation to the scapula, with inadequate scapular upward rotation or posterior tilt increasing the risk of subacromial impingement.34 We observed significant SMS acuity deficits in each of these planes of motion after fatigue, perhaps providing further insight into the development of subacromial impingement.
An inability to maintain the relationship between the scapula and humerus in the horizontal plane during arm cocking may hold implications for other common conditions. During throwing, anterior shear force at the shoulder in excess of 350 N3,35 challenges glenohumeral stability in the horizontal plane. Failure to control these forces provides a mechanism for posterior internal impingement when the posterior glenoid labrum contacts the underside of the rotator cuff, which may lead to fraying.31 Additionally, Kuhn et al33 observed that the arm cocked position places the labrum in a precarious orientation that allows it to be torn from the glenoid with less force than when it is in the ball release position. It is clear that during arm cocking, the glenohumeral joint is in a vulnerable position, making dynamic stability critical. Our results indicate, however, that fatigue decreased SMS acuity of the scapulothoracic and glenohumeral joints, directly affecting the orientation of the humerus to the glenoid. Fatigue had a large effect on the acuity of both glenohumeral rotation and flexion in the arm cocked position. Additionally, fatigue significantly decreased the acuity of scapular motion in all 3 planes, thereby affecting the ability to control the position of the glenoid.
At the elbow joint, fatigue had a large effect on variability in flexion in the arm cocked position. When coupled with past findings, this observation may further our understanding of medial collateral ligament injuries. During the overhead throw, the elbow experiences more than 300 N of medial shear force in the arm cocked position.3 We also understand that the magnitude of this force increases significantly with decreased elbow flexion.36 Without adequate acuity of elbow flexion, overhead throwers may not control the magnitude of medial shear force, thereby placing the medial collateral ligament at risk.
In the ball release position we observed significantly decreased accuracy in the horizontal plane at the scapulothoracic (internal rotation) and glenohumeral (horizontal abduction-adduction) joints. The inability to maintain the relationship between the scapula and humerus in the horizontal plane in a similar arm position is associated with subacromial impingement.37 Interestingly, the failure to maintain this same relationship in the horizontal plane at ball release is a common sign of fatigue in overhead throwers. This breakdown in throwing mechanics may coincide with decreased performance and is described by experienced coaches as a wide arm path38 or a slow arm.39
Although our general observation that fatigue affects position sense is not unique, we observed decreased neuromuscular control after fatigue at multiple joints and planes of motion of the upper extremity. We can integrate these findings into the model of overuse functional stability (Figure 1). However, the mechanisms by which fatigue affects SMS function are largely theoretical. Authors have proposed that changes at the central40 or mechanoreceptor41,42 level may be responsible for such deficits. Although limited, many theories suggest that fatigue desensitizes muscle spindles as a result of altered stiffness, temperature, and chemical environment.26,41–43 Noninvasive measures, however, are unable to differentiate between afferent or efferent mechanisms. Therefore, the deficits we observed after fatigue represent the combined effects through both afferent and efferent mechanisms.
Limitations
Our results are limited to healthy, male National Collegiate Athletic Association baseball players with no history of upper extremity injury or surgery. We tested athletes during the off-season, but the rigors of a demanding in-season schedule may affect results. As with any standardized fatigue protocol, our functional fatigue protocol may not represent actual experience. Subjects threw every 5 seconds at maximal effort from a single-knee position to expedite the onset of fatigue. Our active multijoint position reproduction measure reflects specific afferent and efferent components of the SMS; however, it does not differentiate between the two, nor does it assess additional submodalities of the system.
Future Research
Future SMS researchers should consider using multijoint, 3-dimensional measures as well as functional fatigue protocols to (1) compare throwers with injured shoulders with uninjured controls and (2) examine the relationship between SMS acuity and the development of throwing-related injuries. Investigators should evaluate the effect of interventions, such as therapeutic or injury-prevention protocols and surgery, on similar measures of SMS acuity. Future research is necessary to observe the rate at which joint position sense recovers after fatigue. Examining differences in acuity among populations (age, sex, and activity level) would also add to our understanding of SMS function.
CONCLUSIONS
The purpose of our study was to observe the effects of fatigue on SMS acuity in overhead throwers with functional measures. We used a functional fatigue protocol and measured multijoint reposition acuity of 2 self-selected, unconstrained upper extremity positions. Fatigue decreased overall upper extremity acuity in both positions we tested. Fatigue also affected the reposition acuity of the scapulothoracic, glenohumeral, elbow, and wrist joints individually. We observed decreased accuracy and increased variability after fatigue in multiple planes of motion in these upper extremity joints. These results indicate that fatigue affects proximal and distal joints over several planes of motion during unconstrained active repositioning tasks. Therefore, in their rehabilitative or preventive efforts to enhance endurance and SMS control, clinicians should address the entire upper extremity using multijoint multiplanar exercises. Additionally, clinicians may consider incorporating exercises that emphasize a functional range of motion or multiple upper extremity positions. In general, our findings indicate that fatigue affects the upper extremity at more joints and planes than are observed using traditional insular single-plane measures. We suggest adopting more functional research methods to achieve more readily applicable results.
REFERENCES
- Putnam CA. Sequential motions of body segments in striking and throwing skills: descriptions and explanations. J Biomech. 1993;26((suppl 1)):125–135. doi: 10.1016/0021-9290(93)90084-r. [DOI] [PubMed] [Google Scholar]
- Werner SL, Gill TJ, Murray TA, Cook TD, Hawkins RJ. Relationships between throwing mechanics and shoulder distraction in professional baseball pitchers. Am J Sports Med. 2001;29:354–358. doi: 10.1177/03635465010290031701. [DOI] [PubMed] [Google Scholar]
- Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Riemann BL, Fu FH. Proprioception and Neuromuscular Control in Joint Stability. Champaign, IL: Human Kinetics; 2000.
- Lephart SM, Warner JP, Borsa PA, Fu FH. Proprioception of the shoulder joint in healthy, unstable, surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371–380. doi: 10.1016/S1058-2746(09)80022-0. [DOI] [PubMed] [Google Scholar]
- Voight ML, Hardin JA, Blackburn TA, Tippett S, Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23:348–352. doi: 10.2519/jospt.1996.23.6.348. [DOI] [PubMed] [Google Scholar]
- Borsa PA, Lephart SM, Kocher MS, Lephart SP. Functional assessment and rehabilitation of shoulder proprioception for glenohumeral instability. J Sport Rehabil. 1994;3:84–104. [Google Scholar]
- Lephart S, Henry T. The physiological basis for open and closed kinetic chain rehabilitation for the upper and lower extremity. J Sport Rehabil. 1992;5:71–87. [Google Scholar]
- Forestier N, Nougier V. The effects of muscular fatigue on the coordination of a multijoint movement in humans. Neurosci Lett. 1998;252:187–190. doi: 10.1016/s0304-3940(98)00584-9. [DOI] [PubMed] [Google Scholar]
- Carpenter JE, Blasier RB, Pellizzon GG. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med. 1998;26:262–265. doi: 10.1177/03635465980260021701. [DOI] [PubMed] [Google Scholar]
- Pedersen J, Lonn J, Hellstrom F, Djupsjobacka M, Johansson H. Localized muscle fatigue decreases the acuity of the movement sense in the human shoulder. Med Sci Sports Exerc. 1999;31:1047–1052. doi: 10.1097/00005768-199907000-00019. [DOI] [PubMed] [Google Scholar]
- Myers JB, Guskiewicz KM, Schneider RA, Prentice WE. Proprioception and neuromuscular control of the shoulder after muscle fatigue. J Athl Train. 1999;34:362–367. [PMC free article] [PubMed] [Google Scholar]
- Tripp BL, Boswell L, Gansneder BM, Shultz SJ. Functional fatigue decreases 3-dimensional multijoint position reproduction acuity in the overhead-throwing athlete. J Athl Train. 2004;39:316–320. [PMC free article] [PubMed] [Google Scholar]
- Murray TA, Cook TD, Werner SL, Schlegel TF, Hawkins RJ. The effects of extended play on professional baseball pitchers. Am J Sports Med. 2001;29:137–142. doi: 10.1177/03635465010290020501. [DOI] [PubMed] [Google Scholar]
- National Collegiate Athletic Association. National Collegiate Athletic Association 2000–01 Injury Surveillance System. Overland Park, KS: National Collegiate Athletic Association; 2001.
- Smith RL, Brunolli J. Shoulder kinesthesia after anterior glenohumeral joint dislocation. Phys Ther. 1989;69:106–112. doi: 10.1093/ptj/69.2.106. [DOI] [PubMed] [Google Scholar]
- Tripp BL, Uhl TL, Mattacola CG, Srinivasan C, Shapiro R. Functional multijoint position reproduction acuity in overhead-throwing athletes. J Athl Train. 2006;41:146–153. [PMC free article] [PubMed] [Google Scholar]
- Tripp BL, Uhl TL, Mattacola CG, Srinivasan C, Shapiro R. A comparison of individual joint contributions to multijoint position reproduction acuity in overhead-throwing athletes. Clin Biomech (Bristol, Avon) 2006;21:466–473. doi: 10.1016/j.clinbiomech.2005.12.015. [DOI] [PubMed] [Google Scholar]
- Bente J, Bjarne L, Sjogaard G. Aspects of shoulder function in relation to exposure demands and fatigue—a mini review. Clin Biomech (Bristol, Avon) 2000;15((suppl 1)):17–20. doi: 10.1016/s0268-0033(00)00054-1. [DOI] [PubMed] [Google Scholar]
- Wu G, van der Helm FC, Veeger HE. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion, part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. et al. [DOI] [PubMed] [Google Scholar]
- Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: a validation study. J Biomech Eng. 2001;123:184–190. doi: 10.1115/1.1351892. [DOI] [PubMed] [Google Scholar]
- Borg G. Borg's Perceived Exertion and Pain Scales. Champaign, IL: Human Kinetics; 1998.
- Kang J, Chaloupka EC, Mastrangelo MA, Donnelly MS, Martz WP, Robertson RJ. Regulating exercise intensity using ratings of perceived exertion during arm and leg ergometry. Eur J Appl Physiol Occup Physiol. 1998;78:241–246. doi: 10.1007/s004210050414. [DOI] [PubMed] [Google Scholar]
- Marais G, Weissland T, Robin H, Vanvelcenaher JM, Lavoie JM, Pelayo P. Physiological effects of variations in spontaneously chosen crank rate during submaximal and supramaximal upper body exercises. Int J Sports Med. 1999;19:239–245. doi: 10.1055/s-2007-971124. [DOI] [PubMed] [Google Scholar]
- Schmidt RA, Lee TD. Motor Control and Learning: A Behavioral Emphasis. Champaign, IL: Human Kinetics; 1999.
- Janwantanakul P, Jones M, Magarey M, Miles T. Characteristics of shoulder-position sense: effects of mode of movement, scapular support, and arm orientation. J Sport Rehabil. 2002;11:157. [Google Scholar]
- Adamovich SV, Berkinblit MB, Fookson O, Poizner H. Pointing in 3D space to remembered targets. II: effects of movement speed toward kinesthetically defined targets. Exp Brain Res. 1999;125:200–210. doi: 10.1007/s002210050674. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press; 1969.
- Sargant D. Proprioception: how does it work? Australas J Podiatr Med. 2000;34:86–92. [Google Scholar]
- Jobe FW, Kvitne RS, Giangarra CE. Shoulder pain in the overhand or throwing athlete: the relationship of anterior instability and rotator cuff impingement. Orthop Rev. 1989;18:963–975. [PubMed] [Google Scholar]
- Meister K. Internal impingement in the shoulder of the overhand athlete: pathophysiology, diagnosis, and treatment. Am J Orthop. 2000;29:433–438. [PubMed] [Google Scholar]
- Jobe CM. Posterior superior glenoid impingement: expanded spectrum. Arthroscopy. 1995;11:530–536. doi: 10.1016/0749-8063(95)90128-0. [DOI] [PubMed] [Google Scholar]
- Kuhn JE, Lindholm SR, Huston LJ, Soslowsky LJ, Blasier RB. Failure of the biceps superior labral complex: a cadaveric biomechanical investigation comparing the late cocking and early deceleration positions of throwing. Arthroscopy. 2003;19:373–379. doi: 10.1053/jars.2003.50044. [DOI] [PubMed] [Google Scholar]
- Meskers CG, van der Helm FC, Rozing PM. The size of the supraspinatus outlet during elevation of the arm in the frontal and sagittal plane: a 3-D model study. Clin Biomech (Bristol, Avon) 2002;17:257–266. doi: 10.1016/s0268-0033(02)00021-9. [DOI] [PubMed] [Google Scholar]
- Fleisig GS, Barrentine SW, Zheng N, Escamilla RF, Andrews JR. Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech. 1999;32:1371–1375. doi: 10.1016/s0021-9290(99)00127-x. [DOI] [PubMed] [Google Scholar]
- Werner SL, Murray TA, Hawkins RJ, Gill TJ. Relationship between throwing mechanics and elbow valgus in professional baseball pitchers. J Shoulder Elbow Surg. 2002;11:151–155. doi: 10.1067/mse.2002.121481. [DOI] [PubMed] [Google Scholar]
- Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- Thurston B. The fine art of pitching: coach's perspective. In: Andrews J, Zarins B, Wilk K, eds. Injuries in Baseball. Philadelphia, PA: Lippincott-Raven; 1998:589–603.
- Mazzone L. Pitch Like a Pro. New York, NY: St. Martin's Griffin; 1999.
- Macefield G, Hagbarth KE, Gorman R, Gandevia SC, Burke D. Decline in spindle support to alpha-motoneurones during sustained voluntary contractions. J Physiol. 1991;440:497–512. doi: 10.1113/jphysiol.1991.sp018721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljubisavljevic M, Vukcevic IS, Radovanovic S, Milanovic S, Anastasijevic R. Effects of cutaneous afferent input on fatigue-induced changes in fusimotor activity of decerebrate cats. Neuroscience. 1997;79:935–942. doi: 10.1016/s0306-4522(97)00039-0. [DOI] [PubMed] [Google Scholar]
- Nelson DL, Hutton RS. Dynamic and static stretch responses in muscle spindle receptors in fatigued muscle. Med Sci Sports Exerc. 1985;17:445–450. doi: 10.1249/00005768-198508000-00007. [DOI] [PubMed] [Google Scholar]
- Taylor JL, Butler JE, Gandevia SC. Changes in muscle afferents, motoneurons and motor drive during muscle fatigue. Eur J Appl Physiol. 2000;83:106–115. doi: 10.1007/s004210000269. [DOI] [PubMed] [Google Scholar]