Abstract
Context: Application of cryotherapy modalities is common after acute shoulder injury and as part of rehabilitation. During athletic events, athletes may return to play after this treatment. The effects of cryotherapy on dominant shoulder proprioception have been assessed, yet the effects on throwing performance are unknown.
Objective: To determine the effects of a cryotherapy application on shoulder proprioception and throwing accuracy.
Design: Single-group, pretest-posttest control session design.
Setting: University-based biomechanics laboratory.
Patients or Other Participants: Healthy college-aged subjects (n = 22).
Intervention(s): Twenty-minute ice pack application to the dominant shoulder.
Main Outcome Measure(s): Active joint position replication, path of joint motion replication, and the Functional Throwing Performance Index.
Results: Subjects demonstrated significant increases in deviation for path of joint motion replication when moving from 90° of abduction with 90° of external rotation to 20° of flexion with neutral shoulder rotation after ice pack application. Also, subjects exhibited a decrease in Functional Throwing Performance Index after cryotherapy application. No differences were found in subjects for active joint position replication after cryotherapy application.
Conclusions: Proprioception and throwing accuracy were decreased after ice pack application to the shoulder. It is important that clinicians understand the deficits that occur after cryotherapy, as this modality is commonly used following acute injury and during rehabilitation. This information should also be considered when attempting to return an athlete to play after treatment.
Keywords: functional performance, modalities
Key Points
Shoulder proprioception was diminished after a 20-minute ice bag treatment to the shoulder.
Shoulder cryotherapy treatments impaired throwing accuracy in subjects with healthy shoulders.
Neuromuscular deficits occurred after application of shoulder cryotherapy treatments, potentially impairing the athlete's functional ability in the short term.
The shoulder joint has the greatest range of motion of any joint in the body, which potentially compromises its stability.1 As a result of this large range of motion, muscular coordination is vital to maintaining joint stability. Consequently, the shoulder relies upon proprioceptive feedback to maintain dynamic stability.2 Proprioception results from the integration of neural impulses from a variety of peripheral mechanoreceptors to the central nervous system.3,4 Mechanoreceptors are present in skin, muscle, and joint tissues and are activated by tissue deformation, which subsequently sends afferent neural impulses to the central nervous system, and are used for joint stability and proper joint function.5 The integrity of the mechanoreceptors and neural pathways plays a vital role in allowing shoulder mobility and concurrent stability.
Injury to the body during an athletic event is often immediately treated with cryotherapy modalities.6,7 After an acute shoulder injury in sport, an athlete may return to practice or competition following a cryotherapy treatment to the injured shoulder. Decreases in tissue temperature have been shown to decrease nerve conduction velocity, muscle force production, and muscular power.8,9 Cryotherapy has also been implicated in decreased afferent proprioception information at the knee.10 Consequently, cryotherapy application to the shoulder may decrease proprioception and predispose an athlete to injury as a result of decreases in nerve conduction velocity, muscle force production, proprioceptive afferent information, or a combination of these factors.
Few authors have focused on the effects of cryotherapy on proprioception. Dover and Powers11 assessed the effects of an ice treatment on shoulder joint position sense. They found no differences between active joint reposition sense after ice application compared with before application.11 Ozmun et al12 reported that ice pack application to the knee had no effect on proprioception (replication of active positioning). LaRiviere and Osternig13 also concluded that an ice treatment had no effect on joint position sense at the ankle joint. However, Hopper et al14 found statistically significant decreases in proprioception at the ankle joint after a 15-minute ice bath immersion; yet they deemed their results to have no clinical significance because of the small differences found. The degree to which proprioception is altered after cryotherapy may be minimal, but it is possible that subtle proprioceptive deficits may result in decreased performance on the playing field.
In addition to the lack of literature focusing on cryotherapy and proprioception, no authors to date have examined the influence of cryotherapy on shoulder function and its relationship to diminished proprioception. Cross et al15 found negative performance effects on vertical jump scores and increased shuttle run times after a 20-minute ice immersion session for the lower leg. Examining both proprioception and functional assessments may contribute to the clinician's understanding of the functional mechanisms resulting in alterations of proprioception after cryotherapy at the shoulder joint. Therefore, the purpose of our study was to examine the effect of a cryotherapy treatment on proprioception and functional performance of the throwing shoulder. We hypothesized that subjects would exhibit decreased proprioception as measured by active joint position replication (AJPR), path of joint motion replication (PJMR), and throwing accuracy after the application of cryotherapy to the shoulder.
METHODS
Twenty-two physically active college students (14 men, 8 women; age = 21.6 ± 2.4 years, height = 175.0 ± 11.1 cm, mass = 74.2 ± 10.4 kg,) with no history of neurologic conditions or musculoskeletal injuries to the throwing shoulder volunteered to participate in this study. None of the subjects tested was actively participating as a throwing athlete. All subjects provided informed consent as required by the university institutional review board, which approved the study.
We employed a single-group, pretest-posttest control session design. Dependent variables were AJPR, PJMR, and Functional Throwing Performance Index (FTPI). Proprioceptive measures (AJPR and PJMR) and a functional measure (FTPI) were tested on separate days. Each dependent variable (AJPR, PJMR, and FTPI) was assessed 3 times (2 trials before and 1 trial after ice bag application.) The posttest assessments of AJPR, PJMR, and FTPI were compared with the 2 pretests. Two pretests were used to help control for learning effects and to increase internal validity. The posttest (final assessment) explored the effects of cryotherapy on proprioception (AJPR and PJMR) and functional ability of the shoulder joint (FTPI) compared with the 2 pretests.
Instrumentation
The Biodex System 3 isokinetic dynamometer (Biodex Medical Inc, Shirley, NY) was used for assessing AJPR and PJMR. The Biodex uses a specialized software package combined with a dynamometer containing strain gauges, a potentiometer, and remote range-of-motion set switches, along with several limb attachments for testing, rehabilitation, and diagnostic purposes related to a variety of joints and muscle groups. The dynamometer was used in AJPR to create and standardize the target positions for the subjects. During PJMR, the dynamometer was used to standardize the path to be replicated during the trials.
The 3D Motion Monitor (Innovative Sports Training, Chicago, IL) electromagnetic tracking device is equipped with a short-range transmitter and 6 electromagnetic receivers with 6 degrees of freedom. The short-range transmitter is capable of measuring activity within a 3-ft (0.91-m) radius of the device. A sampling rate of 100 Hz was used. The short-range transmitter creates an electromagnetic field within the 3-ft testing space. Receivers, attached to various anatomical landmarks, record the electromagnetic flux generated by the transmitter and relay the position of each receiver to a computer via hard wiring, thereby creating a 3-dimensional image of the subject. We used the protocol set forth by the International Shoulder Group for shoulder joint analysis.16 This device is used to measure the subject's ability to actively reproduce the path (PJMR) or position (AJPR) during proprioception testing. This instrument is advantageous because subjects are free to move in multiplanar motion.
Active Joint Position Replication
Active joint position replication was assessed using an electromagnetic tracking device and an isokinetic dynamometer. Electromagnetic receivers were placed on the posterior aspect of the head, on the thorax at the T1 spinous process, and on the humerus just proximal and anterior to the elbow. The electromagnetic transmitter was positioned posterior to the subject on a tripod. Subjects actively moved to 1 of 2 target positions: 20° of shoulder flexion with 0° of humeral rotation and full elbow extension (20 FLEX) or 90° of shoulder abduction with 90° of external rotation and full elbow extension (90 ABD-ER) with the isokinetic dynamometer (Figures 1 and 2). These positions were chosen to simulate both a position of daily activity (eg, reaching for a doorknob) and a position of athletic activity at the shoulder (eg, cocking position during throwing). The cocking position in throwing also involves some amount, usually about 90°, of elbow flexion. We did not use this position in our protocol as the equipment was unable to accommodate this elbow flexion angle. The task is similar to aiming studies that assess error of placement under altered vision conditions.17 Subjects were blindfolded to eliminate visual cues. Upon reaching the target position, subjects were instructed to focus on their limb position for 10 seconds. After returning to the starting position, subjects were then asked to reproduce the target position without the aid of the dynamometer. The difference in aiming was calculated using the 3-dimensional position of the humerus. The aiming error was calculated as the variation between the given and reproduced positions and was reported in centimeters of deviation. Each subject performed 3 trials, moving from 20 FLEX to the presented position of 90 ABD-ER, as well as in the opposite direction. The order of the 6 trials was counterbalanced. The intraclass correlations (ICC [2,1]) ranged from .61 to .80 for the proprioception assessment on the electromagnetic tracking device.18
Figure 1. Setup for active joint position replication and path of joint motion replication with Biodex dynamometer. A, Ninety degrees of shoulder flexion with 0° of humeral rotation and full elbow extension. B, Twenty degrees of shoulder flexion with 0° of humeral rotation and full elbow extension.
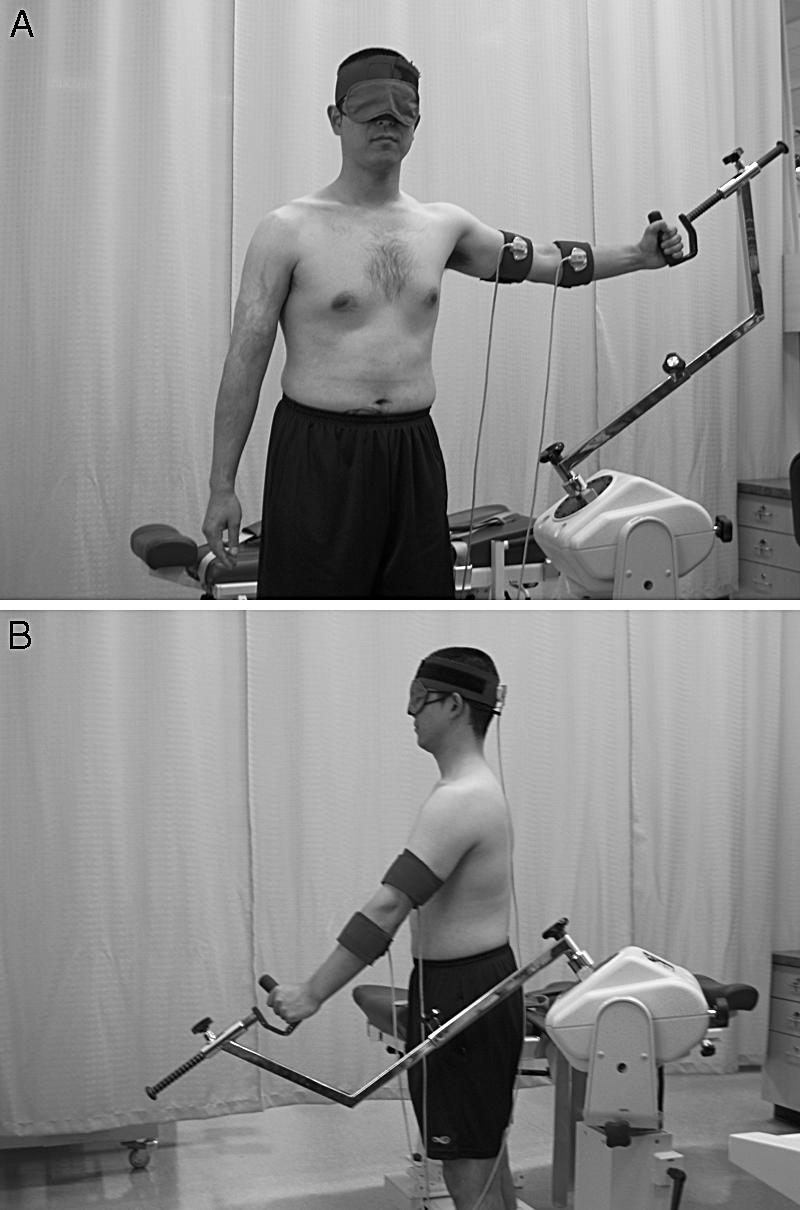
Figure 2. Setup for active joint position replication and path of joint motion replication without Biodex dynamometer. A, Ninety degrees of shoulder flexion with 0° of humeral rotation and full elbow extension. B, Twenty degrees of shoulder flexion with 0° of humeral rotation and full elbow extension.
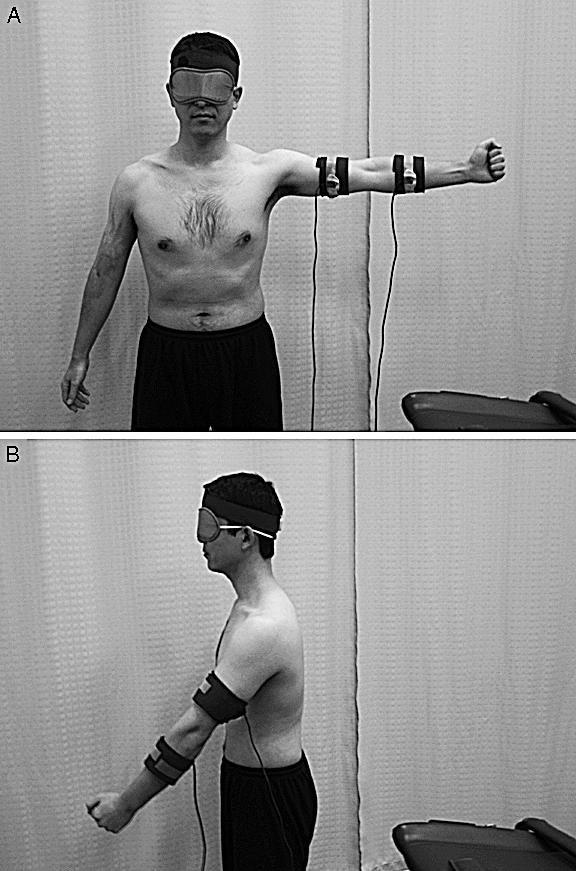
Path of Motion Replication
Similar to AJPR, PJMR was assessed with both the electromagnetic tracking device and the isokinetic dynamometer. Upon instruction, the subject actively moved from the starting position of 20 FLEX to 90 ABD-ER (or vice versa, depending on the trial) (see Figures 1 and 2 for starting and ending positions). The subjects moved at a self-selected speed during PJMR testing. The dynamometer standardized the path of motion between the starting and ending positions, allowing for a single curvilinear path. Once the endpoint was met, the subject returned to the starting position. The subject then reproduced the presented path of motion without aid from the dynamometer. This motion was selected as it grossly represents the motion of overhead throwing. The path of replication error was calculated as the variation between the given path and the reproduced path of movement using the 3-dimensional humeral position. The error was reported as mean centimeters of deviation between the presented and reproduced paths. Each subject performed 3 trials, moving from 20 FLEX to 90 ABD-ER and in the opposite direction from 90 ABD-ER to 20 FLEX. The order of the 6 trials was counterbalanced. The ICC [2,1] ranged from .61 to .80 for the proprioception assessment on the electromagnetic tracking device.18
Functional Throwing Performance Index
Functional ability of the shoulder joint was assessed using the FTPI.19 The subject stood 4.57 m from a target, a 30.48- × 30.48-cm square on a wall at a height of 1.22 m from the floor. The object of the test was to throw a rubber playground ball (50.8-cm circumference) into the target as many times as possible over three 30-second trials. Before testing, subjects performed 8 throws as a warm-up. Testing began immediately after the warm-up and consisted of the subject throwing the ball into the target, catching the rebound off the wall, and repeating as many times as possible within 30 seconds. The FTPI was calculated as the number of throws within the target divided by the total number of balls thrown. To avoid any discrepancies in judgments, the same examiner determined the accuracy of all throws. We chose to assess accuracy as we feel this is the measure most associated with proprioception. As a pilot study, we performed a reliability analysis for the tester measuring the reliability of the FTPI. Good reliability was shown for FTPI (ICC [3,1] = .81).
Cryotherapy Treatment
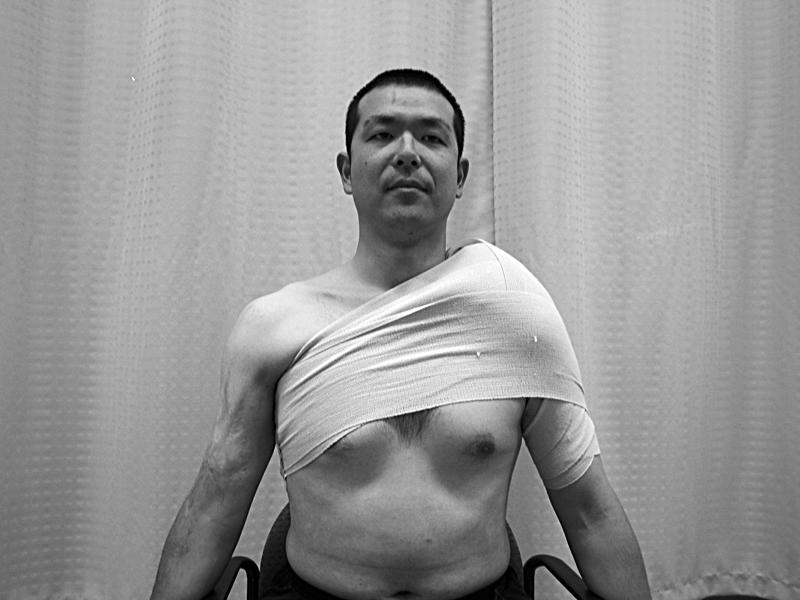
An ice bag treatment was employed as the cryotherapy modality in this study. This particular application is used frequently and is the most functional type of cryotherapy for the shoulder.20 Treatment duration was 20 minutes, based on accepted recommendations.21 A 1-qt (1.15-L) ice bag was filled with approximately 1500 g of cubed ice. The middle of the ice bag was centered over the acromion. Men were tested with their shirts off, and women wore a tank top or sports bra to allow maximal skin/ice bag interface. One double-length 6-in (15.24-cm) elastic bandage was used to secure the ice bag using a shoulder spica (Figure 3). The subject was instructed to relax during the cryotherapy treatment to limit muscle activity and minimize any change in tissue temperature.22 Immediately after the cryotherapy, the posttest assessment was performed.
Figure 3. Cryotherapy application.
Data Analysis
The data were analyzed using repeated-measures analyses of variance calculated by the Statistical Package for Social Sciences (version 11.0; SPSS Inc, Chicago, IL). Post hoc analyses were performed using a Tukey calculation. Significance was set a priori at P < .05.
RESULTS
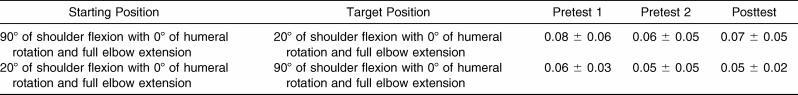
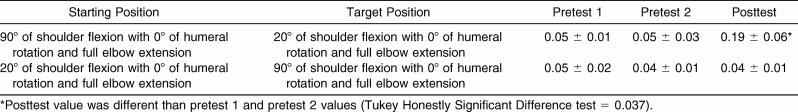
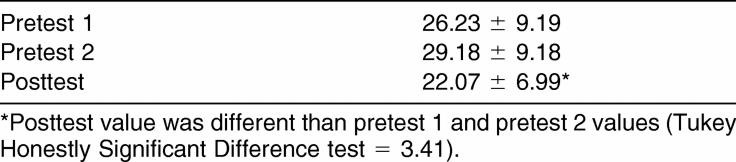
No significant differences were found in AJPR after cryotherapy (Table 1). Our results showed decreases from both pretests during PJMR after cryotherapy treatment when moving from the 90 ABD-ER position to the 20 FLEX position (F2,42 = 79.17, P < .001, Tukey Honestly Significant Difference test = 0.037). However, no evidence of any difference was seen when moving from 20 FLEX to 90 ABD-ER after cryotherapy (Table 2). A decrease on the FTPI (F2,42 = 12.83, P < .001, Tukey Honestly Significant Difference test = 3.41) was also demonstrated, as compared with both pretests, as indicated by a lower percentage of the FTPI after cryotherapy treatment (Table 3).
Table 1. Aiming Error of Angular Reproduction for Acute Joint Position Replication (Mean ± SD, cm).
Table 2. Displacement of Reproduction for Path of Joint Motion Replication (Mean ± SD, cm).
Table 3. Functional Throwing Performance Index (Mean ± SD, %).
DISCUSSION
Our purpose was to examine the effect of a cryotherapy treatment on proprioception and functional performance of the throwing shoulder. We hypothesized that subjects would exhibit decreases in shoulder AJPR, PJMR, and functional performance. In fact, functional performance and one measure of proprioception were negatively affected by the cryotherapy application.
Proprioception
In our study, subjects were able to reproduce endpoints but were unable to reproduce specific movements after cryotherapy. During PJMR, while moving from the 20 FLEX to the 90 ABD-ER position, no change was noted in path displacement. Significant differences were observed in the path of motion while moving from the 90 ABD-ER to the 20 FLEX position. Other authors10,14 have also found deficits in proprioception at the ankle and knee after cryotherapy. Uchio et al10 identified decreases in nerve conduction velocity after cryotherapy as the culprit for altered proprioception. As all tissues surrounding the shoulder joint were subjected to the cryotherapy, we cannot determine which structures were responsible for the alterations during PJMR. We can theorize that as subjects moved from 20 FLEX to 90 ABD-ER, the joint mechanoreceptors were stimulated to a greater degree as the external rotation increased tension on the glenohumeral joint capsule and ligaments. This suggestion is in agreement with the results of Janwantanakul et al,23 who reported greater accuracy of joint position sense at end-range shoulder external rotation than at midrange in healthy shoulders. Conversely, as internal rotation occurs from the 90 ABD-ER position (near end range) to the 20 FLEX position (midrange), the glenohumeral joint capsule would be under less tension and would theoretically decrease the afferent signals from the capsule to the central nervous system. As this occurs, the joint relies more on muscular and other superficial mechanoreceptors' afferent activity. We did not measure subcutaneous tissue temperature. Therefore, whether deeper structures, such as the joint capsule, were affected by treatment is unknown. Potentially the glenohumeral joint capsule was able to compensate for decreased proprioception in the muscle spindles and other superficial mechanoreceptors during the motion from 20 FLEX to 90 ABD-ER, as other authors have suggested.23
No difference was noted in the AJPR measure after cryotherapy application. This finding indicates that when the motion was controlled by the isokinetic dynamometer, the subjects were able to accurately appreciate their hand location in space. This result agrees with that of Dover and Powers,11 who also found no change in joint position sense after cryotherapy treatment to the shoulder. These authors measured internal and external rotation with an inclinometer.11 Alterations in neuromuscular control can be associated with a deficiency in afferent pathways, central integration, and/or efferent pathways.3 Because the cryotherapy did affect PJMR when moving from 90 ABD-ER to the 20 FLEX position, either the afferent or efferent pathway or central integration was likely confounded by the cryotherapy treatment. During AJPR, it is possible that the portions of the sensorimotor system not affected by the application of cryotherapy (mechanoreceptors deep to the cryotherapy application region) were able to compensate for mechanoreceptors influenced by the cryotherapy. The task of AJPR may be less taxing on the sensorimotor system, given that only the position of the arm was tested, versus the path of motion, as in PJMR.
Functional Ability
Subjects showed a decrease in the FTPI after cryotherapy application compared with both pretests. Participating in sports requires dynamic movements at high speeds, as simulated by the FTPI. The motions assessed during PJMR were designed to grossly replicate large portions of the motion required for throwing. However, these motions were performed at a self-selected pace. The pace for PJMR was much slower than the throwing motion in all cases. Additionally, the type of muscle contractions was different, as deceleration during throwing requires an eccentric contraction, which was not required during this study. Thus, moving from a position of 20 FLEX to 90 ABD-ER would simulate wind-up through cocking, whereas moving from 90 ABD-ER to 20 FLEX would simulate cocking through the acceleration and deceleration phases of throwing. It should be noted that both of these are active tasks, which were performed at different speeds, and both showed deficits after cryotherapy. We can infer that the errors in throwing performance occurred from cocking through acceleration, as these were mimicked during PJMR. Also, the decrease in outcomes did not seem to be related to the speed at which the movement was occurring, as both PJMR and FTPI showed decreases. The targets of the cryotherapy were the muscles of the rotator cuff. Reaching the deeper articular structures with superficial cryotherapy is unlikely.24,25
Proprioception and Performance
If we look only at the PJMR and FTPI deficits, our data indicate that, at the shoulder, cryotherapy may disrupt the motor control mechanism vital to not only functional ability and proprioception but also functional stability. Neuromuscular control is the reflexive activation of muscular patterns to provide stability.26 It is assumed that as a result of cryotherapy placement, the deltoid muscle would be the most significantly affected tissue. As such, we can infer that the deficits we saw in proprioception and performance stemmed from alterations within the deltoid and rotator cuff muscles.
Clinical Significance
Because the application of cryotherapy is indicated in many rehabilitation settings, it is imperative to understand how this modality affects proprioception and functional performance. We showed that proprioceptive deficits occurred when functional movements were simulated at slow speeds. Function was also adversely affected by cryotherapy, and caution should be observed when immediately returning athletes to sport after cryotherapy application. Because one of the main indications for use of cryotherapy is postinjury, the decreases in performance and proprioception may be much greater after injury and may be compounded by the cryotherapy.
Limitations
Our study is the first to assess functional performance at the shoulder after cryotherapy application. Several limitations should be noted. All subjects participating in this study had uninjured shoulders. Because cryotherapy application is indicated in acute injuries, the injury or immediate inflammatory processes may not make these results applicable to an injured population. Also, changes in surface and subcutaneous temperature were not measured. We assumed that our cryotherapy application altered the tissue temperature directly below the surface of the ice bag, yet this was not verified. Finally, it should be noted that the dynamometer was used to standardize the motion of testing; it is possible that as a result of anatomical differences among subjects, the paths presented did not represent exact alignment with normal motion for each subject. Thus, the path they were to follow may have represented a noncustomary motion, which might have negatively affected the results.
Future Directions
Future authors should assess functional performance and proprioception using the same protocol in an injured population. Another aspect that should be investigated is the time period that is necessary to return to normal levels of functional performance and proprioception following application of cryotherapy. As rewarming takes place after cryotherapy application, the time required to return to pretreatment levels of functional performance and functional capability will be very useful information for rehabilitation specialists. Additionally, measuring tissue temperature on and below the surface and recording nerve conduction velocity would further strengthen any future study results.
Conclusions
Proprioception and throwing accuracy were decreased after a 20-minute cryotherapy application to the shoulder. Caution should be taken when returning an athlete to play after a cryotherapy treatment.
REFERENCES
- Harryman DT, II,, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA., III. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72:1334–1343. [PubMed] [Google Scholar]
- Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- Myers JB, Lephart SM. Sensorimotor deficits contributing to glenohumeral instability. Clin Orthop Relat Res. 2002;400:98–104. doi: 10.1097/00003086-200207000-00013. [DOI] [PubMed] [Google Scholar]
- Voight ML, Hardin JA, Blackburn TA, Tippett S, Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23:348–352. doi: 10.2519/jospt.1996.23.6.348. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- Covington DB, Bassett FH. When cryotherapy injuries. Physician Sportsmed. 1993;21((3)):78–93. doi: 10.1080/00913847.1993.11710336. [DOI] [PubMed] [Google Scholar]
- Zemke JE, Anderson JC, Guion WK, McMillan J, Joyner AB. Intramuscular temperature responses in the human leg to two forms of cryotherapy: ice massage and ice bag. J Sports Rehabil. 1998;27:301–307. doi: 10.2519/jospt.1998.27.4.301. [DOI] [PubMed] [Google Scholar]
- Lee JM, Warren MP, Mason SM. Effects of ice on nerve conduction velocity. Physiotherapy. 1978;64:2–6. [PubMed] [Google Scholar]
- Sargeant AJ. Effect of muscle temperature on leg extension force and short-term power output in humans. Eur J Appl Physiol Occup Physiol. 1987;56:693–698. doi: 10.1007/BF00424812. [DOI] [PubMed] [Google Scholar]
- Uchio Y, Ochi M, Fujihara A, Adachi N, Iwasa J, Sakai Y. Cryotherapy influences joint laxity and position sense of the healthy knee joint. Arch Phys Med Rehabil. 2003;84:131–135. doi: 10.1053/apmr.2003.50074. [DOI] [PubMed] [Google Scholar]
- Dover G, Powers ME. Cryotherapy does not impair shoulder joint position sense. Arch Phys Med Rehabil. 2004;85:1241–1246. doi: 10.1016/j.apmr.2003.11.030. [DOI] [PubMed] [Google Scholar]
- Ozmun JC, Thieme HA, Ingersoll CD, Knight KL, Ozmun JC. Cooling does not affect knee proprioception. J Athl Train. 1996;31:8–11. [PMC free article] [PubMed] [Google Scholar]
- LaRiviere J, Osternig LR. The effect of ice immersion on joint position sense. J Sport Rehabil. 1994;3:58–67. [Google Scholar]
- Hopper D, Whittington D, Davies J. Does ice immersion influence ankle joint position sense? Physiother Res Int. 1997;2:223–236. doi: 10.1002/pri.108. [DOI] [PubMed] [Google Scholar]
- Cross KM, Wilson RW, Perrin DH. Functional performance following an ice immersion to the lower extremity. J Athl Train. 1996;31:113–116. [PMC free article] [PubMed] [Google Scholar]
- Wu G, van der Helm FC, Veeger HE. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. et al. [DOI] [PubMed] [Google Scholar]
- Gielen CC, Vrijenhoek EJ, Flash T, Neggers SF. Arm position constraints during pointing and reaching in 3-D space. J Neurophysiol. 1997;78:660–673. doi: 10.1152/jn.1997.78.2.660. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Myers JB, Bradley JP, Fu FH. Shoulder proprioception and function following thermal capsulorrhaphy. Arthroscopy. 2002;18:770–778. doi: 10.1053/jars.2002.32843. [DOI] [PubMed] [Google Scholar]
- Davies GJ, Dickoff-Hoffman S. Neuromuscular testing and rehabilitation of the shoulder complex. J Orthop Sports Phys Ther. 1993;18:449–458. doi: 10.2519/jospt.1993.18.2.449. [DOI] [PubMed] [Google Scholar]
- Starkey C. Therapeutic Modalities for Athletic Trainers. Philadelphia, PA: FA Davis; 1993.
- Kanlayanaphotporn R, Janwantanakul P. Comparison of skin surface temperature during the application of various cryotherapy modalities. Arch Phys Med Rehabil. 2005;86:1411–1415. doi: 10.1016/j.apmr.2004.11.034. [DOI] [PubMed] [Google Scholar]
- Belitsky RB, Odam SJ, Hubley-Kozey C. Evaluation of the effectiveness of wet ice, dry ice, and cryogenic packs in reducing skin temperature. Phys Ther. 1987;67:1080–1084. doi: 10.1093/ptj/67.7.1080. [DOI] [PubMed] [Google Scholar]
- Janwantanakul P, Magarey ME, Jones MA, Dansie BR. Variation in shoulder position sense at mid and extreme range of motion. Arch Phys Med Rehabil. 2001;82:840–844. doi: 10.1053/apmr.2001.21865. [DOI] [PubMed] [Google Scholar]
- Enwemeka CS, Allen C, Avila P, Bina J, Konrade J, Munns S. Soft tissue thermodynamics before, during, and after cold pack therapy. Med Sci Sports Exerc. 2002;34:45–50. doi: 10.1097/00005768-200201000-00008. [DOI] [PubMed] [Google Scholar]
- Merrick MA, Jutte LS, Smith ME. Cold modalities with different thermodynamic properties produce different surface and intramuscular temperatures. J Athl Train. 2003;38:28–33. [PMC free article] [PubMed] [Google Scholar]
- Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37:71–79. [PMC free article] [PubMed] [Google Scholar]