Abstract
Objective
The Objective of this follow-up study was to assess the long-term effects of clinical infant home-visiting services on child outcomes at school entry.
Method
Participants were 63 five-year-olds from low-income families, half of whom were referred to parent–infant home-visiting services during the first 18 months of life due to concerns about the caretaking environment. Families received between 0 and 18 months of weekly home visits based on infant age at entry into the study. At age 5, children were rated by teachers on the Preschool Behavior Questionnaire for behavior problems in the classroom and by parents both on the Simmons Behavior Checklist for behavior problems at home and on the Achenbach Social Competence Items for positive play behaviors with friends.
Results
With initial family risk status and child gender controlled, teacher-rated hostile behavior problems decreased in dose–response relation to the duration of early home-visiting services, which accounted for 15% of the variance in child hostile behavior. Parents' reports of positive play behaviors were positively linearly related to service duration. Parents' reports of behavior problems were less reliably related to service duration than teacher reports.
Conclusions
Early home-visiting services reduced the incidence of aggressive behavior problems among socially at-risk children for up to 3.5 years after the end of services.
Keywords: aggression, intervention, preschool, conduct disorder, oppositional disorder
Clinical investigators of conduct disorders have recently called for an increased focus on parent–infant services designed to prevent the early onset of aggression and disruptive behavior (Tremblay et al., 1999). These disorders are the most common, costly, and treatment-resistant disorders identified among school-age children, particularly boys (Greenberg et al., 1995; Hinshaw and Anderson, 1996). About half of the children who show an early onset of disruptive behavior problems continue on a chronic and escalating aggressive trajectory known as the “early starter” pathway (Loeber and Dishion, 1983). Diminishing the early display of aggression and disruptive behaviors is therefore one of the keys to preventing the emergence of juvenile delinquency and associated risks such as school failures and peer rejection.
Risk Factors for Aggressive Behavior in Children
At the level of the family system, risk factors for aggressive behavior include (1) family adversity, (2) ineffective parenting/discipline, (3) atypical child characteristics, and (4) insecure, particularly disorganized, attachment patterns (Greenberg, 1999). First, the effects of sociodemographic factors such as single-parent status or low income have been consistently noted as risk factors for the development of antisocial behavior in childhood. However, multivariate studies find that child and parental risk factors related to low socioeconomic status, such as maternal depression, hostile parenting, parental psychiatric disorder, and child maltreatment are more specific predictors of preschool aggression (Lyons-Ruth et al., 1993).
Second, the relationship between harsh and ineffective parental discipline and aggressive behavior problems is a well-documented finding (for review, see Loeber and Dishion, 1983). Coercive parenting practices have also been shown to be part of a broader constellation of rejecting parental behavior, characterized by the absence of warmly approving, autonomy-respecting, and contingent parental responsiveness (Lyons-Ruth, 1996) and by perceptual and information-processing biases that may be transmitted from parent to child (e.g., Dix and Lochman, 1990).
Third, atypical child factors, such as cognitive functioning, temperament, or neurobiological profiles, also contribute to the onset and maintenance of aggressive behavior disorders (Hinshaw and Anderson, 1996).
Fourth, disorganized patterns of attachment behavior in infancy have been associated with the development of both internalizing and externalizing behavior in the preschool and school years (Lyons-Ruth and Jacobvitz, 1999). Disorganized attachment is chronologically one of the first markers to indicate that a child is at risk, and maternal hostile-intrusive behaviors and child mild mental deficits are also observable by 12 months of age (Lyons-Ruth et al., 1997). Thus, an important research priority lies in developing effective interventions during the infancy period for the prevention of school-age aggression.
Interventions to Prevent Aggressive Behavior
Interventions for aggressive behaviors have generally been concentrated after the first 2 years of childhood and have focused on children already displaying conduct problems. A range of interventions has targeted aspects of the multilayered contributors to aggression, including parenting competencies (Dishion et al., 1991; Forgatch and DeGarmo, 1999; Webster-Stratton et al., 1989), academic competence (Arnold et al., 1999), and school-age children's socioemotional skills (Greenberg et al., 1995; Webster-Stratton and Hammond, 1997).
However, a few programs beginning in infancy have shown effects on later aggression. Johnson and Walker (1987) found that children from poor Mexican-American families who received early interventions were rated as less aggressive and disruptive in elementary school, and Lally et al. (1988) reported that, among children of young African-American single mothers, a program of early home visitation and early day care showed long-term effects in reducing later criminal acts, with 22% of unserved versus 6% of served 16-year-olds having contact with the probation department. Olds et al. (1997, 1998) conducted the largest scale randomized early home-visiting study, using a 2.5-year program of nurse home visitation begun in pregnancy. At 15-year follow-up, there were significant reductions in the number of arrests, convictions, and probation violations among adolescent children of poor unmarried women in the home-visited group. Of note, the work of Olds et al. (1997) showed a dose–response pattern of outcomes on a variety of variables, with mothers visited only during pregnancy having intermediate outcomes compared with nonvisited mothers and mothers visited for 2 years.
Few studies are available, however, that have explored the impact of clinical infant home-visiting services on the early-onset aggressive behaviors evident by school entry that serve as precursors to later serious delinquency. The study reported here examines whether home-visiting services before 18 months of age will show a relationship with decreased aggressive behavior problems among children in preschool and kindergarten, after controlling for demographic and psychosocial risk factors.
METHOD
Participants
The sample consisted of 64 preschool children from low-income families, aged 49 to 71 months (37 male). The subjects were recruited from among 76 low-income families who had participated in a previous study of the impact of family risk factors and early home-visiting services on infant development (Lyons-Ruth et al., 1990). During the infant study, 41 families were referred for services and 35 community families were assessed as socioeconomic status–matched comparisons. At the 5-year-old follow-up, 84% of the families who completed the infant study were reassessed. 11% had moved too far away or could not be relocated, and 5% refused to participate. For two families who participated, the children were not in preschool, so teacher ratings were unavailable.
Infant Home-Visiting Study Procedure
Infants were referred for home-visiting services from a variety of community service agencies due to concerns about the quality of the caregiving for the infant. Infants had to be younger than 9 months of age at the time of referral, and an income ceiling was set at the federal poverty level. Among the 41 families referred for services, 31 families were enrolled in a weekly home-visiting service until 18 months infant age: 10 referred families whose infants were older than 9 months of age were not eligible and these families were assessed when the infant reached 18 months of age. To control for willingness to participate in home-visiting services, families whose infants were past the 9-month cutoff point were provided shortterm home-visiting services (six to eight sessions) after the assessments at 18 months of age to connect them with other available community resources.
Among families offered weekly services, the mean infant age at intake was 4.7 months. Duration of services varied from 9 to 18 months depending on how early the family was referred. By 18 months of age, families had received an average of 13.3 months of service, with an average of 47 completed home visits per family.
The third group assessed in infancy was a matched community group of 35 mothers and infants from the same neighborhoods who had never sought or received social services directed at parenting skills, had never been identified as maltreating, and had never undergone extensive psychiatric treatment. The community-group mothers were individually matched to high-risk mothers on per-person family income; mother's education, age, and race and the child's age, gender, and birth order (first born, later born).
Assessment Procedures: Study Entry
Cumulative demographic risk was represented by the sum of the following factors: mother is not a high school graduate, mother was younger than 20 at birth of first child, mother is a single parent, mother is of minority race, family is supported by government assistance, three or more children are younger than age 6.
Severity of maternal psychosocial problems was coded as 3 if the mother had a state-documented history of child maltreatment, as 2 if she had a history of inpatient psychiatric hospitalization but no maltreatment, and as 1 if at study entry she reported depressive symptoms over the validated cutoff point for possible clinical disorder but no maltreatment or hospitalization history. All other mothers received a score of 0.
The Center for Epidemiologic Studies Depression Scale (CES-D) was administered verbally to mothers at study entry and again when infants were 18 months old. The CES-D is a 20-item questionnaire concerning depressive symptoms during the past week (Radloff, 1977). It has been well validated in large-scale epidemiological studies.
Assessment Procedures: Age 5
Teacher ratings of child behavior problems were made on the Preschool Behavior Questionnaire (PBQ) both for study children and for the three same-gender classmates nearest in age. Classmate scores were included to control for potential differences among teachers in their use of the rating scales. A mean classmate score was computed for each study child by averaging the scores of the three classmates.
The PBQ represents a modified version of Rutter's Children's Behavior Questionnaire, developed for children in the 3- to 6-year-old age range. Total score ranges from 0 to 60. Test–retest values, interrater reliabilities, standardization sample characteristics, and validity are all acceptable. In the standardization data, factor analysis extracted three factors: hostile-aggressive, anxious, and hyperactive. The cutoff score, which maximally discriminated normal and disturbed groups, was at the 90th percentile (Behar and Stringfield, 1974).
Teachers' ratings of study children and same-gender, near-in-age classmates were significantly correlated for total problems (r = 0.28, p < .01), anxious behavior (r = 0.36, p < .002), and hyperactive behavior (r = 0.25, p < .05) but not hostile behavior (r = 0.11, p < .20). Although these could reflect legitimate classroom differences, they could also indicate potential differences across teachers in their baselines for rating problem behaviors. To control for possible baseline effects, mean classmate scores were entered first as covariates in analyses of teacher ratings.
Analyses of variance of teachers' behavior ratings by child age (4 years/5 years) did not reveal any age differences in behavior problems (F1.60 = 0.27–2.58, all not significant [NS]). Age effects over this range were also not ohserved in the PBQ validation study (Behar and Stringfield, 1974).
Achenbach Social Competence Items from the Child Behavior Checklist (Achenbach, 1991) were also asked of mothers. Two questions concerned relationships with friends: “About how many times a week does your child do things with friends (outside of school/daycare)?” and “Compared to others of his/her age, how well does your child get along with other kids?” and two questions concerned relationships with family members: “Compared to others of his/her age, how well does your child a) get along with his/her brothers and sisters? or b) behave with his/her parents?” Response alternatives were coded as follows: 1, worse than other children; 2, about average; 3, better than other children.
Parent ratings of child behavior problems were assessed by the Simmons Behavior Checklist (Reinherz and Gracey, 1983). The Simmons Behavior Checklist is a parent questionnaire designed to assess behavior and emotional functioning among 3- to 6-year-old children, standardized on a large sample of mothers and children. Internal consistency (Cronbach α = .86) and test–retest reliability (mean r = 0.73) are strong. A cutoff score of 93 or above, obtained by 5% of the normative sample, best differentiated normal children from emotionally disturbed children (Reinherz and Gracey, 1983). The factor structure of the Simmons Behavior Checklist yields 11 factors and could not be further simplified (Reinherz and Gracey, 1983). Therefore, only the total score was used for the present analyses. Analysis of variance by child age in the current sample (4 years old/5 years old) did not reveal any significant age differences in behavior problems (F1.63 1.00, NS).
Maternal depressive symptoms were reassessed at age 5 on the CES-D (described under “Assessment Procedures: Study Entry”).
Child verbal and performance abilities were assessed by the Information and Mazes subtests of the Wechsler Preschool and Primary Scales of Intelligence.
RESULTS
Clinical Identification of Risk Status During the First Year and Preschool Outcomes
The first set of analyses examined whether service providers were able to identify, during the infant's first 9 months of life, families whose infants were at risk for later behavior problems. Referred families were compared with community control families on risk factors at study entry and on the set of 5-year-old outcome measures, as shown in Table 1. Eighteen-month maternal and infant outcomes that were the subject of a previous report are also included in the table (Lyons-Ruth et al., 1990).
TABLE 1.
Differences in Initial Risk Status and Outcomes Between Referred Families and Matched Comparison Families
| Social Risk Factors | Community Comparison Families (n = 33) |
High-Risk Referred Families (n = 30) |
Magnitude of Associationa |
|---|---|---|---|
| At study entry | |||
| % Male | 58 | 60 | 0.03 |
| Mother high school graduate (%) | 50 | 50 | 0.00 |
| Per-person family income (weekly) | $48.33 | $45.62 | 0.08 |
| Cumulative demographic risk | 1.8 | 2.7 | 0.36*** |
| Psychosocial problems (%) | 0.18 | 1.67 | 0.69*** |
| Psychiatric hospitalization | 0 | 37 | 0.48*** |
| Maltreatment | 0 | 30 | 0.43*** |
| Depression over clinical cutoff | 28 | 72 | 0.46*** |
| 18-month outcomes | |||
| Mental Development Index | 107.1 | 104.5 | 0.17a,b |
| Security of attachment | 2.07 | 1.75 | 0.18b,c |
| Maternal involvement at home | 0.11 | 0.08 | 0.00b,c |
| Maternal hostile-intrusive behaviors at home | −0.53 | 0.29 | 0.46***b |
| Maternal depressive symptoms | 10.91 | 23.30 | 0.45***b |
| Kindergarten outcomes | |||
| Maternal outcomes (%) | |||
| Maternal depression over clinical cutoff | 27 | 63 | 0.36*** |
| Child cognitive outcomes | |||
| Child verbal ability | 11.36 | 9.60 | 0.30* |
| Child performance ability | 9.01 | 8.27 | 0.13 |
| Child social outcomes at home | |||
| Total behavior problems at home | 75.79 | 83.53 | 0.29* |
| Positive behaviors with siblings (n = 48) | 2.38 | 2.18 | 0.19 |
| Positive behaviors with parents | 2.24 | 2.17 | 0.06 |
| Positive play with friends | 2.24 | 2.23 | 0.07 |
| Time with friends | 2.70 | 2.73 | 0.03 |
| Child social outcomes at school | |||
| Total behavior problems at school | 8.58 | 15.77 | 0.38** |
| % over clinical cutoff | 13 | 50 | 0.40** |
| Hostile behavior problems at school | 1.65 | 6.20 | 0.44*** |
| % over clinical cutoff | 13 | 43 | 0.34** |
| Anxious behavior problems at school | 3.29 | 3.90 | 0.10 |
| % over clinical cutoff | 42 | 50 | 0.08 |
| Hyperactive behavior problems at school | 2.45 | 3.50 | 0.22† |
| % over clinical cutoff | 26 | 47 | 0.22† |
Note: Only families with 5-year-old outcome data are included.
For categorical variables, ϕ is shown; for continuous variables, η is shown. The η statistic is a measure of strength of association for effects measured by F test.
These measures are described and intervention effects are reported on in Lyons-Ruth et al. (1990).
Service effects improved scores of high-risk families (Lyons-Ruth et al., 1990).
p < .10
p < .05
p < .01
p < .001.
The data in Table 1 document the close matching of high-risk and community groups on family demographic factors. The data also confirm that there were highly significant differences (p < .001) in psychosocial risk factors between referred and nonreferred families at study entry. Families referred by service providers had serious psychosocial risks, including high rates of state-documented maltreatment, high rates of lifetime psychiatric hospitalization, and high rates of depressive symptoms. Although providers were often aware of the presence of state-documented maltreatment, psychiatric histories and elevated depressive symptoms were often unknown to pediatric or other providers (e.g., Head Start teachers) at the time of referral. Instead, referrals were made on the basis of clinical judgment regarding the primary caregiver's overall functioning as a parent.
Table 1 also presents the 18-month and kindergarten outcomes for the referred and nonreferred groups. Children in families referred for services showed significantly poorer outcomes both in infancy and at age 5 compared with other low-income families in the community. As can be seen, these differences were consistent among teacher reports, mother reports, and cognitive tests, even though income and education were closely comparable for referred and nonreferred families and intervention services were provided to 77% of referred families.
The data support the conclusion that during the first year of the infant's life, community service providers from a variety of agencies can reliably discriminate low-income families whose caretaking places the child at elevated risk of behavior problems from other low-income families whose caretaking does not contribute to elevated risk.
Duration of Infant Home-Visiting Services and Preschool Outcomes
Teacher-Rated Behavior Problems
A hierarchical multiple regression analysis assessed whether variance in preschool behavior problems was uniquely associated with duration of early home-visiting services. Mean classmate control scores were entered first to control for any teacher baseline differences in the use of the rating scales. Gender, cumulative demographic risk, and severity of maternal psychosocial problems at study entry were then entered to control for variation in risk status at study entry. Duration of services (0–18 months) was then entered, followed by the six two-way interaction terms between service, gender, demographic risk, and psychosocial risk. None of the interaction terms were significant in any analyses, so interaction effects are not reported on further.
As shown in Table 2, months of service accounted for a significant 15% of the variance in hostile behavior problems at age 5 and for a marginally significant portion of variance in total behavior problems: hostile behavior problems, β = −.46; total problems, β = −.41. Scores for hyperactive behavior problems and anxious behavior problems were not significantly related to duration of services.
TABLE 2.
Teacher-Rated Behavior Problem Scores: Hierarchical Regression Results
| Total Behavior Problems |
Hostile Behavior Problems |
||||||
|---|---|---|---|---|---|---|---|
| Predictors | df | βa | R2chg | Fchg | βa | R2chg | Fchg |
| Step 1 | 1,28 | 0.10 | 31.7† | 0.03 | 0.91 | ||
| Classmate controls | .30† | .19 | |||||
| Step 2 | 3,25 | 0.05 | 0.43 | 0.04 | 0.39 | ||
| Male gender | .01 | .19 | |||||
| Demographic risk | .00 | .02 | |||||
| Psychosocial problems | .03 | −.05 | |||||
| Step 3 | 1,24 | 0.13 | 3.99† | 0.15* | 4.66* | ||
| Service time | −.41† | −.46* | |||||
β values are reported for the final equation with all variables entered; significance of individual β values assessed by t test, with all other variables controlled.
p < .10
p < .05.
The continuous behavior problem scores did not reveal whether the problems being reported were severe enough to fall within the range of risk of clinical disorder. Therefore, children were also classified as deviant or nondeviant according to normed PBQ cutoff scores. Hierarchical logistic regression analyses were conducted using the same independent variables as above. Hostile behavior scores in the deviant range were significantly negatively predicted by duration of services with other variables controlled, service time Wald (1,24) = 3.70, p < .05. The corresponding analysis for total behavior problems in the deviant range again just missed reliability by two-tailed test, service time Wald (1,24) = 3.62, p < .06.
Figure 1 shows the dichotomous scores for deviant total problems and deviant hostile behavior problems cross-classified by three levels of service duration: no services (infant referred after 9 months of age), less than 12 months of services (infant referred at age 6–9 months), and 12 or more months of services (infant referred younger than 6 months of age). As can be seen, the significant effect of service time resulted both from children who received no services and from a differential rate of problems within the group of children receiving services. Therefore, there was a dose–response relationship between duration of services and deviant levels of hostile behavior in the preschool classroom.
Fig. 1.
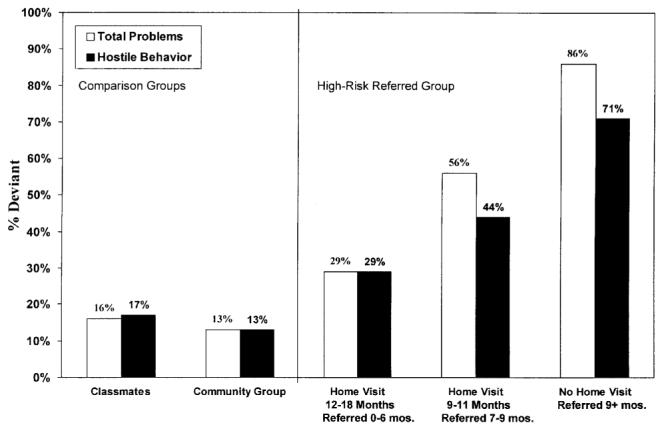
Percentage of children over clinical cutoff scores for total problems and hostile behavior by risk status and duration of services.
The mean demographic and psychosocial risk scores for the three service groups shown in Figure 1 did not differ significantly. In fact, there was a mild trend for the risk means to be lowest among the group with the poorest kindergarten outcomes: mean demographic risk scores for infants served 1 year or more, 2.86; served less than 1 year, 2.56; no service, 2.14 (F2,27 = 1.43, NS); mean psychosocial problems served 1 year or more, 1.71; served less than 1 year, 1.78; no service, 1.43 (F2,27 = 0.23, NS).
Positive Play Behavior With Peers at Age 5: Mother Report
Table 3 displays both the bivariate r values and the multivariate β values relating service time and initial family status variables to the child's positive play behaviors with peers and time spent with friends, as reported by mothers. With initial status variables controlled, duration of services was strongly and significantly related to positive play behaviors with peers at age 5 (β = .45), with 15% of variance accounted for by service time. Time spent with friends at age 5 was not significantly related to service time (β = .25).
TABLE 3.
Parent-Rated Positive Play Behaviors: Hierarchical Multiple Regression Results
| Positive Play Behavior With Peers |
Time Spent With Friends |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | biv r | βa | R2chg | Fchg | df | biv r | βa | R2chg | Fchg | df |
| Step 1 | 0.00 | 0.04 | 3,26 | 0.23 | 2.57† | 3,26 | ||||
| Male gender | 0.02 | .13 | 0.21 | .26 | ||||||
| Demographic risk | 0.05 | −.12 | 0.43** | .34† | ||||||
| Psychosocial problems | −0.04 | −.13 | 0.02 | .06 | ||||||
| Step 2 | 0.15 | 4.43* | 1.25 | 0.04 | 1.54 | 1,25 | ||||
| Service time | 0.35* | .45* | 0.28† | .25 | ||||||
Note: biv r = bivariate r.
β values are reported for the final equation with all variables entered; significance of individual β values assessed by t test, with all other variables controlled.
p < .10
p < .05
p < .01.
Behavior Problems at Home: Mother Report
Children's positive behaviors with family and total behavior problems at home, as reported by mothers, were not related to duration of services, although total behavior problems showed a negative trend consistent with teacher report: total behavior problems (β = −.26, F chg [1,25] = 1.45, NS); positive behavior with parents (β = −.10, F chg [1,25] = 0.18, NS); and positive behavior with siblings (β = .10, F chg [1,17] = 0.15, NS).
DISCUSSION
First, the results of these analyses indicated that service providers in the community can identify during the first year of life families whose infants will demonstrate a high incidence of aggressive behavior problems by school entry. Second, the results indicated that, among poor children, the incidence of teacher-rated hostile-aggressive behavior problems in kindergarten was reduced significantly by early home-visiting services, particularly when those services were delivered weekly for at least 1 year. Service effects were also evident in mothers' reports of how well their children got along with other children. The effect sizes observed in the study were also substantial, with β = −.46 for hostile behavior problems, −.41 for total behavior problems, and .45 for positive play behaviors with peers.
The less strong service effects on mothers' reports of behavior problems, compared with teachers' reports, are consistent with the lack of relation of mothers' behavior problem reports to other important variables in the larger study (Lyons-Ruth et al., 1997). Other studies have shown trends toward overreporting of problems among mothers of secure infants and underreporting among mothers of insecure infants, relative to other observers of the same behavior (Stevenson-Hinde and Shouldice, 1990). Therefore, mothers' reports of behavior problems may be influenced by various attitudinal biases, including biases related to attachment strategies.
These service-related effects at 5 years are consistent with earlier reported positive service effects on maternal responsive involvement with the infant by 12 months of age and with infant mental development and security of infant–parent attachment by 18 months of age (Lyons-Ruth et al., 1990). Based on the large body of research literature reviewed earlier, hostile behavior problems are associated with mild mental deficits, insecure-disorganized early attachment relationships, and lack of parental involvement and coercive parenting. Therefore, affecting these infancy outcomes would be expected to contribute to reduced aggression at later time points. Given the long-term stability of conduct problems among children and the negative adolescent and adult outcomes for such children, these are important effects.
These results converge with results of the larger scale study of Olds et al. (1997, 1998) in three important respects. First, both studies found results among the most at-risk segments of the population of mothers and infants. Second, both studies found a dose–response relationship between duration of services and positive outcomes. Third, both studies found that effects on social outcomes continued to appear long after the end of home-visiting services.
Extending the Olds et al. study, which did not assess preschool or early school-age aggression, these results document that early services can prevent aggressive behavior as early as age 5. Therefore, these results suggest that the decreases in adolescent antisocial behavior associated with the infant or preschool interventions reported by Olds et al. (1998), Schweinhart et al. (1993), and Lally et al. (1988) may be due to an impact on the initial formation of aggressive behaviors during the infant and preschool years, rather than affecting later delinquency through indirect effects such as increased school achievement or decreased association with deviant peers.
Limitations
The major caveat to be observed in interpreting the results of the study is that nonrandomly constituted groups were being compared. Without random assignment, the possibility cannot be ruled out that mothers who were referred earlier into services were more motivated or available to improve than mothers who were referred when their infants were slightly older.
In the current study, the distribution of cumulative demographic and psychosocial risk works against this possibility. The families treated for longer periods incurred substantial risks of compromised development, particularly in relation to the significantly greater proportion of maltreating mothers who received services (Table 1). The contribution of early maltreatment to aggressive behavior has been well documented (e.g., Eckenrode et al., 2001). Thus, any hypothesis regarding positive selection factors among earlier-referred families must be weighed against the slightly higher demographic risk scores and the higher proportion of maltreating families in that group. Early-referred families were also the families most in crisis at the time of referral, with two infants hospitalized for failure to thrive, two families with older children in foster care, and two infants in temporary custody of the state. None of the families referred after 9 months of age were having this level of difficulty.
Another important safeguard against this threat to validity was the dose–response pattern of effects, which makes it unlikely that a particular aspect of the recruitment process led to biased results. The further regression analyses to control any confounding of service effects with initial demographic or psychosocial risk factors also reduces the possibility that other factors could explain the variance in outcomes associated with duration of services.
A second limitation of the study is that, like the Olds et al. (1997, 1998), Johnson and Walker (1987), and Lally et al. (1988) infant intervention studies cited earlier, the intervention was carried out some years ago. It is not clear whether changing social conditions, related, for example, to welfare reform or other factors, would affect the results of a replication of the program. However, because of this concern, Olds et al. (1998) have recently replicated the positive effects of the nurse home-visiting program in another community and are currently conducting a second replication in Denver, so there is reason to be optimistic about the continued current viability of home-based programs for families at high social and psychiatric risk.
Clinical Implications
The home-visiting services evaluated here were targeted toward four clinical goals: (1) building an accepting and trustworthy relationship with the parent; (2) increasing the family's competence in accessing community resources to meet basic needs; (3) modeling and reinforcing more interactive, positive, and developmentally appropriate exchanges between mother and infant; and (4) decreasing social isolation from other mothers through participation in parenting group activities provided by the program. In pursuing these goals, the home visitor served both as an ombudsperson for the parent and as a model for a reliable and responsive attachment partner in relation both to the parent and to the infant.
Consistent with research on the importance of attachment security, the primary focus was on building the quality of the relationship between home visitor and parent. This relationship was viewed as the most powerful vehicle for directly providing new models of relatedness that could be transferred to the parent–infant relationship. The home visitor's ability to be reliably responsive to the parents' concerns and to maintain a concerned dialogue about distressed and angry affects were considered foundational to the more pragmatic interventions of the home visitor around the family's social needs and the mother's care of her infant (see Lyons-Ruth et al., 1984, for more detailed program description).
The clinical/developmental focus of this program also led to the inclusion of several program components not included in the more public health–oriented model of Olds et al. The current program included periodic in-home assessments of an infant's developmental status in the mother's presence, a procedure shown to contribute to improved infant development (Haskins et al., 1978), and a toy demonstration component in which toys fostering interaction between parent and infant were demonstrated by the home visitor and left in the home for subsequent use. In addition, parental social isolation and parenting practices were addressed by gradually introducing parent-group activities.
Given the unreliability of program participation among highly stressed families, it is notable that this focus resulted in a 91% retention rate in the program after the third home visit. Attrition occurred primarily during the initial research interviews to elicit informed consent and during the subsequent transfer to the home visitor rather than after the home visitor had become engaged with the family. This was due to the concerted and persistent outreach by the home visitors to maintain contact with families after early missed or canceled appointments. In addition, weekly group supervision was important in maintaining commitment and clinical focus among the home visitors.
Cost–benefit analyses conducted by the RAND Corporation for the Olds et al. program indicated that in 1980 dollars, the program cost $3,173 per family for 2.5 years of intervention, or about $8,000 in 2002 dollars (Karoly et al., 1998). The savings to government for serving low-income single mothers (but not lower risk mothers) exceeded the cost of the program by a factor of 4 over the life of the child. The program reported on here incurred a similar per-family cost but delivered more visits (47 versus 32 on average) over a shorter period (1.5 years versus 2.5 years).
The mothers and infants served by this program included the full range of socially at-risk infants known to service agencies in the community, including a substantial portion of families with protective service involvement and psychiatric histories. Thus, these findings should address the effectiveness of early home-visiting services for the heterogeneous group of high-risk mothers and infants likely to present to an urban, clinically oriented home-visiting service.
Footnotes
This work was supported by NIH grants 35122 and 62030 and by a grant from an anonymous private foundation. Special thanks to the families who have generously given their time to participate in the study over many years.
BMI Distribution Changes in Adolescent British Girls E. Georgiades, J. J. Reilly, E. Stathopoulou, A. M. Livingston, Y. P. Pitsiladis
Body mass index (BMI) distribution changes were assessed in 2547 relatively affluent English girls, aged 12–16 years, during the UK childhood obesity epidemic (1986–96). An increase in BMI variability was observed only in 12–14 year olds, suggesting that BMI changes for population subgroups were complex, and inconsistent with a generalised increase in BMI. Arch Dis Child 2003;88:978–979. Reproduced with permission from the BMJ Publishing Group.
REFERENCES
- Achenbach TM. Integrative Guide for the 1991 CBCL14-18, YSR and TRF Profiles. University of Vermont; Burlington: 1991. [Google Scholar]
- Arnold DH, Ortiz C, Curry JC, et al. Promoting academic success and preventing disruptive behavior disorders through community partnership. J Community Psychol. 1999;27:589–598. [Google Scholar]
- Behar L, Stringfield S. A behavior rating scale for the preschool child. Dev Psychol. 1974;10:601–610. [Google Scholar]
- Dishion TJ, Patterson GR, Kavanagh K. An experimental test of the coercion model: linking theory, measurement and intervention. In: McCord J, Trembley R, editors. The Interaction of Theory and Practice. Experimental Studies of Intervention. Guilford Press; New York: 1991. [Google Scholar]
- Dix TH, Lochman JE. Social cognition and negative reactions to children: a comparison of mothers of aggressive and nonaggressive boys. J Soc Clin Psychol. 1990;9:418–438. [Google Scholar]
- Eckenrode J, Ziclinski D, Smith E, et al. Child maltreatment and the early onset of problem behaviors: can a program of nurse home visitation break the link? Dev Psychopathol. 2001;13:873–890. [PubMed] [Google Scholar]
- Forgatch M, DeGarmo D. Parenting through change: an effective preventive program for single mothers. J Consult Clin Psychol. 1999;67:711–724. doi: 10.1037//0022-006x.67.5.711. [DOI] [PubMed] [Google Scholar]
- Greenberg M. Attachment and psychopathology in childhood. In: Cassidy J, Shaver P, editors. Handbook of Attachment: Theory, Research, and Clinical Application. Guilford Press; New York: 1999. pp. 469–496. [Google Scholar]
- Greenberg M, Kusche C, Cook E, Quamma J. Promoting emotional competence in school aged children: the effects of the PATHS curriculum. Dev Psychopathol. 1995;7:117–136. [Google Scholar]
- Haskins R, Ramey C, Stedman D, Blacher-Dixon J, Pierce F. Effects of repeated assessment on standardized test performance by infants. Am J Ment Defic. 1978;83:233–239. [PubMed] [Google Scholar]
- Hinshaw SP, Anderson CA. Conduct and oppositional defiant disorder. In: Mash EJ, Barkley RA, editors. Child Psychopathology. Guilford; New York: 1996. pp. 113–149. [Google Scholar]
- Johnson DL, Walker T. Primary prevention of behavior problems in Mexican-American children. Am J Commun Psychol. 1987;15:375–385. doi: 10.1007/BF00915208. [DOI] [PubMed] [Google Scholar]
- Karoly L, Greenwood P, Everingham S, et al. The RAND Corporation; Santa Monica, CA: 1998. Investing in our children: what we know and don't know about the costs and benefits of early childhood interventions. [Google Scholar]
- Lally RJ, Mangione PL, Honig AS. The Syracuse University Family Development Research Program: long-range impact on an early intervention with low-income children and their families. In: Powell D, editor. Parent Education as Early Childhood Intervention: Emerging Directions in Theory, Research and Practice. Ahlex; Norwood, NJ: 1988. pp. 79–104. [Google Scholar]
- Loeber R, Dishion T. Early predictors of male delinquency: a review. Psychol Bull. 1983;93:68–99. [PubMed] [Google Scholar]
- Lyons-Ruth K. Attachment relationships among children with aggressive behavior problems: the role of disorganized early attachment patterns. J Consult Clin Psychol. 1996;64:64–73. doi: 10.1037//0022-006x.64.1.64. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Alpern L, Repacholi B. Disorganized infant attachment classification and maternal psychosocial problems as predictors of hostile-aggressive behavior in the preschool classroom. Child Dev. 1993;64:572–585. doi: 10.1111/j.1467-8624.1993.tb02929.x. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Botein S, Grunebaum G. Intervention With Psychiatrically Disabled Parents and Their Young Children. New Directions for Mental Health Services. Vol. 24. Jossey-Bass; San Francisco: 1984. Reaching the hard-to reach: serving isolated and depressed mothers with infants in the community. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Connell D, Grunebaum H, Botein S. Infants at social risk: maternal depression and family support services as mediators of infant development and security of attachment. Child Dev. 1990;61:85–98. doi: 10.1111/j.1467-8624.1990.tb02762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons-Ruth K, Easterbrooks A, Cibelli C. Infant attachment strategies, infant mental lag, and maternal depressive symptoms: predictors of internalizing and externalizing problems at age 7. Dev Psychol. 1997;33:681–692. doi: 10.1037//0012-1649.33.4.681. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Jacobvitz D. Attachment disorganization: unresolved loss, relational violence, and lapses in behavioral and attentional strategies. In: Cassidy J, Shaver P, editors. Handbook of Attachment: Theory, Research, and Clinical Implications. Guilford; New York: 1999. pp. 520–554. [Google Scholar]
- Olds D, Eckenrode J, Henderson C, Jr, Kitzman H, Powers J, Cole R. Long-term effects of home visitation on maternal life course and child abuse and neglect: 15-year follow-up of a randomized trial. JAMA. 1997;278:637–643. [PubMed] [Google Scholar]
- Olds D, Henderson C, Kitzman H, Eckenrode J, Cole R, Tatelbaum R. The promise of home visitation: results of two randomized trials. J Community Psychol. 1998;26:5–21. [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Reinherz H, Gracey CA. The Simmons Behavior Checklist: technical information. Simmons College School of Social Work; Boston: 1983. [Google Scholar]
- Schweinhart L, Barnes H, Weikart D. Significant Benefits: The High/Scope Perry Preschool Study Through Age 27. High/Scope Press; Ypsilanti, MI: 1993. [Google Scholar]
- Stevenson-Hinde J, Shouldice A. Fear and attachment in 2.5-year-olds. Br J Dev Psychol. 1990;8:319–333. [Google Scholar]
- Tremblay R, Le Marquand D, Vitaro F. The prevention of oppositional defiant disorder and conduct disorder. In: Quay H, Hogan A, editors. Handbook of Disruptive Behavior Disorders. Kluwer Academic/Plenum Publishers; New York: 1999. pp. 525–555. [Google Scholar]
- Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: a comparison of child and parent training interventions. J Consult Clin Psychol. 1997;65:93–109. doi: 10.1037//0022-006x.65.1.93. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hollinsworth T, Kolpacoff M. The long-term effectiveness and clinical significance of three cost-effective training programs for families with conduct-problem children. J Consult Clin Psychol. 1989;57:550–553. doi: 10.1037//0022-006x.57.4.550. [DOI] [PubMed] [Google Scholar]


