Abstract
Study objectives
Because muscle paralysis makes it uncertain whether subjects with spinal cord injury (SCI) can perform spirometry in accordance with American Thoracic Society (ATS) standards, determinants of test failure were examined.
Design
Cross-sectional study.
Setting
Veterans Affairs (VA) medical center.
Participants
Veterans with SCI at VA Boston Healthcare System and nonveterans recruited by mail and advertisement.
Measurements and results
Two hundred thirty of 278 subjects (83%) were able to produce three expiratory efforts lasting ≥ 6 s and without excessive back-extrapolated volume (EBEV). In 217 of 230 subjects (94%), FVC and FEV1 were each reproducible in accordance with 1994 ATS standards. In the remaining 48 subjects, efforts with smooth and continuous volume-time tracings and acceptable flow-volume loops were identified. These subjects had a lower percentage of predicted FVC, FEV1, and maximum expiratory and inspiratory pressures compared to the others, and a greater proportion had neurologically complete cervical injury (42% compared to 16%). In 19 subjects (40%), some expiratory efforts were not sustained maximally for ≥ 6 s but had at least a 0.5-s plateau at residual volume (short efforts). In eight subjects (17%), some efforts were not short but had EBEV. In the remaining 21 subjects (44%), some efforts were short, some had EBEV, and some had both. If these efforts were not rejected, 262 of 278 subjects (94%) would have produced three acceptable efforts, and in 257 subjects (92%), the efforts were reproducible.
Conclusions
Subjects with SCI with the most impaired respiratory muscles and abnormal pulmonary function are able to perform spirometry reproducibly despite not meeting usual ATS acceptability standards. Exclusion of these subjects would lead to bias in studies of respiratory function in SCI. The modification of spirometry testing standards to include efforts with EBEV and with a 0.5-s plateau if < 6 s would reduce the potential for bias.
Keywords: reference standards, spinal cord injury, spirometry
Spinal cord injury (SCI) causes respiratory muscle weakness and paralysis and abnormal pulmonary function. Diseases of the respiratory system are the most common cause of death in chronic SCI.1 It is not known if there is an accelerated decline in lung function contributing to premature mortality, or whether respiratory illness and subsequent premature death are due to other factors. To assess this, we are currently examining longitudinal change in lung function in a large cohort of subjects with chronic SCI.
To be successful, such a study requires both acceptable and reproducible spirometry. The American Thoracic Society (ATS) has established acceptability standards that define the hesitation permitted at the start of a forced expiratory maneuver (method of back-extrapolated volume). Exhalation must last at least 6 s unless there is an obvious plateau in the volume-time curve. Whether ATS standards can be met is not known in SCI. In a pilot investigation,2 it appeared that expiratory muscle weakness caused a relatively long transition time between maximal inhalation and maximal exhalation, resulting in excessive back-extrapolated volume (EBEV) and unacceptable efforts. The results suggested, however, that if the efforts were technically acceptable (apparently satisfactory effort and no leaks, coughing, or glottis closure), the values for FVC and FEV1 were reproducible.2 The results also suggested that subjects whose respiratory muscles were most abnormal were least likely to sustain maximal expiratory efforts for ≥ 6 s, but were able to achieve at least a 0.5-s plateau in expiratory flow at residual volume (RV).
Our preliminary results also raised an issue of importance in the study of longitudinal change in pulmonary function in SCI: if subjects with the most impaired respiratory muscles tend to be excluded because ATS standards were not achieved, results would be biased. In this article, we address the questions raised by our earlier study by considering the determinants of test failure in a large cohort of subjects with SCI. We consider the effect that modifying ATS standards have on the assessment of spirometry acceptability and reproducibility, and consider the impact that these modifications would have on longitudinal studies of pulmonary function in neuromuscular disorders.
Materials and Methods
Population
Between October 1994 and July 1997, 309 subjects with chronic SCI were recruited to assess longitudinal change in pulmonary function. Recruitment was from a pool of 975 subjects, 859 of whom were followed up by the SCI Service at Veterans Affairs (VA) Boston Healthcare System. The remaining 116 were from the National Spinal Cord Injury Association of Massachusetts, New Hampshire, Vermont, Maine, and Rhode Island. Recruitment was by letter with a follow-up phone call, or subjects were approached while at the VA medical center. An additional 52 subjects responded to advertising in SCI journals or recruitment fliers. For inclusion, subjects had to be at least 20 years old, free from acute illness, be at least 1-year postinjury, and free of other neurologic disease. Two hundred sixty-three subjects were recruited from the VA Boston Healthcare System, 11 subjects were recruited from the National Spinal Cord Injury Association, and 35 subjects were recruited from advertising.
The final analytic data set included 278 subjects. Exclusions included subjects with other neuromuscular disease noted after testing (polio, stroke, or multiple sclerosis, n = 15), lung resection (n = 3), if SCI level was not assessed by examination (n = 5), if there was no motor SCI level when examined (n = 4), and 3 women. One subject was excluded because a chest brace could not be removed easily during pulmonary function testing. The protocol was approved by the VA Boston Institutional Review Board, and informed consent was obtained from each subject tested.
Spirometry
Since the study was initiated before the 1994 ATS spirometry guidelines, 1987 guidelines were used during testing. A DSII 10-L water seal spirometer (Warren E. Collins; Braintree, MA) was used. Calibration and leak tests were performed daily. The same technician tested all subjects. Subjects were seated, belts or pant waists were loosened, and nose clips were worn. The maneuver was demonstrated, and instructions were given to inhale completely and “blast” the air out. The subject was encouraged to exhale maximally and sustain the effort at least 6 s, or longer if possible depending on the ability and willingness of the subject to continue, as suggested in both the 1987 and 1994 guidelines. The volume-time curve was recorded on a kymograph, and the flow-volume loop was electronically displayed for review. An acceptable effort had a minimum exhalation time of 6 s, appeared maximal to the technician, had a rapid start of test, had a well-defined early peak in flow, and was smooth and continuous, without leaks. Coughing or glottis closure in the first second of exhalation was not permitted, nor was EBEV. Efforts were made to obtain three acceptable efforts. A maximum of eight expiratory efforts is suggested,3,4 but more were attempted based on the subject’s efforts and willingness to continue.
Volume-time and flow-volume loops were reviewed without regard to SCI level and recoded by at least two technicians and Dr. Garshick to reflect the 1994 ATS spirometry standards. In 1994, the extent of acceptable back-extrapolated volume was increased from 0.100 to 0.150 L, or 5% of the vital capacity, whichever was greater. Reproducibility standards were also modified such that the two largest FVC and the two largest FEV1 readings each had to be within 0.200 L rather than within 5% or 0.100 L, whichever was larger.3,4 In 1987,3 a plateau at the end of a volume-time curve was defined as no discernable volume change over at least 2 s, whereas in 1994,4 this was modified to 1 s.
Efforts with EBEV, but which were otherwise technically acceptable were noted, and the extent of EBEV recorded. For subjects with maximal efforts < 6 s, the duration of no detectable volume change at end-exhalation was also reviewed. Plateaus in expiratory flow at RV of 0.5 s to < 1 s, of 1 s to < 2 s, and of at least 2 s were recorded. Predicted pulmonary function values for white subjects were calculated based on Crapo et al,5 and adjusted for African Americans.6 Maximum expiratory pressure (MEP) and maximum inspiratory pressure (MIP) were measured three times using a pressure transducer and strip chart recorder or computerized data acquisition unit, and the maximal value was reported.7 MEP was obtained with a trumpet-style mouthpiece, use of which started later in the study, so MEP values were available for fewer subjects compared to values for MIP.
Questionnaire, Stature, Level of Injury
A respiratory questionnaire based on the ATS DLD-78 questionnaire was used to define “chronic cough” and “chronic phlegm,” and to assess cigarette smoking.8 “Any wheeze” was wheeze reported most days/nights, wheezing with a cold, or occasionally apart from a cold. A “chest illness” was one that kept a subject off work, indoors at home, or in bed in the preceding year. A trained physician (C.G.T.) determined level and motor completeness of injury based on American Spinal Injury Association guidelines.9,10 Subjects were weighed with a wheelchair scale, and supine length was measured.11 The subject was placed on a thin mat on a firm platform with the head touching a wall and legs fully extended. Length was measured from the wall to a right angle placed at either heel, taking care to have the subject’s heel perpendicular to the mat to eliminate the effect of foot and leg contractures secondary to muscle paralysis. Length was taken as the greater of left and right leg measurements. If severe contractures made measurement impossible or the subject declined measurement, self-reported height was used in the calculation of predicted values of pulmonary function.11
Analysis
SAS (Version, 6.08; SAS Institute; Cary, NC) was used for logistic regression, comparison of means (t test), and proportions (χ2). Data were expressed as mean ± 1 SD unless indicated otherwise.
Results
The mean ± SD age of the 278 subjects was 50.4 ± 14.9 years (range, 23 to 87 years), and mean years since injury was 18.2 ± 12.9 years (range, 1 to 52 years). There were 262 subjects who were white, 14 subjects who were African American, and 2 subjects were other races. One hundred seventy-seven subjects (63.7%) had neurologically motor complete injury: cervical (n = 57; 32.2%), high thoracic (T1–T6) [n = 48; 27.1%], low thoracic (T7–12) [n = 40; 22.6%], and lower levels (n = 32; 18.1%). Of the 101 subjects with neurologically incomplete injury, 60 subjects (59.4%) had a cervical level. There was not a significant difference between subjects with neurologically complete cervical SCI (n = 57) and all others (n = 221) in age (48.0 ± 13.2 years and 51.1 ± 15.3 years, respectively; p = 0.16) and in time since injury (19.9 ± 12.3 years and 17.7 ± 13.1 years, respectively; p = 0.27). Length was recorded in 220 subjects (79.1%).
Reasons for Test Failure
Overall, 230 of 278 subjects (82.7%) produced three expiratory efforts that were technically acceptable, without excessive EBEV based on the 1994 standards, and ≥ 6 s in duration. Of these, 217 subjects were able to produce efforts with the two largest FVC and the two largest FEV1 readings each within 0.200 L. Of the 48 subjects unable to produce three expiratory efforts lasting ≥ 6 s and without excessive EBEV, 19 subjects (39.6%) had some efforts that were only short (< 6 s with at least a 0.5-s plateau); 8 subjects (16.7%) had some efforts only with EBEV, and 21 subjects (43.8%) had some expiratory efforts that were either short, had EBEV, or both. The best FVC and FEV1 were selected from efforts that included those that were short or with EBEV or with both. These 48 subjects had a lower mean percentage of predicted FVC and FEV1, a lower mean MEP and MIP, had attempted more expiratory efforts (Table 1) compared to others, and included a greater proportion of subjects with neurologically complete cervical SCI (41.7% [20 of 48 subjects] vs 16.1% [37 of 230 subjects]), respectively (p < 0.0001). Age (p = 0.132), years since injury (p = 0.340), smoking history (current, p = 0.144; former, p = 0.961 when compared to never-smokers), respiratory symptoms (chronic cough, p = 0.786; chronic phlegm, p = 0.517; any wheeze, p = 0.793), and a history of chest illness (p = 0.663) were not significant predictors of failure to produce three efforts ≥ 6 s and without EBEV.
Table 1.
Comparison of Subjects With Three Expiratory Efforts ≥ 6 s Without EBEV and Subjects With Efforts < 6 s But With EBEV*
| Variables | Subjects, No. | Three Efforts ≥ 6 s and Without EBEV | Without Acceptable Efforts | p Value |
|---|---|---|---|---|
| % Predicted FVC | 271 | 78.5 ± 17.9 (n = 227) | 65.5 ± 17.4 (n = 44) | < 0.0001 |
| % Predicted FEV1 | 271 | 75.1 ± 18.2 (n = 227) | 68.8 ± 17.8 (n = 44) | 0.0370 |
| MIP, cm H2O | 258 | 89.2 ± 33.3 (n = 216) | 76.3 ± 32.4 (n = 42) | 0.0215 |
| MEP, cm H2O | 135 | 96.9 ± 40.7 (n = 115) | 75.3 ± 30.0 (n = 20) | 0.0248 |
| Expiratory efforts, No. | 278 | 6.1 ± 2.9 (n = 230) | 7.8 ± 3.8 (n = 48) | 0.0053 |
| % With > 8 efforts | 278 | 17.4 (n = 40) | 37.5 (n = 18) | 0.0018 |
Subjects who could not produce three efforts ≥ 6 s without EBEV attempted more expiratory efforts and had a lower mean MIP, MEP, and percentage of predicted FVC and FEV1. Percentage of predicted FVC and FEV1 were calculated for 271 of 278 subjects. Two subjects with race other than white or African American were excluded, and one subject with SCI due to a birth injury was excluded because it was not possible to accurately assess stature. In four subjects, none of the expiratory efforts was technically acceptable, so it was not possible to report a value for FVC or FEV1.
Factors Associated With Short Expiratory Efforts
Factors associated with short expiratory efforts and EBEV were examined separately in the 48 subjects unable to produce three acceptable expiratory efforts. In 29 subjects with 69 short expiratory efforts, 13 subjects (44.8%) had complete cervical injury. Subjects with short efforts also had a lower mean percentage of predicted FVC and FEV1 (60.1 ± 17.1%, p < 0.0001; 65.7 ± 19.4%, p = 0.0104), lower mean MIP (72.1 ± 28.2 cm H2O, p = 0.0158; n = 24), and lower mean MEP (69.4 ± 18.2 cm H2O, p = 0.0002; n = 13).
Short Expiratory Efforts and Expiratory Plateau Duration
In subjects with short efforts, an expiratory plateau lasted at least 2 s in nine efforts (13.0%) in eight subjects. Thirty efforts (43.4%) obtained in 16 subjects had an expiratory plateau of between 1 s but < 2 s, and 30 efforts (43.4%) in 19 subjects had an expiratory plateau of at least 0.5 s but < 1 s.
Factors Associated With Excessive Back-Extrapolation
Eighteen subjects (with 43 efforts overall) had at least one effort with EBEV (median, two efforts; range, one to seven efforts). The mean EBEV for each subject ranged from 6 to 10% (overall, 7.4 ± 1.2%). Of these 18 subjects, 8 subjects (44.4%) also had complete cervical injury. Subjects with EBEV had a lower mean percentage of predicted FVC (68.1 ± 20.5%, p = 0.0207) but a similar mean percentage of predicted FEV1 (72.6 ± 19.3%, p = 0.5847) and MIP (83.7 ± 31.6 cm H2O, n = 16; p = 0.5213). The mean MEP was 74.8 ± 27.9 cm H2O, which was less than the mean value of the subjects with three acceptable efforts, but was available in only six subjects and the difference did not achieve statistical significance.
Acceptability of Shorts Efforts and With EBEV
If efforts with EBEV, lasting < 6 s, but with ≥ 0.5-s plateau are considered to be acceptable, 94.2% (n = 262) of the cohort achieved three acceptable efforts and 98.1% (n = 257) of these met the 1994 ATS reproducibility standards (Fig 1). The impact of considering these “modified” criteria was greatest in the subjects with neurologically complete cervical SCI (Table 2). The proportion of these subjects able to achieve at least three acceptable efforts increased from 64.9 to 87.7%.
Figure 1.
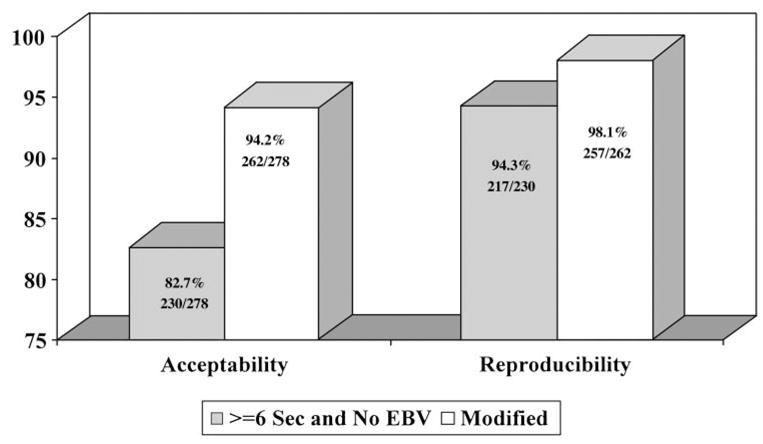
Proportion of subjects with acceptable and reproducible spirometry based on expiratory efforts ≥ 6 s (Sec) and without EBEV (EBV), and modified criteria as defined in this article. If modified criteria are adopted, the proportions of subjects with acceptable and reproducible spirometry results are greater.
Table 2.
Subjects Able To Produce Three Acceptable Expiratory Efforts ≥ 6 s Without EBEV and Efforts Meeting Modified Standards*
| Variables | Neurologically Complete Cervical SCI, ≥ 6-s Exhalation and No EBEV | Neurologically Complete Cervical SCI, Includes Efforts < 6 s with 0.5-s Plateau; EBEV Permitted | Others With SCI, ≥ 6-s Exhalation and No EBEV | Others With SCI, Includes Efforts < 6 s with 0.5-s Plateau; EBEV Permitted |
|---|---|---|---|---|
| Acceptability | 64.9 (37/57) | 87.7 (50/57) | 87.3 (193/221) | 95.9 (212/221) |
| Reproducibility | 66.7 (38/57) | 87.7 (50/57) | 81.0 (179/221) | 93.7 (207/221) |
Data are presented as % (No. of patients/total patients). Reproducibility standards are based on 1994 ATS standards. Use of modified acceptability criteria in subjects with neurologically complete cervical injury increased the proportion of subjects with reproducible spirometry compared to others with neurologically complete and incomplete SCI.
Reproducibility of FVC
There were 42 subjects in the study cohort with their largest FVC taken from an effort that was short, had EBEV, or both. In 17 subjects with short efforts, but who also had an effort of at least 6 s without EBEV, the median difference between FVC values was 0.080 L, and in 82% (14 of 17 subjects), the two values were within 0.200 L. In 31 subjects with EBEV, the median difference between FVC values was 0.060 L, and in 90% (28 of 31 subjects), the two values were within 0.200 L.
Reproducibility of FEV1 Measurements
There were 57 subjects with their largest FEV1 reading taken from an effort that was either < 6 s, had EBEV, or both. In 22 subjects with short efforts, but who also had an effort of least 6 s and without EBEV, the median difference between FEV1 values was 0.090 L; in 77% (17 of 22 subjects) the two values were within 0.200 L. In 44 subjects with EBEV, the median difference between the FEV1 values was 0.080 L; in 89% (39 of 44 subjects), the values were within 0.200 L.
Discussion
We examined whether subjects with SCI could perform acceptable and reproducible spirometry. Seventy-eight percent (217 of 278 subjects) were able to meet usual 1994 ATS acceptability and reproducibility criteria. Subjects unable to expire maximally for 6 s without EBEV had a lower mean percentage of predicted FVC and FEV1, lower mean MIP and MEP, and were more likely to have a neurologically complete cervical injury. When standards were broadened so that two common causes of test failure in SCI (EBEV and short exhalation time) were considered acceptable, 92.4% of all subjects and 87.7% of subjects with neurologically complete cervical injury were able to produce three acceptable efforts that, of importance, met ATS reproducibility criteria.
These results are similar to those from most population-based and occupational cohort studies in able-bodied subjects that showed that ATS acceptability and reproducibility standards for FEV1 were achieved in 82.3 to 97.9%.12–17 Our data are similar to those of prior studies, in that subjects unable to meet ATS standards had the most abnormal pulmonary function.12–16 Able-bodied subjects unable to perform spirometry according to ATS standards have a greater rate of decline in FEV1 and increased mortality,12–16 but comparable data in SCI are not available. Although a history of respiratory symptoms has predicted spirometry test failure in able-bodied subjects, this was not found in our SCI cohort. The reason for this difference is not apparent.
The most common problem was failure to exhale maximally for a minimum of 6 s, in spite of being encouraged to do so. These individuals, who included a greater proportion of subjects with complete cervical injury, had the most impaired pulmonary function and ventilatory muscles. They did not complain of discomfort or shortness of breath during the test. The reason for not exhaling maximally for ≥ 6 s is not apparent to us. In order to address the acceptability of efforts < 6 s, end-of-test criteria are applied. When the study started, the 1987 ATS standards that were in effect that required a 2-s plateau at end-exhalation, a criterion that would have excluded the majority of subjects with short expiratory efforts. Between 1987 and 1994, the end of test criteria changed from 2 to 1 s, and in this study assessed the effect of broadening this to a 0.5-s plateau. We reasoned that RV had been reached, likely the case because of the reproducibility of the FVC in subjects with short efforts.
EBEV was the other reason for failure to meet ATS criteria in our subjects with SCI. The extent of EBEV was modest, a mean of 6 to 10% in each subject, with an overall mean of 7.4%. The degree of EBEV is well with the ATS standards prior to 1987 (10% of the vital capacity or 0.100 L, whichever is greater). This was reduced to 5% because of concern regarding submaximal expiratory efforts and slow starts. Subjects with expiratory muscle weakness appear to have insufficient acceleration of the respiratory system at the onset of expiratory effort. That subjects unable to produce three acceptable efforts due to EBEV was most common in those with the most abnormal MEP and in those with neurologically complete cervical injury (whose ventilatory muscles are impaired most) is consistent with this idea. As illustrated in these data, the FEV1 reading from such efforts may be larger than those obtained when a more maximal effort is performed. This is due both to the larger extent of volume exhaled without being timed and to less dynamic airway compression. However, in this study subjects with EBEV produced values that met ATS reproducibility standards despite muscle weakness.
In longitudinal studies of pulmonary function, the exclusion of subjects unable to perform spirometry according to current ATS standards could lead to biased results because subjects with the most abnormal pulmonary function would be excluded. The ATS has recognized that exclusion of research subjects unable to produce reproducible spirometry should be left up to the investigator.3 However, our data indicate that ATS standards for acceptability in able-bodied subjects are not appropriate for use in SCI. Our data suggest that strict application of all ATS acceptability criteria is not necessary because the reproducibility of FVC and FEV1 in our subjects should allow detection of longitudinal changes in pulmonary function at all levels and neurologic completeness in SCI. Furthermore, the reproducibility of the data obtained using these criteria suggests that it is appropriate to tailor spirometry acceptability and criteria to fit both the purpose for which the data are being acquired and the population of subjects being studied. It is suggested these modified standards may also be appropriate to prevent bias in the reporting of results in cohorts with other neuromuscular diseases, but to our knowledge this has not been studied.
Acknowledgments
We thank the physicians, staff, and patients of the VA Boston Spinal Cord Injury Service, Seth Cohen, and Matthew F. Wein, for programming assistance.
Abbreviations
- ATS
American Thoracic Society
- EBEV
excessive back-extrapolated volume
- MEP
maximum expiratory pressure
- MIP
maximum inspiratory pressure
- RV
residual volume
- SCI
spinal cord injury
- VA
Veterans Affairs
Footnotes
Presented in abstract form at the 1999 annual meeting of American Thoracic Society, April 23–28, 1999; San Diego, CA.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Supported by Health Services R&D (Dr. Garshick), Medical Research Service (Dr. Brown), the Massachusetts Veterans Epidemiology Research and Information Center, Department of Veterans Affairs.
References
- 1.DeVivo MJ, Stover SL. Long-term survival and causes of death. In: Stover SL, DeLisa JA, Whiteneck GG, editors. Spinal cord injury: clinical outcomes from the model systems. Portland, OR: Book News; 1995. pp. 289–316. [Google Scholar]
- 2.Ashba J, Garshick E, Tun CG, et al. Spirometry: acceptability and reproducibility in spinal cord injured subjects. J Am Paraplegia Soc. 1993;16:197–203. doi: 10.1080/01952307.1993.11735901. [DOI] [PubMed] [Google Scholar]
- 3.American Thoracic Society. Standardization of spirometry, 1987 update. Am Rev Respir Dis. 1987;136:1285–1298. doi: 10.1164/ajrccm/136.5.1285. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 5.Crapo RO, Morris AH, Gardner R. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981;123:659–664. doi: 10.1164/arrd.1981.123.6.659. [DOI] [PubMed] [Google Scholar]
- 6.Rossiter CE, Weill H. Ethnic differences in lung function: evidence for proportional differences. Int J Epidemiol. 1974;3:55–61. doi: 10.1093/ije/3.1.55. [DOI] [PubMed] [Google Scholar]
- 7.Tully K, Koke K, Garshick E, et al. Maximal expiratory pressures in spinal cord injury using two mouthpieces. Chest. 1997;112:113–116. doi: 10.1378/chest.112.1.113. [DOI] [PubMed] [Google Scholar]
- 8.Ferris BG. Epidemiologic standardization project (American Thoracic Society) Am Rev Respir Dis. 1978;118(6 Pt 2):1–120. [PubMed] [Google Scholar]
- 9.International standards for neurological and functional classification of spinal cord injury, revised 1996. Chicago, IL: American Spinal Injury Association, International Medical Society of Paraplegia; 1996. [Google Scholar]
- 10.Wien MF, Garshick E, Tun CG, et al. Breathlessness and exercise in spinal cord injury. J Spinal Cord Med. 1999;22:297–302. doi: 10.1080/10790268.1999.11719583. [DOI] [PubMed] [Google Scholar]
- 11.Garshick E, Ashba J, Tun CG, et al. Assessment of stature in spinal cord injury. J Spinal Cord Med. 1997;20:36–42. doi: 10.1080/10790268.1997.11734580. [DOI] [PubMed] [Google Scholar]
- 12.Eisen EA, Oliver LC, Christiani DC, et al. Effects of spirometry in two occupational cohorts. Am Rev Respir Dis. 1985;132:120–124. doi: 10.1164/arrd.1985.132.1.120. [DOI] [PubMed] [Google Scholar]
- 13.Eisen EA, Robins JM, Greaves IA, et al. Selection effects of repeatability criteria applied to lung spirometry. Am J Epidemiol. 1984;120:734–742. doi: 10.1093/oxfordjournals.aje.a113941. [DOI] [PubMed] [Google Scholar]
- 14.Kellie SE, Attfield MD, Hankinson JL, et al. Spirometry variability criteria-association with respiratory morbidity and mortality in a cohort of coal miners. Am J Epidemiol. 1987;125:437–444. doi: 10.1093/oxfordjournals.aje.a114549. [DOI] [PubMed] [Google Scholar]
- 15.Eisen EA, Dockery DW, Speizer FE, et al. The association between health status and the performance of excessively variable spirometry tests in a population-based study in six U.S. cities. Am Rev Respir Dis. 1987;136:1371–1376. doi: 10.1164/ajrccm/136.6.1371. [DOI] [PubMed] [Google Scholar]
- 16.Ng’ang LW, Ernst P, Jaakkola M, et al. Spirometric lung function: distribution and determinants of test failure in a young adult population. Am Rev Respir Dis. 1992;145:48–52. doi: 10.1164/ajrccm/145.1.48. [DOI] [PubMed] [Google Scholar]
- 17.Enright PL, Johnson LR, Connett JE, et al. Spirometry in the Lung Health Study: 1. Methods and quality control Am Rev Respir Dis. 1991;143:1215–1223. doi: 10.1164/ajrccm/143.6.1215. [DOI] [PubMed] [Google Scholar]


