Abstract
Reggio Emilia hospital installed Picture Archiving and Communications Systems (PACS) as the final step towards a completely digital clinical environment completing the HIS/EMR and 1,400 web/terminals for patient information access. Financial benefits throughout the hospital were assessed upfront and measured periodically. Key indicators (radiology exam turnaround time, number of radiology procedures performed, inpatients length of stay before and after the PACS implementation, etc.) were analyzed and values were statistically tested to assess workflow and productivity improvements. The hospital went “filmless” in 28 weeks. Between the half of 2004 and the respective period in 2003, overall Radiology Department productivity increased by 12%, TAT improved by more than 60%. Timelier patient care resulted in decreased lengths of stay. Neurology alone experienced a 12% improvement in average patient stay. To quantify the impact of PACS on the average hospital stays and the expected productivity benefits to inpatient productivity were used a “high level” and a “detailed” business model. Annual financial upsides have exceeded $1.9 millions/year. A well-planned PACS deployment simplifies imaging workflow and improves patient care throughout the hospital while delivering substantial financial benefits. Staff buy-in was the key in this process and on-going training and process monitoring are a must.
Key words: PACS, cost savings, cost-effectiveness, efficiency, PACS system, performance, patient stay
BACKGROUND
Hospital Transition to Full Digital Imaging
Reggio Emilia’ Arcispedale Santa Maria Nuova is a 900-bed public regional acute care hospital. Major investments in medical equipment and health care information systems have been made in recent years. The hospital invests more than 2% of its global budget in Information Technology (IT, Picture Archiving and Communications Systems (PACS) excluded) annually. Approximately 180,000 imaging examinations are performed every year by the Radiology Department, with a large outpatient population of 40%. Emergency department represents 31% of the workload, while inpatient and day patients account for the remaining 29%.
Transition to Full Digital Imaging
A joint multifunctional management project team for PACS was formed during initial project phase and continues to provide guidance in ongoing PACS operations. The team set clear criteria to monitor the implementation and measure the clinical and business outcomes,1–3 providing solutions for specific clinical departmental requirements such as digital orthopedic preoperative planning for the operating room. A medical representative from each of the 37 hospital wards is on the team. Specifications for the system included full PACS/RIS/HIS and modality integration, load balancing mutual take-over PACS server configuration, “Everything on Line (EOL)” architecture in the form of Kodak DirectView PACS 5.2,4–6 automatic speech recognition systems (ASRS), and web-based full-depth 12-bit image ward distribution via an intranet PACS web access on any of the hospital’s 1,400 personal computers.
The deployment was performed in a multistep approach (Table 1). Extensive user training on the PACS web module involved more than 400 medical and nursing professionals.7 To facilitate and accelerate the use of the IT process, a portion of the clinical staff’s incentive plan was tied to the Electronic Patient Record (EPR) component deployment. As an example, during the first half of 2004, 50% of the bonuses were tied to the transition from paper to electronic radiology examination orders.
Table 1.
Schedule of the Implementation of PACS
| Date | Main Activity |
|---|---|
| April 15, 2003 | PACS go live. CT and MR examination archived on PACS. Filmless start in Radiology Department |
| June 15, 2003 | Starts test web images distribution in Neurology |
| July 21, 2003 | No more film printed for CT/MR examinations of inpatient requested by pilot departments |
| August 4, 2003 | No more film printed for CT/MR examinations for outpatient (referral and paper print of key images) |
| October 1, 2003 | Hospital filmless transition completed (images web distribution extended to all departments) |
| May 5, 2004 | 100% digital radiological procedures ordering completed on HIS |
| June 14, 2004 | Referral and images CD for all outpatients |
Measuring PACS Benefits
Peer experience indicates that PACS enables increased productivity in imaging procedures, as well as improved patient care and patient satisfaction.1,2 Three key areas were measured over time (both pre- and post-PACS), analyzed, and documented7–9: film consumption; number and charges billed for outpatient procedures; and inpatient productivity. The number of inpatient procedures were not analyzed per se as in Italy type and number of imaging procedures performed for inpatients do not influence inpatient reimbursements, tied only to DRG reimbursements (business benefits can be related on hospital stay that can be shortened by increased productivity, limiting patient discharge delay due to reports and images unavailability).
Number and Charges Billed for Outpatient Procedures
A set of queries was created to automatically extract the pre and post-PACS information (respectively from October 15th 2002 to April 15th 2003 and from October 15th 2003 to April 15th 2004) from the HIS/RIS data for type and number of outpatient procedures and average ordering waiting time (in days) necessary to have a nonurgent procedure performed. The latter can be a good proxy for recaptured reimbursements from the private sector.8,9
Inpatient Hospital Productivity
Even if the patient stay involves multiple factors, it is reasonable to assume that faster availability of reports can produce quicker clinical treatment. The corresponding improved patient discharge rate may be providing timely and hopefully improved patient care. A set of queries was created to automatically extract the information from the HIS/RIS data for the turnaround time (TAT) and hospital stay measurements. The data before and after the PACS implementation was measured using the same metrics and during the same time of year, thereby eliminating any seasonality effect. Patients who had at least one imaging examination during their hospital stay were compared to patients who had no imaging examination during their hospital stay. Imaging order comparisons were made as well, measuring the average number of examinations per patient.
To assess each clinical department’s reaction to the PACS implementation, each finding was validated by the ward supervisors and staffs via a predetermined form. Evaluation included time required to complete radiological procedures, time to image and report availability, as well as accessibility of previous examinations.
Two different methods were used to quantify the PACS’ impact on the length of average hospital stay and the corresponding inpatient productivity. The first method, called “high level business model approach”, was developed during the initial phase of this study to predict the impact of an integrated PACS/RIS/HIS system.4 This is based on the concept that image and report availability influences the length of the patient’s hospital stay, either by enabling earlier treatment or earlier discharge. The second method, called “detailed business model approach”, considers each hospital department’s performance, and measures each performance improvement. Seventeen clinical and surgical departments were analyzed, ensuring no significant change in the clinical or surgical protocols, nor any unit organizational change. The key variables that the project team chose to analyze and validate were Radiology “turnaround time” and inpatient hospital stay. TAT is defined as the sum of the time that elapses between the moment an imaging exam is ordered, its execution time (ET), and the reporting time (RT), which is the time lapse between the image execution time and the availability of the imaging exam’s report. Turnaround time is the input and inpatient hospital stay is the output used to calculate the resulting hospital productivity. Statistical analysis was performed on the means, median, and variances to validate the results relative to TAT and “hospital stay by unit” both before and after PACS implementation, using Minitab (Minitab release 14, Minitab Inc., PA, USA). Distribution always tested for normality, and none proved to be modeled statistically by a normal curve. Therefore, for variance statistical analysis, Levene test was used; and for median, mood median test was used. F test and ANOVA one-way t tests were used for means analysis. The team checked to ensure that no significant clinical treatment protocol change or staffing change had occurred in the considered timeframes. The “hospital stay” was analyzed for consistency against department flow (chronic versus “regular” patients), use of radiology services, and diagnose related grouping (DRG and/or ICD9 codes), whenever possible. The 17 units that were analyzed were those that ordered the greatest number of radiology procedures for inpatients being prioritized; in this respect, neurology was the first. To quantify economical improvement, media differences were used when the central values had changed. If the variance analysis had also changed, a P95 approach was used.
RESULTS
Film Savings
Film savings during the period immediately following system installation, April to October, 2003, were 15%, and grew to 90% as soon as the workflow became filmless 28 weeks after go live. Only mammography remained film-based. All of the studies’ images were available on intranet PACS web distribution. Outpatients’ key images are automatically burned on CD. Patients who require iconography film prints pay an additional fee. Film savings correspond to $0.84 million per year versus pre-PACS.
Outpatient Productivity
Data analysis measured a 7% increase in the number of radiology department imaging procedures year over year during the same 6-month period (October 15 to April 15) with no increase in the number of technologists or radiologists,13 thanks to the combined PACS and CR/DR implementation. The first year’s period (10/15/02–4/15/03) was pre-PACS implementation; the second year’s period (10/15/03–4/15/04) was postimplementation. Before the PACS implementation, outpatient examination reports were delivered in 5 days. After the introduction of PACS, this time was reduced to 3 days. Urgent examination responses were delivered immediately and the report delivery process did not change during this time.
The elimination of the off-line reports typing has freed up staff resources for other tasks: reminders to outpatients regarding scheduled procedures and filling slots made available by cancellation or reschedule requests. This process enhancement decreased average waitlists for outpatients from 90 to 40 days for nonurgent CT exams and from 90–180 down to 30–60 days for nonurgent ultrasound scans. Shorter waitlists enabled increased outpatient business. Total reimbursements invoiced by the Radiology Department rose 12.9% to $4.2 million during the post-PACS implementation period referenced in Table 2 (line 2). This far exceeds the average annual increase of the preceding 2 years, 2001 and 2002, at 4.7% and 5.2%, respectively. The economical benefit corresponding to the increased number and the higher complexity (average cost per exams rose by more than 5%) of outpatient examinations directly reimbursed to the Hospital, was estimated in more than $0.55 million for the year 2004 (with PACS) with respect to the 2003 (pre-PACS).
Table 2.
Total Reimbursements Invoiced by the Radiology Department
| Number of exams | Equivalent reimbursement | Average exams Cost | Radiology Department working staff (No. eq. full time) | Productivity (per full time) | |
|---|---|---|---|---|---|
| Pre-PACS (10/15/02–4/15/03) | 78,904 | $3,716,368 | $47.1 | 92.5 | $40,177 |
| With PACS (10/15/03–4/15/04 | 84,532 | $4,197,242 | $49.7 | 88.5 | $47,426 |
| Differences | 7.1% | 12.9% | 5.4% | −4 FTEs | 18.0% |
Radiology Department Turnaround Time
Effects of PACS and ASRS on Execution and Reporting Time
Assuming the different percentages of examinations referred/executed/completed as a function of time could be adopted as workflow indicators, a detailed statistical analysis on the TAT data demonstrated that the sample populations corresponded to pre- and post-PACS situations belonged to two different distributions with a 5% confidence level (t test groups). For CT, MRI, general X-ray, or mammography examinations, the percentage of executed examinations in function of time failed to show statistical difference in the image acquisition process: the introduction of digital radiographic image acquisition systems did not produce a statistically significant reduction of the average execution time. Greater productivity is a result of improved workflow (scheduling ability and the resulting reduction of the “idle time”).
The t test for a difference between the percentages of referred examination in function of time showed statistically significant difference in the reporting process with and without PACS.10–12 ASRS in radiologist reporting process permitted greatly diminished average report times for mammography and ultrasound examinations also (Table 3).
Table 3.
p Values Obtained by Student t test on Different Acquisition Modality Execution Time (ET), Referral Time (RT) and Turn Around Time (TAT) between Execution Time, Referral Time and Turn Around Time Pre- and Post-PACS
| Modality | ET | RT | TAT |
|---|---|---|---|
| General X-ray | 0.385 | 4.60E-07 | 1.32E-05 |
| CT | 0.608 | 1.57E-04 | 1.72E-04 |
| MRI | 0.732 | 3.46E-05 | 3.6E-04 |
| US | 0.561 | 1.81E-15 | 2.85E-12 |
| Mammography | 0.592 | 6.83E-06 | 2.51E-05 |
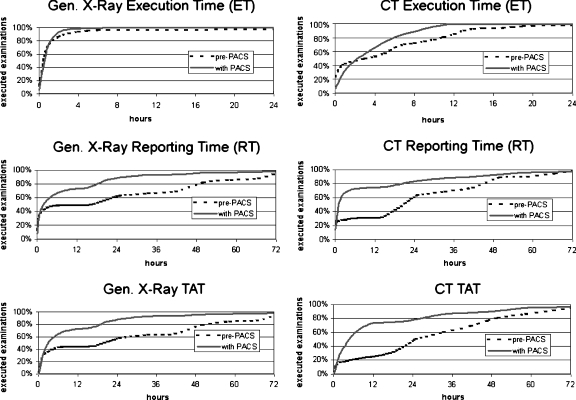
In general, execution time almost never exceeded the daily work time of 12 hours. On the other hand, referral time before PACS and ASRS was typist-dependent, assuming a characteristically step trend (clearly visible in Fig. 1). Please note that 12-hour continuums correspond to the two daily 6-hour work shifts and 12-hour plateaus correspond to night breaks. This is, of course, less evident after introduction of PACS and ASRS (Table 4).
Fig. 1.
Percentage of executed, referred, and completed examination as a function of the time for general X-ray and CT examinations in pre-PACS (dotted line—from 10/15/2002 to 04/15/2003) and with PACS (continuous line—from 10/15/2003 to 04/15/2004) condition
Table 4.
Pre- and Post-PACS Average TAT (hours) for Different Acquisition Modality
| Modality | Pre-PACS | Post-PACS | Difference | Variability |
|---|---|---|---|---|
| General X-ray | 42.1 | 15.4 | −64 % | Statistically reduced >3 times |
| CT | 40.5 | 20.0 | −52% | Statistically reduced 8 times |
| MRI | 44.5 | 32.6 | −28% | Variability statistically not changed |
| Mammography | 41.1 | 16.2 | −61% | Variability statistically reduced >3 times |
Inpatient Workflow
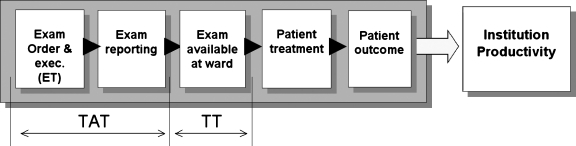
Figure 2 describes the workflow for inpatients requiring radiology procedures and demonstrates how radiology performance influences the length of hospital stay.8–10,14 As stated before, TAT decreased with PACS introduction over 60%, even without adding benefits from eliminating transmission time (TT). MRI, CT, and radiography exams were studied. In all cases, the sample size was statistically significant and large in absolute terms. It is important to note that the transmission time (TT) from the radiology department to the ward was not taken into account. Before PACS, TT was estimated to be between 8–12 hours range, unless the department sent someone to pick up the study (films and report). After PACS implementation, the TT is a matter of seconds.15
Fig. 2.
Workflow of radiology procedures process. The turnaround time, TAT, is defined as the sum of the time that elapses between an imaging examination is ordered and executed. The transfer time, TT, is the time to deliver images and referral to the clinical units. In a fully integrated digital environment images and referrals are immediately available to the ward (TT = 0). In an analogue one, film and paper printed reports need to be physically carried from Radiology to the ordering clinical or surgical unit.
Inpatient MRI Scans
For MRI scans, the mean TAT decreased from 38.4 to 24.9 hours; the median decreased from 29.1 to 11.0 hours, with an improvement of 18.1 hours or 62% (p < 0.001); the “(Q3–Q1)” indicator, used as a proxy for variance and spread, decreased from 42.2 to 28.2 hours (Table 5). Mean and median distributions were statistically different, showing a p-value equal to zero in both cases (note: variance p-value Levene’s test, for nonnormal distributions, is equal to 0.220). Execution time (ET) did not change much; the mean moved from 2.6 to 2.5 hours, and the median increased from 0.6 to 1.4 hours.
Table 5.
Pre- and Post-PACS Inpatient MRI Procedures’ TAT
| MRI scans TAT | Number of exams | Mean (hours) | Standard deviation (hours) | Median (hours) | Q3–Q1 (hours) |
|---|---|---|---|---|---|
| Pre-PACS (1/1/03–30/4/03) | 481 | 38.35 | 28.5 | 29.1 | 42.2 |
| With PACS (1/1/04–30/4/04) | 496 | 24.90 | 31.6 | 11.0 | 28.2 |
| Improvement | 13.4 | 18.1 | 14.0 |
Inpatient CT Scans
For CT scans, the mean TAT decreased from 29.6 to 13.5 hours. The median decreased from 21.1 to 3.1 hours (p < 0.001), a sevenfold improvement. The “(Q3–Q1)” criteria, used as a proxy for variance and spread, decreased from 42.2 to 8.2 hours, an eightfold improvement (Table 6). Mean, median, and variance distributions were statistically different, showing a p-value equal to zero in all cases. Analysis on ET and RT displayed findings similar to those of the MRI studies.
Table 6.
Pre- and Post-PACS Inpatient CT Procedures’ TAT
| CT scans TAT | Number of exams | Mean (hours) | Standard deviation (hours) |
|---|---|---|---|
| Pre-PACS (1/1/03–30/4/03) | 2,093 | 29.6 | 32.36 |
| With PACS (1/1/04–30/4/04) | 1,954 | 13.5 | 24.75 |
| Improvement | 16.1 |
Inpatient Radiography Exams—Chest
To understand the improvement of traditional radiography exams, the chest x-ray examination was analyzed as one of the most common and standardized procedure. The mean TAT decreased from 36.0 to 8.9 hours (p < 0.001) and the median decreased from 20.6 to 2.5 hours, an improvement of 18.0 hours or an eightfold improvement. The “(Q3-Q1)” criteria, used as a proxy for variance and spread, decreased from 44.5 to 4.9 hours, a ninefold improvement. Mean, median, and variance distributions were statistically different, showing a p-value equal to zero in all cases (Table 7).
Table 7.
Pre- and Post-PACS Inpatient Chest Radiography Exams’ TAT
| Chest exams TAT | Number of exams | Mean (hours) | Standard deviation (hours) | Median (hours) | Q3–Q1 (hours) |
|---|---|---|---|---|---|
| Pre-PACS (1/1/03–30/4/03) | 6,754 | 33.9 | 56.25 | 19.1 | 44.2 |
| With PACS (1/1/04–30/4/04) | 7,456 | 9.62 | 26.09 | 2.6 | 5.5 |
| Improvement | 24.3 | – | 16.5 | 39.3 |
Reporting time decreased for the modalities. Even though dictation time is longer for the radiologist with the digital solution, the very nimble reporting process offsets this shortfall with a substantial gain.
Hospital Productivity Driven by Improved Radiology Workflow
The number of inpatients treated in the first half of 2004 versus the first half 2003 did not change: 16,207 versus 16,362.
Inpatient Hospital Productivity Assessment—High-level Business Model Approach
The improved Radiology performance contributes to hospital workflow by enabling the clinical and surgical wards to begin earlier treatment and/or to safely discharge the patient due to the immediate availability of the necessary images and reports according to the relevant clinical protocols.
By extracting the data from the RIS, and assuming savings of a full day in the length of patient stay for each exam performed in the 24-hour period before patient discharge, the hospital anticipates a $2.3 million benefit a year (Table 8). The contribution of earlier treatment decision was not evaluated because the examinations are generally performed before scheduled admissions (day surgery or day hospital admissions are usually preferred over longer and more expensive treatments).
Table 8.
High-level Business Model Approach Expected Benefit. The Percentage of Significant Exams is Assumed as the Percentage of Examination Performed 24 Hours Before Patient Discharge
| Type of procedure | Number of inpatient exams per year | Average hospital patient daily cost | Significant Exams | Expected benefit |
|---|---|---|---|---|
| MRI | 1,740 | $415 | 44% | $328,556 |
| CT | 5,376 | 26% | $483,982 | |
| Radiography | 22,443 | 16% | $1,487,890 | |
| Total | $2,300,428 | |||
Inpatient Hospital Productivity Assessment—Detailed Business Model Approach
The four most important departments of the 17 that showed actual improvements during analysis, are documented in the following section.
Neurology
Neurology treated 589 patients during the first half of 2004, an increase of 9% over the previous year. While 13% did not require radiology procedures, the Chi-square analysis suggested that the “with/without radiological examinations” had not changed during the study period (p-value = 0.276, Chi-square = 1.888). The data from the first half of 2003 and 2004, respectively (Table 9) show a decrease in the mean of 6%, to 10.2 days, a statistically valid decrease for the median of 12% to 7.9 days. Variability decreases as well, but not in statistical terms. Results for the most frequent DRG (DRG014) showed similar patterns (Table 9). For a population of 174 patients, 159 with radiology procedures, length of patient stay with imaging procedures decreased statistically from 8.9 to 6.9 days, with variability increasing mathematically from 6.9 to 7.3 days. The total annual economic benefit is estimated at $360,000, for approximately 1,100 patient bed/days saved, at $331/day.
Table 9.
Patient Stay, Neurology. Pre- and Post-PACS Comparison
| Neurology patients | Patients treated | Patients Treated with Rad. Exam. | Mean (days) | Standard deviation (days) | Median (days) | Q3–Q1 (days) |
|---|---|---|---|---|---|---|
| Pre-PACS (1/1/03–30/6/03) | 541 | 454 | 10.8 | 7.9 | 9.0 | 9.6 |
| With PACS (1/1/04–30/6/04) | 589 | 499 | 10.2 | 8.1 | 7.9 | 8.6 |
| Improvement | +9% | +10% | 6% | −2% | 12% | 11% |
| P = value | 0.197 | 0.589 (F-test) | 0.042 | 0.916 (Levene) |
Thoracic Surgery
The unit treated 224 patients in the first half of 2004, an increase of 14% over the prior year, without altering the number of postsurgery beds available. The amount of “with/without radiological examinations during stay” had changed during the studied period (p-value = 0.016, Chi-square = 11.755). Fifteen percent of the patients in 2004 did not require radiology procedures during their stay, down from 24% the year before. If we study the patient population with radiology procedures during their stay, the data from the first half of 2003 and 2004 respectively show a mathematical decrease for the means of 16% to 7.8 days, with a decrease for the median of 11% to 6.3 days. Variability decreased 42% (F-test p < 0.001, Levene’s p = 0.105). In this case, the benefit is driven by planning the surgical procedures and patient discharges well, as well as the resulting new admissions. Referring physicians felt more comfortable about the greater perceived probability of getting the radiology images and reports within the required time (Table 10). The total economical benefit for the year is estimated at $480,000, for approximately 578 patient bed/days saved.
Table 10.
Thoracic Surgery Patient with Radiological Procedures. Pre- and Post-PACS Patient Stay
| Thoracic surgery patients | Patients Treated | Mean (days) | Standard Deviation (days) | Median (days) | Q3–Q1 (days) |
|---|---|---|---|---|---|
| Pre-PACS (1/1/03–30/6/03) | 149 | 9.3 | 10.6 | 7.0 | 6.1 |
| With PACS (1/1/04–30/6/04) | 191 | 7.8 | 6.1 | 6.3 | 6.3 |
| Improvement/change | +28% | 16% | 42% | 11% | −3% |
| P = value | 0.100 | 0.000 (F-test) | 0.325 | 0.105 (Levene) |
Internal Medicine
The Internal Medicine ward, specialized in hypertension disorder and diabetic patients, treated 874 patients in the first half of 2004, with a decrease of 2.6% versus the year before, reflecting somewhat the decrease of capacity (-6 patient beds). The unit did not change significantly its clinical protocols, as patients using radiology services shrank 6% to 497 (Chi-square p value = 0.450). Overall stay for the department decreased mathematically 7% from 11 to 10.2 days (means) and 3% from 8.7 to 8.3 days (medians); F-test and Levene’s test p values for variance analysis are respectively less than 0.001 and equal to 0.079. While median stay for patients without radiology services did not change—means moved from 7.4 to 7.2 days, medians stable at 6.1 days, patient stay with radiology procedures diminished statistically 10% for both means and medians, from 13.0 to 11.7 days (means) and from 11.1 to 10.0 days (medians). Variability also decreased 6% (Table 11). The two most frequent DRGs show results in line with the general analysis. The total economical benefit for the year is estimated at $193,000, for approx. 920 patient bed/days saved.
Table 11.
Internal Medicine Patient with Radiological Procedures. Pre- and Post-PACS Patient Stay
| Internal medicine patients | Patients treated | Mean (days) | Standard deviation (days) | Median (days) | Q3–Q1 (days) |
|---|---|---|---|---|---|
| Pre-PACS (1/1/03–30/6/03) | 526 | 13.0 | 8.7 | 11.1 | 10.1 |
| With PACS (1/1/04–30/6/04) | 497 | 11.7 | 7.4 | 10.0 | 9.5 |
| Improvement/change | −6% | 10% | 15% | 10% | 6% |
| P = value | 0.011 | 0.000/F-test) | 0.047 | 0.045 (Levene) |
Other Wards
Other units positively benefited by PACS availability: Gastroenterology, Orthopaedics, Vascular Surgery, Neonataology, Children’s Neuropsychiatry, Pneumology, and Neurotrauma experienced a total savings of approximately $870,000 and 1,500 patient bed/days.
The total outcome of the detailed business exceeds $1.9 million per year.
High-level Versus Detailed Business Model Approach
The high-level and detailed business models deliver the same order of savings ($2.3 million per year versus $1.9 million per year, respectively). The high-level approach represents the “theoretical” saving limit achievable with the existing workflow. The detailed business model approach represents the actual (“real life”) estimate.
DISCUSSION
After 18 months, the business outcome upside is evaluated in excess of $2.45 million per year ($1.9 million TAT + $0.55 million outpatient productivity), nearly three times the film savings of $0.84 million per year. Financial criteria were not the driving factors in choosing to adopt a fully integrated PACS solution. Given the current workload of the imaging department, the latest digital imaging technologies cannot be incorporated without moving to a totally digital environment. Clinical quality has been increased due to the availability of tools to review complex multislice CT and MRI studies; the ability to compare a several studies of the same patient across different modalities and timeframes; and finally by enabling detailed simultaneous clinical discussions between the referring physicians and radiology teams.
CONCLUSION
While we are confident in the general conclusions that a PACS system can simplify and speed up an IT integrated hospital workflow, any quantitative aspects could vary due to local context, duration of the period of observation, or by the number of wards analyzed. In particular, the patient stay can vary due to different internal decisions. However, in our case, we ensured that no significant changes in patient treatment occurred during the study period. For these types of evaluation, strong cooperation with the referring physicians is necessary.
A well-planned, fully integrated digital Radiology Department can simplify workflow throughout the hospital. PACS technology, empowered with speech recognition systems and web distribution tools, can deliver significant benefits to a health care institution. Staff and interdepartmental cooperation is key to this process. Driving workflow optimization and detailed continuous performance monitoring are a must, as well.
Acknowledgements
Eastman Kodak Health Group has supported this project. We would like to thank Eugenio Cepollina, Reggio Emilia’s Kodak Project Manager from the Kodak Technology and Innovation Center of Genoa, Italy.
References
- 1.Ondo K. PACS direct experiences: Implementation, selection, benefits realized. J Digit Imaging. 2004;17(4):249–252. doi: 10.1007/s10278-004-1017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pare G, Lepanto L, Sicotte C. Toward a multidimensional assessment of picture archiving and communication system success. Int J Technol Assess Health Care. 2005;21(4):471–479. doi: 10.1017/S0266462305050658. [DOI] [PubMed] [Google Scholar]
- 3.Reiner BI, Siegel EL, Flagle C, Hooper DFJ, Cox RE, Scanlon M. Effect of filmless imaging on the utilization of radiologic services. Radiology. 2000;215:163–167. doi: 10.1148/radiology.215.1.r00ap41163. [DOI] [PubMed] [Google Scholar]
- 4.Levine BA, Mun SK, Benson HR, Horii SC. Assessment of the integration of HIS/RIS with PACS. J Digit Imaging. 2003;16(1):133–140. doi: 10.1007/s10278-002-6022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dumery B. Digital image archiving: Challenges and choice. Radiol Manage. 2002;25:30–38. [PubMed] [Google Scholar]
- 6.Huang HK. PACS and Imaging Informatics: Basic Principles and Applications. New York: Wiley & Sons; 2004. [Google Scholar]
- 7.Inamura K, Umeda T, Harauchi H, Kondoh H, Hasegawa T, Kozuka T, Takeda H, Inoue M. Time and flow study results before and after installation of a hospital information system and radiology information system and before clinical use of a picture archiving and communication system. J Digit Imaging. 1997;10:1–9. doi: 10.1007/BF03168543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reiner BI, Siegel EL, Carrino JA, Goldburgh MM. SCAR radiologic technologist survey: Analysis of the impact of digital technologies on productivity. J Digit Imaging. 2002;15:132–140. doi: 10.1007/s10278-002-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sacco P, Mazzei M, Pozzebon E, Stefani P. PACS Implementation in a university hospital in Tuscany. J Digit Imaging. 2002;15(suppl 1):250–251. doi: 10.1007/s10278-002-5052-7. [DOI] [PubMed] [Google Scholar]
- 10.Lepanto L, Pare´ G, Aubry D, Robillard P, Lesage J. Impact of PACS on dictation turnaround time and productivity. J Digit Imaging. 2006;19:92–97. doi: 10.1007/s10278-005-9245-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattern CW, King BF, Hangiandreou NJ. Electronic imaging impact on image and report turnaround times. J Digit Imaging. 1999;12:155–159. doi: 10.1007/BF03168787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langer SG. Impact of speech recognition on radiologist productivity. J Digit Imaging. 2002;15:203–209. doi: 10.1007/s10278-002-0014-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reiner BI, Siegel EL, Hooper FJ, Siddiqui KM, Musk A, Walker L, Chacko A. Multi-institutional analysis of computed and direct radiography part I. Technologist productivity. Radiology. 2005;236:413–419. doi: 10.1148/radiol.2362040671. [DOI] [PubMed] [Google Scholar]
- 14.Siegel E, Reiner B. Work flow redesign: The key to success when using PACS. AJR Am J Roentgenol. 2002;178:563–566. doi: 10.2214/ajr.178.3.1780563. [DOI] [PubMed] [Google Scholar]
- 15.Nelson EK, Jorge D, Brent L. Predicting Clinical Image Delivery Time by Monitoring PACS Queue Behavior. J Digit Imaging. 2006;19(suppl 1):35–43. doi: 10.1007/s10278-006-0262-z. [DOI] [PMC free article] [PubMed] [Google Scholar]