Abstract
Maladaptive behaviors among 65 people with Prader-Willi syndrome were assessed using the Reiss Screen for maladaptive behaviors. Young adults in their twenties were more likely to display aggressive behavior than adolescents and older adults. Differences in maladaptive behaviors between the typical deletion and uniparental disomy (UPD) subtypes were evaluated. The typical deletion subtype had higher self-injury and stealing scores than the UPD subtype. Subject characteristics were differentially related to maladaptive behavior among the typical deletion and UPD subtypes. Differences in maladaptive behavior were also examined between the typical deletion type I and type II subtypes. The type I deletion subtype had greater physical depression scores than the type II deletion subtype. The Reiss Screen cut-off scores were used to determine whether differences occurred between the subtypes at a clinically significant level. These findings offer insight into the health care needs of people with PWS.
Keywords: behavioral phenotype, chromosome 15q, uniparental disomy, psychopathology
INTRODUCTION
Prader-Willi syndrome (PWS) is a developmental disorder that occurs in approximately 1 in 20,000 live births [Whittington et al., 2001]. It is caused by a chromosomal abnormality consisting of a typical paternal deletion of the proximal long arm of chromosome 15q (15q11-q13) in approximately 70% of the cases and maternal uniparental disomy (UPD) of chromosome 15 in approximately 25% of the cases. Additionally, abnormalities in genetic imprinting affecting paternal gene expression account for less than 5% of PWS cases [Butler and Thompson, 2000; Nicholls and Knepper, 2001]. There is a reported 1:1 ratio of males to females within the typical deletion and UPD genetic subtypes [Gillessen-Kaesbach et al., 1995; Mitchell et al., 1996]; however, additional research suggests that there may be more males than females with the UPD subtype [Mitchell et al., 1996]. People with PWS have high rates of maladaptive behaviors compared to people with cognitive impairments due to other etiologies [Clarke et al., 1996; Dykens and Kasari, 1997; Holland et al., 2003]. Problematic behaviors commonly found among people with PWS include temper tantrums, aggressive behavior, stubbornness, skin picking, compulsivity, overeating, and hoarding [Dykens and Cassidy, 1995; Dykens and Kasari, 1997].
People with typical deletion or UPD genetic subtypes may not exhibit maladaptive behaviors with equivalent frequencies or severities. Previous studies suggest that the UPD subtype has milder maladaptive behaviors than the typical deletion subtype. For example those with the typical deletion subtype have greater rates of skin picking [Dykens et al., 1999; Symons et al., 1999], symptom-related distress on the Yale-Brown Obsessive Compulsive Scale [Dykens et al., 1999], mood-swings, stealing food [Webb et al., 2002] withdrawal, sulking, nail biting, hoarding, and overeating [Dykens et al., 1999] than people with the UPD subtype. The few areas for which those with a UPD are at greater risk include autistic characteristics, particularly in childhood, psychosis, predominantly in young adulthood, and sleep disorders [Boer et al., 2002; Webb et al., 2002]. All of these findings are based on inventories structured for, and normed on, typically developing children or unvalidated checklists of behaviors. The legitimacy of these differences would be greatly supported through an assessment designed and normed on individuals with mental retardation.
Subject Characteristic Risk Factors
Several subject characteristics correlate with maladaptive behaviors and may serve to identify at risk subpopulations of people with PWS. There is a non-linear relationship between age and maladaptive behaviors, with an increase in maladaptive behaviors such as skin picking, compulsivity, and temper tantrums as children get older [Dykens and Kasari, 1997; Dimitropoulos et al., 2001; Dykens, 2004], with young adults showing the greatest incidence of problems. However there are fewer maladaptive behaviors among older adults than in young adults [Dykens, 2004]. Body mass index (BMI) is negatively correlated with hoarding, psychosis, depression, skin picking, and dependent personality disorder, such that people with PWS with greater BMIs demonstrate these problems less often [Dykens and Cassidy, 1995; Dykens, 2004]. There is less clarity on the association between gender and maladaptive behaviors. Some researchers report that males display greater externalizing behaviors, aggression, and depression [Dykens and Cassidy, 1995; Dykens, 2004], and that females demonstrate increased skin picking. However, other studies have not demonstrated these gender differences [Dykens and Kasari, 1997; Einfeld et al., 1999; Symons et al., 1999]. The reported behavioral and emotional differences between the UPD and typical deletion subtypes suggest that subject characteristics may be differentially associated with maladaptive behaviors among these genetic subtypes.
Searching for correlates of maladaptive behavior separately among the genetic subtypes may provide a more fine-grained identification of characteristics related to problematic behavior and help explain the lack of consistency in previous research.
Deletion Type I and Type II
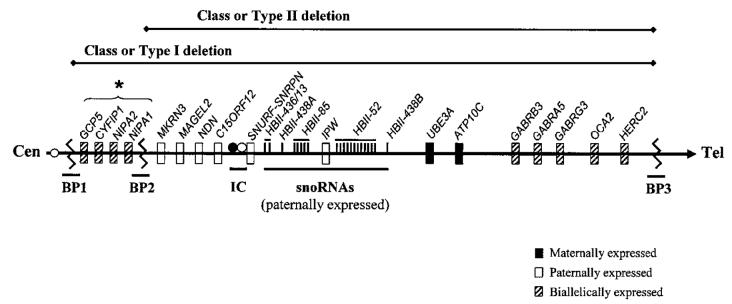
Recently, an additional distinction among the genetic subtypes of PWS has emerged through advances in molecular genetics. The typical deletion subtype seen in PWS involving the 15q11-q13 region can be further grouped into two separate classes of deletions. The proximal breakpoint of the typical 15q11-q13 deletion may occur at two different sites within one of the two large duplicons centromeric to locus MKRN3, allowing for the identification of two deletion subtypes [Nicholls and Knepper, 2001]. People with the class or type I deletion have a breakpoint that is proximal to the D15S541/S1035 loci, whereas those with the class or type II deletion have a breakpoint between loci D15S541/S1035 and D15S543 [Ungaro et al., 2001]. Approximately, 40% of the typical deletions are classified as type I while about 60% are type II [Christian et al., 1995; Butler et al., 2004]. As a result, people with the larger type I deletion have approximately 500 kb less genetic material than people with the smaller type II deletion (Fig. 1). The ratio of males to females with a type I and type II deletion is unknown; however, Butler et al. [2004] found a 1:1 ratio among both deletion types in their study subjects. The greater loss of genetic material among type I deletions may translate into important phenotypic disparities among people with deletion type I or type II. In the only study of its kind, Butler et al. [2004] found that people with type I deletion (n = 12) had more compulsive behavior, more impairment in visual perception, poorer academic performance, and poorer daily living skills than people with type II deletion (n = 14).
Fig. 1.
Human chromosome 15q11-q13 region. Deletion type I spans from breakpoint 1 (BP1) to breakpoint 3 (BP3) whereas deletion type II spans from breakpoint 2 (BP2) to breakpoint 3. IC represents the location of the imprinting center. *Ordered according to the UCSC Genome Browser, May 2004 Assembly http://genome.ucsc.edu/.
Present Study
Using a scale developed for and normed on adults with mental retardation, the present study attempts to further define significant differences in maladaptive behaviors among the typical deletion and UPD subtypes, and to determine if subject characteristics (gender, age, IQ, and BMI) are significant correlates of maladaptive behaviors within the deletion and UPD subtypes. Finally, we assess whether people with a type I deletion have more severe maladaptive behaviors than with a type II deletion.
MATERIALS AND METHODS
Population Assessed
Sixty-five individuals with PWS aged 12-45 year (M = 23.81, SD = 8.87) participated in the study. Forty-seven subjects were evaluated between 1995-1999 at the John F. Kennedy Center, Vanderbilt University, Nashville, Tennessee and 18 subjects with PWS were evaluated between 2000-2003 at the University of Kansas Medical Center (KUMC). All individuals agreed to informed consent approved by institutional review boards. Full Scale IQs ranging from 45-83 (M = 63.02, SD = 8.87) and BMI ranging from 19.46 to 58.28 (M = 34.64, SD had = 9.05). Forty individuals (16 male, 24 female) the typical 15q11-q13 deletion, 23 individuals (11 male, 12 female) had maternal UPD of chromosome 15, and 2 individuals (2 male) had an imprinting defect. A chi-square test indicated that the percentage of participants with the typical deletion (62%), UPD (35%), and imprinting defects (3%) did not significantly differ from the expected percentages of these genetic subtypes among people with PWS [Butler and Thompson, 2000; Nicholls and Knepper, 2001]. A chi-square indicated that the ratio of males to females in both the deletion and UPD subtype did not significantly differ from the 1:1 ratio found in previous research [Gillessen-Kaesbach et al., 1995; Mitchell et al., 1996]. Within the typical deletion subtype, 14 participants (6 male, 8 female) had type I deletion and 20 (7 male, 13 female) had type II deletion. The ratio of people classified with a type I to type II deletion is consistent with past findings [Christian et al., 1995; Butler et al., 2004]. A chisquare indicated that the ratio of males to females for both type I and type II deletion did not differ significantly from the 1:1 ratio found in previous research [Butler et al., 2004].
Sixty participants were Caucasian, two were Hispanic and three were African-American. Typical deletion and UPD individuals did not differ on BMI, age, or Full Scale IQ; however, UPD individuals had significantly higher verbal IQs. There was no difference in use of psychiatric medications or insulin between the typical deletion and UPD subtypes. Six participants were currently being treated with growth hormone and three had received such treatment in the past. Nineteen participants lived at a PWS group home, 5 lived at a group home not specific to PWS, and 41 lived independently, semi-independently, or with their family. There was not a significant difference in place of residence or income level reported by parents/guardians between the typical deletion and UPD subtypes or between the type I and type II deletion subtypes.
Genetic Classification
Genetic subtypes were confirmed through the use of high-resolution chromosome analysis, fluorescent in situ hybridization, and DNA microsatellite analysis to confirm the typical deletion or UPD genetic subtype status [Muralidhar and Butler, 1998; Butler et al., 2002]. Microsatellite markers proximal to D15S541/S1035 loci and between D15S541/S1035 and D15S543 were used to identify type I and type II deletions. The presence of a second breakpoint, between D15S56 and D15S165, on 15q11-q13 was confirmed in all deletion participants through molecular genetic testing. Classifications of type I and type II deletions were based on microsatellite analysis of parental DNA isolated from peripheral blood. Confirmation of classifications was achieved through quantitative PCR using established protocols [Ungaro et al., 2001; Butler et al., 2002]. Type I deletion classifications were made based on the absence of the paternal D15S541/S1035 loci and classification of type II deletions were based on the presence of the D15S541/S1035 loci.
Behavioral Measures
The Reiss Screen for maladaptive behavior [Reiss, 1988] is a 38-item inventory in which informants rate the degree to which each symptom is “No Problem,” “Problem,” or “Major Problem.” The Reiss Screen was chosen to assess psychopathology because this scale was designed for and normed on adults with mental retardation and assesses a wide range of maladaptive behaviors. The Reiss Screen results in eight scale scores (aggressive behavior, autism, psychosis, paranoia, avoidant, depression (behavioral), depression (physical), and dependent personality disorder) each including five items, six maladaptive behavior single item scores (drug/alcohol abuse, overactive, self-injury, sexual problem, suicidal tendencies, stealing), and a 26-item total score indicative of severity of mental health problems. Cut-off scores indicative of a problem likely to be in need of mental health services were used to determine clinically significant psychopathology [Reiss, 1988]. The cutoffs for seven of the eight scale scores were located at two standard deviations above the norms for individuals with mental retardation rated as having no comorbid diagnoses. The cutoff for the Autism scale score was located slightly higher than the mean obtained from a group of individuals with mental retardation diagnosed with autism. The cutoffs for the maladaptive behavior items were based on a priori considerations that an item rated as major problem constituted a problem needing professional evaluation. The cutoff for the 26-item total score was established as the mid-point between the average score for a group of individuals with mental retardation with no comorbid diagnoses and groups with a comorbid diagnosis. The Reiss Screen has been shown to have adequate reliability, internal consistency, and concurrent validity [Reiss, 1988; Walsh and Shenouda, 1999].
When possible, two parents or guardians completed the Reiss Screen and the average score from these two ratings was used. When only one parent or guardian completed the Reiss Screen, this score was used. IQ was assessed through Wechsler scales (WAIS-R or WISC-III; Wechsler, 1981, 1991) and BMI was calculated [weight in kilos/(height in meters)2] for all participants. Age, gender, and ethnicity were reported by parents or guardians of participants.
RESULTS
Deletion Versus UPD
Possible differences in maladaptive behavior between the typical deletion and UPD subtypes were assessed using independent-samples t-tests and Mann-Whitney U-tests. Independent-samples t-tests indicated no significant difference between the typical deletion and UPD subtypes on the eight Reiss scale scores or the 26-item total Reiss score. Mann-Whitney U-tests indicated that the deletion subtype had significantly higher Reiss self-injury scores (U= 294.00, P = 0.011 [one-tailed]) than the UPD subtype. The typical deletion subtype also had significantly higher Reiss stealing scores (U = 311.50, P = 0.033 [one-tailed]) than the UPD subtype. To determine whether = differences existed in clinically significant psychological problems, a chi-square was used to compare the number of deletion and UPD participants at or above the clinically significant cut-off scores (Tables I and II). Results indicated that there were significantly more people with the typical deletion subtype with clinically significant self-injury than with the UPD subtype, χ2 (1, 93) 4.48, P = 0.044 (one-tailed). In addition, there were significantly more people with the typical deletion subtype with clinically significant stealing than with the UPD subtype, χ2 (1, 66) = 7.78, P = 0.005 (one-tailed).
TABLE I.
Percentage of Typical Deletion (N = 40) and UPD (N = 23) Participants Receiving Each Raw Score on the Reiss Screen Scale Scores
| Aggressive behavior |
Autism |
Psychosis |
Paranoia |
Depression (behavioral Signs) |
Depression (physical signs) |
Dependent personality disorder |
Avoidant disorder |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | ||
| 10 | 4.3 | ||||||||||||||||
| 9 | 2.5 | 2.5 | |||||||||||||||
| 8 | 5.0 | 4.3 | |||||||||||||||
| 7 | 7.5 | 2.5 | |||||||||||||||
| 6 | 15.0 | 8.7 | 5.0 | 2.5 | 5.0 | 2.5 | 8.7 | 5.0 | 8.7 | 2.5 | |||||||
| Raw score | 5 | 17.5 | 8.7 | 4.3 | 2.5 | 4.3 | 4.3 | 4.3 | 2.5 | 4.3 | 2.5 | 13.0 | |||||
| 4 | 2.5 | 17.4 | 4.3 | 2.5 | 15.0 | 13.0 | 2.5 | 4.3 | 20.0 | 8.7 | 2.5 | 8.7 | 5.0 | 8.7 | |||
| 3 | 5.0 | 8.7 | 7.5 | 4.3 | 12.5 | 13.0 | 17.5 | 13.0 | 15.0 | 17.4 | 35.0 | 30.4 | 17.5 | 17.4 | 7.5 | 8.7 | |
| 2 | 12.5 | 13.0 | 12.5 | 17.4 | 20.0 | 30.4 | 17.5 | 17.4 | 20.0 | 26.1 | 27.5 | 34.8 | 17.5 | 13.0 | 22.5 | 21.7 | |
| 2 | 2.5 | 2.5 | 2.5 | ||||||||||||||
| 1 | 15.0 | 21.7 | 22.5 | 34.8 | 15.0 | 17.4 | 17.5 | 39.1 | 32.5 | 21.7 | 10.0 | 13.0 | 25.0 | 30.4 | 25.0 | 21.7 | |
| 0 | 17.5 | 13.0 | 57.5 | 39.1 | 42.5 | 34.8 | 22.5 | 13.0 | 22.5 | 26.1 | 2.5 | 30.0 | 17.4 | 35.0 | 26.1 | ||
Shaded areas represent raw scores at or above the clinically significant cut-off score. The 1.5 raw score represents the average score when two raters were used.
TABLE II.
Percentage of Typical Deletion (N = 40) and UPD (N = 23) Participants Receiving Each Raw Score on the Reiss Screen Maladaptive Behavior Items
| Drug/Alcohol abuse |
Overactive |
Self-Injury |
Sexual problem |
Stealing |
Suicidal tendencies |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | Del. | UPD | ||
| 2 | 10.0 | 25.0 | 3.0 | ||||||||||
| Raw score | 1.5 | 3.0 | 3.0 | ||||||||||
| 1 | 2.5 | 3.0 | 14.0 | 30.0 | 14.0 | 3.0 | 10.0 | 23.0 | 33.0 | 3.0 | 5.0 | ||
| 0 | 97.5 | 100 | 0.98 | 86.0 | 56.0 | 86.0 | 98.0 | 90.0 | 50.0 | 67.0 | 95.0 | 95.0 | |
Shaded areas represent raw scores at or above the clinically significant cut-off score.
Subject Characteristics and Maladaptive Behaviors for Typical Deletion and UPD
To determine whether young adolescents with PWS had higher rates of maladaptive behaviors than adolescents and older adults, three age groups (12-19, 20-29, and 30-45 years old) were formed. A one-way analysis of variance indicated a significant difference among the three age groups in aggressive behavior, F (2, 45) = 4.38, P = 0.018. Student-Newman Keuls post-hocs revealed that 20-29 year olds (M = 4.60, SD = 2.87) had significantly higher aggressive behavior scores than 12-19 year olds (M = 2.60, SD = 2.53) and 30-45 years old (M = 1.92, SD = 1.98). Bonferroni-corrected independent samples t-tests indicated no significant differences between the age groups for the Reiss maladaptive behavior items. To determine whether 20-29 years old had higher rates of maladaptive behaviors when the deletion and UPD subtypes were examined separately, one-way ANOVAs and Bonferroni-corrected independent samples t-tests were conducted. Analyses indicated no significant differences among the three age groups on any of the Reiss scores for either the typical deletion or UPD subtype.
The relationship between gender, BMI, and full scale IQ and maladaptive behaviors for the deletion and UPD subtypes were assessed through correlations. Table III shows the correlations between subject characteristics and the Reiss Screen. In the typical deletion subtype, point biserial correlations indicated that gender was significantly related to aggression (r= -0.39, P = 0.014), Reiss depression (physical signs) (r = -0.34, P = 0.030), dependent PD (r= -0.49, P 0.001), and 26-item total scores (r = -0.35, P = 0.025), suggesting that males are at greater risk for these problems. Point Biserial and Kendall’s Tau C correlations indicated that gender was not significantly related to any of the Reiss scale scores or maladaptive behavior items in the UPD subtype. Pearson correlations indicated that BMI was significantly negatively related to Reiss aggressive behavior (r = -0.30, P = 0.042) and Reiss Paranoia (r = -0.37, P = 0.018) and significantly positively related to Reiss depression (physical signs) (r = -0.42, P = 0.041) among the deletion subtype. BMI was significantly negatively related to aggressive behavior (r = -0.68, P = 0.001) in the UPD subtype. Kendall Tau C correlations indicated that IQ was positively related to Reiss stealing (r = 0.45, P = 0.025) and Reiss selfinjury (r = 0.53, P = 0.020) in the UPD subtype but was not significantly related to the maladaptive behavior items in the deletion subtype.
TABLE III.
Correlations Among Subject Characteristics and Reiss Screen Scores
| Subject characteristics |
||||||
|---|---|---|---|---|---|---|
| Typical deletion |
UPD |
|||||
| Reiss Screen score | Gender (N = 40) | IQ (N = 39) | BMI (N = 35) | Gender (N = 23) | IQ (N = 23) | BMI (N = 22) |
| Aggressive behavior | -0.39a | 0.16 | -0.30a | 0.10 | -0.13 | -0.68b |
| Autism | -0.26 | 0.09 | -0.08 | -0.33 | 0.15 | -0.25 |
| Psychosis | -0.14 | 0.03 | -0.03 | -0.18 | 0.23 | -0.26 |
| Paranoia | -0.23 | 0.15 | -0.37a | -0.09 | 0.24 | -0.30 |
| Depression (behavioral signs) | -0.18 | 0.11 | -0.26 | -0.05 | 0.06 | -0.06 |
| Depression (physical signs) | -0.34a | 0.08 | 0.42a | -0.06 | 0.21 | 0.22 |
| Dependent personality disorder | -0.49b | -0.17 | -0.13 | -0.05 | 0.20 | -0.35 |
| Avoidant | -0.26 | -0.05 | -0.09 | -0.05 | 0.12 | -0.14 |
| Drug/Alcohol abuse | ||||||
| Overactive | -0.24 | 0.04 | -0.15 | |||
| Self-injury | -0.07 | -0.07 | -0.11 | 0.11 | 0.53a | 0.27 |
| Sexual problems | -0.06 | -0.11 | -0.06 | 0.02 | 0.06 | -0.12 |
| Stealing | 0.01 | 0.10 | -0.07 | -0.06 | 0.45a | 0.33 |
| Suicidal tendencies | 0.08 | 0.17 | -0.19 | 0.09 | -0.13 | -0.05 |
| 26-item total | -0.35a | 0.16 | -0.31 | 0.17 | 0.12 | -0.41 |
Blank values indicate correlations unavailable due to lack of variation in item response.
Significant at 0.05 alpha level.
Significant at 0.01 alpha level.
Deletion Type I Versus Deletion Type II
Possible differences between the deletion type I and II in maladaptive behavior were assessed using independent-samples t-tests and Mann-Whitney U-tests. Independent samples t-tests revealed that people with type I had significantly higher Reiss depression (physical signs) scores than the deletion type II, t (32) = 1.95, P = 0.030 (one-tailed). There were no other significant differences between the two deletion types in Reiss scale scores or the 26-item total score. Mann-Whitney U-tests indicated no significant differences between the two-deletion types in the Reiss maladaptive behavior items. To determine whether differences existed in clinically significant maladaptive behavior, a chi-square was used to compare the number of participants with type I and type II deletions at or above the clinically significant cut-off scores (Fig. 2). Analyses indicated no significant differences in clinically significant problems between the two deletion types.
Fig. 2.
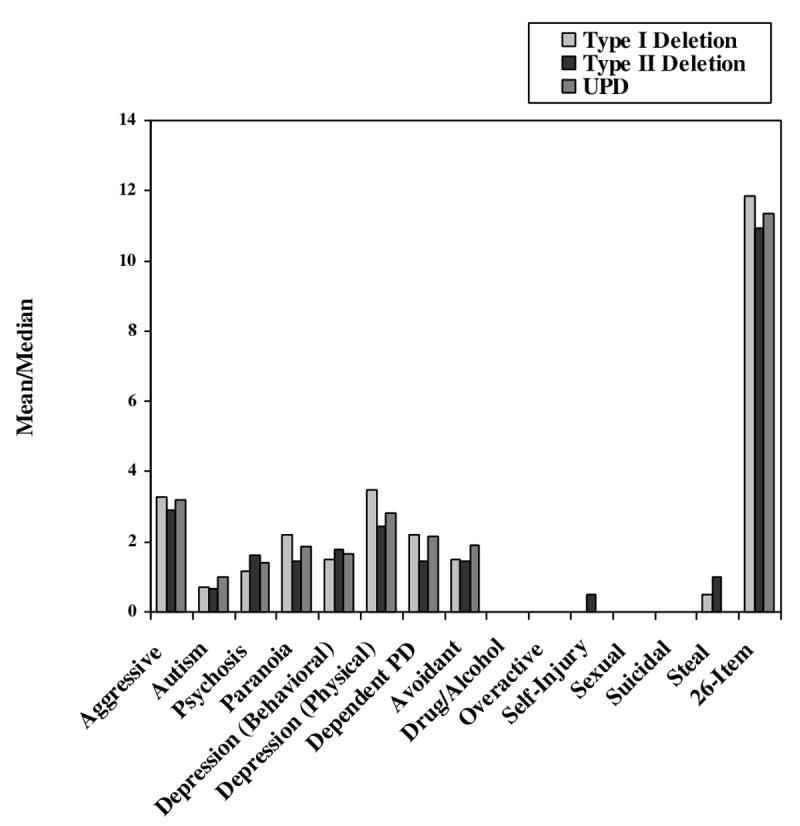
Mean Reiss scale scores and 26-item total score for deletion type I and deletion type II, and median Reiss maladaptive behavior items for deletion type I and deletion type II. Note: Means are used for the eight scale scores and 26-item total score and medians are used for the six maladaptive behavior items.
DISCUSSION
A scale developed for and normed on adults with mental retardation was used to examine maladaptive behavior among people with PWS. For the most part the study confirms the characteristics described by previous observational studies and those that used instruments normed on typically developing children. Maladaptive behaviors are exceedingly common in those with PWS. Furthermore, the frequencies of those maladaptive behaviors vary among causal subtype of PWS. Both the typical deletion and UPD subtype were found to exhibit similar types of problematic behaviors, with the greatest problems for both subtypes occurring in aggressive behavior and physical signs of depression (e.g., low energy, sleep difficulties, and deteriorated hygiene/unkempt appearance). In addition to identifying maladaptive behaviors among people with PWS, the present study addresses the need for mental health services to deal with these behaviors. The present study also demonstrates that the differences between the typical deletion and UPD subtypes are not only statistically significant, but reflect meaningful differences in the percentage of people with severe difficulties requiring professional intervention. The typical deletion subtype had significantly greater self-injury and stealing than the UPD subtype and these differences remained at the clinically significant level, suggesting that the deletion subtype has greater need of mental health services for these problems. It remains unknown whether stealing relates to food or non-food items. However, previous research suggests this may primarily relate to food items [Webb et al., 2002].
Differences in the relationship between subject characteristics and maladaptive behavior were found among the genetic subtypes of PWS. Within the combined PWS group, young adults in their twenties were at greater risk for aggressive behavior than adolescents and older adults. This finding is consistent with recent work suggesting that maladaptive behaviors are highest among young adults with PWS [Dykens, 2004]. The lack of association between age and maladaptive behaviors when the typical deletion and UPD subtypes were analyzed separately may be due to limited power to detect differences.
Gender was significantly related to maladaptive behavior for the typical deletion subtype but not the UPD subtype. Specifically males with the typical deletion subtype are at greater risk for aggressive behavior, depression (physical signs), dependent personality disorder, and overall severity of psychopathology than females with the typical deletion subtype. The apparent inconsistencies between studies reporting heightened rates of maladaptive behaviors among males [Dykens and Cassidy, 1996; Dykens, 2004] and studies reporting no significant gender differences [Dykens and Kasari, 1997; Einfeld et al., 1999; Symons et al., 1999] may be resolved when genetic subtypes are taken into account. The present study suggests gender may only be a significant risk factor for problematic behaviors among the typical deletion subtype.
In line with past research, BMI was significantly negatively related to aggressive behavior in both the typical deletion and UPD subtypes, and significantly negatively related to symptoms of paranoia in the typical deletion subtype. This suggests that thinner individuals are at an increased risk for these problematic behaviors. Hence, obesity may be a factor that influences psychopathology. However, further research is needed to determine whether weight management strategies used by obese individuals, including those with PWS, may evoke aggression and paranoia. BMI was positively related to physical signs of depression within the typical deletion subtype, suggesting that obesity is associated with body stress, eating problems, low energy, and regressive behavior. This association may be reflective of the overlap in symptoms of obesity and physical signs of depression, and not signify a true relationship between BMI and depression. In support of this, there was a trend for BMI to be negatively related to depression (behavioral signs) among the typical deletion subtype.
Unexpectedly, IQ was significantly positively associated with stealing and self-injury among the UPD subtype. A possible reason for the discrepancy between the current finding and past reports of a lack of relationship between intelligence and maladaptive behaviors may be that past methods of combining the PWS genetic subtypes may have obscured this relationship. Further research is necessary to explain these findings.
Individuals with a type I deletion had significantly greater Reiss depression (physical signs) scores than individuals with a type II deletion. However, this difference did not remain significant when examining rates of clinically significant depression (physical signs). This suggests that the additional loss of 500 kb of genetic material incurred by the deletion type I subtype influences the prevalence of physical symptoms of depression but may not affect rates of individuals in need of clinical services. This finding parallels work by Butler et al. [2004] that the type I subtype have more severe pathology and impaired functioning than the type II subtype.
The identification of the interrelationship among etiological subtypes of PWS, subject characteristics, and psychopathology is not meant for diagnostic purposes. Diagnosis of PWS etiologic subtype can only be determined by genetic methods. Differences in psychopathology between the genetic subtypes of PWS have important implications for understanding the genetic basis of the subtypes of PWS and for mental health care of people with PWS. The present study provides insight into the overall need for mental health care among the genetic subtypes of PWS. The findings suggest that there is a great need for mental health services among people with PWS, and the percentages of people requiring professional care are particularly high among those with a typical deletion. The interrelationship between the etiologic subtypes of PWS and subject characteristics may help identify the subpopulation of people with PWS most likely to require services.
REFERENCES
- Boer H, Holland AJ, Whittington JE, Butler JV, Webb T, Clarke DJ. Is psychotic illness inevitable in people with Prader-Willi syndrome due to chromosome 15 maternal uniparental disomy? Lancet. 2002;359:135–136. doi: 10.1016/S0140-6736(02)07340-3. [DOI] [PubMed] [Google Scholar]
- Butler MG, Thompson T. Prader-Willi syndrome: Clinical and genetic findings. Endocrinologist. 2000;10:3S–16S. doi: 10.1097/00019616-200010041-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Bittel D, Talebizadeh Z. Prader-Willi syndrome and a deletion/duplication within the 15q11-q13 region. J Med Genet. 2002;107:69–70. doi: 10.1136/jmg.39.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Bittel DC, Kibiryeva N, Talebizadeh Z, Thompson T. Behavioral differences among subjects with Prader-Willi syndrome and type I or type II deletions and maternal disomy. Pediatrics. 2004;113:565–574. doi: 10.1542/peds.113.3.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian SL, Robinson WP, Huang B, Mutirangura A, Line MR, Nakao M, Surti U, Chakravarti A, Ledbetter DH. Molecular characterization of two proximal deletion breakpoint regions in both Prader-Willi and Angelman syndrome patients. Am J Hum Genet. 1995;57:40–48. [PMC free article] [PubMed] [Google Scholar]
- Clarke DJ, Boer H, Chung MC, Sturmey P, Webb J. Maladaptive behaviour in Prader-Willi syndrome in adult life. J Intellect Disabil Res. 1996;40:159–165. doi: 10.1046/j.1365-2788.1996.743743.x. [DOI] [PubMed] [Google Scholar]
- Dimitropoulos A, Feurer ID, Butler MG, Thompson T. Emergence of compulsive behavior and tantrums in children wth Prader-Willi syndrome. Am J Ment Retard. 2001;106:39–51. doi: 10.1352/0895-8017(2001)106<0039:EOCBAT>2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykens EM. Maladaptive and compulsive behavior in Prader-Willi syndrome: New insights from older adults. Am J Ment Retard. 2004;109:142–153. doi: 10.1352/0895-8017(2004)109<142:MACBIP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Cassidy SB. Correlated of maladaptive behavior in children and adults with Prader-Willi syndrome. Am J Med Genet. 1995;60:546–549. doi: 10.1002/ajmg.1320600612. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Cassidy SB. Prader-Willi syndrome: Genetic behavioural, and treatment issues. Child Adolesc Psychiatr Clin N Am. 1996;5:913–927. [Google Scholar]
- Dykens EM, Kasari C. Maladaptive behaviors in children with Prader-Willi syndrome, Down syndrome, and nonspecific mental retardation. Am J Ment Retard. 1997;102:228–237. doi: 10.1352/0895-8017(1997)102<0228:MBICWP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Cassidy SB, King BH. Maladaptive behavior differences in Prader-Willi syndrome due to paternal deletion versus maternal uniparental disomy. Am J Ment Retard. 1999;104:67–77. doi: 10.1352/0895-8017(1999)104<0067:MBDIPS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Smith A, Durvasula S, Florio T, Tonge B. Behavior and emotional disturbance in Prader-Willi syndrome. Am J Med Genet. 1999;82:123–127. doi: 10.1002/(sici)1096-8628(19990115)82:2<123::aid-ajmg4>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Gillessen-Kaesbach G, Robinson W, Lohmann D, Kaya-Westerloh S, Passarge E, Horsthemke B. Genotype-phenotype correlations in a series of 167 deletion and non-deletion patients with Prader-Willi syndrome. Hum Genet. 1995;96:638–643. doi: 10.1007/BF00210291. [DOI] [PubMed] [Google Scholar]
- Holland AJ, Whittington JE, Butler J, Webb T, Boer H, Clarke D. Behavioural phenotypes associated with specific genetic disorders: Evidence from a population-based study of people with Prader-Willi syndrome. Psychol Med. 2003;33:141–153. doi: 10.1017/s0033291702006736. [DOI] [PubMed] [Google Scholar]
- Mitchell J, Schinzel A, Langlois S, Gillessen-Kaesbach G, Schuffenhauer S, Michaelis R, Abeliovich D, Lerer I, Christian S, Guitart M, McFadden DE, Robinson WP. Comparison of phenotype in uniparental disomy and deletion Prader-Willi syndrome. Am J Med Genet. 1996;65:133–136. doi: 10.1002/(SICI)1096-8628(19961016)65:2<133::AID-AJMG10>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Muralidhar B, Butler MG. Methylation PCR analysis of Prader-Willi syndrome, Angelman syndrome, and control subjects. Am J Med Genet. 1998;80:263–265. [PMC free article] [PubMed] [Google Scholar]
- Nicholls RD, Knepper JL. Genome organization, function and imprinting in Prader-Willi and Angelman syndromes. Annu Rev Genom Hum Genet. 2001;2:321–325. doi: 10.1146/annurev.genom.2.1.153. [DOI] [PubMed] [Google Scholar]
- Reiss S. Reiss screen for maladaptive behaviors: Test manual. 2nd edn. IDS Publishing Corporation; Worthington, OH: 1988. [Google Scholar]
- Symons FJ, Butler MG, Sanders MD, Feurer ID, Thompson T. Selfinjurious behavior and Prader-Willi syndrome: Behavioral forms and body locations. Am J Ment Retard. 1999;104:260–269. doi: 10.1352/0895-8017(1999)104<0260:SBAPSB>2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungaro P, Christian SL, Fantes JA, Mutirangura A, Black S, Reynolds J, Malcolm S, Dobyns WB, Ledbetter DH. Molecular characterization of four cases of intrachromosomal triplication of chromosome 15q11-q14. J Med Genet. 2001;38:26–34. doi: 10.1136/jmg.38.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh KK, Shenouda N. Correlations among the Reiss Screen, the adaptive behavior scale Part II, and the aberrant behavior checklist. Am J Men Retard. 1999;104:236–240. doi: 10.1352/0895-8017(1999)104<0236:CATRST>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Webb T, Whittington J, Clarke D, Boer H, Butler J, Holland AA. A study of the influence of different genotypes on the physical and behavioral phenotypes of children and adults ascertained clinically as having PWS. Clin Genet. 2002;62:273–281. doi: 10.1034/j.1399-0004.2002.620404.x. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler adult intelligence scale-revised. The Psychological Corporation; San Antonio, TX: 1981. p. 349. [Google Scholar]
- Wechsler D. Wechsler adult intelligence scale for children, 3rd edn. The Psychological Corporation; San Antonio, TX: 1991. p. 293. [Google Scholar]
- Whittington JE, Holland AJ, Webb T, Butler JV, Clarke DJ, Boer H. Population prevalence and estimated birth incidence and mortality rate for people with Prader-Willi syndrome in one UK health region. J Med Genet. 2001;38:792–798. doi: 10.1136/jmg.38.11.792. [DOI] [PMC free article] [PubMed] [Google Scholar]