Abstract
Rationale: Although caregiver burden is well described in chronic illness, few studies have examined burden among caregivers of survivors of critical illness. In existing studies, it is unclear whether the observed burden is a consequence of critical illness or of preexisting patient illness.
Objectives: To describe 1-yr longitudinal outcomes for caregivers of patients who survived critical illness, and to compare depression risk between caregivers of patients with and without pre–intensive care unit (ICU) functional dependency.
Methods: Prospective, parallel, cohort study of survivors of prolonged (greater than 48 h) mechanical ventilation and their informal caregivers. Caregivers were divided into two cohorts on the basis of whether patients were functionally independent (n = 99, 59%), or dependent (n = 70, 41%) before admission. Functional dependency was defined as dependency in one or more activities of daily living or in three or more instrumental activities of daily living. Patient and caregiver outcomes were measured 2, 6, and 12 mo after mechanical ventilation initiation.
Measurements and Main Results: We studied three caregiver outcomes: depression risk, lifestyle disruption, and employment reduction. Most patients were male (59.8%), with a mean (SD) age of 56.6 (19.0) yr. Caregivers were mostly female (75.7%), with a mean (SD) age of 54.6 (14.7) yr. Prevalence of caregiver depression risk was high at all time points (33.9, 30.8, and 22.8%; p = 0.83) and did not vary by patient pre-ICU functional status. Lifestyle disruption and employment reduction were also common and persistent.
Conclusions: Depression symptoms, lifestyle disruption, and employment reduction were common among informal caregivers of critical illness survivors. Depression risk was high regardless of patient pre-ICU functional status.
Keywords: caregivers, depression, mechanical ventilation, outcomes research, quality of life
AT A GLANCE COMMENTARY
Scientific Knowledge on the Subject
Informal caregivers of intensive care unit survivors have significant burden, including increased risk for depression and post-traumatic stress disorder. It is not known, however, whether this burden is new and whether it changes or persists over time.
What This Study Adds to the Field
Caregivers have an elevated and persistent risk of depression, disruption in lifestyle, and reduction in employment over a 12-month period after the onset of critical illness.
More than 40 million Americans serve as informal caregivers to their ill loved ones (1), and often suffer physical (2), psychologic (3), and financial (4) burden as a result. Most evidence for caregiver burden relates to the care of the chronically ill (5–7), but a few small studies report that informal caregivers of intensive care unit (ICU) survivors and family members of current ICU patients also have significant burden (8), including increased risk for depression (9–14) and post-traumatic stress disorder (15, 16). It is not known from these studies, however, whether the post-ICU caregiver burden is new, or simply the ongoing burden of caring for individuals who had chronic conditions before ICU admission. We also do not know whether this burden changes or persists over time.
We explored this issue in the Quality of Life after Mechanical Ventilation (QOL-MV) study, which was specifically designed to examine the longitudinal outcomes of mechanically ventilated critically ill patients and their informal caregivers. We previously reported a descriptive analysis of caregiver burden at 2 mo (12). The objectives of the current article were to determine depression risk, lifestyle disruption, and effect on employment for informal caregivers up to 1 yr after initiation of mechanical ventilation. To test whether this caregiver burden was new, we compared outcomes of two caregiver cohorts, those caring for patients who were either previously healthy or physically disabled before their episode of critical illness. We hypothesized that, if there was substantial new caregiver burden, then even caregivers of previously healthy subjects would have burden, perhaps of similar magnitude to that of caregivers of previously functionally dependent subjects. Furthermore, if the burden was a new and sustained problem, then caregiver burden would be similar between groups as long as 1 yr later. Some of the results of this study have been previously reported in the form of an abstract (17, 18).
METHODS
Study Design
This prospective, parallel cohort study was designed to examine longitudinal outcomes of survivors of critical illness and their informal caregivers. A detailed description was previously reported (19). The QOL-MV cohort included patients admitted to medical, surgical, neurotrauma, and neurologic ICUs at a tertiary care teaching hospital in Pittsburgh, Pennsylvania, from June 1997 to July 1999. Patients and their caregivers were eligible if mechanical ventilation was required for 48 h or more. This report describes caregiver outcomes 2, 6, and 12 mo after initiation of mechanical ventilation. The protocol was approved by the University of Pittsburgh Institutional Review Board.
Patient Data Collection and Measurements
Baseline patient data were collected at the time of enrollment and included sociodemographics, ICU admission diagnosis, Acute Physiology and Chronic Health Evaluation (APACHE) III score (20), Short Form–36 Physical Function (SF-36 PF) (21), and the Charlson Comorbidity Index score (22). Baseline functional status was assessed retrospectively at the time of enrollment, a previously validated approach (23). Post-ICU functional status and residence location data were collected 2, 6, and 12 mo after the initiation of mechanical ventilation. Functional status was measured with two scales; the Activities of Daily Living (ADL) Scale, ranging from 0 to 6, and the Instrumental Activities of Daily Living (IADL) Scale, ranging from 0 to 8 (24, 25). Functional dependency was defined as the presence of at least one ADL or three IADL dependencies (26). Patient or caregiver use of paid assistance was measured by asking the question: “In the past week have any paid caregivers provided help?” “Help” was defined as supervision, direction, or personal assistance.
Informal Caregiver Data Collection and Measurements
Informal caregiver data were collected 2, 6, and 12 mo after the initiation of mechanical ventilation, and included sociodemographic information and outcomes in three domains: depression risk, lifestyle disruption, and reduction in employment. Depression symptoms were measured with the Center for Epidemiologic Studies Depression (CES-D) Scale (27), a 20-item instrument that has good reliability and validity (28). A score of at least 16 indicates being at risk of suffering from depression. The CES-D Scale is a screening tool for depression; formal diagnosis of depression requires further evaluation. Lifestyle disruption was evaluated with the Activity Restriction Scale (ARS), an 11-item instrument designed to measure changes in caregiver activities due to caring for the patient (29). Reduction in employment was assessed by measuring the proportion of caregivers that stopped working in order to provide care.
Statistical Analysis
To be included in the analysis of caregiver outcomes, patients had to survive at least until the initial 2-mo caregiver interview. Continuous variables are reported as mean (SD) or median (interquartile range [IQR]) where appropriate; categorical variables are reported as proportions. Comparisons between cohorts stratified by pre-ICU functional status were made by t test or Wilcoxon rank sum test for continuous variables and chi-square test or Fisher exact test for categorical variables with no adjustment for multiple comparisons. Longitudinal analyses were performed with pattern mixture models accounting for repeated measures and missing data (30, 31). Changes over time in individual variables were analyzed using time as an independent variable, with the caregiver outcome as the dependent variable (i.e., CES-D, ARS, or employment status). Predictors of depression risk (CES-D ⩾ 16) were determined by building a pattern mixture model in a stepwise manner. Patient- and caregiver-specific independent variables were included in the model if associated with CES-D in univariate analysis at a significance level of p < 0.20. p < 0.05 was used to indicate statistical significance in the final multivariable pattern mixture model and goodness of fit was assessed by the Hosmer-Lemeshow test. Statistical analyses were performed with SAS (version 8.2; SAS Institute, Cary, NC) and Stata (version 8; StataCorp, College Station, TX). Additional detail regarding study methods is provided in the online supplement.
RESULTS
Patient and Informal Caregiver Characteristics
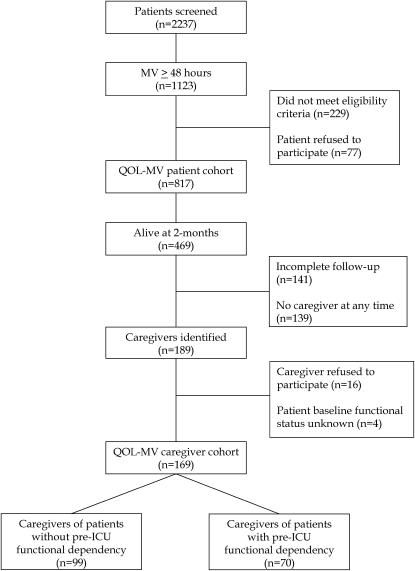
The initial QOL-MV patient cohort consisted of 817 critically ill patients who were mechanically ventilated for at least 48 h. Of these, 469 (57.4%) were alive 2 mo after the initiation of mechanical ventilation (Figure 1). A total of 189 caregivers were identified among these 2-mo survivors. Of caregivers identified, 169 were eligible for inclusion in the caregiver study, providing a total of 314 interviews over the 1-yr follow-up period. Characteristics of the 300 remaining 2-mo survivors not included in the caregiver study did not differ significantly from those of the 169 who were included (see Table E1 in the online supplement).
Figure 1.
Patient and caregiver enrollment. ICU = intensive care unit; MV = mechanical ventilation; QOL-MV = quality of life after mechanical ventilation.
Baseline patient characteristics are provided in Table 1. The majority of patients were male (59.8%) and white (89.9%). Mean (SD) age was 56.6 (19.0) yr, and 41.4% had pre-ICU functional dependency (i.e., they were dependent in at least one ADL or three IADLs). At admission, 65.7% of patients had a medical diagnosis, 22.5% had a diagnosis of trauma, and 11.8% had a surgical diagnosis.
TABLE 1.
PATIENT CHARACTERISTICS
| Patients Stratified by Pre-ICU Functional Status
|
||||
|---|---|---|---|---|
| Characteristic | All Patients | Dependent | Independent | p Value* |
| No. | 169 | 70 | 99 | |
| Age (yr), mean (SD) | 56.6 (19.0) | 64.4 (14.9) | 51.1 (19.8) | < 0.001 |
| Male, n (%) | 101 (59.8) | 33 (47.1) | 68 (68.7) | 0.05 |
| Race, n (%) | ||||
| White | 152 (89.9) | 63 (90.0) | 89 (89.9) | 0.99 |
| Black | 16 (9.5) | 7 (10.0) | 9 (9.1) | 0.99 |
| Other | 1 (0.6) | 0 (0.0) | 1 (1.0) | 0.99 |
| Education ⩾ 12th grade, n (%) | 124 (73.4) | 54 (77.1) | 70 (70.7) | 0.57 |
| Missing | 8 (4.7) | 2 (2.9) | 6 (6.1) | |
| Income, n (%) | ||||
| $0–$19,999 | 69 (40.8) | 30 (42.6) | 39 (39.4) | 0.73 |
| $20,000–$29,999 | 33 (19.5) | 18 (25.7) | 15 (15.2) | 0.24 |
| ⩾ $30,000 | 37 (21.9) | 15 (21.4) | 22 (22.2) | 0.57 |
| Missing | 30 (17.8) | 7 (10.0) | 23 (23.2) | |
| Charlson comorbidity score, median (IQR) | 1 (0–3) | 2 (1–4) | 0 (0–2) | < 0.001 |
| Baseline ADL (range, 0–6), median (IQR) | 0 (0–1) | 1 (0–4) | 0 (0–0) | < 0.001 |
| Baseline IADL (range, 0–8), median (IQR) | 1 (0–4) | 4 (4–7) | 0 (0–0) | < 0.001 |
| Disease category, n (%) | ||||
| Medical | 111 (65.7) | 57 (81.4) | 54 (54.5) | < 0.001 |
| Surgical | 20 (11.8) | 9 (12.9) | 11 (11.1) | 0.81 |
| Trauma | 38 (22.5) | 4 (5.7) | 34 (34.3) | < 0.001 |
| Tracheostomy, n (%) | 72 (42.6) | 29 (41.4) | 43 (43.4) | 0.88 |
| APACHE III, median (IQR) | 56 (44–73) | 62 (49–88) | 53.5 (42–67) | 0.008 |
| Missing, n (%) | 8 (4.7) | 5 (7.1) | 3 (3.0) | |
| SF-36 PF, median (IQR) | 70 (20–100) | 20 (5–40) | 100 (75–100) | < 0.001 |
| Missing, n (%) | 5 (3.0) | 1 (1.4) | 4 (4.0) | |
| MV duration (d), median (IQR) | 9 (5–18) | 7 (4–18) | 10 (5–18) | 0.42 |
| ICU LOS (d), median (IQR) | 14 (8–23) | 16.5 (7–27) | 14 (8–20) | 0.26 |
| Hospital LOS (d), median (IQR) | 23 (16–34) | 26 (18–39) | 22 (15–33) | 0.10 |
Definition of abbreviations: ADL = activities of daily living; APACHE = Acute Physiology and Chronic Health Evaluation; IADL = instrumental activities of daily living; ICU = intensive care unit; IQR = interquartile range; LOS = length of stay; MV = mechanical ventilation; SF-36 PF = Short Form–36 Physical Function.
Refers to comparison between patients with and without pre-ICU functional dependency.
Caregiver characteristics are listed in Table 2. The majority of caregivers were female (75.7%) and white (91.1%). Mean (SD) age was 54.6 (14.7) yr, 53% were spouses, and 89% had a high school education. When stratified by pre-ICU functional status, caregivers of functionally dependent patients were more likely to be male and older than caregivers of functionally independent patients, although the majority of caregivers were women in either group.
TABLE 2.
CAREGIVER CHARACTERISTICS
| Caregivers Stratified by Pre-ICU Patient Functional Status
|
||||
|---|---|---|---|---|
| Characteristic | All Caregivers | Dependent | Independent | p Value* |
| No. | 169 | 70 | 99 | |
| Age (yr), mean (SD) | 54.6 (14.7) | 58.9 (13.9) | 51.6 (14.6) | 0.001 |
| Male, n (%) | 41 (24.3) | 24 (34.3) | 17 (17.2) | 0.02 |
| Race, n (%) | ||||
| White | 154 (91.1) | 64 (91.4) | 90 (90.1) | 0.99 |
| Black | 14 (8.3) | 6 (8.6) | 8 (8.1) | 0.99 |
| Other | 1 (0.6) | 0 (0.0) | 1 (1.0) | 0.99 |
| Education ⩾ 12th grade, n (%) | 150 (88.8) | 62 (88.6) | 88 (88.9) | |
| Income, n (%) | ||||
| $0–$19,999 | 50 (29.6) | 18 (25.7) | 32 (32.3) | 0.23 |
| $20,000–$29,999 | 50 (29.6) | 26 (37.1) | 24 (24.2) | 0.17 |
| ⩾ $30,000 | 54 (32.0) | 23 (32.9) | 31 (31.3) | 0.99 |
| Missing | 15 (8.9) | 3 (4.3) | 12 (12.1) | |
| Relationship, n (%) | ||||
| Spouse | 89 (52.7) | 37 (52.9) | 52 (52.5) | 0.99 |
| Other family | 60 (35.5) | 25 (35.7) | 35 (35.3) | 0.99 |
| Not family | 20 (11.8) | 8 (11.4) | 12 (12.1) | 0.99 |
Definition of abbreviation: ICU = intensive care unit.
Refers to comparison between caregivers of patients with and without pre-ICU functional dependency.
Patient and Informal Caregiver Outcomes
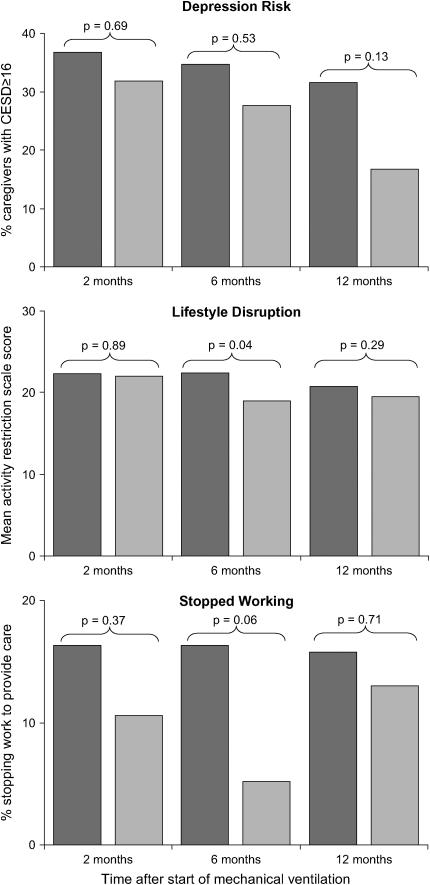
Over the 1-yr follow-up period, the proportion of functionally dependent survivors decreased (104 [91.2%], 82 [78.1%], and 64 [69.6%]; p < 0.001), and the respective proportion of patients living at home increased (57 [49.6%], 82 [77.4%], 81 [88.0%]; p < 0.001). One-third of caregivers were at risk of depression (CES-D ⩾ 16) at 2 mo (Table 3). Although the proportion of caregivers at risk of depression decreased over time, this difference was not statistically significant. When stratified by pre-ICU patient functional status (Figure 2, top), caregiver depression risk tended to be higher in those caring for patients with pre-ICU functional dependency, although these differences were not statistically significant.
TABLE 3.
CAREGIVER OUTCOMES
| Time Point
|
||||
|---|---|---|---|---|
| 2 mo (n = 115) | 6 mo (n = 107) | 12 mo (n = 92) | p Value | |
| Risk of depression | ||||
| CES-D, mean (SD) | 13.2 (11.0) | 12.7 (11.2) | 10.6 (10.7) | 0.88 |
| CES-D ⩾ 16, n (%) | 39 (33.9) | 33 (30.8) | 21 (22.8) | 0.83 |
| Lifestyle disruption | ||||
| ARS, mean (SD) | 22.1 (8.5) | 20.5 (8.4) | 20.0 (8.4) | 0.38 |
| Employment, n (%) | ||||
| Employed | 33 (28.7) | 32 (29.9) | 31 (33.7) | 0.53 |
| Stopped working to provide assistance | 15 (13.0) | 11 (10.3) | 13 (14.1) | 0.42 |
| Hours spent helping, mean (SD) | ||||
| All caregivers | 5.9 (4.8) | 5.4 (5.4) | 4.7 (5.0) | 0.43 |
| Caregivers of patients at home | 7.2 (5.5) | 5.8 (5.5) | 4.9 (5.1) | 0.008 |
| Caregivers of patients in an institution | 4.6 (3.6) | 4.0 (4.5) | 2.6 (2.7) | 0.87 |
Definition of abbreviations: ARS = Activity Restriction Scale; CES-D = Center for Epidemiologic Studies Depression Scale; mo = months after initiation of mechanical ventilation.
Figure 2.
Caregiver depression risk (top), activity restriction (middle), and employment reduction (bottom) stratified by pre-ICU patient functional status. These measures of burden were persistently elevated and tended to be higher in caregivers of patients with pre-ICU functional dependency, although this difference was significant only for 6-mo activity restriction. Dark-shaded bars, pre-ICU patient functional dependence; light-shaded bars, no pre-ICU patient functional dependency. CES-D = Center for Epidemiologic Studies Depression Scale.
Reduction in employment and disruption in lifestyle were common (Table 3). At 2 mo, only 28.7% of caregivers were employed and 13.0% indicated that they had stopped working in order to provide care. Lifestyle disruption, as measured by the ARS, was high with a mean (SD) ARS score of 22.1 (8.5) (of 44 possible) and with moderate or great restriction reported in a mean (SD) of 3.5 (3.4) lifestyle activities. Similar to depression risk, there was no statistically significant change in either employment status or lifestyle disruption over time. When stratified by pre-ICU patient functional status (Figure 2, middle and bottom), lifestyle disruption and employment reduction tended to be higher in caregivers of those with pre-ICU functional dependency, although these differences were significant only for 6-mo lifestyle disruption.
Caregivers reported spending nearly 6 h/d providing assistance at the 2-mo time point, with no significant reduction in the amount of time spent helping over the follow-up period. Time spent helping was generally greater for those caring for patients at home than for patients who were institutionalized, but this difference was only statistically significant at 2 mo (mean [SD] hours spent by location (home vs. institution): 2 mo, 7.2 [5.5] vs. 4.6 [3.6], p = 0.006; 6 mo, 5.8 [5.5] vs. 4.0 [4.5], p = 0.16; 12 mo, 4.9 [5.1] vs. 2.6 [2.7], p = 0.17). Caregivers spent more time helping patients with their IADLs than with their ADLs. Assistance was provided most often for problem solving, shopping, laundry, housekeeping, and managing finances.
In univariate analysis, the following variables were associated with caregiver depression risk (p < 0.20) and entered into the multivariable model: patient sex, patient age, caregiver sex, Charlson Comorbidity Index score, pre-ICU functional dependency, post-ICU functional dependency, tracheostomy, hospital length of stay, location (home vs. institution), and paid assistance. The subsequent multivariable model showed a good fit to the data, with a Hosmer-Lemeshow statistic of 7.19 on 8 degrees of freedom (p = 0.52). In the final multivariable model, only patient age (p = 0.005) and “paid help” (p = 0.049) were significant predictors of caregiver depression risk, indicating that caregivers of older patients and those using paid help had an increased risk of depression. Patient sex (p = 0.07) and Charlson Comorbidity Index score (p = 0.06) approached statistical significance, indicating that caregivers may have had an increased risk of depression when caring for patients who were male or had greater comorbidity. Notably, neither functional dependency nor location after discharge (home or institution) was an independent predictor of caregiver depression risk.
DISCUSSION
In the longest longitudinal follow-up to date of the informal caregivers of critical illness survivors, we found a high prevalence of depression risk, and that reduction in employment and lifestyle disruptions were common and persistent. Furthermore, our results are the first to suggest that this burden may be a direct consequence of critical illness; caregiver burden was high regardless of pre-ICU patient functional status. This study strengthens growing evidence that the negative societal impact of critical illness goes beyond short-term mortality to include significant lifestyle disruption not only for ICU survivors but also their informal caregivers.
Comparing caregivers of ICU survivors with other caregiver populations provides important insight into the negative impact of critical illness. Our results demonstrate lifestyle disruption and risk for depression that are much greater than that of the general population and similar to caregivers of Alzheimer's patients. In the general population, the prevalence of depression risk is reported to be approximately 15% (32), whereas the mean ARS score is 13.2 among community-dwelling seniors (29). Among caregivers of patients with Alzheimer's disease, depression risk may be as high as 38% (33) and is reported to be 36% among caregivers of patients with other chronic illnesses (34). Considering the tremendous caregiver burden that frequently results from caring for those with dementia, our findings underscore the severity of the downstream impairment that can occur after critical illness.
Identifying predictors of adverse caregiver outcomes, such as depression risk, is important for targeting intervention strategies. Previous studies have found a variety of predictors of caregiver depression symptoms including female sex, being a spouse, older age, more chronic conditions (35), burden (36), lifestyle interference, lower mastery (9), and overload (10). Patient depression may even be a risk factor for depression symptoms in the caregiver (9). In our study, we found that increased patient age and paid assistance were independently associated with caregiver depression symptoms. These predictors have not been previously described in informal caregivers of ICU survivors and might be surrogate markers for unmeasured patient characteristics, such as cognitive dysfunction or behavioral problems, or for caregiver depression itself, if depression led caregivers to hire help. Our ability to identify other predictors may have been limited by our sample size and the use of CES-D as a dichotomous, rather than a continuous, outcome. Interestingly, neither post-ICU functional dependency nor cohabitation was a significant predictor in our model. This is consistent with findings by others that caregiver depression symptoms occur regardless of patient location (10, 37). Moreover, the fact that functional dependency and cohabitation were not predictors in our model suggests that there might be other opportunities to improve caregiver outcomes beyond the traditional methods of respite care, rehabilitation, caregiver training (38), and occupational therapy (39). Therefore, it will be important for future studies to evaluate nonphysical patient risk factors for adverse caregiver outcomes, such as patient emotional symptoms. It will also be important to focus on early identification of risk factors, given that caregiver interventions implemented earlier in the course of patient illness could have a greater impact on caregiver outcomes (40).
Other studies have shown increased caregiver risk of depression for those caring for survivors of critical illness, but these studies were small, cross-sectional in nature, limited to a single ICU admitting diagnosis, or of limited follow-up duration (8–12, 15, 16). Although this was a single center study, patients were enrolled from four different types of ICUs (medical, surgical, trauma, and neurologic), making our results generalizable to other heterogeneous ICU patient populations.
A key limitation of our study is a lack of preillness information about patients and caregivers, a common limitation in ICU outcome studies. In particular, we did not know whether caregivers already had symptoms of depression at baseline. We inferred that caregivers of patients with pre-ICU functional dependency had greater baseline burden and depression symptoms. Although this relationship has face validity, it remains to be proven. We did not have information about prior caregiving experience, which might affect a caregiver's ability to adapt. Determining detailed preillness characteristics would require recruiting and monitoring a large cohort of patients and caregivers before critical illness develops. Given the low incidence of critical illness in the general population, such an approach would be impractical: on the basis of 6,000,000 annual ICU admissions in the United States (41) with 33% requiring mechanical ventilation (42), nearly 25,000 patients and their caregivers would have to be monitored prospectively in order to obtain the 169 caregivers in our study within a 1-yr period. Our failure to demonstrate significant decreases in caregiver burden over time or between groups may be due to our relatively small sample size and power, even though ours is the largest and only longitudinal ICU caregiver study to date with 1-yr follow-up. The depression instrument we used for this study, the CES-D, is a screening tool that measures depression symptoms; formal diagnosis of depression requires further evaluation. Even so, the CES-D scale is commonly used to determine depression risk in studies of caregiver outcomes (3). Missing data are a common problem in longitudinal studies. In our study, only 48 (28.4%) caregivers provided interviews at all three time points. We accounted for these missing data by using a general estimating equation, pattern mixture model in our analyses (30, 31). Although we did not examine caregiver mortality, one study suggests that risk of death may be greater for those whose spouse was recently hospitalized (43). We completed enrollment for this study in 1999. Our findings might underestimate the effects of critical illness on caregivers today, as shorter hospital stays may result in increased reliance on informal caregivers.
Conclusions
The impact of critical illness can be profound and long lasting for both patients and their informal caregivers. We have shown that caregivers have an elevated and persistent risk of depression, disruption in lifestyle, and reduction in employment over a 12-mo period after the onset of critical illness. Traditionally, caregiver burden has been recognized in the context of chronic illness. It is also important to study burden in the context of recovery from acute illness given that, similar to early intervention in patient illness (e.g., sepsis, stroke), improved caregiver outcomes might be expected with timely intervention. Further research is needed to identify which informal caregivers are at risk and might benefit from anticipatory guidance and interventions.
Supplementary Material
Acknowledgments
The authors thank Javier Martinez for assistance with data analysis, and Tony Dremsizov and Mike Coughlin for assistance with manuscript preparation.
Supported by NIH grants AG11970-05, HL07820, HL67181, and HS011620.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200604-493OC on October 26, 2006
Conflict of Interest Statement: None of the authors has a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.National Alliance for Caregiving; AARP. Caregiving in the United States. Available from: http://www.caregiving.org/data/04execsumm.pdf (accessed November 2006).
- 2.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA 1999;282:2215–2219. [DOI] [PubMed] [Google Scholar]
- 3.Schulz R, O'Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. Gerontologist 1995;35:771–791. [DOI] [PubMed] [Google Scholar]
- 4.Covinsky KE, Goldman L, Cook EF, Oye R, Desbiens N, Reding D, Fulkerson W, Connors AF Jr, Lynn J, Phillips RS; SUPPORT Investigators. The impact of serious illness on patients' families: Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. JAMA 1994;272:1839–1844. [DOI] [PubMed] [Google Scholar]
- 5.Hankey GJ. Informal care giving for disabled stroke survivors. BMJ 2004;328:1085–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: “they don't know what they don't know.” JAMA 2004;291:483–491. [DOI] [PubMed] [Google Scholar]
- 7.Schulz R, O'Brien A, Czaja S, Ory M, Norris R, Martire LM, Belle SH, Burgio L, Gitlin L, Coon D, et al. Dementia caregiver intervention research: in search of clinical significance. Gerontologist 2002;42:589–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foster M, Chaboyer W. Family carers of ICU survivors: a survey of the burden they experience. Scand J Caring Sci 2003;17:205–214. [DOI] [PubMed] [Google Scholar]
- 9.Cameron JI, Herridge MS, Tansey CM, McAndrews MP, Cheung AM. Well-being in informal caregivers of survivors of acute respiratory distress syndrome. Crit Care Med 2006;34:81–86. [DOI] [PubMed] [Google Scholar]
- 10.Douglas SL, Daly BJ. Caregivers of long-term ventilator patients: physical and psychological outcomes. Chest 2003;123:1073–1081. [DOI] [PubMed] [Google Scholar]
- 11.Douglas S, Daly B, Genet Kelley C, O'Tolle E, Montenegro H. Impact of a disease management program upon caregivers of chronically critically ill patients. Chest 2005;128:3925–3936. [DOI] [PubMed] [Google Scholar]
- 12.Im K, Belle SH, Schulz R, Mendelsohn AB, Chelluri L. Prevalence and outcomes of caregiving after prolonged (⩾48 hours) mechanical ventilation in the ICU. Chest 2004;125:597–606. [DOI] [PubMed] [Google Scholar]
- 13.Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, Grassin M, Zittoun R, Le Gall JR, Dhainaut JF, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 2001;29:1893–1897. [DOI] [PubMed] [Google Scholar]
- 14.Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Merouani A, Moulront S, Pigne E, Pingat J, et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death: a prospective multicenter study. J Crit Care 2005;20:90–96. [DOI] [PubMed] [Google Scholar]
- 15.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, et al.; FAMIREA Study Group. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–994. [DOI] [PubMed] [Google Scholar]
- 16.Jones C, Skirrow P, Griffiths RD, Humphris G, Ingleby S, Eddleston J, Waldmann C, Gager M. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive Care Med 2004;30:456–460. [DOI] [PubMed] [Google Scholar]
- 17.Van Pelt DC, Milbrandt EB, Chelluri L, Rotondi AJ, Angus DC, Pinsky MR; QOL-MV Investigators. Prevalence and outcomes of caregiving after prolonged mechanical ventilation [abstract]. Proc Am Thorac Soc 2005;2:A596. [Google Scholar]
- 18.Van Pelt DC, Milbrandt EB, Chelluri L, Rotondi AJ, Angus DC, Pinsky MR. Lifestyle disruption among informal caregivers of survivors of mechanical ventilation of greater than 48 hours [abstract]. Proc Am Thorac Soc 2006;3:A833. [Google Scholar]
- 19.Chelluri L, Rotondi AJ, Mendelsohn AB, Sirio CA, Donahoe MP, Pinsky MR, Belle SH, Schulz R. 2-Month mortality and functional status of critically ill adult patients receiving prolonged mechanical ventilation. Chest 2002;121:549–558. [DOI] [PubMed] [Google Scholar]
- 20.Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A. The APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991;100:1619–1636. [DOI] [PubMed] [Google Scholar]
- 21.McDowell I, Newell C. Measuring health: a guide to rating scales and questionnaires, 2nd ed. New York: Oxford University Press; 1996.
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 23.Covinsky KE, Palmer RM, Counsell SR, Pine ZM, Walter LC, Chren MM. Functional status before hospitalization in acutely ill older adults: validity and clinical importance of retrospective reports. J Am Geriatr Soc 2000;48:164–169. [DOI] [PubMed] [Google Scholar]
- 24.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged, the index of adl: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–919. [DOI] [PubMed] [Google Scholar]
- 25.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–186. [PubMed] [Google Scholar]
- 26.Wu JH, Haan MN, Liang J, Ghosh D, Gonzalez HM, Herman WH. Diabetes as a predictor of change in functional status among older Mexican Americans: a population-based cohort study. Diabetes Care 2003;26:314–319. [DOI] [PubMed] [Google Scholar]
- 27.Radloff L. The Center for Epidemiological Studies-Depression Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 28.Radloff L, Teri L. Use of the center for epidemiological studies depression scale with older adults. Clin Gerontol 1986;5:119–135. [Google Scholar]
- 29.Williamson GM, Schulz R. Pain, activity restriction, and symptoms of depression among community-residing elderly adults. J Gerontol 1992;47:367–372. [DOI] [PubMed] [Google Scholar]
- 30.Little RJ, Wang Y. Pattern-mixture models for multivariate incomplete data with covariates. Biometrics 1996;52:98–111. [PubMed] [Google Scholar]
- 31.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13–22. [Google Scholar]
- 32.Zhang X, Norris SL, Gregg EW, Cheng YJ, Beckles G, Kahn HS. Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol 2005;161:652–660. [DOI] [PubMed] [Google Scholar]
- 33.Schulz R, Williamson GM. A 2-year longitudinal study of depression among Alzheimer's caregivers. Psychol Aging 1991;6:569–578. [DOI] [PubMed] [Google Scholar]
- 34.Tennstedt S, Cafferata GL, Sullivan L. Depression among caregivers of impaired elders. J Aging Health 1992;4:58–76. [DOI] [PubMed] [Google Scholar]
- 35.Baumgarten M, Battista RN, Infante-Rivard C, Hanley JA, Becker R, Gauthier S. The psychological and physical health of family members caring for an elderly person with dementia. J Clin Epidemiol 1992;45:61–70. [DOI] [PubMed] [Google Scholar]
- 36.Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol 1991;46:181–189. [DOI] [PubMed] [Google Scholar]
- 37.Schulz R, Belle SH, Czaja SJ, McGinnis KA, Stevens A, Zhang S. Long-term care placement of dementia patients and caregiver health and well-being. JAMA 2004;292:961–967. [DOI] [PubMed] [Google Scholar]
- 38.Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, Donaldson N. Training carers of stroke patients: randomised controlled trial. BMJ 2004;328:1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW. A randomized, controlled trial of a home environmental intervention: effect on efficacy and upset in caregivers and on daily function of persons with dementia. Gerontologist 2001;41:4–14. [DOI] [PubMed] [Google Scholar]
- 40.Whitlatch CJ, Feinberg LF, Sebesta DS. Depression and health in family caregivers: adaptation over time. J Aging Health 1997;9:222–243. [DOI] [PubMed] [Google Scholar]
- 41.Angus DC. The future of critical care. Crit Care Clin 2005;21:163–169. [DOI] [PubMed] [Google Scholar]
- 42.Esteban A, Anzueto A, Alia I, Gordo F, Apezteguia C, Palizas F, Cide D, Goldwaser R, Soto L, Bugedo G, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med 2000;161:1450–1458. [DOI] [PubMed] [Google Scholar]
- 43.Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med 2006;354:719–730. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.