Abstract
The mutation spectrum of CYP1B1 among 104 primary congenital glaucoma patients of the genetically heterogeneous Iranian population was investigated by sequencing. We also determined intragenic single nucleotide polymorphism (SNP) haplotypes associated with the mutations and compared these with haplotypes of other populations. Finally, the frequency distribution of the haplotypes was compared among primary congenital glaucoma patients with and without CYP1B1 mutations and normal controls. Genotype classification of six high-frequency SNPs was performed using the PHASE 2.0 software. CYP1B1 mutations in the Iranian patients were very heterogeneous. Nineteen nonconservative mutations associated with disease, and 10 variations not associated with disease were identified. Ten mutations and three variations not associated with disease were novel. The 13 novel variations make a notable contribution to the ∼70 known variations in the gene. CYP1B1 mutations were identified in 70% of the patients. The four most common mutations were G61E, R368H, R390H, and R469W, which together constituted 76.2% of the CYP1B1 mutated alleles found. Six unique core SNP haplotypes were identified, four of which were common to the patients with and without CYP1B1 mutations and controls studied. Three SNP blocks determined the haplotypes. Comparison of haplotypes with those of other populations suggests a common origin for many of the mutations.
Glaucoma is a heterogeneous group of optic neuropathies with common manifestations including a specific pattern of visual field loss and degeneration of the optic nerve resulting in a characteristic glaucomatous appearance.1,2 Degeneration of the optic nerve may be caused by apoptosis of retinal ganglion cells.3 Glaucoma leads to blindness if left untreated, and it is considered the second leading cause of blindness worldwide.4 The disease is subclassified based on etiology, anatomy of the anterior chamber of the eye, and age of onset.2 The subgroup primary congenital glaucoma (PCG; Online Mendelian Inheritance of Man no. 231300) is a severe form of the disease. It is characterized by an anatomical defect of the trabecular meshwork (trabeculodysgenesis) and an age of onset in the neonatal or infantile period, generally before the age of 3 years.5 The developmental anomaly at the angle of the anterior chamber manifests itself by increased intraocular pressure (IOP), corneal edema, excessive tearing, photophobia, enlargement of the globe (buphthalmos), and opacity of the cornea. The details of the pathogenic pathways, including the relationship between elevated IOP and optic nerve damage, are not well understood. PCG occurs in both sporadic and familial patterns. In familial cases, inheritance is usually autosomal recessive, sometimes associated with incomplete penetrance.5,6 Pseudodominant transmission has also been reported.7 The incidence of PCG is geographically and ethnically variable, estimated at 1:10,000 in Western countries5 and higher in inbred populations such as those of Andhra Pradesh in India (1:3300),8 Saudi Arabia (1:2500),6 Slovakia Roma (1:1250),9 and Arab Bedouins of the Negro region in Israel (1 of 1200).10
So far, three PCG loci have been identified by linkage analysis in multiply affected families, GLC3A,11 GLC3B,12 and GLC3C.5,13 Only the gene associated with GLC3A, CYP1B1 (Online Mendelian Inheritance of Man no. 601771), has been identified.14 The CYP1B1 gene spans ∼12 kb on chromosome 2, has three exons, encodes cytochrome P4501B1, and is a member of the cytochrome P450 superfamily of genes.15 Protein products of these genes catalyze oxidative, peroxidative, and reductive reactions and have roles in the metabolism of various substrates. Expression of the CYP1 gene family, which includes CYP1B1, is induced by the aryl hydrocarbon receptor. Although physiological studies have confirmed that mutations in CYP1B1 can cause disease, the pathway by which CYP1B1 affects development of the anterior chamber of the eye is unknown.15,16 Presumably, the metabolism of an endogenous substrate by the CYP1B1 protein is involved. Expression of CYP1B1 in the posterior segment of the eye, notably in the neuroretina, may be relevant to glaucoma pathogenesis.17 In addition to glaucoma, CYP1B1 may have a role in carcinogenesis. Unusually high expression of the gene or increased frequencies of alleles coding more active isoforms have been reported in some cancers.18,19,20
The proportion of PCG patients whose disease is attributable to CYP1B1 mutations is generally high but varies among populations. Comparisons are not definitive, particularly because of differences in sample size, composition of samples with regard to familial and sporadic classifications, and detection protocols; nevertheless, the published figures clearly indicate that the variation exists. The numbers range from 100 to 20%: 100% in Slovakia Roma,9 ∼90% in Saudi Arabia,6 ∼50% in Brazil21 and France,22 ∼40% in India23 and Morocco,24 and ∼20% in Japan.25 CYP1B1 may have a lesser role in the disease status of African PCG patients as compared with Europeans.21
The worldwide profile of variations thus far reported is heterogeneous and includes ∼70 alterations (Human Genome Mutation Database; http://www.hgmd.cf.ac.uk/ac/index.php). The degree of heterogeneity within different populations, as well as the distribution of mutations, is quite variable.26 A single allele, E387K, constitutes all CYP1B1 mutated alleles among the Slovak Roma patients.9 Likewise, only the V364M mutation was found among PCG patients of Indonesian descent.27 In Saudi Arabia, G61E constitutes ∼75% of the mutated alleles, and R469W and D374N account for almost all of the rest.6,28 Mutation g.4339delG is the predominant mutation among patients from Morocco.24 Among less than 30 PCG patients with CYP1B1 mutations from India23 and Brazil,21 respectively, 16 and 11 different mutations were found. However, a single mutation, R368H in India and g.4340delG in Brazil, constituted ∼20% of the aberrant alleles in their respective populations. In contrast to these populations, 11 different mutations were found among only eight patients of French descent carrying CYP1B1 mutations.22 The same number of mutations was identified among 13 Japanese patients.25 These differences are likely attributable to variations in frequencies of consanguineous marriages and gene pools among the different populations.
The genetic basis of PCG among Iranian patients has not been previously studied. Iran, having been a major gateway in human history, has encountered many populations and is expected to have a rich genetic legacy. Here, we report the frequency of Iranian PCG patients carrying mutations in the coding regions of the CYP1B1 gene. Mutations thought to be associated with PCG, including 10 novel ones, and variations thought not to be associated with PCG, three of which are novel, are described. Intragenic single nucleotide polymorphism (SNP) haplotypes associated with the mutations are presented and compared with those previously reported for other populations.
Materials and Methods
This research was performed in accordance with the Helsinki Declaration and with the approval of the ethics board of the International Institute for Genetic Engineering and Biotechnology in Iran. The families of patients all consented to participate after being informed of the nature of the research. One hundred four unrelated patients were recruited mostly from the ophthalmic divisions of the Farabi (associated with Tehran University of Medical Sciences), Labbafi-Nejhad (associated with Shaheed Beheshti University of Medical Sciences and Health Services), and Hazrat Rasoolakram (associated with Iran University of Medical Sciences) hospitals in Tehran. The hospitals are national reference centers, and patients from throughout the country are referred to them. All patients were diagnosed by glaucoma specialists. Slit lamp biomicroscopy, measurement of IPO, gonioscopy (if corneal clarity permitted), fundus examination, and measurement of perimetry were performed whenever possible. IOP measurements were obtained using Goldmann tonometry or the Tono-Pen (Medtronic, Minneapolis, MN) in cases with limited cooperation or central corneal scars. PCG manifested in the patients by IOP of ≥21-mm mercury (21 to 56 mm Hg) in at least one eye before treatment, corneal edema, Descemet membrane rupture, megalocornea (corneal diameter >12 mm), and optic nerve head changes suggestive of glaucomatous damage including high cup/disc ratio or neuronal rim thinning or notching. The cup/disc ratio of affected eyes when available ranged from 0.3 to total cupping (average, 5.8). Patients with other ocular or systemic anomalies were excluded. For example, patients diagnosed with Peters’ anomaly or aphakic glaucoma after congenital cataract surgery were not included. Age of onset ranged from birth to 3 years. One hundred sixty ethnically matched but unrelated control individuals were recruited from those older than 60 years of age and without self-reported familial history of ocular diseases. Older individuals were recruited because mutations in CYP1B1 has been reported in some late onset glaucoma patients.22,29
The patients were recruited consecutively, without regard to familial status of disease. Of the 104 PCG patients, 33 were sporadic in the sense that their parents indicated no consanguinity and no other incidence of disease in relatives of the patient. Fifty-eight patients were offspring of consanguineous parents. Of these, 46 had no other affected family member. Seventeen patients were recurrent cases in the sense that more than one family member was affected with PCG. Five of these were progeny of reported nonconsanguineous marriages. PCG in progeny of consanguineous marriages and in recurrent cases was considered familial; there were thus 63 familial PCG patients. The sporadic/familial status of eight patients could not be ascertained.
Exon 1 of the CYP1B1 gene was amplified by polymerase chain reaction (PCR) in 50 patients. The primers corresponded to sequences adjacent to the exon (F, forward; R, reverse) (1F: 5′-GAAAGCCTGCTGGTAGAGCTCC-3′; 1R: 5′-CTGCAATCTGGGGACAACGCTG-3′). Exon 2, which contains the initiation codon, was amplified in all 104 patients in two overlapping PCR fragments (2Fa: 5′-ATTTCTCCAGAGAGTCAGCTCCG-3′; 2Ra: 5′-TGTAGCGGCAGCCGAAACACAC-3′; Fb: 5′-GCATGATGCGCAACTTCTTCACG-3′; 2Rb: 5′-TCACTGTGAGTCCCTTTACCGAC-3′). The coding region of exon 3 was also amplified in all of the patients (3F: 5′-AATTTAGTCACTGAGCTAGATAGCC-3′; 3R: 5′-TATGGAGCACACCTCACCTGATG-3′). The amplicon of exon 1 included 172 nucleotides upstream of the transcriptional initiation site and 136 nucleotides of intron 1. The amplicons of exon 2 included 133 and 161 nucleotides of introns 1 and 2, respectively. The amplicon of exon 3 included 129 nucleotides of intron 2 and 155 nucleotides downstream of its protein coding region. All PCR products were sequenced in both forward and reverse directions with the same primers as used in the PCRs, using the ABI Big Dye terminator chemistry and an ABI Prism 3700 instrument (Applied Biosystems, Foster City, CA). The CYP1B1 amplicons of 10 control individuals were also fully sequenced. Sequences were analyzed by the Sequencher software (Gene Codes Corp., Ann Arbor, MI).
Four of the novel single nucleotide variations deemed to be possibly associated with disease were assessed in 60 to 109 control individuals by restriction enzyme digestion and fragment length polymorphism (RFLP) as described below. All of the controls were Iranian, and at least 50 were from the same region of the country as the patients carrying the variations. Likewise, five SNPs contributing to unique core haplotypes were assessed in 100 control individuals from throughout Iran by RFLP. The enzymes used for g.3947C>G (R48G), g.4160G>T (A119S), g.8131G>C (V432L), g.8184T>C (D449D), and g.8195A>G (N453S) were BsaWI, NaeI, AleI, BseGI, and MwoI, respectively. The restriction enzymes were purchased from New England BioLabs (Boston, MA), Roche (Mannheim, Germany), or Cinnagen (Tehran, Iran). One SNP of the haplotypes of the controls, g.3793T>C, was assessed only in the 10 individuals sequenced because a restriction enzyme appropriate for its analysis by RFLP was not identified.
Unique core haplotypes consisting of six SNPs were assessed in patients with CYP1B1 mutations, patients without CYP1B1 mutations, and the control group using the PHASE 2.0 software.30,31 This program of the software implements a Bayesian statistical method for reconstructing haplotypes. Use of the fastPHASE 1.0.1 software, which is based on a cluster model that includes an E-M algorithm, produced identical results.32 Statistical comparisons of haplotype frequencies between and among groups were done using χ2 contingency tables.33
Sequence variations and numbering were assessed by comparison with reference sequences associated with CYP1B1 available at National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov; genomic sequence, NT_022184.14; cDNA sequence, NM_000104.2, protein sequence, NP_000095.1). Predicted effects of variant sequences on splicing were determined by comparison with known canonical splice site motifs (http://www.fruitfly.org/seq_tools/splice.html). For determination of extent of conservation of amino acids altered because of nucleotide variations, the amino acid sequences of 34 cytochrome P450 proteins from 18 species were obtained from SwissProt (http://expasy.org./sprot/) and aligned using the ClustalW software (European Bioinformatics Institute, Hinxton, UK; http://www.ebi.ac.uk/clustalw).
Results
Novel Variations
Twenty-nine sequence variations were identified in the regions of the CYP1B1 gene sequenced in DNA of the Iranian PCG patients and controls (Tables 1 and 2). Ten of the variations have been previously reported to be mutations associated with disease in the literature and six others reported as variations thought not to cause PCG; most of these are listed in the Human Genome Mutation Database. Although CYP1B1 polymorphisms and mutations associated with PCG have now been reported in various ethnic groups, only limited information is available on genotype-phenotype correlations.21,34,35,36 Among the previously reported disease-causing mutations also found among the Iranian patients, some phenotypic data for T404fs (g.8037-8096dup10) in the Brazilian population are available.21 The phenotypic features of two Brazilian homozygotes carrying this mutation were similar to those of the single homozygous Iranian patient: the three were diagnosed before the age of 1 month, both eyes were affected in all, and their maximum recorded IOP ranged from 26 to 31.5 mm Hg. Phenotypic features associated with mutations found among a larger number of both Iranian and Indian patients are presented in Table 3.35 Only data on homozygous patients are presented so as to eliminate variations attributable to effects of differing second mutations. Data on R390H and R469W are included because these are common mutations among the Iranian patients. The data on R390H of the Iranians also allow comparison with R390C, which affects the same amino acid position and is found among the Indian patients. The remaining 13 novel variations were designated mutations associated with PCG or variations probably not associated with the disease on the basis of causing frameshifts or creating stop codons during translation, absence in control individuals, presence in more than one unrelated patient, occurring at same site as a previously reported mutation, nature of amino acid change caused, and/or degree of conservation during evolution.
Table 1.
CYP1B1 Mutations Associated with PCG in Iranian Patients
| Gene location* | cDNA location*† | Exon | Effect on protein* | Nature of amino acid change‡ | Number of patients
|
Total no. alleles | Percent of PCG causing chromosomes§ | Percent of mutated CYP1B1 alleles | |
|---|---|---|---|---|---|---|---|---|---|
| Hom | Het | ||||||||
| g.3987G>A | c.182G>A | 2 | p.G61E | NC | 15 | 15 | 45 | 21.6% | 32.4% |
| g.3988delA¶ | c.183delA¶ | 2 | p.G61fs¶ | 1 | 0 | 2 | 1.0% | 1.4% | |
| g.4048C>A¶ | c.243C>A¶ | 2 | p.Y81X¶ | 1 | 0 | 2 | 1.0% | 1.4% | |
| g.4322G>A | c.517G>A | 2 | p.E173K | NC | 2 | 0 | 4 | 1.9% | 2.9% |
| g.4410C>A¶ | c.620C>A¶ | 2 | p.A202D¶ | NC | 0 | 1 | 1 | 0.5% | 0.7% |
| g.4490G>A | c.685G>A | 2 | E229K | NC | 1 | 1 | 3 | 1.4% | 2.2% |
| g.4611_4619 dupGCAACTTCA¶ | c.806–814 dupGCAACTTCA¶ | 2 | p.N265_R266 insSNL¶ | 1 | 0 | 2 | 1.0% | 1.4% | |
| g.4673_4674insC | c.862insC | 2 | p.R290fs | 2 | 0 | 4 | 1.9% | 2.9% | |
| g.4677A>G¶ | c.872A>G¶ | 2 | p.D291G¶ | NC | 1 | 0 | 2 | 1.0% | 1.4% |
| g.4791G>T¶ | c.986G>T¶ | 2 | p.G329V¶ | NC | 0 | 2 | 2 | 1.0% | 1.4% |
| g.7934delG¶ | c.1097delG¶ | 3 | p.R366fs¶ | 1 | 0 | 2 | 1.0% | 1.4% | |
| g.7939C>T¶ | c. 1102C>T¶ | 3 | p.R368C¶ | NC | 1 | 1 | 3 | 1.4% | 2.2% |
| g.7940G>A | c. 1103G>A | 3 | p.R368H | NC | 2 | 9 | 13 | 6.3% | 9.4% |
| g.8006G>A | c. 1169G>A | 3 | p.R390H | NC | 12 | 8 | 32 | 15.4% | 23.0% |
| g.8037_8046 dupTCATGCCACC | c.1200_1209 dupTCATGCCACC | 3 | p.T404fs | 1 | 1 | 3 | 1.4% | 2.2% | |
| g.8162C>G | c.1325C>G | 3 | p.P442R | NC | 0 | 1 | 1 | 0.5% | 0.7% |
| g.8242C>T | c.1405C>T | 3 | p.R469W | NC | 7 | 2 | 16 | 7.7% | 11.5% |
| g.8341delA¶ | c.1504 del A¶ | 3 | p.M503fs¶ | 0 | 1 | 1 | 0.5% | 0.7% | |
| g.8354_8373del GTTATGGTCT-AACCATTAAA¶ | c.1517_1536 delGTTATGGT-CTAACCATTAAA¶ | 3 | p.S506fs¶ | 1 | 0 | 2 | 1.0% | 1.4% | |
| 67.5% | ∼100% | ||||||||
The four most common mutations are shown in bold. Reference sequences used were NT_022184.14, NM_000104.2, and NP_000095.1.
A of the initiation codon was designated +1.
Based on biochemical properties of size and charge.
Assuming autosomal recessive status of disease in all patients.
Novel mutation.
Hom, homozygous; Het, heterozygous; fs, frameshift: NC, nonconservative.
Table 2.
CYP1B1 Variations Not Associated with PCG in Iranian Patients
| Gene location | cDNA location* | Exon | Effect on protein | Nature of amino acid change† | Number of patients
|
Total no. alleles | Minor allele frequency | Reference SNP number‡ | |
|---|---|---|---|---|---|---|---|---|---|
| Hom | Het | ||||||||
| g.3318 insC | 5′NC.-487insC | 2 | 50 | 0 | 100 | 0% | |||
| g.3793 T>C | IVS I.-13T>C | 2 | 17 | 21 | 55 | 27.0% | rs4987134 | ||
| g.3947 C>G | c.142C>G | 2 | p.R48G | NC | 17 | 21 | 55 | 27.0% | rs1001 |
| g.4131 A>G§ | c.326A>G§ | 2 | p.Q109R§ | C | 1 | 0 | 2 | 1.0% | |
| g.4160 G>T | c.355G>T | 2 | p.A119S | C | 17 | 21 | 55 | 27.0% | rs1056827 |
| g.4612 C>T§¶ | c.807C>T§¶ | 2 | p.S269S§¶ | S | 0 | 1 | 1 | 0.5% | |
| g.8032 A>G§ | c.1195A>G§ | 3 | p.I399V§ | C | 1 | 0 | 2 | 1.0% | |
| g.8131 G>C | c.1294G>C | 3 | p.V432L | C | 39 | 25 | 103 | 49.5% | rs1056836 |
| g.8184 T>C | c.1347T>C | 3 | p.D449D | S | 39 | 25 | 103 | 49.5% | rs1056837 |
| g.8195 A>G | c.1358A>G | 3 | p.N453S | C | 8 | 10 | 26 | 12.5% | rs1800440 |
A of the initiation codon was designated +1.
Based on biochemical properties of size and charge.
From build 125 of the SNP database at the National Center for Biotechnology Information.
Novel variation.
This variation was found in a control individual.
Hom, homozygous; Het, heterozygous; NC, nonconservative; C, conservative; S, synonymous.
Table 3.
Phenotype-Genotype Correlations in PCG Patients of Iran and India
| Mutation* | Onset by birth†
|
Corneal diameter (mm) ‡
|
IOP (mm Hg)‡
|
C/D ratio‡§
|
||||
|---|---|---|---|---|---|---|---|---|
| India | Iran | India | Iran | India¶ | Iran∥ | India | Iran | |
| G61E | 3 (3) | 9 (15) | 3.9 (6) | 13.4 (29) | 30.2 (6) | 29.1 (28) | 0.48 (4) | 0.49 (15) |
| R368H | 17 (19) | 1 (2) | 13.0 (38) | 15.3 (3) | 26.1 (36) | 29.7 (3) | 0.48 (20) | 0.87 (3) |
| R390C | 5 (5) | 12.5 (8) | 26.6 (10) | 0.30 (2) | ||||
| R390H | 5 (8) | 12.7 (24) | 33.4 (24) | 0.65 (8) | ||||
| R469W | 2 (3) | 13.9 (8) | 30.0 (14) | 0.60 (6) | ||||
Data for patients from India based on Ref. 35.
All homozygous.
Number of patients (no. of patients with the mutation).
Average of eyes for which data is available (no. of eyes for which data is available).
Cup/disc ratio of the optic nerve.
IOP at diagnosis.
Maximum IOP.
Variations g.3988delA(G61fs), g.7934delG(R366fs), g.8341delA(M503fs), and g.8354_8373delGTTATGGTCT-AACCATTAAA(S506fs) were considered as pathogenic because they all caused frameshifts (Table 1). The Y81X alteration was classified as disease-causing because it results in very early truncation of the CYP1B1 protein. Variations A202D, D291G, G329V, and R368C were also considered putative disease-causing mutations. The nucleotide substitutions causing these amino acid changes were not found in the DNA of control individuals by RFLP analysis (not shown). All result in nonconservative amino acid alterations with respect to size and charge at positions where the wild-type residue is highly conserved (Table 4). In addition, D291G lies within a –PGAARDM– sequence and G329V within a 15-amino acid sequence (–TDIFGASQDTLSTAL–) in helix I common to CYP1B1 sequences of distally related species (Table 4). G329V and R368C were observed in more than one patient. Furthermore, R368C affects the same amino acid position as R368H, which has been reported by others to be associated with disease.34,37 Finally, g.4611_4619dupGCAACTTCA causes an in-frame insertion of Ser/Asn/Leu after residue 265 and was considered a disease-causing mutation. This 9-bp sequence is tandemly repeated twice in the CYP1B1 reference sequence NT_022184.14. Deletion of one of the repeats has previously been reported as a deleterious mutation.6 Furthermore, the insertion disrupts the –NRNFS– sequence that is highly conserved among CYP1B1s of species as distally related as the dolphin and human (not shown).
Table 4.
Alignment of Novel Amino Acid Variations in Cytochrome P450 Proteins
| Variation | Q109R | A202D | D291G | G329V | R368C | I399V | Seq ID* |
|---|---|---|---|---|---|---|---|
| CYP1A1_Human | QALVRQGD | VVSVTNVIC | EK-GHIRDIT | IVLDLFGAGFDTVTTAIS | RKIQEELDTVIGRSRRPRLS | VPFTIPHST | sp P04798 |
| CYP1A1_Mouse | QALVRQGD | VVSVANVIC | EK-GHIRDIT | IVLDLFGAGFDTVTTAIS | RKIQEELDTVIGRDRQPRLS | VPFTIPHST | sp P00184 |
| CYP1A1_Rat | QALVKQGD | VVSVANVIC | EK-GHIRDIT | IVFDLFGAGFDTITTAIS | RKIQEELDTVIGRDRQPRLS | VPFTIPHST | sp P00185 |
| CYP1A1_Monkey | QALVQQGD | VISVANVIC | EK-GHIRDIT | VVLDLFGAGFDTVTTAIS | RKIQEELDTVIGRSRRPRLS | VPFTIPHST | sp Q6GUR1 |
| CYP1A1_Dog | QALVRQGD | VVSVANVIC | EK-GQIRDVT | VVLDLFGAGFDTVTTAIS | KKIQKELDTVIGRARQPRLS | VPFTIPHST | sp P56590 |
| CYP1A1_Sheep | QALVRQGD | VVSVANVIC | EK-GHIRDIT | VVMDLFGAGFDTVTTAIS | KKIQEELDTVIGRARWPQLS | VPFTIPHST | sp P56591 |
| CYP1A1_Guinea pig | QALVRQGD | VVSVANVIS | EK-GHIRDIT | IVLDLFGAGFDTITTAIS | KKIQEELDTVIGRERQPQLA | MPFTIPHST | sp Q06367 |
| CYP1A1_Hamster | QALVRQGD | VVSVTNVIC | EK-GHIRDIT | IIVDLFGAGFDTVTTAIS | RKIQEELDTVIGRSRRPRLC | LPFTIPHST | sp Q00557 |
| CYP1A1_Rabbit | QALVRQGD | VMSVANVIC | EK-GHIRDIT | IVLDLFGAGFDTVTTAIS | RKIQEELDAVVGRARRPRFS | LPFTIPHST | sp P05176 |
| CYP1A1_Sea bream | QALIKQGD | VVSVANVIC | DK-DNIRDIT | IVNDLFGAGFDTISTALS | ERLYQEMKESVGLDRTPCLS | LPFTIPHCS | sp O42457 |
| CYP1A1_Scup | QALIKQGD | VVSVANVIC | DK-DNIRDIT | IVNDLFGAGFDTISTALS | ERLYQEMNETVGPDRTPCLS | LPFTIPHCT | sp Q92116 |
| CYP1A1_Plaice | QALIKQGD | VVSVANVIC | NK-DNIRDIT | IVNDLFGAGFDTVSTALS | ERLYQEIEDKVGLDRMPLLS | LPFTIPHCT | sp Q92100 |
| CYP1A1_Oyster | QALIKQGE | VVSVANVIC | NK-DNIRDIT | IVNDLFGAGFDTVSTGLS | ERLYQEIKDSVGTERMPLLS | LPFTIPHCT | sp Q92095 |
| CYP1A1_Trout | QALIKQGE | VVSVANVIC | DK-DNIRDIT | IVNDLFGAGFDTISTALS | ERLHQELKEKVGMIRTPRLS | LPFTIPHCT | sp Q92110 |
| CYP1A1_Tomcod | QALIKQGH | VVSVANVIC | DK-DNIRDIT | IVNDLFGAGFDTVSTALS | ERLHQEIKDKVGLSRSPVLT | LPFTIPHCA | sp Q92148 |
| CYP1A2_Human | QALVRQGD | VVSVANVIG | DK-NSVRDIT | LVNDIFGAGFDTVTTAIS | RKIQKELDTVIGRERRPRLS | LPFTIPHST | sp P05177 |
| CYP1A2_Dog | QALVRQGD | LLSVANVIG | DE-RSVQDIT | LINDIFGAGFDTVTTAIS | RQIQKELDTVIGRARQPRLS | VPFTIPHST | sp P56592 |
| CYP1A2_Rabbit | QALVRQGD | VVSAARVIG | DR-NSIQDIT | LVNDIFGAGFDTITTALS | RKIQEELDAVVGRARQPRLS | VPFTIPHST | sp P00187 |
| CYP1A2_Mouse | QALVRQGD | VESVANVIG | NK-NSIQDIT | IVNDIFGAGFDTVTTAIT | RKIHEELDTVVGRDRQPRLS | VPFTIPHST | sp P00186 |
| CYP1A2_Rat | QALVKQGD | VESVANVIG | NK-NSIQDIT | IVNDIFGAGFETVTTAIF | RKIHEELDTVIGRDRQPRLS | VPFTIPHST | sp P04799 |
| CYP1A2_Hamster | QALVRQGD | VESVANVIG | NK-NSIQDIT | IVNDLFGAGFDTVTTAIT | RKIHKELDTVIGRDRQPRLS | VPFTIPHST | sp P24453 |
| CYP1A2_Guinea pig | QALVRQSD | VGSVANVIG | DK-NHVQDIA | LVNDIFGAGFDTVTTAIS | KKIHKELDAVIGRDRKPRLA | LPFTIPHCT | sp Q64391 |
| CYP1A3_Trout | QALIKQGE | VVSVANVIC | DK-DNIRDIT | IVNDLFGAGFDTISTALS | ERLHQELKEKVGMIRTPRLS | LPFTIPHCT | sp Q92109 |
| CYP1A4_Chicken | QALVRQAE | MVSVANVIC | DK-EHIRDVT | IVNDLFGAGFDTVTTALS | KKIQAELDQTIGRERRPRLS | LPFTIPHCT | sp P79760 |
| CYP1A5_Chicken | QALVRQAE | VVSVANVIC | DK-NNIRDVT | LVNDIFGAGFDTVTTALS | KKIQAELDQTIGRERRPRLS | MPFTIPHST | sp P79761 |
| CYP1B1_Human | QALVQQGS | VVAVANVMS | RPGAAPRDMM | TITDIFGASQDTLSTALQ | TRVQAELDQVVGRDRLPCMG | VPVTIPHAT | sp Q16678 |
| CYP1B1_Mouse | QALVQQGS | IVAVANVMS | VPGAAPRDMT | TITDIFGASQDTLSTALL | ARVQAELDQVVGRDRLPCMS | LPVTIPHAT | sp Q64429 |
| CYP1B1_Rat | QALVQQGG | IVAVANVMS | VPGAAPRDMM | TITDIFGASQDTLSTALL | ARVQAELDQVVGRDRLPCMS | LPVTLPHAT | sp Q64678 |
| CYP1B1_Dolphin | -------- | -----NVMS | RPGAAPRDMM | TVTDIFGASQDTLSTALQ | ARVQAELDQVVGRDRLPCLD | VPVTIPHAT | tr Q8SQH0 |
| CYP1B_Plaice | QALVKQGT | VVSTANIMS | QS-STTRDMT | TMGDIFGASQDTLSTALQ | LRIQQEVDKVVDRTRLPSIE | VPLTIPHST | tr Q9W713 |
| CYP1B_Zebrafish | -------- | --------- | ---------- | --------SQDTLSTALQ | KRLQEDVDRVVDRSRLPTIA | TPLTIPHST | tr Q8QFQ1 |
| CYP1C1_Scup | EALIQHST | TVAAANIMC | DP-EVTRDMS | TVTDLIGAGQDTVSTVMQ | AKLQELIDKVVGQDRLPSIE | VPVTIPHST | tr Q8QGR5 |
| CYP1C2_Scup | EALIQHST | TVAAANVIC | DP-EVTRDIS | TVSDLIGAGLDTVSTALH | TKLHELIDKVVGRQRLPSIE | VPVTIPHST | tr Q8QGR1 |
| CYP2V1_Zebrafish | KVLNDQGN | NNGVSNIIC | DP-SSPRDFI | AVLDLFVAGTETTSTTLL | EKVQAEIDKVVGRYRRPSMD | VPLSVPRMT | tr Q4L203 |
Sequence ID numbers at Expasy server (http://www.expasy.org/sprot/).
The insertion g.3318_3319insC (5′NC-487insC) in the 5′ noncoding region of the mRNA (exon 1) was found on all chromosomes of the 50 patients and 10 control individuals sequenced (Table 2). It is not represented in the CYP1B1 reference gene sequences. However, it is present in GenBank sequence gb/U56438.1, suggesting that this variation is a polymorphism. Because no other sequence variation was found in the chromosomes of the 50 patients sequenced, this exon was not investigated in the remaining patients. Exon 1 of CYP1B1 has not been extensively investigated in other PCG studies probably because of the absence of mutations in that region. Only one sequence variation in exon 1 (g.3130C>T) has been previously reported as a possible PCG-causing mutation.25 Q109R and I399V produce conservative amino acid alterations. Furthermore, arginine is found at the position corresponding to amino acid 109 in 15 of 34 aligned cytochrome P450 proteins, and valine is found at the position corresponding to amino acid 399 in one of the aligned proteins (Table 4). I399S was reported as a disease-causing alteration in a French PCG patient.22 However, serine does not occur at this position in any of the cytochromes sequenced, and this change causes the substitution of a polar amino acid for a nonpolar one. The g.4612C>T variation changes codon AGC to AGT, both of which code serine at position 269. The variation was found in only one control individual, and it is therefore considered a synonymous variation not associated with disease.
Available phenotypic features of patients carrying novel and non-novel mutations associated with PCG are described in Tables 5 and 6, respectively. Among patients carrying homozygous mutations, available data suggest that those with E229K, R368H, and T404fs had the most severe phenotypes. Among compound heterozygous patients, the A202D/G61E, R368C/E229K, and M503fs/G61E genotypes were associated with notably severe phenotypes. The affects of the novel missense mutations on the three-dimensional model of CYP1B1 protein constructed using homology modeling was assessed with the WHATIF structure analysis software program (http://swift.cmbi.kun.nl/WIWWWI/). The alterations had no notable affect on H-bonding or surface accessibility parameters (not shown). The templates used for model construction had at least 70% sequence similarity with CYP1B1, and the model constructed had an RMSD value of at least 0.74 Å as compared with the known structure of each of the templates.
Table 5.
Phenotype of PCG Patients with Novel CYP1B1 Mutations
| Mutation | Hom/Cpd Het | Fam/Sp* | Age of onset | Effected eye | C/D ratio R/L | Corneal opacity† R/L | Edema R/L | Megalo-cornea‡ R/L | Haab’s striaie§ | IOP Max (mm Hg) R/L | Surgery (trabec-ulotomy) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| G61fs | Hom | F | Birth | Bilateral | ++/++ | +/+ | 28/28 | Multiple | |||
| Y81X | Hom | F | Birth | Bilateral | ++/++ | +/+ | +/+ | + | 3× | ||
| A202D | Het(2nd mut G61E) | S | 6 months | Bilateral | En/0.6 | En/− | +/+ | En/ | En/36 | Multiple | |
| N265ins SNL | Hom | ? | Bilateral | 0.6/0.6 | ++/++ | +/+ | /+ | 30/30 | |||
| D291G | Hom | F | Birth | Bilateral | ++/++ | +/+ | +/+ | + | 28/26 | 1× | |
| G329V | Het(2nd mut R368H) | ? | Birth | Bilateral | 0.5/0.6 | ++/++ | +/+ | 30/30 | 4× | ||
| G329V | Het(2nd mut G61E) | F | Birth | Bilateral | 0.5/0.6 | ++/++ | +/+ | 28/30 | |||
| R366fs | Hom | F | <1 year | Left | 0.35/0.9 | −/− | +/+ | 17/30 | 1× | ||
| R368C | Hom | F | 3 days | Bilateral | 0.6/0.5 | +/+ | +/+ | +/+ | + | 1× | |
| R368C | Het(2nd mut E229K) | F | 5 months | Right | 0.4/0.6 | +/+ | +/+ | 40/12 | |||
| M503fs | Het(2nd mut G61E) | F | Birth | Bilateral | ++/++ | +/+ | 27/35 | Multiple | |||
| S506fs | Hom | F | 7 months | Bilateral | ++/++ | +/+ | +/+ | − | 28/28 | Multiple |
Unknown phenotypic features are left blank.
Familial/sporadic status of patients: F, familial; S, sporadic; ?, unknown.
++, very hazy; +, moderately hazy; −, clear.
Corneal diameter >12 mm.
Indicative of rupture of Descemet’s membrane.
Hom, homozygous; Cpd Het, compound heterozygous; C/D ratio, cup/disc ratio of optic nerve; En, enucleated; R, right eye; L, left eye.
Table 6.
Phenotype of PCG Patients with Non-Novel CYP1B1 Mutations
| Mutation | Hom/Cpd Het* | Fam/Sp† | Age of onset | Effected eye | C/D ratio‡ | Corneal opacity§ | Edema§ | Megalocor-nea§¶ | Haab’s striaie§∥ | IOP Max‡ (mm Hg) | Surgery (trabec-ulotomy) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| G61E | Hom;15 | 10/4/1 | 9:birth; 1:7 days; 2:6 months | 11:bilat; 1:R;1:L | 0.49 | 4:++;4:+;6:− | 8+;6- | All + | 10:+; 6:− | 29.1 | |
| G61E | Het(2nd mut R368H);3 | 1/2/0 | 2:birth; 1:3 years | 3:bilateral | 0.48 | 2:++;2:− | 2:+,2:− | 4:+;2:− | 6:+ | 23.2 | |
| G61E | Het(2nd mut R390H);4 | 0/4/0 | 3:birth; 1:3 years | 4:bilateral | 0.65 | All + | 2:+ | 30.0 | |||
| G61E | Het(2nd mut T404fs);1 | 1/0/0 | Birth | Bilateral | 0.30 | 1:++; 1:+ | 2:+ | 2:− | 22.0 | 2× | |
| G61E | Het(2nd mut P422R);1 | 0/1/0 | Birth | Bilateral | 2:+ | 1× | |||||
| G61E | Het(2nd mut R469W);2 | 2/0/0 | 1:2 months; 1:4 months | 2:bilateral | |||||||
| G61E | Het(2nd mut not found);1 | 0/1/0 | Birth | Right | 0.50 | 1:+ | 1:+ | 27.0 | 2× | ||
| E173K | Hom;2 | 1/1/0 | 1:birth;1:8 days | 1:bilat;1:R | 0.30 | 3:+ | 3:+ | 1:+;3:− | 24.0 | ||
| E299K | Hom;1 | 1/0/0 | Bilateral | 2:+ | 2:+ | 4:+ | 2:+ | 32.5 | |||
| R290fs | Hom;2 | 2/0/0 | 1 birth;1:7 months | ||||||||
| R368H | Hom;2 | 2/0/0 | 1:birth;1:2 years | 1:bilat;1:R | 0.87 | 2:+;2:− | 2:+;2:− | 3:+ | 2:− | 29.7 | |
| R368H | Het(2nd mut R390H);2 | 2/0/0 | 1:birth;1:4 months | 2:bilateral | 0.7 | 4:− | 4:− | 4:+ | 2:− | 24.8 | |
| R368H | Het(2nd mut not found);3 | 0/3/0 | 1:birth;1:4 months 1:1 year | 3:bilateral | 0.58 | 2:− | 2:− | 2:− | 2:+;4:− | 25.0 | |
| R390H | Hom;12 | 9/2/1 | 5:birth;1:6 days. 2:3–5 months | 12:bilat | 0.65 | 3++;6:+; 1:− | 7:+; 3:− | 16:+; 8:− | 6:+;4:− | 29.1 | |
| R390H | Het(2nd mut not found);1 | 0/1/0 | Birth | Bilateral | 27.0 | Multiple | |||||
| T404fs | Hom;1 | 1/0/0 | Birth | Bilateral | 0.70 | 1:++;1:− | 1:+;1:− | 2:+ | 2:− | 31.5 | 2× |
| R469W | Hom;7 | 6/0/1 | 2:birth; 1:2 months; 1:1 year | 7:bilateral | 0.60 | 2:++;1:+;4:− | 3:+;3:− | 8:+ | 4:+;4:− | 30.0 | |
| No CYP1B1 mut | 32 | 16/13/3 | 8:birth; 14:1–6 months; 4:7–12 months | 20:bilat; 2:R;4:L | 0.59 | 2:++;13:+;11:− | 15:+; 11:− | 41:+;5:− | 36:+; 18:− | 22.9 |
Number after semicolon indicates no. of patients; each heterozygote listed only once.
Familial/sporadic status of patients: no. familial/no. sporadic/no. unknown status.
Average of all eyes.
Numbers indicate no. of eyes.
Corneal diameter >12 mm.
Indicative of rupture of Descemet’s membrane.
CYP1B1 Mutation Frequency and Haplotype Analysis
Putative disease-causing mutations were identified in 139 of the 208 chromosomes investigated, indicating a CYP1B1 mutation allele frequency of 66.8% among the Iranian PCG patients (Table 1). Nineteen different mutations were found in 72 patients, and no CYP1B1 mutation was found in 32 of the PCG patients. The large proportion of the Iranian PCG patients carrying homozygous mutations in the CYP1B1 gene (49 of 72) is indicative of extensive consanguineous marriages in this population.38 If we assume the CYP1B1 mutation found in the few patients in whom only one mutation was identified had a role in their disease status, then CYP1B1 is the cause of disease in 69.2% of Iranian PCG patients.
Among the 47 probands of familial status with CYP1B1 mutations, nine carried two different mutations (compound heterozygotes), and the rest were homozygous. In one of the homozygous patients, the two identical mutations were carried on different SNP haplotypes, suggesting independent origins. (The intragenic SNP haplotypes identified among the Iranians are presented in Table 7.) Therefore, the disease status of 21% (10 of 47) of the probands of familial cases was not attributable to identity by descent. This signifies a correspondingly high frequency of mutated CYP1B1 alleles in the Iranian population.
Table 7.
CYP1B1 Haplotype Frequencies of Iranian PCG Patients and Controls
| Haplotype | PCG patients with CYP1B1 mutations (n = 72)
|
PCG patients without CYP1B1 mutations (n = 32)
|
Controls (n = 99)
|
|||
|---|---|---|---|---|---|---|
| % | SD | % | SD | % | SD | |
| H1: CCGGTA | 62.5 | 0.10 | 20.3 | 0.13 | 26.0 | 2.18 |
| H2: TGTCCA | 25.3 | 0.34 | 29.7 | 0.03 | 31.8 | 2.37 |
| H3: CCGCCA | 8.7 | 0.34 | 17.2 | 0.13 | 24.8 | 3.05 |
| H4: CCGCCG | 3.5 | 0.0055 | 32.8 | 0.13 | 11.0 | 2.11 |
| H5: TGTCCG | 3.9 | 1.91 | ||||
| H6: TGTGTA | 1.4 | 1.13 | ||||
| Others (each <1%) | 1.1 | |||||
| Total | 100.0 | 100.0 | 100.0 | |||
No CYP1B1 mutation was found in 25% (16 of 63) of familial cases of PCG, whereas the corresponding figure for the sporadic cases was 39% (13 of 33). This difference is consistent with data from other populations wherein CYP1B1 was less often found to be causative of disease among sporadic as compared with familial cases.5,39 In Japan, where CYP1B1 was found to be causative for only 20% of PCG cases, all cases investigated were sporadic.25
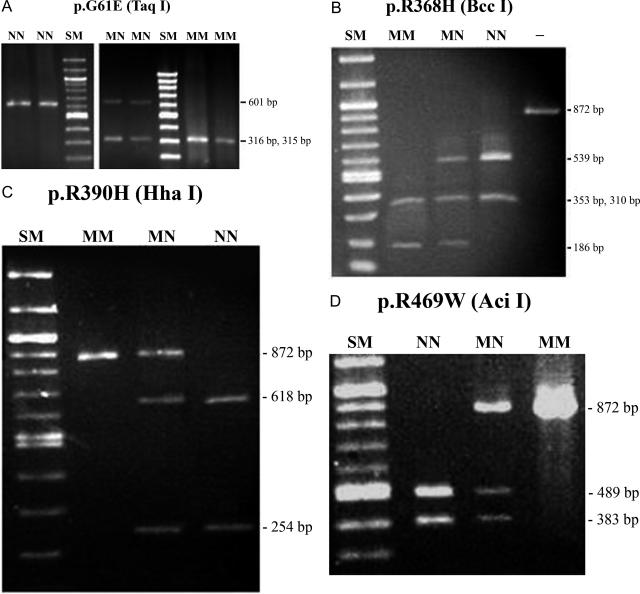
The g.3987G>A mutation, which produces G61E, was the most frequently mutated CYP1B1 allele among the Iranian PCG patients, found in 21.6% of the patients’ chromosomes examined and in 28.8% of the patients. The next most frequent mutations among the patients’ chromosomes were R390H (g.8006G>A), R469W (g.8242C>T), and R368H (g.7940G>A) found in 14.9, 7.7, and 6.3% of patients, respectively. These four common mutations together constituted 50.5% of the PCG patients’ CYP1B1 alleles and 76.2% of the mutated CYP1B1 alleles found in the Iranian cohort. They were found in the homozygous or heterozygous state in 66.3% of the patients. The probable contribution of these four mutations to the disease status of the Iranian PCG patients and the clinical implications of this finding directed the design of simple RFLP assays for their detection (Figure 1). The remaining 15 putative disease-causing mutations were each detected in less than 2% of the chromosomes. Six mutations were found in two patients and nine in only one.
Figure 1.
RFLP electrophoresis patterns of common CYP1B1 mutations of Iranian PCG patients. A: g.3987G>A; B: g.7940G>A; C: g.8006G>A; D: g.8242C>T. SM, size markers; NN, homozygous normal; MM, homozygous mutant; MN, heterozygous; −, undigested PCR product. PCR amplicon of exon 2 (primers 2aF and 2aR) was digested for detection of mutation G61E and PCR amplicon of exon 3 for detection of the other three common mutations. TaqI digestion of normal and G61E mutated exon 2 amplicons produces 70- and 75-bp fragments that migrate out of the gel. Likewise, BccI digestion of normal and R368H mutated exon 3 amplicons produces a 23-bp fragment that also migrates out of the gel.
Haplotypes based on six intragenic SNPs, four of which have been extensively reported in other studies, were constructed for Iranian PCG patients with and without CYP1B1 mutations and controls. The six SNPs identified in this population were g.3793T>C, g.3947C>G (R48G), g.4160G>T (A119S), g.8131G>C (V432L), g.8184T>C (D449D), and g.8195A>G (N453S) (Table 2). The genotypes of a majority of the patients carrying CYP1B1 mutations (54 of 72) were homozygous at all six SNP loci, allowing unambiguous haplotype description. The majority of the heterozygotes were those carrying either the R368H (10 of 18) or R390H (7 of 18) mutations. However, the PCG patients without CYP1B1 mutations and the control individuals were mostly heterozygous at two or more of these six SNP loci, and the PHASE 2 software was essential for haplotype analysis in these individuals.
Four haplotypes were found among patients with CYP1B1 mutations and also among patients without CYP1B1 mutations. These same haplotypes and several additional minor haplotypes were predicted in the controls. The four frequent haplotypes were H1, -CCGGTA-; H2, -TGTCCA-; H3, -CCGCCA-; and H4, -CCGCCG-. The only other haplotypes that reached a frequency of larger than 1% in the control group were H5, -TGTCCG- (3.9%), and H6, -TGTGTA- (1.4%). Estimated frequency distributions of these haplotypes are presented in Table 7. The frequency distributions of the haplotypes are significantly different between PCG patients with and without CYP1B1 mutations (P < 0.001) and between patients with CYP1B1 mutations and controls (P < 0.001). By far the most common (62%) haplotype among patients with CYP1B1 mutations was H1 (-CCGGTA-). This haplotype was associated with all patients carrying three of the four most common CYP1B1 mutations (G61E, R368H, and R469W) among the Iranian PCG patients, and these patients made a large contribution to the total frequency of the haplotype (Table 8). H1 was predicted for ∼25% of the chromosomes of the Iranian control individuals. It is interesting that the haplotype distribution between PCG patients without CYP1B1 mutations and controls were also found to be significantly different (P < 0.01). The most notable difference relates to haplotype H4 (-CCGCCG-), the frequency of which is approximately three times lower in the control group (11.0 versus 32.8%).
Table 8.
CYP1B1 Haplotypes Associated with CYP1B1 Mutations in PCG Patients
| Country | Mutation | g.3987G>A (p.G61E) | g.3988delA (p.G61fs) | g.4048C>A (p.Y81X) | g.4322G>A (p.E173K) | g.4410C>A (p.A202D) | g.4490G>A (p.E229K) | g.4611_4619dup9bp (p.N265_R266insSNL) | g 4673_4674insC (p.R290fs) | g.4677A>G (p.D291G) | g.4791G>T (p.G329V) | g.7934delG (p.R366fs) | g.7939C>T (p.R368C) | g.7940G>A (p.R368H) | g.8006G>A (p.R390H) | g.8037_8046dup10bp (p.T404fs) | g.8162C>G (p.P442R) | g.8242C>T (p.R469W) | g.8341delA (p.M503fs) | g.8354_8373del20 (p.S506fs) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Iran | 1 | 2 | 1 | 2 | 3 | 2 | 3 | 1 | 4 | 1 | 1 | 4 | 1 | 1,2,3 | 1 | 2 | 1 | 2 | 1 | |
| (Present study) | ||||||||||||||||||||
| Saudi Arabia | 1 | 1 | ||||||||||||||||||
| (Bejjani et al, 2000) | ||||||||||||||||||||
| Ecuador | 1 | |||||||||||||||||||
| (Curry et al, 2004) | ||||||||||||||||||||
| India | 1 | 2,6 | 1,2 | 1 | ||||||||||||||||
| (Chakrabarti et al, 2006) | ||||||||||||||||||||
| Morocco | 1 | 1 | ||||||||||||||||||
| (Belmouden et al, 2002) | ||||||||||||||||||||
| Brazil | 1 | 1 | ||||||||||||||||||
| (Stoilov et al, 2002) |
Haplotypes are designated as follows: 1, (C) CGGTA; 2, (T) GTCCA; 3, (C) CGCCA; 4, (C) CGCCG; 6, -_GTGTA-.
Among the patients, it is apparent that the core haplotypes consist of three blocks with members that consistently co-segregate. The three blocks consist of g.3793T>C, g.3947C>G (R48G), g.4160G>T (A119S); g.8131G>C (V432L), g.8184T>C (D449D); and g.8195A>G (N453S). The same pattern was observed in the predicted genotypes of the vast majority of control individuals (Table 7). The frequency distributions of the blocks between PCG patients with CYP1B1 mutations and controls are compared in Table 9. The difference in distributions of the first block is not significantly different between the two groups (P = 0.25). However, the difference in distributions of the second and third blocks are significantly different (P < 0.001 and P = 0.01, respectively). The existence of the blocks reflects nucleotide substitution and recombination events during human history, but differences in their frequencies among the groups need to be considered (see the last paragraph of Discussion).
Table 9.
Comparison of Distribution of Blocks within CYP1B1 Core Haplotypes between PCG Patients with CYP1B1 Mutations and Control Individuals
| Block 1
|
Block 2
|
Block 3
|
||||
|---|---|---|---|---|---|---|
| TGT | CCG | GT | CC | A | G | |
| PCG patients with CYP1B1 mutation, n = 144* | 36 | 108 | 90 | 54 | 139 | 5 |
| Controls, n = 198* | 75 | 123 | 51 | 147 | 173 | 25 |
| P | 0.25 | <0.001 | 0.01 | |||
Blocks are defined in text.
Number of alleles.
Table 8 presents the haplotype background of CYP1B1 mutations found among the Iranian PCG patients. For mutations among these that have been previously reported in other populations, Table 8 also shows associated haplotypes in those populations. As recently reported, the mutations are clustered on the background of the H1 haplotype (-CCGGTA- or _CGGTA-).26 Most mutations are found on the same haplotype in patients from different countries, suggesting a common origin. For two of the mutations that are associated with multiple haplotypes (R368H and R390H), interchange between the haplotypes of each would require more than one mutation or recombination event. This suggests that these are recurrent mutations without common ancestry. The observation that a high proportion of patients carrying these mutations are compound heterozygotes and are sporadic is consistent with this proposal (Tables 1and 6). The two haplotypes H1 (-CGGTA-) and H2 (-GTCCA-), associated with R368H and R390H, have been proposed to be ancient human haplotypes.26 Interchange between two haplotypes associated with E229K could have resulted from a single recombination event between one of these (H2: -TGTCCA-) and the common haplotype H1 (-CCGGTA-). There was no notable difference in the phenotypes of patients carrying the same mutation on different haplotype backgrounds.
Discussion
Considerable sequence heterogeneity was observed in the CYP1B1 gene among the Iranian PCG patients. High sequence heterogeneity in the CFTR gene of cystic fibrosis patients from this population has also been reported.40 Ten novel mutations were identified, making a notable contribution to the previously reported mutations. This is important because mutations constitute a tool for understanding the biochemical and physiological role of CYP1B1 in the PCG phenotype. It is possible that some mutations were not detected because of the sequencing strategy used. Variations outside the regions of the gene sequenced and large heterozygous deletions would have been missed. Nevertheless, nearly 70% of the Iranian PCG patients carried CYP1B1 mutations, signifying the clinical importance of this gene. This figure is lower than the corresponding figure for the more homogeneous and inbred populations of Slovakia Roma and Saudi Arabia (∼100%). However, it is higher than the corresponding figure for the populations of Brazil and France (∼50%) and of the heterogeneous population of India (∼40%). The four most common mutations detected among the Iranians were p.G61E, p.R390H, p.R469W, and p.R368H. These together constituted 51% of the Iranian CYP1B1 alleles studied and 76.2% of the mutated CYP1B1 alleles observed.
Our results are consistent with a geographic distribution of CYP1B1 mutations. Two mutated alleles, g.8037_8046dupTCATGCCACC and g.4611_4619delGCAACTTCA (S269_F271del), have been proposed to be ancient on the basis of haplotype analysis and, therefore, are expected to be spread widely; however, only the first was found among the Iranian patients.41 The second mutation represents deletion of one copy of a 9-bp repeat in the wild-type nucleotide sequence. A further duplication of the repeat was identified as a novel mutation (N265_R266insSNL) among the Iranian patients, suggesting that this may be a mutational hotspot. G61E, the most frequent (∼75%) mutant allele among PCG patients of Saudi Arabia, was also the most frequent (21.6%) one among the Iranian patients, although at a significantly lower frequency. The second most common mutation among the Saudi Arabians (R469W) was also one of the common mutations among the Iranian patients.6 Both mutations occurred on the same haplotype background in the two populations, thus suggesting a common ancestral origin.
R368H has been observed in significant numbers of patients only in India (17%) and is the most common CYP1B1 mutation in that population.23,34 It is also one of the most common mutations in Iran, found in 11.5% of the PCG patients. Again, the haplotype background of this mutation in the two populations is the same. R390H, another common mutation found in 19.2% of the PCG patients in Iran, was first identified in a Pakistani patient42 and subsequently reported in Indian PCG patients23 and in an early-onset primary open angle glaucoma French patient.29 E173K, among the more infrequent mutations in the Iranians, was only recently reported as a novel mutation in an Egyptian family,43 and g.4673_4674insC was previously found in a Turkish pedigree.14 In contrast, most of the mutations of patients from the American continents and Western Europe were not observed among the Iranians.41,42 An exception is the E229K mutation, which was reported to be a possible dominant cause of PCG and early-onset primary open angle glaucoma in French patients.22,29 However, of the two Iranian patients who carried this mutation, one was homozygous and the other also carried a second mutation. The mutations found in patients from Japan and Indonesia seem to be unique to the Far East and have not been reported elsewhere; they were also not found in Iran.27,36,44,45
Four core haplotypes defined by six common intragenic SNPs, five of which are coding SNPs, were found among patients with CYP1B1 mutations and among patients without mutations as well as unaffected controls. The frequency distributions of the haplotypes were significantly different among the groups, with the greatest difference being between the PCG patients with and without CYP1B1 mutations. The most common haplotype segregating with the mutated alleles was H1 (-CCGGTA-), as has been reported for other populations. The frequency of this haplotype was estimated at 35% in a Saudi Arabian control cohort under the assumption of Hardy-Weinberg equilibrium.6 The haplotype has a similar frequency among Iranian controls (26%). The haplotype distribution in the Iranian CYP1B1 mutation group was strikingly similar to that recently reported for the corresponding group of patients from India.26 The exception was H6 (-_GTGTA-) associated with some E229K alleles among the Indian population and absent among the Iranian patients. The difference in frequency distributions between patients without CYP1B1 mutations and controls may be attributable to the concentration of the patients without CYP1B1 mutations within a geographic or ethnic subpopulation not well represented by the controls. Less likely possibilities are that the PCG phenotype in a fraction of these patients is attributable to mutations in parts of the CYP1B1 gene that were not sequenced, long-range deletions in CYP1B1, or mutations in a gene proximal to CYP1B1.
Considering the different mutations individually, haplotype analysis suggests a common origin for most of the mutations. The two mutations R368H and R390H may have occurred more than once during the human evolution. Our data are consistent with the parsimonious scenario of evolution of various CYP1B1 haplotypes proposed for the human population.26 It expands on that scenario by extending the length of each of the two proposed ancestral haplotypes by one nucleotide (H1: -CGGTA- to -CCGGTA- and H2: -GTCCA- to -TGTCCA-). It is interesting that descendants of one of the chromosome products (-_GTGTA-) of the proposed recombination event between the ancestral haplotypes is rare both among the PCG patients and the control populations studied. The two proposed ancestral haplotypes have become diluted through human history by mutation and recombination events, and their frequency in the normal population is now comparable with that of two other haplotypes, H3 (-_CGCCA-) and H4 (-_CGCCG-). The finding of most common PCG-causing mutations on the proposed ancestral haplotypes despite their dilution suggests that they are ancient mutations. The more rare mutations often found on haplotypes H3 (-_CGCCA-) and H4 (-_CGCCG-), probably occurred more recently.
Finally, it is evident that the difference in core haplotype distributions between PCG patients with CYP1B1 mutations and control individuals is almost entirely attributable to differences in distributions of blocks 2 (consisting of V432L and D449D) and 3 (N453S) therein (Table 9). The two alleles at position 432 and the two alleles at position 453 have been reported to code for proteins that differ in enzymatic activity or stability.18,46 Furthermore, the alleles with higher enzymatic activity or stability (V432, N453) have been found in higher frequencies in patients afflicted with various forms of cancers as compared with normal controls.19,20,47,48 These same alleles were found to be more frequent in the Iranian cohort of PCG patients with CYP1B1 mutations as compared with control individuals used in this study (Table 9). For example, the frequencies of the V432 allele in these two groups were 62.5 and 25.8%, respectively. The corresponding numbers for N453 were 96.5 and 87.4%. From an evolutionary perspective, these data are consistent with the proposition that maintenance of PCG-causing mutations, which generally disrupt protein function, may partly serve to compensate for cancer-promoting alterations in the gene sequences.
Acknowledgments
We thank all of the patients and their families for consenting to participate in this study.
Footnotes
Supported by the National Institute for Genetic Engineering and Biotechnology, Tehran, Iran (grant 231).
F.C. and B.K.T. contributed equally to this article.
References
- Sarfarazi M. Recent advances in molecular genetics of glaucomas. Hum Mol Genet. 1997;6:1667–1677. doi: 10.1093/hmg/6.10.1667. [DOI] [PubMed] [Google Scholar]
- Ray K, Mukhopadhyay A, Acharya M. Recent advances in molecular genetics of glaucoma. Mol Cell Biochem. 2003;253:223–231. doi: 10.1023/a:1026059800470. [DOI] [PubMed] [Google Scholar]
- Farkas RH, Grosskreutz CL. Apoptosis, neuroprotection, and retinal ganglion cell death: an overview. Int Ophthalmol Clin. 2001;41:111–130. doi: 10.1097/00004397-200101000-00011. [DOI] [PubMed] [Google Scholar]
- Thylefors B, Negrel AD. The global impact of glaucoma. Bull World Health Organ. 1994;72:323–326. [PMC free article] [PubMed] [Google Scholar]
- Sarfarazi M, Stoilov I, Schenkman JB. Genetics and biochemistry of primary congenital glaucoma. Ophthalmol Clin North Am. 2003;16:543–554. doi: 10.1016/s0896-1549(03)00062-2. [DOI] [PubMed] [Google Scholar]
- Bejjani BA, Stockton DW, Lewis RA, Tomey KF, Dueker DK, Jabak M, Astle WF, Lupski JR. Multiple CYP1B1 mutations and incomplete penetrance in an inbred population segregating primary congenital glaucoma suggest frequent de novo events and a dominant modifier locus. Hum Mol Genet. 2000;9:367–374. doi: 10.1093/hmg/9.3.367. [DOI] [PubMed] [Google Scholar]
- Hewitt AW, Mackinnon JR, Elder JE, Giubilato A, Craig JE, Mackey DA. Familial transmission patterns of infantile glaucoma in Australia (abstract). Invest Ophthalmol Vis Sci. 2005;46:E3207. [Google Scholar]
- Dandona L, Williams JD, Williams BC, Rao GN. Population-based assessment of childhood blindness in southern India. Arch Ophthalmol. 1998;116:545–546. [PubMed] [Google Scholar]
- Plásilová M, Stoilov I, Sarfarazi M, Kadasi L, Ferakova E, Ferak V. Identification of a single ancestral CYP1B1 mutation in Slovak Gypsies (Roms) affected with primary congenital glaucoma. J Med Genet. 1999;36:290–294. [PMC free article] [PubMed] [Google Scholar]
- Levy J, Tessler Z, Tamir O, Lifshitz T. Primary congenital glaucoma. Harefuah. 2004;143:876–910. [PubMed] [Google Scholar]
- Sarfarazi M, Akarsu AN, Hossain A, Turacli ME, Aktan SG, Barsoum-Homsy M, Chevrette L, Sayli BS. Assignment of a locus (GLC3A) for primary congenital glaucoma (Buphthalmos) to 2p21 and evidence for genetic heterogeneity. Genomics. 1995;30:171–177. doi: 10.1006/geno.1995.9888. [DOI] [PubMed] [Google Scholar]
- Akarsu AN, Turacli ME, Aktan SG, Barsoum-Homsy M, Chevrette L, Sayli BS, Sarfarazi M. A second locus (GLC3B) for primary congenital glaucoma (Buphthalmos) maps to the 1p36 region. Hum Mol Genet. 1996;5:1199–1203. doi: 10.1093/hmg/5.8.1199. [DOI] [PubMed] [Google Scholar]
- Sarfarazi M, Stoilov I: The third genetic locus (GLC3C) for primary congenital glaucoma (PCG) maps to chromosome 14q24.3. Presented at the ARVO Annual Meeting, 2002 May 5–10, Fort Lauderdale, FL [Google Scholar]
- Stoilov I, Akarsu AN, Sarfarazi M. identification of three different truncating mutations in cytochrome P4501B1 (CYP1B1) as the principal cause of primary congenital glaucoma (Buphthalmos) in families linked to the GLC3A locus on chromosome 2p21. Hum Mol Genet. 1997;6:641–647. doi: 10.1093/hmg/6.4.641. [DOI] [PubMed] [Google Scholar]
- Nebert DW, Russell DW. Clinical importance of the cytochromes P450. Lancet. 2002;360:1155–1162. doi: 10.1016/S0140-6736(02)11203-7. [DOI] [PubMed] [Google Scholar]
- Stoilov I, Jansson I, Sarfarazi M, Schenkman JB. Roles of cytochrome P450 in development. Drug Metabol Drug Interact. 2001;18:33–55. doi: 10.1515/dmdi.2001.18.1.33. [DOI] [PubMed] [Google Scholar]
- Bejjani BA, Xu L, Armstrong D, Lupski JR, Reneker LW. Expression patterns of cytochrome P4501B1 (Cyp1b1) in FVB/N mouse eyes. Exp Eye Res. 2002;75:249–257. [PubMed] [Google Scholar]
- Bandiera S, Weidlich S, Harth V, Broede P, Ko Y, Friedberg T. Proteasomal degradation of human CYP1B1: effect of the Asn453Ser polymorphism on the post-translational regulation of CYP1B1 expression. Mol Pharmacol. 2005;67:435–443. doi: 10.1124/mol.104.006056. [DOI] [PubMed] [Google Scholar]
- Guengerich PF, Chun YJ, Kim D, Gillam EM, Shimada T. Cytochrome P450 1B1: a target for inhibition in anticarcinogenesis strategies. Mutat Res. 2003;523–524:173–182. doi: 10.1016/s0027-5107(02)00333-0. [DOI] [PubMed] [Google Scholar]
- Ko Y, Abel J, Harth V, Bröde P, Antony C, Donat S, Fischer HP, Ortiz-Pallardo ME, Their R, Sachinidis A, Vetter H, Bolt HM, Herberhold C, Brüning C. Association of CYP1B1 codon 432 mutant allele in head and neck squamous cell cancer is reflected by somatic mutations of p53 in tumor tissue. Cancer Res. 2001;61:4398–4404. [PubMed] [Google Scholar]
- Stoilov IR, Costa VP, Vasconcellose PC, Melo MB, Betinjane AJ, Carani JCE, Oltrogge EV, Sarfarazi M. Molecular genetics of primary congenital glaucoma in Brazil. Invest Ophthalmol Vis Sci. 2002;43:1820–1827. [PubMed] [Google Scholar]
- Colomb E, Kaplan J, Garchon1 H-J. Novel cytochrome P450 1B1 (CYP1B1) mutations in patients with primary congenital glaucoma in France. Hum Mutat. 2003;22:496. doi: 10.1002/humu.9197. [DOI] [PubMed] [Google Scholar]
- Reddy ABM, Kaur K, Mandal AK, Panicker SG, Thomas R, Hasnain SE, Balasubramanian D, Chakrabarti S. Mutation spectrum of the CYP1B1 gene in Indian primary congenital glaucoma patients. Mol Vis. 2004;10:696–702. [PubMed] [Google Scholar]
- Belmouden A, Melki R, Hamdani M, Zaghloul K, Amraoui A, Nadifi S, Akhayat O, Garchon HJR. A novel frameshift founder mutation in the cytochrome P450 1B1 (CYP1B1) gene is associated with primary congenital glaucoma in Morocco. Clin Genet. 2002;62:334–339. doi: 10.1034/j.1399-0004.2002.620415.x. [DOI] [PubMed] [Google Scholar]
- Mashima Y, Suzuki Y, Sergeev Y, Ohtake Y, Tanino T, Kimura I, Miyata H, Aihara M, Tanihara H, Inatani M, Azuma N, Iwata T, Araie M. Novel cytochrome P4501B1 (CYP1B1) gene mutations in Japanese patients with primary congenital glaucoma. Invest Ophthalmol Vis Sci. 2001;42:2211–2216. [PubMed] [Google Scholar]
- Chakrabarti S, Kaur K, Kaur I, Mandal AK, Parikh RS, Thomas R, Majumder PP. Globally, CYP1B1 mutations in primary congenital glaucoma are strongly structured by geographic and haplotype backgrounds. Invest Ophthalmol Vis Sci. 2006;47:43–47. doi: 10.1167/iovs.05-0912. [DOI] [PubMed] [Google Scholar]
- Sitorus R, Ardjo SM, Lorenz B, Preising M. CYP1B1 gene analysis in primary congenital glaucoma in Indonesian and European patients. J Med Genet. 2003;40:e9. doi: 10.1136/jmg.40.1.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bejjani BA, Lewis RA, Tomey KF, Anderson KL, Dueker DK, Jabak M, Astle WF, Otterud B, Leppert M, Lupski JR. Mutations in CYP1B1, the gene for cytochrome P4501B1, are the predominant cause of primary congenital glaucoma in Saudi Arabia. Am J Hum Genet. 1998;62:325–333. doi: 10.1086/301725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melki R, Colomb E, Lefort N, Brezin AP, Garchon H-J. CYP1B1 mutations in French patients with early-onset primary open-angle glaucoma. J Med Genet. 2004;41:647–651. doi: 10.1136/jmg.2004.020024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens M, Smith NJ, Donnelly P. A new statistical method for haplotype reconstruction from population data. Am J Hum Genet. 2001;68:978–989. doi: 10.1086/319501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens M, Donnelly P. A comparison of Bayesian methods for haplotype reconstruction from population genotype data. Am J Hum Genet. 2003;73:1162–1169. doi: 10.1086/379378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheet P, Stephens M. A fast and flexible statistical model for large-scale population genotype data: applications to inferring missing genotypes and haplotypic phase. Am J Hum Genet. 2006;78:629–644. doi: 10.1086/502802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage P, Berry G. Statistical Methods in Medical Research. Boston: Blackwell Scientific Publications,; 1987:371–378. [Google Scholar]
- Panicker SG, Reddy ABM, Mandal AK, Ahmed N, Nagarajaram HA, Hasnain SE, Balasubramanian D. Identification of novel mutations causing familial primary congenital glaucoma in Indian pedigrees. Invest Ophthalmol Vis Sci. 2002;43:1358–1366. [PubMed] [Google Scholar]
- Panicker SG, Mandal AK, Reddy ABM, Gothwal VK, Hasnain SE. Correlations of genotype with phenotype in Indian patients with primary congenital glaucoma. Invest Ophthalmol Vis Sci. 2004;45:1149–1156. doi: 10.1167/iovs.03-0404. [DOI] [PubMed] [Google Scholar]
- Ohtake Y, Tanino T, Suzuki Y, Miyata H, Taomoto M, Azuma N, Tanihara H, Araie M, Mashima Y. Phenotype of cytochrome P4501B1 gene (CYP1B1) mutations in Japanese patients with primary congenital glaucoma. Br J Ophthalmol. 2003;87:302–304. doi: 10.1136/bjo.87.3.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent AL, Billingsley G, Buys Y, Levin AV, Priston M, Trope G, Williams-Lyn D, Héon E. Digenic inheritance of early-onset glaucoma: CYP1B1, a potential modifier gene. Am J Hum Genet. 2002;70:448–460. doi: 10.1086/338709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mani A, Meraji SM, Houshyar R, Radhakrishnan J, Mani A, Ahangar M, Rezaie TM, Taghavinejad MA, Broumand B, Zhao H, Nelson-Williams C, Lifton RP. Finding genetic contributions to sporadic disease: a recessive locus at 12q24 commonly contributes to patent ductus arteriosus. Proc Natl Acad Sci USA. 2002;99:15054–15059. doi: 10.1073/pnas.192582999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarfarazi M, Stoilov I. Molecular genetics of primary congenital glaucoma. Eye. 2000;14:422–428. doi: 10.1038/eye.2000.126. [DOI] [PubMed] [Google Scholar]
- Elahi E, Khodadad A, Kupershmidts I, Ghassemi F, Alinasab B, Eason RG, Amini M, Esmaiili M, Esmaiili MR, Sanati MH, Davis RW, Ronaghi M, Thorstenson YR. A haplotype framework for cystic fibrosis mutations in Iran. J Mol Diagn. 2006;8:119–127. doi: 10.2353/jmoldx.2006.050063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sena DF, Finzi S, Rodgers K, Del Bono E, Haines JL, Wiggs JL. Founder mutations of CYP1B1 gene in patients with congenital glaucoma from the United States and Brazil. J Med Genet. 2004;41:e6. doi: 10.1136/jmg.2003.010777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoilov I, Akarsu AN, Alozie I, Child A, Barsoum-Homsy M, Turacli ME, Or M, Lewis RA, Ozdemir N, Brice G, Aktan SG, Chevrette L, Coca-Prados M, Sarfarazi M. Sequence analysis and homology modeling suggest that primary congenital glaucoma on 2p21 results from mutations disrupting either the hinge region or the conserved core structures of cytochrome P4501B1. Am J Hum Genet. 1998;62:573–584. doi: 10.1086/301764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Ashry MF, Abd El-Aziz MM, Bhattacharya SS. Mutation screening of CYP1B1 gene in Egyptian and Saudi Arabian patients with primary congenital glaucoma: identification of a novel mutation. Invest Ophthalmol Vis Sci. 2005;46:E1096. [Google Scholar]
- Kakiuchi-Matsumoto T, Isashiki Y, Ohba N, Kimura K, Sonoda S, Unoki K. Cytochrome P450 1B1 gene mutations in Japanese patients with primary congenital glaucoma (1). Am J Ophthalmol. 2001;131:345–350. doi: 10.1016/s0002-9394(00)00808-4. [DOI] [PubMed] [Google Scholar]
- Ohtake Y, Kubota R, Tanino T, Miyata H, Mashima Y. Novel compound heterozygous mutations in the cytochrome P4501B1 gene (CYP1B1) in a Japanese patient with primary congenital glaucoma. Ophthalmic Genet. 2000;21:191–193. [PubMed] [Google Scholar]
- Wormhoudt LW, Commandeur JNN, Vermeulen NPE. Genetic polymorphisms of human N-acetyltransferase, cytochrome P450, glutathione S-transferase and epoxide hydrolyse enzymes: relevance to xenobiotic metabolism and toxicity. Crit Rev Toxicol. 1999;29:59–124. doi: 10.1080/10408449991349186. [DOI] [PubMed] [Google Scholar]
- Fritsche E, Bruning T, Jonkmanns C, Ko Y, Bolt HM, Abel J. Detection of cytochrome P4501B1 Bfr I polymorphism: genotype distribution in healthy German individuals and in patients with colorectal carcinoma. Pharmacogenetics. 1999;9:405–408. [PubMed] [Google Scholar]
- McGrath M, Hankinson SE, Arbeitman L, Colditz GA, Hunter DJ, De Vivo I. Cytochrome P450 1B1 and catechol-O-methyltransferase polymorphisms and endometrial cancer susceptibility. Carcinogenesis. 2004;25:559–565. doi: 10.1093/carcin/bgh039. [DOI] [PubMed] [Google Scholar]