Abstract
Multiple cystic fibrosis (CF) testing platforms, using diverse and rapidly evolving technologies, are available to clinical laboratories commercially or for evaluation. Considerations when choosing a CF platform may include: sensitivity, specificity, accuracy, signal discrimination, ability to genotype, ability to reflex test, no calls/repeat rate, composition of mutation panel, hands-on time, start-to-finish time, integration into laboratory workflow, data analysis methods, flexibility regarding custom test design, and required instrumentation. Mindful of these considerations, we evaluated five technologically diverse CF platforms: 1) eSensor, an electronic detection assay system; 2) InPlex, a signal amplification methodology using a microfluidics card; 3) oligonucleotide ligation assay, an electrophoretic-based separation of amplicon-derived ligation-generated products; and two liquid bead arrays; 4) Signature, a direct hybridization assay using allele-specific capture probes; and 5) Tag-It, an assay using allele-specific primer extension and a universal microarray. A core of 150 samples, focusing on mutations in the American College of Medical Genetics/American College of Obstetricians and Gynecologists mutation panel, was tested throughout several runs for each platform. All of the platforms performed comparably in respect to sensitivity, specificity, and no-call rate. As our results indicate, consideration of all of the parameters evaluated may be useful when selecting the most appropriate platform for the specific setting.
Cystic fibrosis (CF), caused by mutations in the cystic fibrosis transmembrane conductance regulator gene (CFTR), is one of the most common autosomal recessive diseases in the North American Caucasian population with an incidence of 1 in 2500 to 3300 live births.1,2,3,4 The carrier frequency in non-Hispanic Caucasians is ∼1 in 25 to 30, in individuals of Ashkenazi Jewish descent 1 in 29, in Hispanics 1 in 46, in Africans 1 in 65, and in Asians 1 in 90.5,6,7 In 2001, the American College of Medical Genetics (ACMG) and the American College of Obstetricians and Gynecologists (ACOG) recommended that CF carrier screening be offered to reproductive couples.6 Of the 1300 CFTR sequence variants identified (http://www.genet.sickkids.on.ca), a screening panel of 25 CFTR mutations was initially selected based on inclusion criterion of mutations having a threshold of 0.1% frequency in the general US population.8 In addition, they recommended reflex testing for R117H of the 5/7/9T polymorphic alleles in intron 8, as well as reflex testing for individuals homozygous for ΔF508, ie, testing for interference from benign variants I506V, I507V, and F508C. This panel was modified in 2004 and currently includes 23 CFTR mutations as well as the R117H and ΔF508 reflex tests.7 Using this panel, the resulting carrier detection rate, for Ashkenazi Jews, Northern European Caucasians, Hispanics, African Americans, and Asians is 94 to 97%, 90%, 72%, 64 to 69%, and 49%, respectively.6,7,8 Frequency and ethnic distribution of additional CFTR mutations in the US population, with prevalence of <0.1%, that may be of interest to clinical laboratories are described by Heim and colleagues.9
The ACMG and ACOG recommendations prompted an increase in CF testing and concomitant stimulation of development of multiple CF testing reagents and systems. In addition, as of 2004, eight states were using newborn screening programs in which DNA analysis to detect specific CFTR mutation followed an elevated immunoreactive trypsinogen test.10 The CF testing options available to clinical laboratories commercially or for evaluation are as diverse as the rapidly evolving technologies used to create them. In 2003, Tomaiuolo and colleagues11 evaluated (accuracy, time, cost) the following four procedures for molecular diagnosis of CF: allele-specific oligonucleotide dot-blot (homebrew), reverse dot-blot (Innogenetics, Gent, Belgium), amplification refractory mutation system (ARMS) (Zeneca Diagnostics, Oxfordshire, UK), and oligonucleotide ligation assay (OLA)-polymerase chain reaction (PCR) (PE Applied Biosystems, Foster City, CA). Recently, a time-motion analysis of six commercially available CF testing platforms was performed by Krafft and Lichy on CF v3 OLA analyte-specific reagent (ASR) (Abbott Laboratories/Celera Diagnostics, Abbott Park, IL), INNO-LiPA CFTR 35 (Innogenetics: INNO-LiPA), CF Gold 1.0 (Roche, Indianapolis, IN), Tag-It CF 40 + 4 (Tm Biosciences, Toronto, ON, Canada), CF eMAP/Bead Chip (BioArray Solutions, Warren, NJ), and Invader (Third Wave Technology, Madison, WI).12 Several platforms have been evaluated individually as well: Tag-It CF 40 + 4 (Tm Biosciences) by Amos and colleagues13; Signature (Asuragen, Austin, TX) by Hadd and colleagues14; CF eMAP/BeadChip (BioArray Solutions) by Edelmann and colleagues15; and CF APEX DNA microarray chip by Schrijver and colleagues.16 The bases of many of the CFTR testing technologies have been reviewed as well.17,18,19
Here, we report a comparative study of five technologically diverse CFTR testing platforms: 1) eSensor CF carrier detection system (Osmetech Molecular Diagnostics, Pasadena, CA); 2) CFTR InPlex ASR (Third Wave Technology); 3) CF v3 OLA ASR (Abbott Laboratories/Celera Diagnostics); 4) Signature CF 2.0 ASR (Asuragen); and 5) Tag-It mutation detection kit for CFTR 40 + 4 (currently known as Tag-It cystic fibrosis kit) (Tm Biosciences). Parameters evaluated include sensitivity, specificity, accuracy, ability to genotype, ability to reflex test according to ACMG recommendations, no calls/repeat rate, mutation panel content, hands-on time, start-to-finish time, laboratory work flow, input DNA range, data analysis methods, custom test design options, and required instrumentation. The resulting data demonstrate the diversity among the platforms and underline the need to evaluate the specific requirements and resources of a testing center in an effort to select the most appropriate CF platform.
Materials and Methods
CF Systems: Technologies
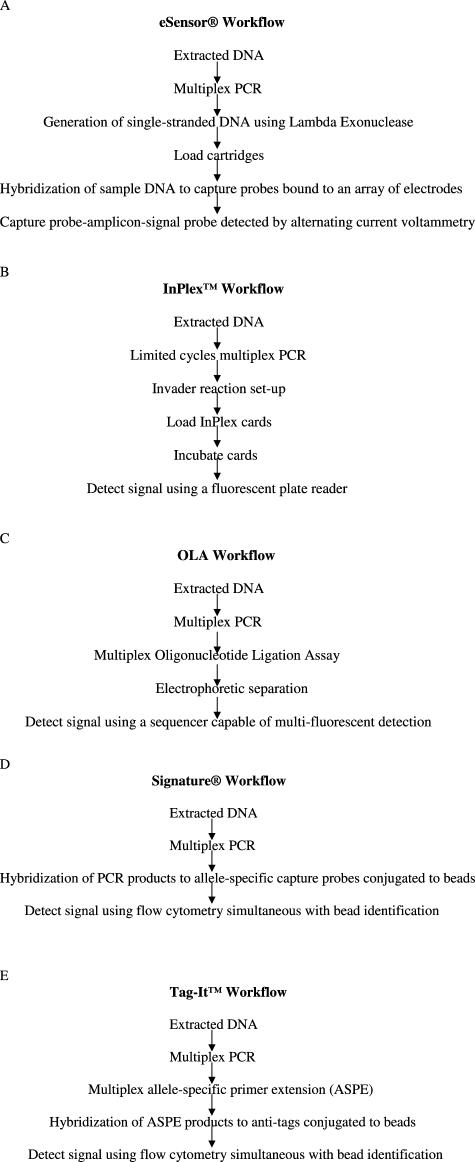
Working protocols were developed according to manufacturers’ instructions, and all genotype results were determined by autocalls, using the manufacturers’ software. An overview of the workflow of each of the five platforms described below is shown in Figure 1, A–E.
Figure 1.
Workflow overviews of each of the five platforms evaluated.
The eSensor cystic fibrosis carrier detection system (Osmetech Molecular Diagnostics) uses multiplex PCR products to hybridize to captured probes bound to an array of electrodes on specialized printed circuit boards clad in plastic chambers. Signal probes containing electrochemically-active ferrocene derivatives specifically bind to amplicons, and the capture probe-amplicon-signal probe complexes are detected by alternating current voltammetry using the eSensor instrument.
The CFTR InPlex ASR (Third Wave Technology) uses Third Wave Invader DNA chemistry using cleavase enzymes to recognize and cleave specific structures formed by the addition, in tandem, of two oligonucleotides to a nucleic acid target (multiplex PCR amplicons). Likewise, in a secondary reaction, a detectable fluorescent signal is generated via fluorescence resonance energy transfer. Both reactions take place in a microfluidics card containing dried Invader oligos/FRET cassettes. Signal is detected using a fluorometer.
The CF v3.0 OLA (oligonucleotide ligation assay) ASR (Abbott Laboratories/Celera Diagnostics) is based on hybridization of an exact-match PCR primer to the target sequence. Two oligonucleotide probes, one specific to the genotype and one common, then hybridize to the resulting amplicon. Because the genotype-specific probe carries a mobility-modifying 5′ tail, and the common probe contains a fluorescent dye marker, the resulting ligation products can then be separated electrophoretically. Signal is detected using an ABI Prism 3100/3130 genetic analyzer.
The Signature CF 2.0 ASR (Asuragen) technology is based on a multiplex PCR using biotin-modified PCR primers and allele-specific capture probes directly conjugated to coded beads on the Luminex 100xMAP platform.
The Tag-It Mutation Detection Kit for CFTR 40 + 4, currently known as Tag-It Cystic Fibrosis Kit, (Tm Biosciences) incorporates multiplex PCR followed by multiplex allele-specific primer extension with Tm’s proprietary Universal Tag sorting system on the Luminex 100xMAP platform.
Reagents
Reagents and required instrumentation, not currently used in our laboratory, were generously provided by the manufacturers for evaluation.
DNA Samples and DNA Amplification
Seven independent amplifications and runs were performed to challenge each platform with the same core set of 150 DNA samples (Table 1) allowing for comparison of study parameters discussed below. This core set represented the ACMG/ACOG 23 and normal samples. All of the ACMG/ACOG recommended panel of 23 CFTR mutations are represented except 2184delA. The samples included coded anonymized patient samples, CAP samples, and Coriell samples. Patient sample DNA was isolated using either MagNa Pure LC DNA isolation kit 1 (Roche) or the Gentra Generation capture column kit (Gentra Systems, Minneapolis, MN). In addition to the core set of samples, DNA from eight additional split patient samples was isolated using both MagNa Pure LC DNA Isolation Kit 1 and Gentra Generation capture column kit for direct comparison of utility of these isolation methods on each panel. For all assays, DNA amplification steps were performed on a PTC-200 DNA engine thermal cycler (MJ Research/Bio-Rad, Hercules, CA).
Table 1.
Genotypes of DNA Samples Tested on Each Platform
| Mutation/s | Mutation/s | Mutation/s |
|---|---|---|
| ΔF508 | N1303K | G85E/ΔF508 |
| ΔF508/ΔF508 | N1303K/ΔF508 | |
| ΔF508/N1303K | R334W | |
| ΔF508/1717 − 1G>A | R553X | |
| ΔF508/2789 + 5G>A | R553X/G551D | R347P/ΔF508 |
| ΔF508/R1162X | ||
| ΔF508/G85E | 621 + 1G>T | 711 + 1G>T/ΔF508 |
| ΔF508/711 + 1G>T | 621 + 1G>T/W1282X | |
| ΔF508/G551D | 1898 + 1G>A/R117H | |
| ΔF508/R117H | 621 + 1G>T/G542X | |
| ΔF508/R347P | 621 + 1G>T/3120 + 1G>A | 3849 + 10kbC>T |
| ΔF508/G542X | ||
| R117H | 2789 + 5G>A | |
| ΔI507 | R117H/ΔF508 | 2789 + 5G>A/ΔF508 |
| R117H/1898 + 1G>A | ||
| G542X | 3659delC | |
| G542X/G542X | 1717 − 1G>A | |
| G542X/621 + 1G>T | 1717 − 1G>A/ΔF508 | I148T |
| G542X/ΔF508 | ||
| G551D | A455E/ΔF508 | 3120 + 1G>A/621 + 1G>T |
| G551D/ΔF508 | R560T | Normal (100 archived samples) |
| G551D/R553X | ||
| W1282X | R1162X | |
| W1282X/621 + 1G>T | R1162X/ΔF508 |
Study Parameters
We evaluated each platform with respect to sensitivity, specificity, accuracy, signal discrimination, ability to genotype, ability to reflex test according to ACMG recommendations, no calls/repeat rate, number of and specific mutations (relating to ethnicity) in the available panels, hands-on time, start-to-finish time, laboratory work flow (including DNA extraction methods), data analysis methods, availability of additional tests, flexibility in respect to custom test design, and required instrumentation.
Results
Table 2 summarizes our evaluation of the five platforms.
Table 2.
Summary of Platform Evaluation
| eSensor | InPlex | OLA | Signature | Tag-It | |
|---|---|---|---|---|---|
| % Concordance | 100 | 100 | 100 | 100 | 100* |
| % No calls | 0.7 | 0.7 | 0.7 | 0.7 | 0.0* |
| Signal to noise ratio | NA† | NA† | NA† | 10:1‡ | 20:1 to 100:1‡ |
| Mutations§ | Total: 23 ACMG/ACOG 23 | Total: 42 ACMG/ACOG 23 and V520F, 3876delA, 394delTT, R347H, I148T, 1078delT, 3905insT, S549N, Y122X, Y1092X S549R(T>G), 2183AA>G, S549R(A>C), D1152H, 3849 + 4A>G,E60X, Q493X, D1270N, Y1092X(C>G) | Total: 32 ACMG/ACOG 23 and V520F, 3876delA, 394delTT, R347H, I148T, 1078delT, 3905insT, S549N/R | Total: 23 ACMG/ACOG 23 | Total: 40 ACMG/ACOG 23 and V520F, 3876delA, 394delTT, R347H, I148T, 1078delT, 3905insT, S549N, Y122X, S549R(T>G), 2183AA>G, Y1092X, 2307insA, A559T, 1898 + 5G>T, M1101K, S1255X |
| Reflex tests: are poly-T reflex tests masked or run separately? | Masked¶ | Masked | Separately | Separately | Masked |
| Does the assay detect interfering benign variants (I506V, I507V, F508C) in the case of unexpected ΔF508 homozygosity? | NA∥ | NA** | Yes | Yes | Yes |
| Input DNA range (ng)†† | 10 to 600 | 25 to 350 | 1 to 15 | 10 to 1000 | 2 to 200 |
| Extraction methods used‡‡ | MP,G | MP,G | MP,G | MP,G | MP,G |
| Start to finish time (hours)§§ | 6 to 7 | 3.5 to 4 | 6 to 7 | 5 to 6 | 6.5 to 8 |
| Hands-on time (hours)§§ | 2.5 | <1 | 1.5 | 1 | 1.5 to 2.5 |
| Number of sample transfers | 3 | 2 | 2 | 2 | 4 |
| Ease of protocol¶¶ | 2 | 1 | 2 | 2 | 3 |
| Open platform∥∥ | No | No | Yes | Yes | Yes |
| Required instrumentation specific to assay | eSensor 4800 | GeNios or GeniosFL fluorometer, card bucket and clips, card sealer | ABI Prism 3100/3130 genetic analyzer | Luminex 100xMAP system | Luminex 100xMAP system |
| IVD or ASR | IVD*** | ASR | ASR | ASR | IVD |
NA, not applicable; ACMG, American College of Medical Genetics; ACOG, American College of Obstetrician and Gynecologists; MP, MagNa Pure LC DNA isolation kit 1; G, Gentra Generation capture column kit; IVD, In Vitro Diagnostic; ASR, analyte-specific reagent.
Data reported here were generated by a Tm Bioscience technician performing the assay in our laboratory. Modifications to the research use-only protocol (RUO) were made by the Tm technician. The RUO was the only available protocol at the time this study was performed. These modifications were made in an effort to minimize the previously high no-call rate and shorten the start-to-finish time and hands-on time. The modifications are as follows: 1) Exo-Sap denaturation was run 30 seconds instead of 15 minutes; 2) multiplex ASPE annealing was performed at 56°C instead of 52°C; 3) ASPE extension was run for 30 seconds instead of 1 minute; and 4) bead hybridization at 37°C was run 30 minutes instead of 1 hour.
The concepts of signal and noise do not apply to these assays.
Signal to noise ratio was calculated as follows: for Tag-It, signal is the median fluorescence intensity (MFI) generated by an allele in the sample and noise is the MFI generated by allele in the no template control; for Signature, signal is the allele ratio (mutant signal/mutant signal + wild-type signal) and noise is the standard deviation of the allele ratio.
The following platforms were able to resolve a G551D/R553X compound heterozygote: InPlex, TagIt, Signature, and eSensor. The study evaluated only the ACMG/ACOG panel of 23 mutations (2184delA was not represented). Mutations in italics are unique to that IVD/ASR.
Software for unmasking reflex test results was not available at time of evaluation; poly-T reflex test results were not evaluated.
The polymorphisms do not interfere with panel mutation genotyping in the eSensor method (information provided by the manufacturer). We did not test this aspect of the platform.
Because of the Invader chemistry, ie, the specificity with which the cleavage products are produced, the I506V and I507V polymorphisms do not interfere with genotyping (information provided by the manufacturer). We did not test this aspect of the platform. The F508C variant is assayed during the initial run with results masked.
Information provided by manufacturer.
MagNa Pure LC DNA isolation kit 1- and Gentra Generation capture column kit-extracted samples were tested on each platform. No other extraction methods were tested.
Time determined was averaged throughout several runs for 24 samples/run, excluding DNA extraction. Time calculations were based on use of a PTC-200 DNA engine thermal cycler (MJ Research/Bio-Rad). Tag-It start to finish time reflects protocol modifications indicated in *, ie, ASPE extension was run for 30 seconds instead of 1 minute; bead hybridization at 37°C was run 30 minutes instead of 1 hour.
As determined by our laboratory based on number of steps in the protocol, tolerances within those steps, and number of sample transfers.
Facilitates custom test development.
eSensor is FDA-cleared for carrier testing.
Specificity, Sensitivity, and No-Call Rate
All platforms evaluated demonstrated excellent specificity and sensitivity (100% concordance) and acceptable no call rates (all ≤0.7%). The following platforms were able to resolve a G551D/R553D compound heterozygote: InPlex, Tag-It, Signature, and eSensor. Note that because all platforms were challenged with the same set of 150 DNA samples, only normal samples and samples with genotypes representing the ACMG/ACOG panel of 23 were tested; eSensor and Signature test only the ACMG/ACOG panel of 23.
Reflex Tests
Both the OLA and Signature platforms require poly-T reflex tests to be run separately, whereas the InPlex, Tag-It, and eSensor platforms allow the poly-T reflex test to be run concurrently with other mutations and are masked until user chooses to unmask that data. As to the detection, via reflex testing, of ΔF508 interfering benign polymorphic variants (I506V, I507V, and F508C), Tag-It, Signature, and OLA require a separate run, whereas eSensor does not require reflex testing for these variants, and InPlex does not require reflex testing for I506V and I507V because, according to the manufacturers, these polymorphisms do not interfere with the hybridization of the wild-type probe on these platforms. We did not test this aspect of either assay. The InPlex probe set does include probes for the identification of F508C and are part of the initial run. The F508C result is masked in the absence of ΔF508.
Time Considerations
The start-to-finish time and hands-on time are in respect to processing of 24 samples (excluding DNA extraction). We found InPlex to require the least time in both categories. Here, the reported times are based on use of a PTC-200 DNA engine thermal cycler (MJ Research/Bio-Rad).
Input DNA
All platforms tested performed equally well using either MagNa Pure LC DNA Isolation Kit 1 or Gentra Generation capture column kit for DNA isolation from whole blood. The DNA input range, as stated by the manufacturer, is quite broad with the exception of the OLA platform. None of the platforms required DNA quantitation, ie, expected yields as described by the manufacturers of the DNA isolation kits were sufficient to use as estimates of DNA concentration.
Ease of Protocol
We determined ease of protocol based on number of steps, tolerances within those steps, and number of sample transfers. We found the InPlex platform to be of greatest ease, Tag-It to be the most complex, and the remaining three platforms falling in between these.
Signal:Noise Ratio
The signal:noise ratio was not calculable for three of the panels, and therefore this factor was unfortunately not comparable among all platforms.
Required Instrumentation Specific to the Assay
All of the platforms require specialized instrumentation. With the exception of the eSensor, additional tests can be run using the same instrumentation. In addition, three platforms, Tag-It, Signature, and OLA. are considered to be open platforms, ie, enable development of custom tests.
Mutation Panel
All of the panels test, at a minimum, the ACMG/ACOG-recommended panel of 23 CFTR mutations. Of the panels evaluated, InPlex tests for the greatest number of mutations. After the completion of this study, Tm Bioscience introduced a CFTR 70 + 6 ASR; however, this method was not analyzed in this study.
Discussion
All five platforms evaluated demonstrated excellent specificity and sensitivity as well as acceptable no call rates (Table 2). The ACMG/ACOG panel of 23 mutations (excluding 2184delA) was successfully detected by all platforms (Table 1). Three platforms, InPlex, OLA, and Tag-It, include mutations in addition to the ACMG/ACOG panel of 23. All of the additional mutations in the OLA panel are contained in the InPlex and Tag-It panels, whereas InPlex and Tag-It contain additional common mutations beyond the OLA panel as well as unique mutations (Table 2). After completion of this study, Tm Bioscience introduced a CFTR 70 + 6 ASR. Signature has a panel of 46 mutations that is in preparation to be submitted to the Food and Drug Administration (FDA). The three platforms in this study that include mutations beyond the ACMG panel of 23 mutations require running of all mutations in the panel, ie, specific mutation exclusion is not possible during the run, and only InPlex allows masking of results to facilitate evaluation limited to the ACMG 23 mutations.
The ACMG/ACOG panel is panethnic yet primarily based on mutation frequencies in non-Hispanic Caucasian populations and Ashkenazi Jewish population because of high frequency of the disease and availability of mutation data.8 Depending on mutation frequencies of the populations serviced by a particular laboratory, consideration of target mutations may be a determining point in panel selection. Determination of the appropriate test panel may be challenging because of admixture among ethnic groups, inaccurate self-reporting of ethnicity, and extreme heterogeneity of the US population.9
The InPlex, OLA, and Tag-It platforms used in this study contain I148T and 1078delT, which are no longer recommended by ACMG for inclusion in a CF carrier screening panel.7 After completion of this study these variants were removed from the Tag-It panel (which has since been FDA-cleared). Abbott dropped I148T from their OLA panel that has been submitted for FDA clearance. Third Wave Technologies removed I148T and 1078delT from their panel in preparation for FDA regulatory submission. Questions have arisen as to the clinical relevance of two additional mutations, D1270N and D1152H, present in the InPlex panel. Recent publications suggest that D1152H is pathogenic in respect to CF whereas D1270N may not be a causative factor of CF by itself.20,21,22 D1270N has been removed from the InPlex panel for FDA submission.
Reflex testing varied significantly throughout the platforms evaluated. Two platforms, OLA and Signature, required poly-T reflex testing be performed on a separate run, ie, the software did not have masking capabilities. eSensor does not reflex for ΔF508 variants. The manufacturers assert the polymorphisms do not interfere with genotyping. For the same reason, InPlex does not reflex for I506V or I507V. Probes for F508C are included in the initial InPlex run with the result masked in the absence of ΔF508.
All platforms performed well with DNA extracted using either of the methods used in this study, ie, MagNa Pure LC DNA Isolation Kit 1 and Gentra Generation capture column kit. Although we did not test blood spots, all platform manufacturers except Osmetech Molecular Diagnostics (eSensor) state DNA extracted from blood spots is compatible with their platform. In addition, a recent report summarizing the use of DNA from buccal cells for genotyping suggests that this source of DNA might be a reliable replacement for the analysis of leukocytes for the exclusion of CF in children.23 Information supplied by the manufacturers of the platforms we tested indicate that DNA extracted from buccal swabs has been successfully used with InPlex, Signature, and OLA and has not been fully tested on Tag-It CF or eSensor platforms. As to tolerance of input DNA range (ng), all platforms, except OLA, have a wide window of acceptability (Table 2). Although OLA has a narrow range, 1 to 15 ng, in this study we did not quantitate the DNA after extraction and still successfully ran the protocol based on expected DNA extraction concentrations.
The signal-to-noise ratio was not easily compared from platform to platform because of differences in technology, methods of signal calculations and manufacturers’ definitions of noise. Only Signature and Tag-It, the two liquid bead array assays, provided a signal-to-noise ratio value (Table 2). Tag-It demonstrated a very stringent signal to noise ratio.
In consideration of hands-on time and total processing time of each assay, we found the InPlex platform required less than 1 hour and 3.5 to 4 hours, respectively, the least time in both categories of all platforms tested. Throughout the study, MJ PTC-200 thermal cylers were used. After completion of this study, we found that the use of an Eppendorf Mastercycler EP S (Hamburg, Germany) does reduce the start-to-finish time for those assays requiring long or multiple amplification steps. We found the hands-on time determined in this study is a reflection of the complexity of the protocol in the case of Tag-It and for eSensor is attributable to the manual manipulations, eg, dual biochips are required for each sample. Krafft and Lichy12 recently reported a time-motion analysis study of six CF mutation detection systems, including two reported in this study (Tag-It and OLA) as well as the Invader plate system that preceded the InPlex card studied here. Their resulting labor and total assay times are comparable with results reported here.
As shown in Table 2, all five platforms require instrumentation specific to the detection system, ie, in addition to common laboratory equipment such as a thermal cycler, hybridization oven, and centrifuge. Although instrumentation for four of the platforms is commonly used for detection of mutations in addition to CF, the eSensor is currently used solely for CF testing. The OLA, Signature, and Tag-It platforms are considered to be open platforms allowing for custom test development. Currently, Tag-It and eSensor are FDA-cleared. eSensor is cleared for carrier testing only. Abbott/Celera and Third Wave have completed FDA submissions for their OLA and InPlex products, respectively, whereas Asuragen is actively pursuing a regulatory submission for their expanded Signature panel.
Because pricing of reagents is determined by both the number of tests contracted to be run (including required controls/run) and by the contracted purchase of combinations of multiple test reagents, ie, the number of different test reagents/instrumentation purchased from the same company, calculating actual costs of reagents/patient sample for informational purposes is approximate at best. Here, we estimated the following costs of reagents/patient sample using a capital purchase of equipment model, no discounts for multikit types being run in the laboratory, and ∼250 samples run per year: InPlex, $39.00; OLA, $64.00; Tag-It, $50.00; Signature, $45.00. Osmetech offers the eSensor 4800 and related reagents as a reagent rental agreement only with the reagent costs being between $65 to $100, depending on volume of tests. A second cost consideration is instrumentation. Future direction of the laboratory may dictate how instruments are acquired, eg, direct purchase or lease. Purchasing an instrument specific to a platform may financially lock the laboratory into using that platform for a period of time that may extend beyond its usefulness. An estimate of direct purchase instrumentation costs (excluding common laboratory equipment such as thermal cyclers, centrifuges, and hybridization ovens) is as follows: InPlex (fluorometer, card bucket and clips, card sealer) $12,900; OLA (ABI Prism 3100/3130 genetic analyzer, 16 capillary), $100,000 to $145,000; Tag-It (Luminex 100xMAP System), $45,000; and Signature (Luminex 100xMAP System), $45,000; eSensor is not offered as a direct purchase. With the exception of the eSensor 4800, all of these instruments are used for multiple platforms. An additional significant arm of cost calculation is the required technician time. Hands-on technician time is shown in Table 2. Costs of test/patient sample, estimated above, may be reduced with consideration of purchase models, ie, reagent rental versus capital purchase agreements. In addition, test volume and the menu of tests run from the same manufacturer influence reagent cost quotes. All approximate costs of reagents and instrumentation given above are specific to our institution and valid as of the writing of this article and are intended to be used for ballpark comparison purposes only.
Availability of mutation-positive controls is a consideration for all clinical assays. None of the ASRs or in vitro diagnostic tests evaluated in this study includes positive controls. Both DNA and cell line controls for all 23 of the ACMG mutations are available from National Institute of General Medical Sciences Human Genetic Cell Repository (http://locus.umdnj.edu/nigms/). In addition, positive CF controls are available commercially. Aytay and colleagues24 reported the compatibility of Optiqual CF mutation controls (Acrometrix, Benicio, CA) with several CF mutation detection systems including three (Tag-It, OLA, and Signature) evaluated in this study. These synthetic CFTR mutation controls include the 23 ACMG mutations plus five additional mutations. Molecular Controls (Sacred Heart Medical Center, Spokane, WA) offers another synthetic oligonucleotide mixture that has been validated with both the OLA and Tag-It platforms and has applications to other platforms as well. Maine Molecular Quality Controls, Inc. (Scarborough, ME) offers a recently FDA-cleared source of stabilized synthetic nucleic acids CFTR-positive control. This control is designed to mimic whole blood and to be used to assess the performance of the extraction, amplification, and detection protocols for CF. It monitors the presence of the ACMG 23 mutations plus 15 additional mutations and has been validated for OLA, Signature, Tag-It, and eSensor and several other platforms not included in this study. Collaboration with Third Wave regarding validation of this control with InPlex is in progress. This brief description of mutation-positive controls is not intended to be exhaustive, rather to illustrate the commercial variety of choices available to laboratories.
In summary, a prudent choice of a CFTR mutation detection system depends on many parameters, some of which were discussed above. Evaluation of these factors provided valuable information regarding the selection of the CF platform most appropriate for our small academic/hospital clinical laboratory.
Footnotes
C.S.R. was contracted to evaluate the eSensor platform through an agreement with Clinical MicroSensors (now Osmetech) entitled “Multicenter Prospective/Retrospective Evaluation of the Performance Capabilities of the eSensor Cystic Fibrosis Carrier Screening System.” Partial support to attend the 2005 Association for Molecular Pathology conference was provided to M.A.J. by Third Wave Technologies.
References
- Rommens JM, Iannuzzi MC, Kerem B-S, Drumm ML, Melmer G, Dean M, Rozmahel R, Cole JL, Kennedy D, Hidaka N, Zsiga M, Buchwald M, Riordan JR, Tsui LC, Collins FS. Identification of the cystic fibrosis gene: chromosome walking and jumping. Science. 1989;245:1059–1065. doi: 10.1126/science.2772657. [DOI] [PubMed] [Google Scholar]
- Riordan JR, Rommens JM, Kerem B-S, Alon N, Rozmahel R, Grzelczak Z, Zielenski J, Lok S, Plavsic N, Chou JL, Drumm ML, Iannuzzi MC, Collins FS, Tsui LC. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science. 1989;245:1066–1073. doi: 10.1126/science.2475911. [DOI] [PubMed] [Google Scholar]
- Kerem B-S, Rommens JM, Buchanan JA, Markiewicz D, Cox TK, Chakravarti A, Buchwalk M, Tsui LC. Identification of the cystic fibrosis gene: genetic analysis. Science. 1989;245:1073–1080. doi: 10.1126/science.2570460. [DOI] [PubMed] [Google Scholar]
- Palomaki GE, Haddow JE, Bradley LA, FitzSimmons SC. Updated assessment of cystic fibrosis mutation frequencies in non-Hispanic Caucasians. Genet Med. 2002;4:90–94. doi: 10.1097/00125817-200203000-00007. [DOI] [PubMed] [Google Scholar]
- Farrell PM, Fost N. Prenatal screening for cystic fibrosis: where are we now? J Pediatr. 2002;141:758–768. doi: 10.1067/mpd.2002.127666. [DOI] [PubMed] [Google Scholar]
- Grody WW, Cutting GR, Klinger KW, Richards CS, Watson MS, Desnick RJ. Laboratory standards and guidelines for population-based cystic fibrosis carrier screening. Genet Med. 2001;3:149–154. doi: 10.1097/00125817-200103000-00010. [DOI] [PubMed] [Google Scholar]
- Watson MS, Cutting GR, Desnick RJ, Driscoll DA, Klinger K, Mennuti M, Palomaki GE, Popovich BW, Pratt VM, Rohlfs EM, Strom CM, Richards CS, Witt DR, Grody WW. Cystic fibrosis population carrier screening: 2004 revision of American College of Medical Genetics mutation panel. Genet Med. 2004;6:387–391. doi: 10.1097/01.GIM.0000139506.11694.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards CS, Bradley LA, Amos J, Allitto B, Grody WW, Maddalena A, McGinnis MJ, Prior TW, Popovich BW, Watson MS. Standards and guidelines for CFTR mutation testing. Genet Med. 2002;4:379–391. doi: 10.1097/00125817-200209000-00010. [DOI] [PubMed] [Google Scholar]
- Heim RA, Sugarman EA, Allitto BA. Improved detection of cystic fibrosis mutations in the heterogeneous U.S. population using an expanded, pan-ethnic mutation panel. Genet Med. 2001;3:168–176. doi: 10.1097/00125817-200105000-00004. [DOI] [PubMed] [Google Scholar]
- Grosse SD, Boyle CA, Botkin JR, Comeau AM, Kharrazi M, Rosenfeld M, Wilfond BS, CDC Newborn screening for cystic fibrosis. MMWR Recomm Rep. 2004;53(RR13):1–36. [PubMed] [Google Scholar]
- Tomaiuolo R, Spina M, Castaldo G. Molecular diagnosis of cystic fibrosis: comparison of four analytical procedures. Clin Chem Lab Med. 2003;41:26–32. doi: 10.1515/CCLM.2003.006. [DOI] [PubMed] [Google Scholar]
- Krafft AE, Lichy JH. Time-motion analysis of 6 cystic fibrosis mutation detection systems. Clin Chem. 2005;51:1116–1122. doi: 10.1373/clinchem.2004.047423. [DOI] [PubMed] [Google Scholar]
- Amos JA, Bridge-Cook P, Ponek V, Jarvis MR. A universal array-based multiplexed test for cystic fibrosis carrier screening. Expert Rev Mol Diagn. 2006;6:15–22. doi: 10.1586/14737159.6.1.15. [DOI] [PubMed] [Google Scholar]
- Hadd AG, Brown JT, Andruss BF, Ye F, Walker Peach CR. Adoption of array technologies into the clinical laboratory. Expert Rev Mol Diagn. 2005;5:409–420. doi: 10.1586/14737159.5.3.409. [DOI] [PubMed] [Google Scholar]
- Edelmann L, Hashmi G, Song Y, Han Y, Kornreich R, Desnick RJ. Cystic fibrosis carrier screening: validation of a novel method using BeadChip technology. Genet Med. 2004;6:431–438. doi: 10.1097/01.gim.0000140836.66050.88. [DOI] [PubMed] [Google Scholar]
- Schrijver I, Oitmaa E, Metspalu A, Gardner P. Genotyping microarray for detection of more than 200 CFTR mutations in ethnically diverse populations. J Mol Diagn. 2005;7:375–387. doi: 10.1016/S1525-1578(10)60567-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uphoff TS, Highsmith WE., Jr Introduction to molecular cystic fibrosis testing. Clin Lab Sci. 2006;19:24–31. [PubMed] [Google Scholar]
- Richards CS, Grody WW. Prenatal screening for cystic fibrosis: past, present and future. Expert Rev Mol Diagn. 2004;4:49–62. doi: 10.1586/14737159.4.1.49. [DOI] [PubMed] [Google Scholar]
- Lyon E, Miller C. Current challenges in cystic fibrosis screening. Arch Pathol Lab Med. 2003;127:1133–1139. doi: 10.5858/2003-127-1133-CCICFS. [DOI] [PubMed] [Google Scholar]
- Mussaffi H, Prais D, Mei-Zahav M, Glau H. Cystic fibrosis mutations with widely variable phenotype: the D1152H example. Pediatr Pulmonol. 2006;41:250–254. doi: 10.1002/ppul.20343. [DOI] [PubMed] [Google Scholar]
- Highsmith WE, Jr, Friedman KJ, Burch LH, Spock A, Silverman LM, Boucher RC, Knowles MR. A CFTR mutation (D1152H) in a family with mild lung disease and normal sweat chlorides. Clin Genet. 2005;68:88–90. doi: 10.1111/j.1399-0004.2005.00459.x. [DOI] [PubMed] [Google Scholar]
- Claustres M, Altieri J-P, Guittard C, Templin C, Chevalier-Porst F, Des Georges M. Are p.I148T, p.R74W and p.D1270N cystic fibrosis causing mutations? BMC Med Genet. 2004;5:19. doi: 10.1186/1471-2350-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries TW, Ajubi N, Slomp J, Storm H. Analyzing DNA from buccal cells is a reliable method for the exclusion of cystic fibrosis. Results of a pilot study. Genet Med. 2006;8:175–177. doi: 10.1097/01.gim.0000201066.23642.b1. [DOI] [PubMed] [Google Scholar]
- Aytay S, Lebo RV, Galehouse D, Johnson MA, Webb M, Neuwald P. Performance evaluation of OptiQual™ CF mutation controls in eight different cystic fibrosis ASRs. The Association for Molecular Pathology Annual Meeting, 2005 Nov 11–13, Scottsdale, AZ. Poster G03. J Mol Diagn. 2005;7:648. [Google Scholar]