Abstract
p150/95 (CD11c/CD18, CR4) is a member of the β2-integrin family of adhesion molecules and is considered an important phagocytic receptor. The role of p150/95 in the development of central nervous system demyelinating diseases, including multiple sclerosis, remains unexplored. To determine p150/95-mediated mechanisms in experimental autoimmune encephalomyelitis (EAE), we performed EAE using CD11c-deficient (CD11c−/−) mice. EAE in CD11c−/− mice was significantly attenuated and characterized by markedly reduced spinal cord T-cell infiltration and interferon-γ production by these cells. Adoptive transfer of antigen-restimulated T cells from wild-type to CD11c−/− mice produced significantly attenuated EAE, whereas transfer of CD11c−/− antigen-restimulated T cells to control mice induced a very mild, monophasic EAE. T cells from MOG35–55 peptide-primed CD11c−/− mice displayed an unusual cytokine phenotype with elevated levels of interleukin (IL)-2, IL-4, and IL-12 but reduced levels of interferon-γ, tumor necrosis factor-α, IL-10, IL-17, and transforming growth factor-β compared with control mice. Overall, CD11c−/− T cells from primed mice proliferated comparably to that of control T cells on MOG35-55 restimulation. Our results indicate that expression of p150/95 is critical on both T cells as well as other leukocytes for the development of demyelinating disease and may represent a novel therapeutic target for multiple sclerosis.
Multiple sclerosis (MS) is considered a T-cell-mediated autoimmune disease, with self-reactivity directed against numerous myelin-derived antigens, including myelin basic protein and myelin oligodendrocyte glycoprotein (MOG). A variety of other cell types, including macrophages, dendritic cells, glial cells, and γδ T cells, as well as various blood-borne and membrane-anchored effector molecules (eg, cytokines, antibody, and complement), also contribute to MS pathogenesis and inflammation.1,2,3,4,5 A classic feature of MS is the trafficking of antigen-specific T cells and macrophages into the central nervous system (CNS), where they initiate inflammation and destruction of oligodendrocytes and eventually neurons. The movement of these inflammatory cells into the CNS is regulated by a number of molecules including leukocyte/endothelial cell adhesion proteins and chemoattractant/activating molecules. CNS inflammatory model systems, including the MS model, experimental autoimmune encephalomyelitis (EAE), strongly suggest that the adhesion molecules VLA-4 and its ligand vascular cell adhesion molecule-1, as well as the β2-integrin molecules LFA-1 and Mac-1 (CD11a and CD11b, respectively), play an integral part in this process.6,7,8 The role of other β2-integrin molecules, adhesion molecules, in particular CD11c/CD18 (CR4, p150/95), remains unexplored.
p150/95 is expressed by myeloid cells including macrophages, neutrophils, dendritic cells, and lymphocytes, and expression increases on treatment with a variety of chemoattractants, cytokines, phorbol esters, or on antigen-mediated activation.9,10,11,12,13,14,15,16,17 In the CNS, microglia and infiltrating macrophages constitutively express this adhesion molecule, and p150/95 expression increases on activation of these phagocytic cells.18,19,20,21,22 p150/95 binds to cells via a limited number of known ligands including iC3b, fibrinogen, intercellular adhesion molecule-1, and lipopolysaccharide (LPS)10,15,23,24,25,26 and is important in the phagocytic clearance of bacteria and apoptotic cells.14,27,28,29,30,31 Studies have also suggested a role for p150/95 in monocyte/endothelium interactions or conjugate formation between cytotoxic T cells and target cells of various types,14,18,32,33,34,35 but the in vivo relevance of these findings remains unclear. These studies combined with our previous work demonstrating an important role for the other iC3b receptor, Mac-1, in the development and progression of EAE6 prompted us to examine the role of p150/95 in this animal model of autoimmune demyelinating disease.
We report here the results of EAE studies using CD11c−/− mice. The absence of CD11c resulted in significantly attenuated disease severity with reduced cellular infiltration and demyelination compared with wild-type mice. In addition, adoptive transfer experiments demonstrated that p150/95 expression is required on T cells for the development of EAE; however, loss of p150/95 did not affect T-cell proliferation in in vitro restimulation assays. In fact at higher antigen concentration, T-cell proliferation was enhanced using CD11c-deficient T cells. Despite normal proliferation, CD11c−/− T cells isolated from either spleens or spinal cords of mice with EAE produced a profile of cytokines favoring an anti-inflammatory response. Our results suggest that p150/95 is important at multiple levels for the development of EAE, particularly at the level of effector T-cell functions, and may also contribute to both phagocytosis of myelin debris and leukocyte trafficking during the pathogenesis of EAE.
Materials and Methods
Mice
Mice containing a null mutation for CD11c were generated by gene targeting using 129/Sv-embryonic stem cells as previously described.36 The CD11c mutation was then backcrossed onto the C57BL/6 strain for at least seven generations (The Jackson Laboratory, Bar Harbor, ME). Inbred C57BL/6 mice were used as controls for all experiments. All studies were performed with approval from the University of Alabama at Birmingham Institutional Animal Care and Use Committee. CD11c−/− mice have normal splenic and lymph node structure, architecture, and cellularity compared with control mice. In our hands, MOG-induced EAE in 129/Sv mice is essentially identical to that seen in C57BL/6 mice.
Induction of Active and Transferred EAE
For active EAE, control and CD11c−/− mice were immunized with MOG peptide35-55 as described,37 except that the mice received only one MOG peptide injection. MOG peptide was synthesized by standard 9-fluorenyl-methoxycarbonyl chemistry and was >95% pure as determined by reversed phase-high performance liquid chromatography (Biosynthesis, Lewisville, TX). Onset and progression of EAE symptoms were monitored daily using a standard clinical scale ranging from 0 to 6 as follows: 0, asymptomatic; 1, loss of tail tone; 2, flaccid tail; 3, incomplete paralysis of one or two hind limbs; 4, complete hind limb paralysis; 5, moribund; and 6, dead. Only mice with a score of at least 2 (flaccid tail) for more than 2 consecutive days were judged to have onset of EAE. For each animal a cumulative disease index was calculated from the sum of the daily clinical scores observed between day 7 and day 30. For transferred EAE, spleens of control or CD11c−/− donors were removed 2 to 3 weeks after induction of active EAE and prepared as previously described.37 Passive EAE was induced by injecting ∼5 × 106 purified T cells derived from wild-type mice into CD11c−/− mice or by injecting the same number of purified T cells derived from CD11c−/− mice into wild-type mice. In both cases, purified T cells derived from wild-type mice were injected into wild-type mice as a control to monitor disease development.
Histopathology
Mice with actively induced EAE were sacrificed at 32 days after induction by CO2 inhalation, and spinal columns were removed, fixed in 10% buffered formalin, and paraffin-embedded. Sections (5 μm thick) from the cervical, thoracic, and lumbar spinal cord were cut and either stained with hematoxylin and eosin for overall lesion evaluation and characterization of inflammatory responses or with Luxol fast blue for evaluation of demyelination. The extent of inflammation and demyelination was scored based on lesion size (0 to 4), and lesions were evaluated for lymphocyte accumulation, neutrophil infiltration, demyelination, axonal degeneration, and gliosis (0 to 4). Tissues were evaluated without identification as to experimental group. Severity scores were calculated as the mean overall segments of the products of the intensity scores multiplied by the extent scores for each lesion characteristic (inflammation, axonal degeneration, gliosis, and demyelination). The means of the individual lesion characteristic severity scores were summed to give the overall severity score.
Isolation and Flow Cytometric Analysis of Leukocytes from Spinal Cords
Spinal cords were removed from control and CD11c−/− mice with active EAE (days 12 to 15) after perfusion with phosphate-buffered saline (PBS), ground through a cell strainer, washed in PBS, resuspended in 40% Percoll, and layered on 70% Percoll. After centrifugation at 2000 rpm (room temperature, 25 minutes), cells at the interface were removed and washed in PBS and stained as described. Cells obtained from spinal cords were incubated with anti-CD16/32 (24G2, FcR block) to prevent nonspecific staining. Spinal cord leukocytes were stained with anti-CD4-fluorescein isothiocyanate [GK1(CR1).5], anti-CD-8-phycoerythrin (53-6.7), anti-CD45-fluorescein isothiocyanate (30F11), anti-tumor necrosis factor-α-phycoerythrin (MP6-XT22), and anti-interferon (IFN)-γ-fluorescein isothiocyanate (XMG1.2), all from eBiosciences, San Diego, CA. Stained cells and forward scatter were analyzed using a FACSCalibur and the data analyzed using CellQuest software (BD Biosciences, San Jose, CA).
T-Cell Proliferation and Cytokine and Chemokine Production
Antigen-specific T-cell proliferation assays were performed as previously described.37 Single cell suspensions from spleens obtained 14 days after EAE induction were cultured in 96-well plates at 5 × 105 cells/well with increasing concentrations of MOG35-55 peptide in triplicate. After 48 hours, cultures were pulsed with [3H]thymidine for an additional 18 hours, and incorporation of thymidine was measured. The in vitro cytokine assays were performed essentially as described for the proliferation assay. Duplicate cultures were either left untreated or stimulated with MOG peptide alone (5 μg/ml). Culture supernatants were collected at 48 hours for use in cytokine enzyme-linked immunosorbent assays. Enzyme-linked immunosorbent assay kits for murine cytokines [IFN-γ, tumor necrosis factor-α, interleukin (IL)-2, IL-4, IL-10, IL-12, IL-17, and transforming growth factor-β] were purchased from R&D Systems (Minneapolis, MN). Each assay was performed according to the manufacturer’s instructions. Cytokine production by cultures of wild-type and CD11c−/− cells is reported as the mean ± SEM of four mice per group. The data are pooled from two separate experiments.
Statistics
Statistical significance between control and CD11c−/− mice for active and transferred EAE experiments was calculated using the Wilcoxon signed-rank test; for proliferation assays the Student’s t-test was used. Results of evaluations for inflammation and demyelination were analyzed using analysis of variance for main effects and Tukey’s test for pairwise mean comparisons.
Results
Deletion of p150/95 Significantly Attenuates Active EAE
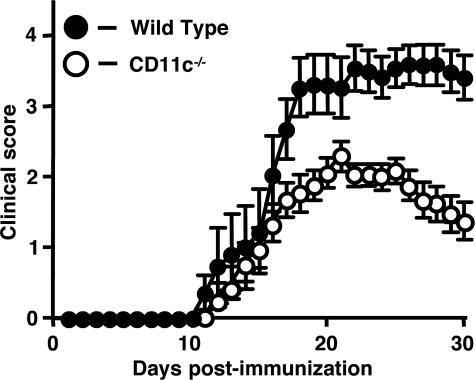
To determine the role of p150/95 in EAE, we immunized wild-type and CD11c−/− mice using MOG35-55 peptide and followed the course of disease for 30 days. CD11c−/− mice developed EAE slightly later than wild-type mice (19 days versus 16 days); however, the difference was not statistically significant (Figure 1, Table 1). Both groups of mice had a similar disease course during the acute phase of disease, but the chronic phase of disease was attenuated in CD11c−/− mice compared with wild type. The cumulative disease index for CD11c−/− mice was significantly lower than that of controls (32.1 versus 58, respectively; P < 0.0001, Wilcoxon signed-rank test) (Table 1).
Figure 1.
The clinical course of active EAE is attenuated in CD11c−/− mice. Active EAE was induced with MOG35–55 peptide and symptoms scored for 30 days as described in Materials and Methods. Results shown are the daily mean clinical score for wild-type (n = 11) and CD11c−/− mice (n = 17) from three experiments.
Table 1.
EAE Symptoms in Wild-Type Mice and CD11c−/− Mice
| Mice | CDI* | Disease onset† | Disease incidence‡ |
|---|---|---|---|
| Wild type, n = 11 | 58 | 16 days | 100 |
| CD11c−/−, n = 17 | 32.1 | 19 days | 94 |
Cumulative disease index is the mean of the sum of daily clinical scores observed between days 7 and 30.
Disease onset is defined as the 1st day of 2 consecutive days with a clinical score of two or more.
Disease incidence is defined as the percent of mice that displayed any clinical signs of disease
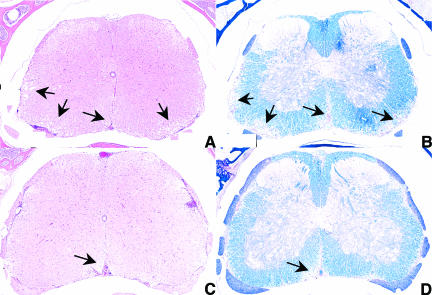
Cellular Infiltration and Demyelination in CD11c−/− Mice with EAE
We next performed histopathological analysis on spinal cords of wild-type and CD11c−/− mice with active EAE to determine the extent and nature of the cellular infiltrate and the amount of demyelination between the two groups of mice. Representative spinal cord sections from wild-type mice obtained 32 days after disease induction had significant cellular infiltration in the meninges and white matter (Figure 2A) with corresponding demyelination (Figure 2B). Sections obtained from CD11c−/− mice had little cellular infiltration, inflammation, axonal degeneration, and demyelination throughout the spinal cord, compared with wild-type mice (Figure 2, C and D). The overall mean score for these parameters for all regions of the spinal cord in CD11c−/− mice was 0.82, whereas wild-type mice had a mean score of 3.1.
Figure 2.
Leukocyte infiltration and demyelination are reduced in CD11c−/− mice in EAE. Spinal cords from wild-type and CD11c−/− mice (n = 3 for each group) were obtained at 32 days after immunization, fixed in 10% buffered formalin, and paraffin-embedded. Sections from the cervical, thoracic, and lumbar regions (5 μm) were stained with H&E or Luxol fast blue (LFB) and scored as described in Materials and Methods. A: Representative section from a wild-type mouse stained with H&E. Arrows indicate widespread cellular infiltration and inflammation. B: Section from the same specimen as in A stained with LFB. Arrows indicates regions of significant demyelination. C: Representative section from an CD11c−/− mouse stained with H&E. Note the lack of cellular infiltration and inflammation. D: Section from the same specimen as in C stained with LFB. Little to no demyelination was observed throughout the white matter. Original magnifications, ×4.
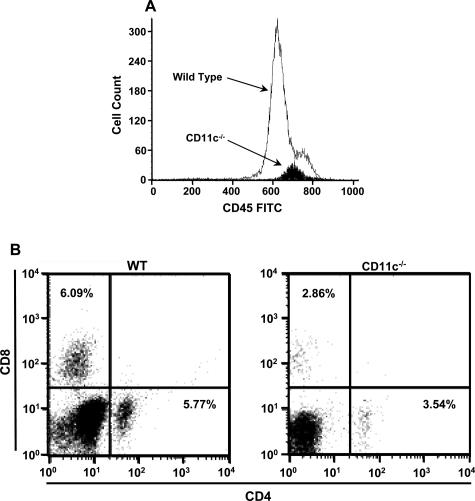
We also analyzed leukocyte infiltration early in EAE development and observed that total CD45+ leukocyte infiltration in the spinal cords of CD11c−/− mice was not different before disease onset (day 10, data not shown), but was substantially reduced during the acute phase of disease (day 15, Figure 3A). Of the leukocytes that did infiltrate the spinal cords of CD11c−/− mice, there were fewer CD4+ and CD8+ T cells compared with wild type (Figure 3B). CD4+ and CD8+ T-cell infiltration was reduced 39 and 53%, respectively, in CD11c−/− mice compared with controls. However, when normalized for the differences in overall CNS infiltration between the two groups, CD4+ and CD8+ T-cell infiltration was reduced 94.5 and 95.8%, respectively, in CD11c−/− compared with wild-type mice. These data demonstrate that the absence of p150/95 significantly reduces trafficking of leukocytes to the CNS. The reduced trafficking of CD11c−/− leukocytes was not attributable to changes in expression of the other β2-integrins (data not shown).
Figure 3.
Leukocyte subset infiltration in the spinal cord of CD11c−/− mice with EAE is reduced compared with control mice. A: Leukocytes isolated from spinal cords of control (n = 5) and CD11c−/− mice (n = 5) as described in Materials and Methods were immunostained for CD45. The infiltration of CD45+ leukocytes at day 15 after immunization was markedly reduced in CD11c−/− mice compared with controls. B: Leukocytes isolated from spinal cords of control (n = 5) and CD11c−/− mice (n = 5) as described in Materials and Methods were immunostained for CD4 and CD8. The results shown are from cells pooled within each group of mice.
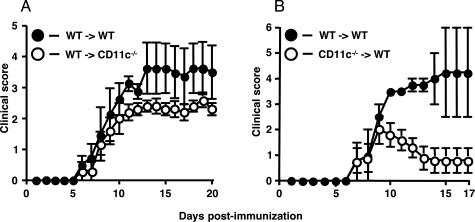
Transfer of Wild-Type MOG-Sensitized T Cells to CD11c−/− Mice Modestly Attenuates Transferred EAE, Whereas CD11c−/− MOG-Sensitized T Cells Induce Mild, Monophasic EAE
We also induced EAE by adoptively transferring MOG-sensitized T cells from wild-type mice to CD11c−/− mice. Onset of EAE in CD11c−/− recipient mice was identical to control transfers and similar to the course of EAE observed during active EAE (Figure 4A, Table 2). The overall severity of disease as assessed by cumulative disease index was significantly lower in CD11c−/− recipient mice (48.1 versus 28.4; P < 0.0001, Wilcoxon signed-rank test). To determine whether p150/95 deficiency on antigen-specific T cells would result in attenuated disease, we performed transferred EAE using MOG-sensitized T cells from CD11c−/− mice (Figure 4B, Table 2). Wild-type mice receiving CD11c−/− T cells developed EAE at the same time as control transfers; however, the disease peaked 3 days after onset of symptoms and remitted to a significantly milder form of disease (cumulative disease index: 35.5 versus 12.5; P = 0.002, Wilcoxon signed-rank test).
Figure 4.
The clinical course of adoptively transferred EAE is attenuated in CD11c−/− mice. A: Transferred EAE was induced in wild-type (n = 5) and CD11c−/− mice (n = 5) mice by injecting encephalitogenic T cells (∼5 × 106) derived from wild-type mice with active EAE. Results shown are the daily mean clinical score from two separate experiments. B: Transferred EAE was induced in wild-type (n = 5) mice by injecting encephalitogenic T cells (∼5 × 106) derived from CD11c−/− mice with active EAE. As a control, transferred EAE was induced in wild-type mice (n = 2) by injecting encephalitogenic T cells (∼5 × 106) derived from wild-type mice with active EAE. Results shown are the daily mean clinical score from three separate experiments.
Table 2.
Transferred EAE Symptoms in Wild-Type Mice and CD11c−/− Mice
| Mice | CDI* | Disease onset† | Disease incidence‡ |
|---|---|---|---|
| WT > WT, n = 4 | 41.8 | 9.3 days | 100 |
| WT > CD11c−/−, n = 5 | 28.1 | 9.4 days | 100 |
| WT > WT, n = 2 | 35.5 | 8.5 days | 100 |
| CD11c−/− > WT, n = 5 | 12.5 | 8 days | 80 |
Cumulative disease index is the mean of the sum of daily clinical scores observed between days 0 and 20 (WT > CD11c−/− experiments) or 0 and 17 (CD11c−/− > WT experiments).
Disease onset is defined as the 1st day of 2 consecutive days with a clinical score of two or more.
Disease incidence is defined as the percent of mice that displayed any clinical signs of disease.
CD11c−/− T Cells Proliferate Comparably but Have an Altered Cytokine Profile Compared with Wild-Type T Cells
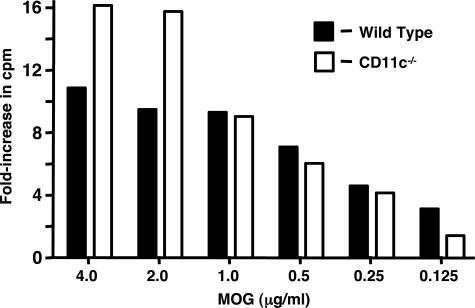
To test the possibility that attenuated active and transferred EAE in CD11c−/− mice could be attributable to impaired T-cell proliferation, we performed in vitro proliferation assays as previously described.37 Stimulation of MOG-sensitized T cells from wild-type and CD11c−/− mice with various concentrations of MOG revealed no overall significant difference in proliferation (Figure 5; P = 0.64, unpaired t-test). Interestingly, at the highest MOG peptide concentrations (2 and 4 μg/ml), T cells from CD11−/− mice proliferated significantly more than those from control mice (P = 0.009, unpaired t-test). The increased T-cell proliferation seen in CD11c−/− mice, using the higher concentrations of MOG peptide, is consistent with a nearly twofold increase in IL-2 production observed on in vitro restimulation of splenic T cells from CD11c−/− mice compared with control (Figure 6A). The levels of several proinflammatory cytokines produced by CD11c−/− T cells (including IFN-γ, tumor necrosis factor-α, and IL-17) were markedly lower, although IL-12 levels were elevated more than 1.5-fold relative to control mice (Figure 6A). The production of anti-inflammatory cytokines such as IL-4, IL-10, and transforming growth factor-β by CD11c−/− T cells was comparable or only modestly reduced compared with control mice. We also examined for the production of IFN-γ by CD4+ and CD8+ T cells in the spinal cord of wild-type and CD11c−/− mice during the acute phase of EAE development (15 days after infection) (Figure 6B). Surprisingly, we observed essentially no IFN-γ-producing CD4+ and CD8+ T cells that infiltrated the spinal cords of CD11c−/− mice compared with controls. In contrast, CD11c−/− splenic T cells readily produced IFN-γ at the same time period after induction (Figure 6A).
Figure 5.
CD11c−/− T cells proliferate comparably to wild-type T cells. Encephalitogenic T cells enriched by nylon-wool adherence from the spleens of wild-type (n = 4) or CD11c−/− mice (n = 4) undergoing active EAE, or T cells from healthy controls (naïve cells), were co-cultured with irradiated splenic APCs plus MOG peptide (0.125 to 4 μg/ml). The cells were pulsed with [3H]thymidine and harvested at 18 hours for determination of radioisotope incorporation. The results shown are expressed as the mean + SEM of fold induction of wild-type or CD11c−/− T-cell proliferation relative to background proliferation.
Figure 6.
Splenic CD11c−/− T cells produce a unique repertoire of cytokines during EAE. A: Encephalitogenic T cells enriched by nylon-wool adherence from the spleens of wild-type (n = 4) or CD11c−/− mice (n = 4) undergoing active EAE (day 15) were co-cultured with irradiated splenic APCs from naïve donors and stimulated with MOG peptide (1 μg/well). Supernatants were collected 48 hours after stimulation and assayed by enzyme-linked immunosorbent assay to quantitate production of each cytokine. Cytokine production by cultures of wild-type and CD11c−/− cells is reported as the mean ± SEM in picograms per milliliter. The mean value for each cytokine is shown above the bar. B: Production of IFN-γ in CD4+ and CD8+ T cells isolated from the spinal cords of control and CD11c−/− mice with active EAE. Leukocytes isolated from spinal cords of control (n = 5) and CD11c−/− mice (n = 5) as described in Materials and Methods were immunostained for CD4, CD8, and IFN-γ. The data shown are derived from gating on IFN-γ-producing cells. The results shown are from cells pooled within each group of mice.
Discussion
The results we report here demonstrate that p150/95 plays an important role in the progression of the inflammatory events leading to demyelination and paralysis during EAE. The mechanisms underlying CD11c-mediated protection in EAE are difficult to readily decipher attributable, in part, to poor understanding of the major role(s) of p150/95 in the host immune response. Functionally, p150/95 is best known for its contribution to phagocytosis of bacteria (particularly Mycobacterium) and apoptotic cells.14,27,28,29,30,31 Resting and activated microglia as well as infiltrating macrophages all express p150/95, and expression increases on activation of these phagocytic cells.18,19,20,21,22 This expression pattern of p150/95 on macrophages and microglia, combined with the reduced demyelination observed in the spinal cords of CD11c−/− mice (Figure 2), supports a role for p150/95 in promoting myelin damage and subsequent neuronal injury during EAE. However, to date, no studies using antibodies to block p150/95-mediated phagocytosis in the CNS have been performed, unlike for Mac-1 in which both in vitro and in vivo studies have clearly established a role for this adhesion molecule in this process.38,39,40,41,42 Studies directly addressing the role of p150/95 in phagocytosis in demyelinating disease and other CNS inflammatory diseases are required to enhance our understanding of this potentially important aspect of p150/95 biology.
The contribution of p150/95-mediated phagocytosis to demyelination may be minor given that leukocyte infiltration into the CNS of CD11c−/− mice is substantially lower than that seen in control mice (Figure 3). There is little experimental support for p150/95 as an adhesion molecule important in leukocyte migration. Numerous studies have documented a role for p150/95 in both monocyte/endothelium interactions using static in vitro adhesion assays and in conjugate formation between cytotoxic T cells and target cells of various types.14,18,32,33,34,35 However, in vivo adhesion studies investigating the contribution of p150/95 in mediating leukocyte/endothelial interactions under normal or inflammatory conditions are lacking. Thus the importance of p150/95 in leukocyte trafficking remains primarily unexplored. Nevertheless, our results provide strong indirect evidence suggesting that p150/95 may be important for cellular trafficking into the CNS.
p150/95 expression increases on activated B and T cells, particularly cytotoxic T cells, the latter of which suggests a role in adhesive events leading to target cell killing15,16,17,32,35 These studies also raise the possibility that p150/95 contributes to the development and or stability of the immunological synapse along with LFA-1. The absence of p150/95 on either T cells or antigen-presenting cells (APCs) could result in reduced T-cell activation and an altered pattern of cytokine production, a finding we obtained with CD11c−/− mice in EAE (Figure 6). Despite the unusual pattern of cytokines produced by CD11c−/− splenic T cells during EAE, there was no significant reduction in the antigen-specific proliferative capacity of T cells derived from these mice as determined by in vitro assays (Figure 5). Nevertheless, the markedly attenuated EAE observed when CD11c−/− T cells were transferred to control mice (Figure 4) indicates that loss of this β2-integrin on T cells is more critical to disease development than loss of expression on APCs and other leukocyte subsets. This finding coupled with the development of attenuated EAE when control T cells were transferred to CD11c−/− mice, argues that the expression of p150/95 on dendritic cells is not critical for the development of EAE. p150/95 is the common cell surface marker for the identification of dendritic cells, although not all dendritic cells appear to express p150/95.43 More importantly, little information is available for a functional role for p150/95 on dendritic cells. Nevertheless, the absence of p150/95 on either APCs or T cells may alter the extent and rate of activation events for both cell types leading to the attenuated disease phenotype we report here.
Our data combined with previous studies show that three of the four β2-integrins play critical, nonredundant roles in demyelinating disease. Numerous reports have shown that treatment of mice with anti-CD11a (LFA-1) and CD11b (Mac-1) antibodies attenuates or prevents the development of EAE.44,45,46,47 In support of these antibody studies, we have observed markedly attenuated MOG-induced EAE using CD11b−/− and CD11a−/− mice6 (K. Dugger, J. Hu, D. Bullard, and S.R. Barnum, unpublished observations). In contrast, the deletion of CD11d (namely α-D) had no effect of the development or progression of EAE,48 although antibodies to CD11d were protective in animal models of spinal cord injury.49,50,51 Taken together, it is clear that LFA-1, MAC-1, and p150/95 contribute uniquely to demyelinating disease, despite their overlapping ligand specificity and expression on leukocytes.
Therapeutic approaches targeting integrin function in neurodegenerative diseases, including demyelinating disease, have been investigated for more than a decade. Antibody-mediated inhibition of several members of both the α4 and β2 integrin families attenuates or prevents EAE.6,38,39,40,44,45,46,52,53,54 Most importantly, anti-α4 integrin antibody has become a major component of the treatment arsenal for relapsing-remitting MS, despite the potentially serious side effects for a small subset of patients.55,56,57,58 The data we present here for p150/95 suggest that members of the β2-integrin family of adhesion molecules, particularly Mac-1 and p150/95, represent a viable therapeutic option for MS. Unlike LFA-1, which is important in trafficking of numerous cell types as well as T-cell activation events, inhibition of Mac-1 and p150/95 may affect a repertoire of functions in demyelinating disease without leaving the host significantly immunocompromised. Given the overlapping functions of Mac-1 and p150/95, deletion of both receptors may result in a complete inhibition of disease similar to that seen when their common ligand intercellular adhesion molecule-1 is deleted.59 Thus, the β2-integrin family members, including p150/95, may offer new therapeutic approaches for demyelinating disease.
Acknowledgments
We thank the University of Alabama at Birmingham Comparative Pathology Laboratory for providing histology services.
Footnotes
Address reprint requests to Dr. Scott R. Barnum, Department of Microbiology, University of Alabama at Birmingham, 845 19th St. S., BBRB/842, Birmingham, AL 35294. E-mail: sbarnum@uab.edu.
Supported by the National Multiple Sclerosis Society (grant RG-3437-A-6) and the National Institutes of Health (NS46032 to S.R.B., RR017009 to D.C.B., and GM08111-18 to J.E.A.).
D.C.B. and X.H. are co-first authors of the article.
Editorial note: A guest editor acted as editor-in-chief for this manuscript. No person at the University of Alabama at Birmingham was involved in the peer review process or final disposition for this article.
References
- Sospedra M, Martin R. Immunology of multiple sclerosis. Annu Rev Immunol. 2005;23:683–747. doi: 10.1146/annurev.immunol.23.021704.115707. [DOI] [PubMed] [Google Scholar]
- Rajan AJ, Gao YL, Raine CS, Brosnan CF. A pathogenic role for gamma delta T cells in relapsing-remitting experimental allergic encephalomyelitis in the SJL mouse. J Immunol. 1996;157:941–949. [PubMed] [Google Scholar]
- Secor VH, Secor WE, Gutekunst CA, Brown MA. Mast cells are essential for early onset and severe disease in a murine model of multiple sclerosis. J Exp Med. 2000;191:813–822. doi: 10.1084/jem.191.5.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmer B, Kieseier B, Cepok S, Hartung HP. New immunopathologic insights into multiple sclerosis. Curr Neurol Neurosci Rep. 2003;3:246–255. doi: 10.1007/s11910-003-0085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens T. The enigma of multiple sclerosis: inflammation and neurodegeneration cause heterogeneous dysfunction and damage. Curr Opin Neurol. 2003;16:259–265. doi: 10.1097/01.wco.0000073925.19076.f2. [DOI] [PubMed] [Google Scholar]
- Bullard DC, Hu X, Schoeb TR, Axtell RC, Raman C, Barnum SR. Critical requirement of CD11b (Mac-1) on T cells and accessory cells for development of experimental autoimmune encephalomyelitis. J Immunol. 2005;175:6327–6333. doi: 10.4049/jimmunol.175.10.6327. [DOI] [PubMed] [Google Scholar]
- Engelhardt B. Immune cell migration across the blood-brain barrier: molecular mechanisms and therapeutic targeting. Future Neurol. 2006;1:47–56. doi: 10.1007/s00702-005-0409-y. [DOI] [PubMed] [Google Scholar]
- Engelhardt B. Molecular mechanisms involved in T cell migration across the blood-brain barrier. J Neural Transm. 2006;113:477–485. doi: 10.1007/s00702-005-0409-y. [DOI] [PubMed] [Google Scholar]
- Hogg N, Takacs L, Palmer DG, Selvendran Y, Allen C. The p150,95 molecule is a marker of human mononuclear phagocytes: comparison with expression of class II molecules. Eur J Immunol. 1986;16:240–248. doi: 10.1002/eji.1830160306. [DOI] [PubMed] [Google Scholar]
- Miller LJ, Schwarting R, Springer TA. Regulated expression of the Mac-1, LFA-1, p150,95 glycoprotein family during leukocyte differentiation. J Immunol. 1986;137:2891–2900. [PubMed] [Google Scholar]
- Miller LJ, Bainton DF, Borregaard N, Springer TA. Stimulated mobilization of monocyte Mac-1 and p150,95 adhesion proteins from an intracellular vesicular compartment to the cell surface. J Clin Invest. 1987;80:535–544. doi: 10.1172/JCI113102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myones BL, Dalzell JG, Hogg N, Ross GD. Neutrophil and monocyte cell surface p150,95 has iC3b-receptor (CR4) activity resembling CR3. J Clin Invest. 1988;82:640–651. doi: 10.1172/JCI113643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenthal PS, Steinman RM. The distinct surface of human blood dendritic cells, as observed after an improved isolation method. Proc Natl Acad Sci USA. 1990;87:7698–7702. doi: 10.1073/pnas.87.19.7698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keizer GD, Te Velde AA, Schwarting R, Figdor CG, De Vries JE. Role of p150, 95 in adhesion, migration, chemotaxis and phagocytosis of human monocytes. Eur J Immunol. 1987;17:1317–1322. doi: 10.1002/eji.1830170915. [DOI] [PubMed] [Google Scholar]
- Postigo AA, Corbi AL, Sanchez-Madrid F, de Landazuri MO. Regulated expression and function of CD11c/CD18 integrin on human B lymphocytes. Relation between attachment to fibrinogen and triggering of proliferation through CD11c/CD18. J Exp Med. 1991;174:1313–1322. doi: 10.1084/jem.174.6.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huleatt JW, Lefrancois L. Antigen-driven induction of CD11c on intestinal intraepithelial lymphocytes and CD8+ T cells in vivo. J Immunol. 1995;154:5684–5693. [PubMed] [Google Scholar]
- Lin Y, Roberts TJ, Sriram V, Cho S, Brutkiewicz RR. Myeloid marker expression on antiviral CD8+ T cells following an acute virus infection. Eur J Immunol. 2003;33:2736–2743. doi: 10.1002/eji.200324087. [DOI] [PubMed] [Google Scholar]
- Anderson DC, Miller LJ, Schmalstieg FC, Rothlein R, Springer TA. Contributions of the Mac-1 glycoprotein family to adherence-dependent granulocyte functions: structure-function assessments employing subunit-specific monoclonal antibodies. J Immunol. 1986;137:15–27. [PubMed] [Google Scholar]
- Akiyama H, McGeer PL. Brain microglia constitutively express beta-2 integrins. J Neuroimmunol. 1990;30:81–93. doi: 10.1016/0165-5728(90)90055-r. [DOI] [PubMed] [Google Scholar]
- Ulvestad E, Williams K, Mork S, Antel J, Nyland H. Phenotypic differences between human monocytes/macrophages and microglial cells studied in situ and in vitro. J Neuropathol Exp Neurol. 1994;53:492–501. doi: 10.1097/00005072-199409000-00008. [DOI] [PubMed] [Google Scholar]
- Ulvestad E, Williams K, Bjerkvig R, Tiekotter K, Antel J, Matre R. Human microglial cells have phenotypic and functional characteristics in common with both macrophages and dendritic antigen-presenting cells. J Leukoc Biol. 1994;56:732–740. doi: 10.1002/jlb.56.6.732. [DOI] [PubMed] [Google Scholar]
- Ponomarev ED, Shriver LP, Maresz K, Dittel BN. Microglial cell activation and proliferation precedes the onset of CNS autoimmunity. J Neurosci Res. 2005;81:374–389. doi: 10.1002/jnr.20488. [DOI] [PubMed] [Google Scholar]
- Bilsland CA, Diamond MS, Springer TA. The leukocyte integrin p150,95 (CD11c/CD18) as a receptor for iC3b. Activation by a heterologous beta subunit and localization of a ligand recognition site to the I domain. J Immunol. 1994;152:4582–4589. [PubMed] [Google Scholar]
- Loike JD, Sodeik B, Cao L, Leucona S, Weitz JI, Detmers PA, Wright SD, Silverstein SC. CD11c/CD18 on neutrophils recognizes a domain at the N terminus of the A alpha chain of fibrinogen. Proc Natl Acad Sci USA. 1991;88:1044–1048. doi: 10.1073/pnas.88.3.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingalls RR, Golenbock DT. CD11c/CD18, a transmembrane signaling receptor for lipopolysaccharide. J Exp Med. 1995;181:1473–1479. doi: 10.1084/jem.181.4.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Fougerolles AR, Diamond MS, Springer TA. Heterogenous glycosylation of ICAM-3 and lack of interaction with Mac-1 and p150,95. Eur J Immunol. 1995;25:1008–1012. doi: 10.1002/eji.1830250422. [DOI] [PubMed] [Google Scholar]
- Schlesinger LS, Horwitz MA. Phagocytosis of Mycobacterium leprae by human monocyte-derived macrophages is mediated by complement receptors CR1 (CD35), CR3 (CD11b/CD18), and CR4 (CD11c/CD18) and IFN-gamma activation inhibits complement receptor function and phagocytosis of this bacterium. J Immunol. 1991;147:1983–1994. [PubMed] [Google Scholar]
- Schlesinger LS, Bellinger-Kawahara CG, Payne NR, Horwitz MA. Phagocytosis of Mycobacterium tuberculosis is mediated by human monocyte complement receptors and complement component C3. J Immunol. 1990;144:2771–2780. [PubMed] [Google Scholar]
- Hirsch CS, Ellner JJ, Russell DG, Rich EA. Complement receptor-mediated uptake and tumor necrosis factor-alpha-mediated growth inhibition of Mycobacterium tuberculosis by human alveolar macrophages. J Immunol. 1994;152:743–753. [PubMed] [Google Scholar]
- Mevorach D, Mascarenhas JO, Gershov D, Elkon KB. Complement-dependent clearance of apoptotic cells by human macrophages. J Exp Med. 1998;188:2313–2320. doi: 10.1084/jem.188.12.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittoni V, Valesini G. The clearance of apoptotic cells: implications for autoimmunity. Autoimmun Rev. 2002;1:154–161. doi: 10.1016/s1568-9972(02)00032-0. [DOI] [PubMed] [Google Scholar]
- Keizer GD, Borst J, Visser W, Schwarting R, de Vries JE, Figdor CG. Membrane glycoprotein p150,95 of human cytotoxic T cell clone is involved in conjugate formation with target cells. J Immunol. 1987;138:3130–3136. [PubMed] [Google Scholar]
- te Velde AA, Keizer GD, Figdor CG. Differential function of LFA-1 family molecules (CD11 and CD18) in adhesion of human monocytes to melanoma and endothelial cells. Immunology. 1987;61:261–267. [PMC free article] [PubMed] [Google Scholar]
- Stacker SA, Springer TA. Leukocyte integrin P150,95 (CD11c/CD18) functions as an adhesion molecule binding to a counter-receptor on stimulated endothelium. J Immunol. 1991;146:648–655. [PubMed] [Google Scholar]
- Beyer M, Wang H, Peters N, Doths S, Koerner-Rettberg C, Openshaw PJ, Schwarze J. The beta2 integrin CD11c distinguishes a subset of cytotoxic pulmonary T cells with potent antiviral effects in vitro and in vivo. Respir Res. 2005;6:70. doi: 10.1186/1465-9921-6-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren B, McCrory MA, Pass C, Bullard DC, Ballantyne CM, Xu Y, Briles DE, Szalai AJ. The virulence function of Streptococcus pneumoniae surface protein A involves inhibition of complement activation and impairment of complement receptor-mediated protection. J Immunol. 2004;173:7506–7512. doi: 10.4049/jimmunol.173.12.7506. [DOI] [PubMed] [Google Scholar]
- Szalai AJ, Nataf S, Hu XZ, Barnum SR. Experimental allergic encephalomyelitis is inhibited in transgenic mice expressing human C-reactive protein. J Immunol. 2002;168:5792–5797. doi: 10.4049/jimmunol.168.11.5792. [DOI] [PubMed] [Google Scholar]
- Brück W, Friede RL. Anti-macrophage CR3 antibody blocks myelin phagocytosis by macrophages in vitro. Acta Neuropathol. 1990;80:415–418. doi: 10.1007/BF00307696. [DOI] [PubMed] [Google Scholar]
- Huitinga I, Damoiseaux JG, Dopp EA, Dijkstra CD. Treatment with anti-CR3 antibodies ED7 and ED8 suppresses experimental allergic encephalomyelitis in Lewis rats. Eur J Immunol. 1993;23:709–715. doi: 10.1002/eji.1830230321. [DOI] [PubMed] [Google Scholar]
- van der Laan LJ, Ruuls SR, Weber KS, Lodder IJ, Dopp EA, Dijkstra CD. Macrophage phagocytosis of myelin in vitro determined by flow cytometry: phagocytosis is mediated by CR3 and induces production of tumor necrosis factor-alpha and nitric oxide. J Neuroimmunol. 1996;70:145–152. doi: 10.1016/s0165-5728(96)00110-5. [DOI] [PubMed] [Google Scholar]
- Brück W. The role of macrophages in Wallerian degeneration. Brain Pathol. 1997;7:741–752. doi: 10.1111/j.1750-3639.1997.tb01060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ME. Phagocytosis of myelin in demyelinative disease: a review. Neurochem Res. 1999;24:261–268. doi: 10.1023/a:1022566121967. [DOI] [PubMed] [Google Scholar]
- Blom B, Spits H. Development of human lymphoid cells. Annu Rev Immunol. 2006;24:287–320. doi: 10.1146/annurev.immunol.24.021605.090612. [DOI] [PubMed] [Google Scholar]
- Gordon EJ, Myers KJ, Dougherty JP, Rosen H, Ron Y. Both anti-CD11a (LFA-1) and anti-CD11b (MAC-1) therapy delay the onset and diminish the severity of experimental autoimmune encephalomyelitis. J Neuroimmunol. 1995;62:153–160. doi: 10.1016/0165-5728(95)00120-2. [DOI] [PubMed] [Google Scholar]
- Kobayashi Y, Kawai K, Honda H, Tomida S, Niimi N, Tamatani T, Miyasaka M, Yoshikai Y. Antibodies against leukocyte function-associated antigen-1 and against intercellular adhesion molecule-1 together suppress the progression of experimental allergic encephalomyelitis. Cell Immunol. 1995;164:295–305. doi: 10.1006/cimm.1995.1173. [DOI] [PubMed] [Google Scholar]
- Kawai K, Kobayashi Y, Shiratori M, Sobue G, Tamatani T, Miyasaka M, Yoshikai Y. Intrathecal administration of antibodies against LFA-1 and against ICAM-1 suppresses experimental allergic encephalomyelitis in rats. Cell Immunol. 1996;171:262–268. doi: 10.1006/cimm.1996.0202. [DOI] [PubMed] [Google Scholar]
- Willenborg DO, Staykova MA, Miyasaka M. Short term treatment with soluble neuroantigen and anti-CD11a (LFA-1) protects rats against autoimmune encephalomyelitis: treatment abrogates autoimmune disease but not autoimmunity. J Immunol. 1996;157:1973–1980. [PubMed] [Google Scholar]
- Adams JE, Webb MS, Hu X, Staunton D, Barnum SR. Disruption of the β(2)-integrin CD11d (α(D)β2) gene fails to protect against experimental autoimmune encephalomyelitis. J Neuroimmunol. 2007;184:180–187. doi: 10.1016/j.jneuroim.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabon PJ, Weaver LC, Dekaban GA. Inhibition of monocyte/macrophage migration to a spinal cord injury site by an antibody to the integrin alphaD: a potential new anti-inflammatory treatment. Exp Neurol. 2000;166:52–64. doi: 10.1006/exnr.2000.7488. [DOI] [PubMed] [Google Scholar]
- Gris D, Marsh DR, Oatway MA, Chen Y, Hamilton EF, Dekaban GA, Weaver LC. Transient blockade of the CD11d/CD18 integrin reduces secondary damage after spinal cord injury, improving sensory, autonomic, and motor function. J Neurosci. 2004;24:4043–4051. doi: 10.1523/JNEUROSCI.5343-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gris D, Marsh DR, Dekaban GA, Weaver LC. Comparison of effects of methylprednisolone and anti-CD11d antibody treatments on autonomic dysreflexia after spinal cord injury. Exp Neurol. 2005;194:541–549. doi: 10.1016/j.expneurol.2005.03.016. [DOI] [PubMed] [Google Scholar]
- Yednock TA, Cannon C, Fritz LC, Sanchez-Madrid F, Steinman L, Karin N. Prevention of experimental autoimmune encephalomyelitis by antibodies against α4β1 integrin. Nature. 1992;356:63–66. doi: 10.1038/356063a0. [DOI] [PubMed] [Google Scholar]
- Baron JL, Madri JA, Ruddle NH, Hashim G, Janeway CA., Jr Surface expression of alpha 4 integrin by CD4 T cells is required for their entry into brain parenchyma. J Exp Med. 1993;177:57–68. doi: 10.1084/jem.177.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brocke S, Piercy C, Steinman L, Weissman IL, Veromaa T. Antibodies to CD44 and integrin alpha4, but not L-selectin, prevent central nervous system inflammation and experimental encephalomyelitis by blocking secondary leukocyte recruitment. Proc Natl Acad Sci USA. 1999;96:6896–6901. doi: 10.1073/pnas.96.12.6896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DH, Khan OA, Sheremata WA, Blumhardt LD, Rice GP, Libonati MA, Willmer-Hulme AJ, Dalton CM, Miszkiel KA, O’Connor PW. A controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2003;348:15–23. doi: 10.1056/NEJMoa020696. [DOI] [PubMed] [Google Scholar]
- Langer-Gould A, Atlas SW, Green AJ, Bollen AW, Pelletier D. Progressive multifocal leukoencephalopathy in a patient treated with natalizumab. N Engl J Med. 2005;353:375–381. doi: 10.1056/NEJMoa051847. [DOI] [PubMed] [Google Scholar]
- Kleinschmidt-DeMasters BK, Tyler KL. Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis. N Engl J Med. 2005;353:369–374. doi: 10.1056/NEJMoa051782. [DOI] [PubMed] [Google Scholar]
- Ransohoff RM. Natalizumab and PML. Nat Neurosci. 2005;8:1275. doi: 10.1038/nn1005-1275. [DOI] [PubMed] [Google Scholar]
- Bullard DC, Hu X, Schoeb TR, Collins RG, Beaudet AL, Barnum SR. Intercellular adhesion molecule-1 expression is required on multiple cell types for the development of experimental autoimmune encephalomyelitis. J Immunol. 2007;178:851–857. doi: 10.4049/jimmunol.178.2.851. [DOI] [PubMed] [Google Scholar]