Abstract
The crucial role played by the myofibroblast in wound healing and pathological organ remodeling is well established; the general mechanisms of extracellular matrix synthesis and of tension production by this cell have been amply clarified. This review discusses the pattern of myofibroblast accumulation and fibrosis evolution during lung and liver fibrosis as well as during atheromatous plaque formation. Special attention is paid to the specific features characterizing each of these processes, including the spectrum of different myofibroblast precursors and the distinct pathways involved in the formation of differentiated myofibroblasts in each lesion. Thus, whereas in lung fibrosis it seems that most myofibroblasts derive from resident fibroblasts, hepatic stellate cells are the main contributor for liver fibrosis and media smooth muscle cells are the main contributor for the atheromatous plaque. A better knowledge of the molecular mechanisms conducing to the appearance of differentiated myofibroblasts in each pathological situation will be useful for the understanding of fibrosis development in different organs and for the planning of strategies aiming at their prevention and therapy.
After tissue injury, fibroblasts differentiate into contractile and secretory myofibroblasts that contribute to tissue repair during wound healing, but that can severely impair organ function when contraction and extracellular matrix (ECM) protein secretion become excessive, such as in hypertrophic scars, scleroderma, and Dupuytren’s disease as well as in heart and kidney fibrosis.1,2,3 Moreover, myofibroblasts present in the so-called stroma reaction of epithelial tumors may promote the progression of cancer invasion.4 Here, we discuss the role of myofibroblasts in causing pathological deformation of two vital organs, liver3 and lung,5 and in contributing to the formation of the atheromatous plaque and restenotic lesions.6,7 Myofibroblast differentiation is a complex phenomenon that follows distinct patterns in different organs. To counteract therapeutically organ dysfunction caused by myofibroblasts, it is crucial to understand the general molecular pathways regulating their evolution and function to distinguish the mechanisms common to all situations from those specific to a given organ and/or disease.
General Mechanisms of Myofibroblast Differentiation and Biological Action
As we shall discuss below, myofibroblasts may have very heterogeneous origins; however, their development follows a well-established sequence of events. In normal conditions, fibroblastic cells exhibit few or no actin-associated cell-cell and cell-matrix contacts and little ECM production.8 After tissue injury, they become activated to migrate into the damaged tissue and to synthesize ECM components1 by cytokines locally released from inflammatory and resident cells9 or from malignant epithelial cells.4 Another important stimulus for this phenotypic transition is the change of the mechanical microenvironment; whereas fibroblasts in intact tissue are generally stress-shielded by the crosslinked ECM, this protective structure is lost in the continuously remodeled ECM of injured tissue.8 In response to mechanical challenge, fibroblasts acquire contractile stress fibers that are first composed of cytoplasmic actins,8 hallmarking the “protomyofibroblast.” Stress fibers are connected to fibrous ECM proteins at sites of integrin-containing cell-matrix junctions10 and between cells via de novo established N-cadherin-type adherens junctions.11 These features closely resemble those of cultured fibroblasts that have been mechanically activated by the rigid plastic substrate, whereas stress fibers do not form on very soft culture substrate hydrogels or in compliant collagen gels (Figure 1).10
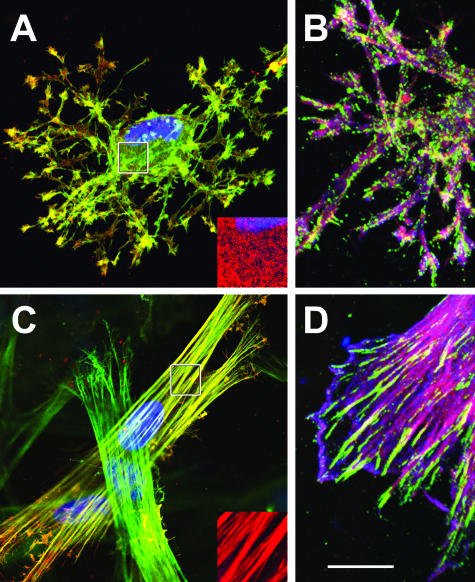
Figure 1.
ECM compliance controls development of the myofibroblast phenotype in three-dimensional collagen gels. Differentiated rat lung myofibroblasts were grown in mechanically restrained collagen gels produced very soft with a concentration of 0.5 mg/ml (A, B) and comparably stiff with 3.5 mg/ml (C, D). Cells were immunostained after 36 hours for α-SMA (A, C: red; B, D: blue), β-cytoplasmic actin (A, C: green; B, D: red), focal adhesion protein vinculin (B, D: green), and nuclei (A, C: blue) and observed by confocal microscopy. Note that cells in soft gels attain a dendritic morphology with cortical actin distribution and point-like small adhesion sites; α-SMA is not organized in stress fibers (A, inset). In stiff collagen, myofibroblasts develop α-SMA-positive stress fibers (C, inset) that terminate in supermature FAs. Bars: 25 μm and 10 μm (insets).
In culture, the protomyofibroblast is a stable phenotype, representing an intermediate step in most in vivo conditions where it proceeds toward the “differentiated myofibroblast” that is characterized by de novo expression of α-smooth muscle actin (α-SMA), its most commonly used molecular marker. Expression of α-SMA in stress fibers confers to the differentiated myofibroblast at least a twofold stronger contractile activity compared with α-SMA-negative fibroblasts in culture.12 It is still unclear how α-SMA generates higher contraction compared with other actin isoforms, but the α-SMA-specific N-terminal amino acid sequence AcEEED plays an important role in this mechanism. Cytoplasmic delivery of this sequence as a peptide selectively removes α-SMA from persisting β-cytoplasmic actin stress fibers and reduces in vivo and in vitro myofibroblast contraction.13
At least three local events are needed to generate α-SMA-positive differentiated myofibroblasts: 1) accumulation of biologically active transforming growth factor (TGF) β1, 2) the presence of specialized ECM proteins like the ED-A splice variant of fibronectin, and 3) high extracellular stress, arising from the mechanical properties of the ECM and cell remodeling activity.8 Mechanoperception is mediated by specialized cell-matrix junctions, called “fibronexus” in vivo and “supermature focal adhesions” (FAs) in vitro.10 Analogously, small N-cadherin-type cell-cell adhesions develop into larger OB-cadherin (cadherin-11)-type junctions during generation of the differentiated myofibroblast in vitro and in vivo.11
It has become increasingly accepted that ECM rigidity determines the size of the cell’s anchors, which in turn limits the level of tension generated within stress fibers.10 Only when substrate stiffness permits formation of supermature FAs (8 to 30 μm long), and thus generation of approximately fourfold greater stress compared with the usual FAs (2 to 6 μm long), does α-SMA become incorporated into pre-existing β-cytoplasmic actin stress fibers; hence, α-SMA can be considered a mechanosensitive protein14,15 (Figure 1). The myofibroblast cytoskeleton may function as a mechanotransducer translating to biochemical signals involving tyrosine phosphatase and kinase pathways.16 Mechanical force-induced p38 phosphorylation seems to be dependent on an α-SMA stress fiber-dependent pathway that uses a feed-forward amplification loop to synergize force-induced α-SMA expression with p38 activation.15 Cell adhesion signaling via focal adhesion kinase may represent another central pathway through which biochemical and biophysical ECM signals as well as soluble growth factor signals are integrated.14,17 The main myofibroblast inducer TGFβ1 up-regulates expression of fibronectin and its integrin receptors in lung fibroblasts; this is closely linked to the activation/phosphorylation of focal adhesion kinase essential for the induction of myofibroblast differentiation.17 At the end of tissue repair, the reconstructed ECM again takes over the mechanical load and myofibroblasts disappear by massive apoptosis8; stress release is a powerful promoter of myofibroblast apoptosis in vivo.18 Thus, interrupting the mechanical feedback loop of myofibroblast contraction and gradually increasing ECM tension at the level of stress perception (ie, cell-ECM contacts) is one promising strategy to prevent tissue contracture.
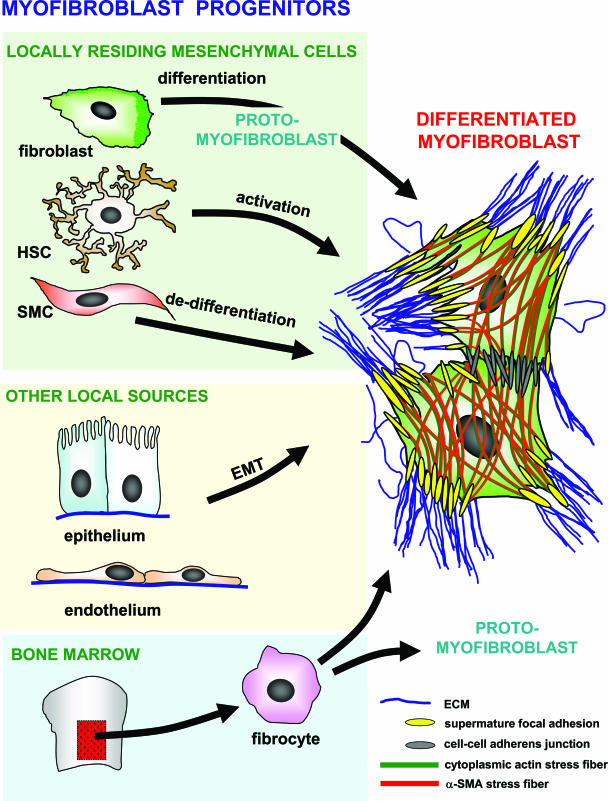
An alternative strategy to decrease tissue contracture consists in preventing myofibroblast formation in the first place, requiring knowledge of the myofibroblast origin. Depending on the type of tissue to be remodeled, myofibroblast precursor cells are recruited from different sources; among these, locally residing fibroblasts seem to be the most common.1 Other mesenchymal cells that are discussed to serve as myofibroblast progenitors are pericytes and smooth muscle cells (SMCs) from the vasculature; they seem to play an important role during vessel repair7 and have been suggested to contribute to fibrosis in scleroderma.19 In addition, bone marrow (BM)-derived circulating cells known as fibrocytes20 have been suggested to represent an alternative source for myofibroblasts during skin wound healing and in liver, lung, and kidney fibrosis, as well as in the stroma reaction to epithelial tumors.21,22,23,24 Other studies do not support this view as further discussed below.25,26 Finally, myofibroblasts have been shown to derive from epithelial-mesenchymal transition (EMT).27,28,29 Thus, damaged organs seem to recruit myofibroblast precursors from several sources to satisfy the temporarily high demand of cells with tissue remodeling activity (Figure 2).
Figure 2.
One cell, multiple origins. Differentiated myofibroblasts are characterized by increased production of ECM proteins and by the development of α-SMA-positive stress fibers that are connected with the ECM at sites of supermature FAs and between cells via adherens junctions. The main myofibroblast progenitor after injury of different tissues seems to be the locally residing fibroblast, which transiently differentiates into a protomyofibroblast, characterized by α-SMA-negative stress fibers. In the liver, myofibroblasts are additionally recruited from HSCs that follow an activation process and from epithelial cells that undergo EMT. In the lung, endothelial-to-mesenchymal transition may provide another mechanism to generate myofibroblasts. During atheromatous plaque formation, de-differentiating SMCs (ie, that lose late SMC markers) from the media are suggested to be the major source of myofibroblastic cells. The relative contribution of BM-derived circulating fibrocytes to the formation of differentiated myofibroblasts in different fibrotic lesions is unclear at present; it is conceivable that fibrocyte transdifferentiation terminates at the protomyofibroblast stage.
Origin and Role of the Myofibroblast in Pulmonary Fibrosis
The presence of stable protomyofibroblasts in normal alveolar septa is well established. The repair process in response to lung injury is characterized by neoformation of differentiated myofibroblasts. In view of its many characteristics that encompass the notable features of fibrosis, such as the elaboration of ECM and expression/activation of TGFβ1,30,31 the persistence of the myofibroblast is thought to be of significance in the propagation of fibrosis with evolution to terminal end-stage fibrotic lung disease. Early studies of the origin of the myofibroblast in lung injury and fibrosis suggest several possibilities based on observations of its cytoskeletal phenotype, tissue localization, and in vitro studies. Based on evidence that myofibroblasts arise de novo and on the kinetics of the induction of α-SMA expression, the perivascular and peribronchiolar adventitial fibroblasts are suggested as precursors.30 However, circulating fibrocytes (expressing CD45, CD34, collagen I, and CXCR4) have been reported to migrate to sites of tissue injury and differentiate into myofibroblasts.20,32 Furthermore, other studies using BM chimeric mice, in which the donated BM cells express a marker protein for tracking purposes, as well as human transplant studies, demonstrate that BM-derived progenitors can give rise to lung fibroblasts.25,33 However, the ability of BM-derived fibroblasts to differentiate to myofibroblasts cannot be demonstrated in some studies.25,26 Moreover, another study using α-SMA promoter-driven green fluorescent protein BM chimeric mice indicates that the BM is not a source of progenitor cells for α-SMA-expressing cells.34 Thus, the evidence for BM derivation of myofibroblasts in lung fibrosis is controversial, suggesting potentially multiple origins, including intrapulmonary precursors. Additional possibilities for intrapulmonary precursors are suggested by evidence of both endothelial to mesenchymal transition and EMT. Endothelial cells as a source of α-SMA-expressing mesenchymal cells have been shown in the development of the vasculature and when they are stimulated with TGFβ1 in vitro.35 Derivation from epithelial cells via EMT has been suggested recently by both in vitro and in vivo studies,28,36 but this could not be demonstrated in another study.37 The relative contribution by these different potential sources of myofibroblasts requires further study.
The mechanism underlying the genesis of the myofibroblast is complex; here, the focus is on downstream effects of myofibroblast-modulating factors on α-SMA transcription, which is particularly well studied in lung fibroblasts. With respect to the Smad signaling pathway, the presence of a Smad3-binding element is essential for myofibroblast differentiation.38,39 However, regulation of the α-SMA gene is more complex and in many respects different from that in SMCs.16,38,39 Additional transcription factors, including C/EBPβ (CCAAT/enhancer-binding protein β), GKLF (gut-enriched Krüppel-like factor), Sp1/Sp3, c-myb, and the downstream effector component of Notch signaling, have been implicated to regulate this gene in a complex and interactive manner.39,40,41,42,43 In addition to inducers, suppressors such as the liver-enriched inhibitory protein isoform of C/EBPβ may serve to keep the precursor fibroblast in an undifferentiated state under normal homeostasis. Epigenetic regulation is implicated by evidence that inhibitors of DNA methylation or histone deacetylation suppress myofibroblast differentiation in the liver.44 Because differentiation is usually accompanied by activation of gene expression, this implies that myofibroblast differentiation is actively suppressed in the quiescent precursor cell by products of certain genes whose expression is suppressed by DNA methylation and deacetylated (or poorly acetylated) histones. Further elucidation is required to understand fully the mechanisms involved in the de novo genesis of the myofibroblast in pulmonary fibrosis.
The role of the myofibroblast in pulmonary fibrosis can be extrapolated from its known functional activities in vivo and in vitro. Early observations focus on the expression of α-SMA in prominent stress fibers, suggesting a role in tissue contractility or compliance. The significance of this α-SMA expression, however, seems to extend beyond these mechanical properties, with evidence pointing to important roles in modulating signal transduction and regulation of gene expression, including ECM components.13,15,45,46 Indeed, the myofibroblast is found in abundance in areas of high ECM expression and represents the predominant source of heightened ECM and cytokine gene expression.30 It is a factor in alveolar epithelial apoptosis, denudation, and retardation of epithelial regeneration.47 Thus, in addition to its potential contribution to reduction in lung tissue compliance, the myofibroblast is likely to play significant roles in promoting ECM deposition, release of inflammatory mediators, and epithelial injury, all of which are considered to be key factors in perpetuating the cycle of injury and fibrosis.
The fate of recruited/activated myofibroblasts in injured tissues may ultimately determine whether normal healing occurs or progression to end-stage fibrosis ensues. Resolution with myofibroblast apoptosis would terminate progression; however, this would be countered by persistence of TGFβ1 expression and ECM deposition, which promote the prosurvival/anti-apoptotic phenotype.48,49 TGFβ1 can induce p38 mitogen-activated protein kinase pathway activation with subsequent activation of the prosurvival phosphatidylinositol 3-kinase-AKT pathway.49 Interestingly, deficiency in PTEN, a phosphatidylinositol 3-kinase-AKT pathway inhibitor, is associated with increased myofibroblast differentiation.50 Thus, in addition to promoting myofibroblast differentiation, combinatorial activation of the adhesion-dependent focal adhesion kinase pathway and the soluble growth factor-mediated AKT pathway confers anoikis/apoptosis resistance to TGFβ1-differentiated myofibroblasts.51 Finally, selective susceptibility of myofibroblasts to nitric oxide-induced apoptosis has been reported in vitro.48 Thus the additive effects of reduced growth factor expression, increased ECM turnover, and nitric oxide generation may set the stage for triggering of myofibroblast apoptosis during the resolution of tissue repair and remodeling. However, mesenchymal cells isolated from the lungs of patients with persistent acute respiratory distress syndrome acquire stable alterations in prosurvival signaling and resistance to apoptosis.52 The importance of such a phenotype to fibrosis is suggested by evidence that pharmacological intervention to inhibit prosurvival focal adhesion kinase and Akt signaling pathways reduces myofibroblast presence and confers protection from fibrosis following lung injury in mice.53 Future studies into the physiological trigger(s) for myofibroblast apoptosis and mechanisms for the stable/durable acquisition of apoptosis resistance under pathological contexts will probably lead to identification of novel, more effective therapies for chronic fibrotic diseases.
Origin and Role of the Myofibroblast in Liver Fibrosis
Fibrosis is the wound healing response of the liver to toxic, infectious, or metabolic agents that is characterized by disruption of the hepatic architecture, associated with increased expression of collagen, proteoglycans, and glycoproteins.54 De novo formation of differentiated myofibroblasts is thought to be primarily responsible for this excessive ECM production; hence, delineating the mechanisms of myofibroblast activation seems indispensable for designing rational therapeutic strategies to inhibit the fibrogenic process leading to cirrhosis.3 Over the last 3 decades, several distinct myofibroblast precursor cells and subpopulations have been described in the fibrotic liver that all share similar ultrastructural and molecular characteristics but may exhibit specific aspects according to the respective pattern of fibrosis.55
The most accepted myofibroblast progenitors in the liver are hepatic stellate cells (HSCs) located along each sinusoid, between the centrolobular vein and the portal tract.55,56 In normal liver, HSCs represent the major reservoir of vitamin A in the human body; during liver injury, HSCs become activated and differentiate into myofibroblasts in response to a variety factors. Reactive oxygen species are probably the principal initiators of this transdifferentiation process by activating proinflammatory and profibrogenic factors57 that promote HSC activation such as monocyte chemoattractant protein-1, insulin-like growth factor, fibroblast growth factor, epidermal growth factor, interleukin-6, and leptin.58,59 Concomitantly, HSCs up-regulate the expression of key inflammatory receptors, including intercellular adhesion molecule-1 and chemokine receptors, as well as receptors mediating lipopolysaccharide signaling such as Toll-like receptor 4.60 TGFβ1, produced by Kupffer cells, endothelial cells, hepatocytes, bile duct epithelial cells, and by HSCs in an autocrine manner, is the most potent profibrogenic cytokine-activating HSCs.61 In addition, alteration of the mechanical properties of the ECM during progression of liver injury plays a crucial role in the acquisition and maintenance of the myofibroblastic phenotype.62
The control of gene expression is a major aspect of HSC activation; similar to adipocytes, quiescent HSCs express high levels of the nuclear receptor peroxisome proliferator-activated receptor γ, which is lost, however, during myofibroblast differentiation.63 Inducing peroxisome proliferator-activated receptor γ transcriptional control inhibits HSC activation, suggesting that peroxisome proliferator-activated receptor γ repression is a key step in the acquisition of the myofibroblast phenotype.64 Likewise, the LIM homeodomain protein Lhx2 seems to repress HSC activation because HSCs in normal liver of Lhx2−/− mice constitutively develop the myofibroblastic phenotype.65 On the contrary, the Krüppel-like factor-6 is induced as an immediate-early gene during HSC activation and is involved in the transcriptional control of target genes such as TGFβ1, its receptors, and contractile cytoskeletal proteins.66
It has been postulated that the exaggerated contraction of activated HSCs increases intrahepatic resistance after injury and contributes to portal hypertension. In normal liver, HSCs reside in the space of Disse in close contact with sinusoidal endothelial cells and hepatocytes. The anatomical features of HSCs are remarkably similar to those of pericytes, which regulate capillary blood flow via pericapillary constriction.67 Interestingly, ex vivo liver perfusion induces HSC activation, expression of α-SMA, and significant changes in the perisinusoidal ECM, confirming the role of these cells in the regulation of sinusoidal blood pressure.68 Thus, regulation of HSCs contractility represents an important potential target of therapeutic intervention for portal hypertension.
In addition to HSCs, other resident cells have recently been described as sources of liver myofibroblasts using different animal models of liver fibrosis: 1) bile duct ligation, 2) CCl4 intoxication, 3) excessive alcohol administration, and 4) viral infection.55 After bile duct ligation, myofibroblasts derive from portal fibroblasts that reside in the connective tissue around vessels and biliary structures.69 In chronic viral hepatitis, fibrotic extensions begin at the branching point of the preterminal portal tract bridging the neighboring portal area; they are the consequence of ECM deposition by α-SMA-positive myofibroblasts derived from portal fibroblasts and by another set of fibrogenic cells present at the interface between portal tract and the parenchyma.70 A third myofibroblast subpopulation seems to originate from second-layer fibroblasts located around the centrolobular vein. Second-layer fibroblasts have been suggested to differentiate into ECM-producing myofibroblasts in the liver of alcohol-fed baboons, causing typical alcoholic-type fibrosis.71 Indeed, both alcoholic and nonalcoholic steatohepatitis-activated HSCs and second-layer fibroblasts contribute to the early fibrotic changes that are concentrated in the centrolobular vein area around sinusoids and hepatocytes with a typical chicken-wire pattern.70
HSCs and portal fibroblasts similarly express intercellular adhesion molecule, vascular cell adhesion molecule, desmin, vimentin, collagen type IV, and fibronectin.70 Expression of fibulin-2 and interluekin-6 was found only in cultured portal fibroblast, whereas CD95L, α2-macroglobulin, P100, and reelin are restricted to HSCs.69 Interestingly, cellular retinol binding protein-1 (CRBP-1) is expressed in HSC and up-regulated during activation. In contrast, CRBP-1 is absent in portal fibroblasts, but in culture these cells may develop both CRBP-1 and α-SMA.72 Fibulin-2-positive cells can contaminate HSC cultures and transdifferentiate into myofibroblasts in vitro.73 These vitamin A-negative myofibroblasts differ from HSC 1) in their mechanism of undergoing CD95-mediated apoptosis, 2) in their response to tumor necrosis factor-α and insulin-like growth factor-1, and 3) in the absence of the HSC markers desmin, P100, and α2-microglobulin.74,75 cDNA microarray analysis identified six novel representative genes in vitamin A-negative myofibroblasts that seem to be scattered around fibrotic septa and in parenchyma: Avpr1a, Sfrp4, gremlin, osteopontin, Colα3(V), and lumican.75
After CCl4 injury, approximately 33% of liver myofibroblasts express markers typically found in BM-derived cells such as intercellular adhesion molecule, CCR5, and CD40, suggesting a fibrocyte origin.76 In humans transplanted with sex-mismatched organs or receiving a BM transplant, BM-derived myofibroblasts were described in the fibrotic reaction of the liver.22 Kisseleva and coworkers,26 using chimeric mice transplanted with BM from collagen α1(I)-green fluorescent protein reporter mice, reported that in response to bile-duct induced liver injury, α-SMA-positive-differentiated myofibroblasts do not originate from circulating fibrocytes, despite the localization of these cells at the site of injury and their participation to the fibrotic process. EMT is another important source of liver myofibroblasts as demonstrated in bile duct ligation-induced fibrosis.29,77 Myofibroblasts have been suggested to derive from bile duct epithelium, which coexpresses epithelial cytokeratin-19 and α-SMA and also produces type I collagen. Furthermore, bile duct EMT leading to myofibroblast formation is induced in vitro with TGFβ1, indicating that EMT represents a potential avenue to generate myofibroblasts in response to fibrogenic stimuli.29
Besides their role in the fibrogenic process and in regulation of blood flow, liver myofibroblasts are also involved in stromal response to hepatic tumors.4 Recently, it has been shown that liver myofibroblasts secrete ADAM-9S, a family member of transmembrane proteins with disintegrin and metalloprotease domains that therefore have both cell-adhesive and protease activities. These invasion-promoting activities suggest that ADAM-9S seems to represent an important mediator of tumor-stroma interaction and a determinant of cancer cell ability to invade and colonize the liver.78
Origin and Role of the Myofibroblast in Atheromatous Plaque Evolution
SMCs originating from the media contribute importantly to atheroma plaque formation; during this process, SMCs dedifferentiate, and the question of their potential myofibroblastic nature has been raised.7 Presently, the most accepted sequence of events leading to atherosclerotic plaque formation implies the establishment of a chronic inflammation process within the arterial intima; this is stimulated by several factors among which oxidized low density lipoproteins are the most important.79 In addition to inflammatory cells such as macrophages and lymphocytes, the main constituent of the plaque fibrotic tissue is the SMC that contributes most ECM components, eg, collagen types I and III.80 As in all chronic inflammatory situations, the fibrotic component predominates within the plaque. Here, fibrosis can cause thrombotic complications following endothelial loss because of excessive production of cytokines and of proteolytic enzymes by resident cells.81 However, fibrosis has also been shown to represent an efficient protective barrier against complications when it forms the so-called fibrous cup over the necrotic core.80 Altogether these features of the plaque resemble those of a chronic fibrotic lesion, where excessive tissue remodeling is one of the main characteristics.1
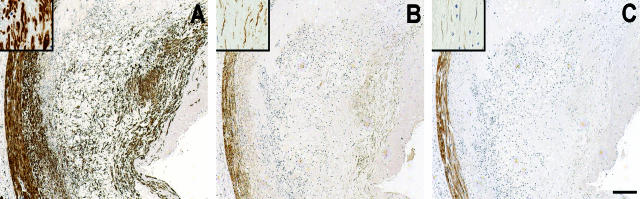
A variety of cell types are discussed to contribute to the remodeling of injured arteries and to plaque formation, including local sources like SMCs from the media and adventitial fibroblasts6,82 as well as circulating BM-derived cells.83 SMCs and pericytes have been suggested as myofibroblast precursors during the stroma reaction accompanying epithelial malignancies.4 Only recently has this possibility been systematically investigated during the evolution of human coronary atherosclerotic plaque and restenotic lesion using markers of early and late SMC differentiation.7 It is well accepted that myofibroblasts share with SMCs the expression of α-SMA, which is considered a early differentiation marker of vascular SMCs.84 Unlike SMCs, however, myofibroblasts express relatively low amounts of smooth muscle myosin heavy chain and do not express smoothelin, a late marker of SMC differentiation.85 During all stages of coronary lesions, including mildly stenotic plaques, highly stenotic stable plaques and erosions, and restenotic lesions, fusiform cells within the intima are positive for α-SMA, express very low amounts of smooth muscle myosin heavy chain, and do not express smoothelin.7 In contrast, SMCs of the media beneath the plaque, albeit hypotrophic, maintain significant expression of all three above-mentioned SMC markers7 (Figure 3). Although the possibility that plaque myofibroblasts derive from adventitial fibroblasts cannot be excluded,6,82 these results support the assumption that SMCs from the media acquire the phenotypic features of myofibroblasts during the migratory and replicative process occurring in plaque formation. Recent work supports the local origin of plaque SMCs in a mouse model of spontaneously arising atheromatous lesions.86
Figure 3.
Cytoskeletal protein expression in a coronary artery atheromatous plaque classified as erosion. Coronary arteries were immunostained for α-SMA (A), smooth muscle myosin heavy chains (B), and smoothelin (C). Insets highlight regions of intimal thickening at higher magnification. Intimal SMCs express high amounts of α-SMA, very low amounts of smooth muscle myosin heavy chains, and no smoothelin, indicating their modulation toward the myofibroblastic phenotype. Note that the media express the three proteins similarly in all cases. Bars: 250 μm and 25 μm (insets).
SMC-to-myofibroblast transition becomes relevant in view of recent work indicating that during fibrotic situations, myofibroblasts develop the capacity of producing a long-lasting tension essentially regulated at the level of Rho/Rho kinase-mediated inhibition of myosin light chain phosphatase, compared with the usual contraction-relaxation activity depending on Ca2+-induced phosphorylation of myosin light chain kinase taking place in SMCs.87 Myofibroblast-generated tension is instrumental for tissue remodeling and deformation during fibrocontractive diseases and could play a role in deformation and fissuration of the plaque, thus contributing to the onset of complications. Interestingly, human and pig intimal myofibroblasts, in contrast to media SMCs, express S100A4,88 a protein of the S100 family that has been shown to be implicated in cancer cell migration.89 Moreover, S100A4 seems to be implicated in cultured SMC-derived myofibroblast replication and motility.88 These results suggest that S100A4 represents a hitherto unavailable marker of SMC-to-myofibroblast phenotypic transition and an in vivo marker of activated intimal SMCs. The question remains whether S100A4-positive plaque myofibroblasts derive from a distinct SMC phenotype, which is consistent with the concept of SMC phenotypic heterogeneity that has been validated in several species, including human.90
Conclusion and Perspectives
The presence of myofibroblasts is well established in few normal tissues, such as alveolar septa, intestinal pericryptal cells, and bone marrow stroma, but its function here is little explored.8 Even less is known about the role of myofibroblasts during embryological development, despite their characterization in several developing organs.8 In contrast, in situations when connective tissue or parenchymal repair are needed, the above-presented data (together with those reported in the literature concerning the healing of organs or tissues not covered in this review1) point to the myofibroblast as the primordial emergency cell contributing to tissue remodeling. Myofibroblasts accomplish this task through synthesis and organization of ECM as well as through force production. Over the years, it has become evident that myofibroblasts arise from a variety of sources, according to the involved organ and the physiological or pathological situation.8 Most commonly, they differentiate locally from fibroblastic cells that may show distinct biological features, thus supporting the concept of fibroblastic phenotypic heterogeneity; they are also produced through transdifferentiation of other mesenchymal or epithelial cells. Finally, the notion that they can derive from blood-borne cells is now established. This large spectrum of precursors (Figure 2) further underlines the crucial function of the myofibroblast in maintaining tissue homeostasis and may furnish, at least in part, an explanation to the well-known heterogeneity of the myofibroblastic phenotype that has been described in different lesions.91
Although it seems that TGFβ1 together with mechanical stress is playing an important role in fibrosis development and evolution, much less is known about factors inhibiting myofibroblast activities and thus controlling fibrosis. Interferon-γ has been shown to exert such an action, possibly through its anti-TGFβ1 effect.61 The α-SMA N-terminal peptide AcEEED reduces force generation by the myofibroblast and exerts an antifibrotic activity probably through its capacity to displace α-SMA from stress fibers.13 Moreover, reducing intracellular tension by interfering with cell-ECM adhesions and/or with ECM compliance prevents development of the myofibroblast.10 Utilization of these tools and finding of new tools capable of controlling myofibroblast function will be very useful for the study of the mechanisms regulating tissue remodeling and for the control of several invalidating diseases characterized by fibrosis development.
Footnotes
Address reprint requests to Boris Hinz, Ph.D., Laboratory of Cell Biophysics, Ecole Polytechnique Fédérale de Lausanne (EPFL), Bâtiment SG–AA-B143, Station 15, CH-1015 Lausanne, Switzerland. E-mail: boris.hinz@epfl.ch.
Supported by MUIR grant SM2378 and FiorGen Foundation (to A.G.), the Swiss National Science Foundation grants 3100A0-102150/1 and 3100A0-113733/1 (to B.H.), the Swiss National Science Foundation grant 32-068034.02 (to M.-L.B.P.), the National Institutes of Health grants HL28737, HL31963, HL52285, and HL77297S and an award from the Sandler Program in Asthma Research (to H.P.), and the National Institutes of Health grants HL74024 and HL67967 (to V.J.T.).
References
- Hinz B. Formation and function of the myofibroblast during tissue repair. J Invest Dermatol. 2007;127:526–537. doi: 10.1038/sj.jid.5700613. [DOI] [PubMed] [Google Scholar]
- Brown RD, Ambler SK, Mitchell MD, Long CS. The cardiac fibroblast: therapeutic target in myocardial remodeling and failure. Annu Rev Pharmacol Toxicol. 2005;45:657–687. doi: 10.1146/annurev.pharmtox.45.120403.095802. [DOI] [PubMed] [Google Scholar]
- Desmoulière A, Darby IA, Gabbiani G. Normal and pathologic soft tissue remodeling: role of the myofibroblast, with special emphasis on liver and kidney fibrosis. Lab Invest. 2003;83:1689–1707. doi: 10.1097/01.lab.0000101911.53973.90. [DOI] [PubMed] [Google Scholar]
- De Wever O, Mareel M. Role of tissue stroma in cancer cell invasion. J Pathol. 2003;200:429–447. doi: 10.1002/path.1398. [DOI] [PubMed] [Google Scholar]
- Thannickal VJ, Toews GB, White ES, Lynch JP, 3rd, Martinez FJ. Mechanisms of pulmonary fibrosis. Annu Rev Med. 2004;55:395–417. doi: 10.1146/annurev.med.55.091902.103810. [DOI] [PubMed] [Google Scholar]
- Zalewski A, Shi Y, Johnson AG. Diverse origin of intimal cells: smooth muscle cells, myofibroblasts, fibroblasts, and beyond? Circ Res. 2002;91:652–655. doi: 10.1161/01.res.0000038996.97287.9a. [DOI] [PubMed] [Google Scholar]
- Hao H, Gabbiani G, Camenzind E, Bacchetta M, Virmani R, Bochaton-Piallat ML. Phenotypic modulation of intima and media smooth muscle cells in fatal cases of coronary artery lesion. Arterioscler Thromb Vasc Biol. 2006;26:326–332. doi: 10.1161/01.ATV.0000199393.74656.4c. [DOI] [PubMed] [Google Scholar]
- Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodeling. Nat Rev Mol Cell Biol. 2002;3:349–363. doi: 10.1038/nrm809. [DOI] [PubMed] [Google Scholar]
- Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835–870. doi: 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- Hinz B. Masters and servants of the force: the role of matrix adhesions in myofibroblast force perception and transmission. Eur J Cell Biol. 2006;85:175–181. doi: 10.1016/j.ejcb.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Hinz B, Pittet P, Smith-Clerc J, Chaponnier C, Meister JJ. Myofibroblast development is characterized by specific cell-cell adherens junctions. Mol Biol Cell. 2004;15:4310–4320. doi: 10.1091/mbc.E04-05-0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinz B, Celetta G, Tomasek JJ, Gabbiani G, Chaponnier C. Alpha-smooth muscle actin expression upregulates fibroblast contractile activity. Mol Biol Cell. 2001;12:2730–2741. doi: 10.1091/mbc.12.9.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinz B, Gabbiani G, Chaponnier C. The NH2-terminal peptide of alpha-smooth muscle actin inhibits force generation by the myofibroblast in vitro and in vivo. J Cell Biol. 2002;157:657–663. doi: 10.1083/jcb.200201049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffin JM, Pittet P, Csucs G, Lussi JW, Meister JJ, Hinz B. Focal adhesion size controls tension-dependent recruitment of alpha-smooth muscle actin to stress fibers. J Cell Biol. 2006;172:259–268. doi: 10.1083/jcb.200506179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Zohar R, McCulloch CA. Multiple roles of α-smooth muscle actin in mechanotransduction. Exp Cell Res. 2006;312:205–214. doi: 10.1016/j.yexcr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Giannone G, Sheetz MP. Substrate rigidity and force define form through tyrosine phosphatase and kinase pathways. Trends Cell Biol. 2006;16:213–223. doi: 10.1016/j.tcb.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Thannickal VJ, Lee DY, White ES, Cui Z, Larios JM, Chacon R, Horowitz JC, Day RM, Thomas PE. Myofibroblast differentiation by transforming growth factor-β1 is dependent on cell adhesion and integrin signaling via focal adhesion kinase. J Biol Chem. 2003;278:12384–12389. doi: 10.1074/jbc.M208544200. [DOI] [PubMed] [Google Scholar]
- Carlson MA, Longaker MT, Thompson JS. Wound splinting regulates granulation tissue survival. J Surg Res. 2003;110:304–309. doi: 10.1016/s0022-4804(02)00098-7. [DOI] [PubMed] [Google Scholar]
- Rajkumar VS, Howell K, Csiszar K, Denton CP, Black CM, Abraham DJ. Shared expression of phenotypic markers in systemic sclerosis indicates a convergence of pericytes and fibroblasts to a myofibroblast lineage in fibrosis. Arthritis Res Ther. 2005;7:R1113–R1123. doi: 10.1186/ar1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abe R, Donnelly SC, Peng T, Bucala R, Metz CN. Peripheral blood fibrocytes: differentiation pathway and migration to wound sites. J Immunol. 2001;166:7556–7562. doi: 10.4049/jimmunol.166.12.7556. [DOI] [PubMed] [Google Scholar]
- Schmidt M, Sun G, Stacey MA, Mori L, Mattoli S. Identification of circulating fibrocytes as precursors of bronchial myofibroblasts in asthma. J Immunol. 2003;171:380–389. doi: 10.4049/jimmunol.171.1.380. [DOI] [PubMed] [Google Scholar]
- Forbes SJ, Russo FP, Rey V, Burra P, Rugge M, Wright NA, Alison MR. A significant proportion of myofibroblasts are of bone marrow origin in human liver fibrosis. Gastroenterology. 2004;126:955–963. doi: 10.1053/j.gastro.2004.02.025. [DOI] [PubMed] [Google Scholar]
- Direkze NC, Forbes SJ, Brittan M, Hunt T, Jeffery R, Preston SL, Poulsom R, Hodivala-Dilke K, Alison MR, Wright NA. Multiple organ engraftment by bone-marrow-derived myofibroblasts and fibroblasts in bone-marrow-transplanted mice. Stem Cells. 2003;21:514–520. doi: 10.1634/stemcells.21-5-514. [DOI] [PubMed] [Google Scholar]
- Ishii G, Sangai T, Oda T, Aoyagi Y, Hasebe T, Kanomata N, Endoh Y, Okumura C, Okuhara Y, Magae J, Emura M, Ochiya T, Ochiai A. Bone-marrow-derived myofibroblasts contribute to the cancer-induced stromal reaction. Biochem Biophys Res Commun. 2003;309:232–240. doi: 10.1016/s0006-291x(03)01544-4. [DOI] [PubMed] [Google Scholar]
- Hashimoto N, Jin H, Liu T, Chensue SW, Phan SH. Bone marrow-derived progenitor cells in pulmonary fibrosis. J Clin Invest. 2004;113:243–252. doi: 10.1172/JCI18847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisseleva T, Uchinami H, Feirt N, Quintana-Bustamante O, Segovia JC, Schwabe RF, Brenner DA. Bone marrow-derived fibrocytes participate in pathogenesis of liver fibrosis. J Hepatol. 2006;45:429–438. doi: 10.1016/j.jhep.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Zeisberg M, Kalluri R. The role of epithelial-to-mesenchymal transition in renal fibrosis. J Mol Med. 2004;82:175–181. doi: 10.1007/s00109-003-0517-9. [DOI] [PubMed] [Google Scholar]
- Kim KK, Kugler MC, Wolters PJ, Robillard L, Galvez MG, Brumwell AN, Sheppard D, Chapman HA. Alveolar epithelial cell mesenchymal transition develops in vivo during pulmonary fibrosis and is regulated by the extracellular matrix. Proc Natl Acad Sci USA. 2006;103:13180–13185. doi: 10.1073/pnas.0605669103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia JL, Dai C, Michalopoulos GK, Liu Y. Hepatocyte growth factor attenuates liver fibrosis induced by bile duct ligation. Am J Pathol. 2006;168:1500–1512. doi: 10.2353/ajpath.2006.050747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K, Rekhter MD, Gordon D, Phan SH. Myofibroblasts and their role in lung collagen gene expression during pulmonary fibrosis. A combined immunohistochemical and in situ hybridization study. Am J Pathol. 1994;145:114–125. [PMC free article] [PubMed] [Google Scholar]
- Zhang K, Gharaee-Kermani M, Jones ML, Warren JS, Phan SH. Lung monocyte chemoattractant protein-1 gene expression in bleomycin-induced pulmonary fibrosis. J Immunol. 1994;153:4733–4741. [PubMed] [Google Scholar]
- Phillips RJ, Burdick MD, Hong K, Lutz MA, Murray LA, Xue YY, Belperio JA, Keane MP, Strieter RM. Circulating fibrocytes traffic to the lungs in response to CXCL12 and mediate fibrosis. J Clin Invest. 2004;114:438–446. doi: 10.1172/JCI20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bröcker V, Langer F, Fellous TG, Mengel M, Brittan M, Bredt M, Milde S, Welte T, Eder M, Haverich A, Alison MR, Kreipe H, Lehmann U. Fibroblasts of recipient origin contribute to bronchiolitis obliterans in human lung transplants. Am J Respir Crit Care Med. 2006;173:1276–1282. doi: 10.1164/rccm.200509-1381OC. [DOI] [PubMed] [Google Scholar]
- Yokota T, Kawakami Y, Nagai Y, Ma JX, Tsai JY, Kincade PW, Sato S. Bone marrow lacks a transplantable progenitor for smooth muscle type alpha-actin-expressing cells. Stem Cells. 2006;24:13–22. doi: 10.1634/stemcells.2004-0346. [DOI] [PubMed] [Google Scholar]
- Frid MG, Kale VA, Stenmark KR. Mature vascular endothelium can give rise to smooth muscle cells via endothelial-mesenchymal transdifferentiation: in vitro analysis. Circ Res. 2002;90:1189–1196. doi: 10.1161/01.res.0000021432.70309.28. [DOI] [PubMed] [Google Scholar]
- Willis BC, Liebler JM, Luby-Phelps K, Nicholson AG, Crandall ED, du Bois RM, Borok Z. Induction of epithelial-mesenchymal transition in alveolar epithelial cells by transforming growth factor-β1: potential role in idiopathic pulmonary fibrosis. Am J Pathol. 2005;166:1321–1332. doi: 10.1016/s0002-9440(10)62351-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth K, Reh J, Sturrock A, Kasper M. Epithelial vs myofibroblast differentiation in immortal rat lung cell lines—modulating effects of bleomycin. Histochem Cell Biol. 2005;124:453–464. doi: 10.1007/s00418-005-0048-2. [DOI] [PubMed] [Google Scholar]
- Ramirez AM, Shen Z, Ritzenthaler JD, Roman J. Myofibroblast transdifferentiation in obliterative bronchiolitis: TGF-β signaling through smad3-dependent and -independent pathways. Am J Transplant. 2006;6:2080–2088. doi: 10.1111/j.1600-6143.2006.01430.x. [DOI] [PubMed] [Google Scholar]
- Hu B, Wu Z, Liu T, Ullenbruch MR, Jin H, Phan SH. Gut-enriched Kruppel-like factor interaction with Smad3 inhibits myofibroblast differentiation. Am J Respir Cell Mol Biol. 2007;36:78–84. doi: 10.1165/rcmb.2006-0043OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogan JG, Subramanian SV, Polikandriotis JA, Kelm RJ, Jr, Strauch AR. Vascular smooth muscle α-actin gene transcription during myofibroblast differentiation requires Sp1/3 protein binding proximal to the MCAT enhancer. J Biol Chem. 2002;277:36433–36442. doi: 10.1074/jbc.M203232200. [DOI] [PubMed] [Google Scholar]
- Hu B, Wu Z, Jin H, Hashimoto N, Liu T, Phan SH. CCAAT/enhancer-binding protein β isoforms and the regulation of α-smooth muscle actin gene expression by IL-1β. J Immunol. 2004;173:4661–4668. doi: 10.4049/jimmunol.173.7.4661. [DOI] [PubMed] [Google Scholar]
- Hu B, Ullenbruch MR, Jin H, Gharaee-Kermani M, Phan SH. An essential role for CCAAT/enhancer binding protein β in bleomycin induced pulmonary fibrosis. J Pathol. 2007;211:455–462. doi: 10.1002/path.2119. [DOI] [PubMed] [Google Scholar]
- Noseda M, Fu Y, Niessen K, Wong F, Chang L, McLean G, Karsan A. Smooth muscle α-actin is a direct target of Notch/CSL. Circ Res. 2006;98:1468–1470. doi: 10.1161/01.RES.0000229683.81357.26. [DOI] [PubMed] [Google Scholar]
- Mann J, Oakley F, Akiboye F, Elsharkawy A, Thorne AW, Mann DA. Regulation of myofibroblast transdifferentiation by DNA methylation and MeCP2: implications for wound healing and fibrogenesis. Cell Death Differ. 2007;14:275–285. doi: 10.1038/sj.cdd.4401979. [DOI] [PubMed] [Google Scholar]
- Chaqour B, Yang R, Sha Q. Mechanical stretch modulates the promoter activity of the profibrotic factor CCN2 through increased actin polymerization and NF-kappaB activation. J Biol Chem. 2006;281:20608–20622. doi: 10.1074/jbc.M600214200. [DOI] [PubMed] [Google Scholar]
- Leivonen SK, Chantry A, Hakkinen L, Han J, Kahari VM. Smad3 mediates transforming growth factor-beta-induced collagenase-3 (matrix metalloproteinase-13) expression in human gingival fibroblasts. Evidence for cross-talk between Smad3 and p38 signaling pathways. J Biol Chem. 2002;277:46338–46346. doi: 10.1074/jbc.M206535200. [DOI] [PubMed] [Google Scholar]
- Waghray M, Cui Z, Horowitz JC, Subramanian IM, Martinez FJ, Toews GB, Thannickal VJ. Hydrogen peroxide is a diffusible paracrine signal for the induction of epithelial cell death by activated myofibroblasts. FASEB J. 2005;19:854–856. doi: 10.1096/fj.04-2882fje. [DOI] [PubMed] [Google Scholar]
- Zhang HY, Phan SH. Inhibition of myofibroblast apoptosis by transforming growth factor β1. Am J Respir Cell Mol Biol. 1999;21:658–665. doi: 10.1165/ajrcmb.21.6.3720. [DOI] [PubMed] [Google Scholar]
- Horowitz JC, Lee DY, Waghray M, Keshamouni VG, Thomas PE, Zhang H, Cui Z, Thannickal VJ. Activation of the pro-survival phosphatidylinositol 3-kinase/AKT pathway by transforming growth factor-β1 in mesenchymal cells is mediated by p38 MAPK-dependent induction of an autocrine growth factor. J Biol Chem. 2004;279:1359–1367. doi: 10.1074/jbc.M306248200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White ES, Atrasz RG, Hu B, Phan SH, Stambolic V, Mak TW, Hogaboam CM, Flaherty KR, Martinez FJ, Kontos CD, Toews GB. Negative regulation of myofibroblast differentiation by PTEN (phosphatase and tensin homolog deleted on chromosome 10). Am J Respir Crit Care Med. 2006;173:112–121. doi: 10.1164/rccm.200507-1058OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JC, Rogers DS, Sharma V, White ES, Cui Z, Thannickal VJ. Combinatorial activation of FAK and AKT by transforming growth factor-β1 confers an anoikis-resistant phenotype to myofibroblasts. Cell Signal. 2007;19:761–771. doi: 10.1016/j.cellsig.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JC, Cui Z, Moore TA, Meier TR, Reddy RC, Toews GB, Standiford TJ, Thannickal VJ. Constitutive activation of prosurvival signaling in alveolar mesenchymal cells isolated from patients with nonresolving acute respiratory distress syndrome. Am J Physiol. 2006;290:L415–L425. doi: 10.1152/ajplung.00276.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittal R, Horowitz JC, Moore BB, Zhang H, Martinez FJ, Toews GB, Standiford TJ, Thannickal VJ. Modulation of prosurvival signaling in fibroblasts by a protein kinase inhibitor protects against fibrotic tissue injury. Am J Pathol. 2005;166:367–375. doi: 10.1016/S0002-9440(10)62260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005;115:209–218. doi: 10.1172/JCI24282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyot C, Lepreux S, Combe C, Doudnikoff E, Bioulac-Sage P, Balabaud C, Desmouliere A. Hepatic fibrosis and cirrhosis: the (myo)fibroblastic cell subpopulations involved. Int J Biochem Cell Biol. 2006;38:135–151. doi: 10.1016/j.biocel.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Gressner AM, Weiskirchen R. Modern pathogenetic concepts of liver fibrosis suggest stellate cells and TGF-beta as major players and therapeutic targets. J Cell Mol Med. 2006;10:76–99. doi: 10.1111/j.1582-4934.2006.tb00292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galli A, Svegliati-Baroni G, Ceni E, Milani S, Ridolfi F, Salzano R, Tarocchi M, Grappone C, Pellegrini G, Benedetti A, Surrenti C, Casini A. Oxidative stress stimulates proliferation and invasiveness of hepatic stellate cells via a MMP2-mediated mechanism. Hepatology. 2005;41:1074–1084. doi: 10.1002/hep.20683. [DOI] [PubMed] [Google Scholar]
- Yang C, Zeisberg M, Mosterman B, Sudhakar A, Yerramalla U, Holthaus K, Xu L, Eng F, Afdhal N, Kalluri R. Liver fibrosis: insights into migration of hepatic stellate cells in response to extracellular matrix and growth factors. Gastroenterology. 2003;124:147–159. doi: 10.1053/gast.2003.50012. [DOI] [PubMed] [Google Scholar]
- Issa R, Williams E, Trim N, Kendall T, Arthur MJ, Reichen J, Benyon RC, Iredale JP. Apoptosis of hepatic stellate cells: involvement in resolution of biliary fibrosis and regulation by soluble growth factors. Gut. 2001;48:548–557. doi: 10.1136/gut.48.4.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bataller R, Paik YH, Lindquist JN, Lemasters JJ, Brenner DA. Hepatitis C virus core and nonstructural proteins induce fibrogenic effects in hepatic stellate cells. Gastroenterology. 2004;126:529–540. doi: 10.1053/j.gastro.2003.11.018. [DOI] [PubMed] [Google Scholar]
- Weng H, Mertens PR, Gressner AM, Dooley S. IFN-gamma abrogates profibrogenic TGF-beta signaling in liver by targeting expression of inhibitory and receptor Smads. J Hepatol. 2007;46:295–303. doi: 10.1016/j.jhep.2006.09.014. [DOI] [PubMed] [Google Scholar]
- Wells RG. The role of matrix stiffness in hepatic stellate cell activation and liver fibrosis. J Clin Gastroenterol. 2005;39:S158–S161. doi: 10.1097/01.mcg.0000155516.02468.0f. [DOI] [PubMed] [Google Scholar]
- Galli A, Crabb D, Price D, Ceni E, Salzano R, Surrenti C, Casini A. Peroxisome proliferator-activated receptor gamma transcriptional regulation is involved in platelet-derived growth factor-induced proliferation of human hepatic stellate cells. Hepatology. 2000;31:101–108. doi: 10.1002/hep.510310117. [DOI] [PubMed] [Google Scholar]
- Galli A, Crabb DW, Ceni E, Salzano R, Mello T, Svegliati-Baroni G, Ridolfi F, Trozzi L, Surrenti C, Casini A. Antidiabetic thiazolidinediones inhibit collagen synthesis and hepatic stellate cell activation in vivo and in vitro. Gastroenterology. 2002;122:1924–1940. doi: 10.1053/gast.2002.33666. [DOI] [PubMed] [Google Scholar]
- Wandzioch E, Kolterud A, Jacobsson M, Friedman SL, Carlsson L. Lhx2−/− mice develop liver fibrosis. Proc Natl Acad Sci USA. 2004;101:16549–16554. doi: 10.1073/pnas.0404678101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratziu V, Lalazar A, Wong L, Dang Q, Collins C, Shaulian E, Jensen S, Friedman SL. Zf9, a Kruppel-like transcription factor up-regulated in vivo during early hepatic fibrosis. Proc Natl Acad Sci USA. 1998;95:9500–9505. doi: 10.1073/pnas.95.16.9500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockey DC. Hepatic blood flow regulation by stellate cells in normal and injured liver. Semin Liver Dis. 2001;21:337–349. doi: 10.1055/s-2001-17551. [DOI] [PubMed] [Google Scholar]
- Oikawa H, Masuda T, Kawaguchi J, Sato R. Three-dimensional examination of hepatic stellate cells in rat liver and response to endothelin-1 using confocal laser scanning microscopy. J Gastroenterol Hepatol. 2002;17:861–872. doi: 10.1046/j.1440-1746.2002.02831.x. [DOI] [PubMed] [Google Scholar]
- Ramadori G, Saile B. Portal tract fibrogenesis in the liver. Lab Invest. 2004;84:153–159. doi: 10.1038/labinvest.3700030. [DOI] [PubMed] [Google Scholar]
- Cassiman D, Libbrecht L, Desmet V, Denef C, Roskams T. Hepatic stellate cell/myofibroblast subpopulations in fibrotic human and rat livers. J Hepatol. 2002;36:200–209. doi: 10.1016/s0168-8278(01)00260-4. [DOI] [PubMed] [Google Scholar]
- Lieber CS. Alcoholic liver disease: new insights in pathogenesis lead to new treatments. J Hepatol. 2000;32:113–128. doi: 10.1016/s0168-8278(00)80420-1. [DOI] [PubMed] [Google Scholar]
- Lepreux S, Bioulac-Sage P, Gabbiani G, Sapin V, Housset C, Rosenbaum J, Balabaud C, Desmouliere A. Cellular retinol-binding protein-1 expression in normal and fibrotic/cirrhotic human liver: different patterns of expression in hepatic stellate cells and (myo)fibroblast subpopulations. J Hepatol. 2004;40:774–780. doi: 10.1016/j.jhep.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Ramadori G, Saile B. Mesenchymal cells in the liver—one cell type or two? Liver. 2002;22:283–294. doi: 10.1034/j.1600-0676.2002.01726.x. [DOI] [PubMed] [Google Scholar]
- Saile B, DiRocco P, Dudas J, El-Armouche H, Sebb H, Eisenbach C, Neubauer K, Ramadori G. IGF-I induces DNA synthesis and apoptosis in rat liver hepatic stellate cells (HSC) but DNA synthesis and proliferation in rat liver myofibroblasts (rMF). Lab Invest. 2004;84:1037–1049. doi: 10.1038/labinvest.3700116. [DOI] [PubMed] [Google Scholar]
- Ogawa T, Tateno C, Asahina K, Fujii H, Kawada N, Obara M, Yoshizato K. Identification of vitamin A-free cells in a stellate cell-enriched fraction of normal rat liver as myofibroblasts. Histochem Cell Biol. 2007;127:161–174. doi: 10.1007/s00418-006-0237-7. [DOI] [PubMed] [Google Scholar]
- Baba S, Fujii H, Hirose T, Yasuchika K, Azuma H, Hoppo T, Naito M, Machimoto T, Ikai I. Commitment of bone marrow cells to hepatic stellate cells in mouse. J Hepatol. 2004;40:255–260. doi: 10.1016/j.jhep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Liu Y. Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol. 2004;15:1–12. doi: 10.1097/01.asn.0000106015.29070.e7. [DOI] [PubMed] [Google Scholar]
- Mazzocca A, Coppari R, De Franco R, Cho JY, Libermann TA, Pinzani M, Toker A. A secreted form of ADAM9 promotes carcinoma invasion through tumor-stromal interactions. Cancer Res. 2005;65:4728–4738. doi: 10.1158/0008-5472.CAN-04-4449. [DOI] [PubMed] [Google Scholar]
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- Virmani R, Kolodgie FD, Burke AP, Finn AV, Gold HK, Tulenko TN, Wrenn SP, Narula J. Atherosclerotic plaque progression and vulnerability to rupture: angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol. 2005;25:2054–2061. doi: 10.1161/01.ATV.0000178991.71605.18. [DOI] [PubMed] [Google Scholar]
- Lutgens E, van Suylen RJ, Faber BC, Gijbels MJ, Eurlings PM, Bijnens AP, Cleutjens KB, Heeneman S, Daemen MJ. Atherosclerotic plaque rupture: local or systemic process?. Arterioscler Thromb Vasc Biol. 2003;23:2123–2130. doi: 10.1161/01.ATV.0000097783.01596.E2. [DOI] [PubMed] [Google Scholar]
- Sartore S, Chiavegato A, Faggin E, Franch R, Puato M, Ausoni S, Pauletto P. Contribution of adventitial fibroblasts to neointima formation and vascular remodeling: from innocent bystander to active participant. Circ Res. 2001;89:1111–1121. doi: 10.1161/hh2401.100844. [DOI] [PubMed] [Google Scholar]
- Sata M, Saiura A, Kunisato A, Tojo A, Okada S, Tokuhisa T, Hirai H, Makuuchi M, Hirata Y, Nagai R. Hematopoietic stem cells differentiate into vascular cells that participate in the pathogenesis of atherosclerosis. Nat Med. 2002;8:403–409. doi: 10.1038/nm0402-403. [DOI] [PubMed] [Google Scholar]
- Owens GK, Kumar MS, Wamhoff BR. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev. 2004;84:767–801. doi: 10.1152/physrev.00041.2003. [DOI] [PubMed] [Google Scholar]
- Niessen P, Clement S, Fontao L, Chaponnier C, Teunissen B, Rensen S, van Eys G, Gabbiani G. Biochemical evidence for interaction between smoothelin and filamentous actin. Exp Cell Res. 2004;292:170–178. doi: 10.1016/j.yexcr.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Bentzon JF, Weile C, Sondergaard CS, Hindkjaer J, Kassem M, Falk E. Smooth muscle cells in atherosclerosis originate from the local vessel wall and not circulating progenitor cells in ApoE knockout mice. Arterioscler Thromb Vasc Biol. 2006;26:2696–2702. doi: 10.1161/01.ATV.0000247243.48542.9d. [DOI] [PubMed] [Google Scholar]
- Tomasek JJ, Vaughan MB, Kropp BP, Gabbiani G, Martin MD, Haaksma CJ, Hinz B. Contraction of myofibroblasts in granulation tissue is dependent on Rho/Rho kinase/myosin light chain phosphatase activity. Wound Repair Regen. 2006;14:313–320. doi: 10.1111/j.1743-6109.2006.00126.x. [DOI] [PubMed] [Google Scholar]
- Brisset AC, Hao H, Camenzind E, Bacchetta M, Geinoz A, Sanchez JC, Chaponnier C, Gabbiani G, Bochaton-Piallat ML. Intimal smooth muscle cells of porcine and human coronary artery express S100A4, a marker of the rhomboid phenotype in vitro. Circ Res. 2007;100:1055–1062. doi: 10.1161/01.RES.0000262654.84810.6c. [DOI] [PubMed] [Google Scholar]
- Marenholz I, Heizmann CW, Fritz G. S100 proteins in mouse and man: from evolution to function and pathology (including an update of the nomenclature). Biochem Biophys Res Commun. 2004;322:1111–1122. doi: 10.1016/j.bbrc.2004.07.096. [DOI] [PubMed] [Google Scholar]
- Hao H, Gabbiani G, Bochaton-Piallat ML. Arterial smooth muscle cell heterogeneity: implications for atherosclerosis and restenosis development. Arterioscler Thromb Vasc Biol. 2003;23:1510–1520. doi: 10.1161/01.ATV.0000090130.85752.ED. [DOI] [PubMed] [Google Scholar]
- Schurch W, Seemayer TA, Hinz B, Gabbiani G. Myofibroblast. Mills SE, editor. Philadelphia: Lippincott-Williams & Wilkins Publishers,; Histology for Pathologists. 2007:pp 123–164. [Google Scholar]