Abstract
Glycoproteins M and N (gM and gN, respectively) are among the few proteins that are conserved across the herpesvirus family. The function of the complex is largely unknown. Whereas deletion from most alphaherpesviruses has marginal effects on the replication of the respective viruses, both proteins are essential for replication of human cytomegalovirus (HCMV). We have constructed a series of mutants in gN to study the function of this protein. gN of HCMV is a type I glycoprotein containing a short carboxy-terminal domain of 14 amino acids, including two cysteine residues directly adjacent to the predicted transmembrane anchor at positions 125 and 126. Deletion of the entire carboxy-terminal domain as well as substitution with the corresponding region from alpha herpesviruses or mutations of both cysteine residues resulted in a replication-incompetent virus. Recombinant viruses containing point mutations of either cysteine residue could be generated. These viruses were profoundly defective for replication. Complex formation of the mutant gNs with gM and transport of the complex to the viral assembly compartment appeared unaltered compared to the wild type. However, in infected cells, large numbers of capsids accumulated in the cytoplasm that failed to acquire an envelope. Transiently expressed gN was shown to be modified by palmitic acid at both cysteine residues. In summary, our data suggest that the carboxy-terminal domain of gN plays a critical role in secondary envelopment of HCMV and that palmitoylation of gN appears to be essential for function in secondary envelopment of HCMV and virus replication.
The formation of an infectious herpesvirus is exceedingly complex and requires the assembly of an enveloped particle containing >70 proteins. The morphogenesis of this particle is still not understood. A currently widely accepted view suggests that two separate envelopment stages occur within the infected host cell and have led to the proposed envelopment-de-envelopment-reenvelopment model (36). According to this model, a primary envelopment occurs when capsids bud at the inner nuclear membrane to become enveloped particles in the perinuclear space. These particles subsequently fuse with the outer nuclear membrane, leading to the release of capsids into the cytoplasm. The secondary envelopment occurs when capsids which have accumulated tegument proteins in the cytoplasm bud into the lumen of a compartment that carries markers of the late secretory pathway and the trans-Golgi network (TGN), operationally defined as the assembly compartment (49). It is here where herpesviruses acquire their complete set of envelope glycoproteins. It should be noted that this model is not universally accepted (31). In any case, the successful envelopment of the tegumented capsid requires that all envelope components be concentrated in the assembly compartment, a process that in itself also likely demands a high degree of structural and temporal coordination.
Glycoproteins M and N (gM and gN, respectively) are among the few envelope glycoproteins that are conserved throughout the entire family of Herpesviridae which, on first glance, might indicate that they serve a common function. However, despite this conservation, there are clear differences with respect to protein modification, complex formation, and requirement for virus replication. The gMs are in general highly hydrophobic proteins containing 6 to 8 predicted transmembrane domains, leaving most of the protein buried in the membrane. These proteins carry low levels or no carbohydrate sugar modifications (4, 14, 27, 30, 41, 57). gNs are small type I glycoproteins containing a single predicted transmembrane anchor. The primary amino acid sequence of gN proteins from the different human herpesviruses ranges from 75 to 138 amino acids (aa) (1, 23, 29, 33, 46). With respect to glycosylation, the gN molecules from different herpesviruses show extensive heterogeneity. Proteins from the alphaherpesviruses carry a low level of sugar modification, whereas gN of human cytomegalovirus (HCMV) is extensively modified by N-linked and O-linked sugars contributing over 40 kDa of mass to the 15 kDa polypeptide backbone (34). gM and gN form a complex which in some viruses is covalently linked by a disulfide bond (23, 33, 35, 57). The physical interaction seems to be necessary for correct posttranslational modification and transport of the complex through the exocytic pathway (29, 34).
The high degree of conservation within the family Herpesviridae indicates that both gM and gN are important for viral replication. However, deletion of the gM gene in some alphaherpesviruses, such as herpes simplex virus 1 (HSV-1), pseudorabies virus (PRV) or equid herpesvirus 1 (EHV-1), has only minimal effects on virus replication in cell culture (3, 15, 40). In contrast, in other members of the alphaherpesviruses, like EHV-4 or Marek's disease virus, the deletion of gM has been shown to severely impair virus replication or even result in a null phenotype (54, 58). Similar observations have been reported following the deletion of gN. The protein is dispensable for efficient replication of PRV but is essential for Marek's disease virus (22, 54). In vivo, a PRV gM deletion mutant exhibits strongly attenuated phenotype in its natural hosts, pigs (13). In the betaherpesviruses, both proteins seem to be essential, since deletion of either gM or gN results in a null phenotype (18, 35).
The function of gM, gN, or the complex during the infectious cycle is largely unknown. Reports in the literature suggest potentially important roles for gM/gN in viral assembly and egress. For example, disruption of gM coding sequences in HSV-1, PRV, or EHV-1 have all been reported to reduce viral titers and plaque size, although to various degrees (3, 15, 40). Similar observations have been made when the gN coding region was disrupted in a number of herpesviruses, such as PRV, EHV-1, varicella-zoster virus (VZV), and Epstein-Barr virus (22, 28, 46, 48). Interpretation of the results from these studies has been hindered by the fact that in the absence of one partner of the complex, the second protein can have different posttranslational modifications and/or exhibit differences in intracellular trafficking. In transient-transfection assays, the gM or the gM/gN complexes from a number of different herpesviruses have been shown to inhibit membrane fusion caused by conserved herpesviral fusion proteins, such as gB, gD, gH, and gL, but also by heterologous fusion proteins from RNA viruses (25, 27). Evidence has been presented that gM/gN from HSV-1 and gM from PRV cause relocalization of several membrane proteins from the plasma membrane to the TGN, suggesting that gM/gN can inhibit cell-cell fusion by removing fusogenic proteins from the cells surface (12). Combinatorial deletion of gM and the tegument protein UL11 as well as gM and gE/gI result in a severe defect in secondary envelopment in PRV-infected cells, indicating a role of gM and perhaps the gM/gN complex in the final stages of virion morphogenesis for this virus (7, 26). On the other hand, simultaneous deletion of gM and gE from HSV-1 has an insignificant effect on virus replication (8). Thus, from data in the literature, it seems evident that different herpesviruses have different requirements for glycoprotein expression during the process of virion morphogenesis and final envelopment.
The gM/gN complex of HCMV was originally designated the gCII complex, and it was reported that components of the gCII complex have heparin-binding activity (24). Subsequent studies have identified the protein products of the open reading frames UL100 and UL73 as gM and gN, respectively (34). Both genes are indispensable for the replication of HCMV in fibroblasts (18, 35). HCMV gM is a 45-kDa protein that is glycosylated and retained in the endoplasmic reticulum (ER) when expressed in the absence of gN. In contrast, glycosylation of gN only occurs in the presence of gM, and the protein is not transported through the secretory pathway in the absence of gM (34). Both proteins are covalently linked through a disulfide bond which involves cysteines at positions 41 in gM and 90 in gN, respectively (35). The disulfide bond, however, is not required for complex formation and transport of the complex into the assembly compartment of the virus. Moreover, mutant viruses that lack a disulfide bridge between gM and gN replicate with efficiencies similar to wild-type viruses.
In an attempt to further characterize the role of the gM/gN complex in HCMV replication and assembly, we constructed a number of plasmids and recombinant viruses that carried mutations within the cytoplasmic domain of gN. This domain consists of a short stretch of 14 amino acids including two cysteine residues at positions 125 and 126, immediately adjacent to the putative transmembrane domain of gN. Our data indicate that deletion of the cytoplasmic domain, replacement of this sequence with a homologous sequence from HSV-1 gN, and mutation of both cysteines are incompatible with virus replication. Mutation of either cysteine resulted in a profound inhibition of viral replication compared to wild-type virus. The phenotype was associated with reduction in secondary envelopment of cytoplasmic capsids. However, gM/gN complex formation and transport of the complex to the site of final viral assembly were unaffected by the mutations. Transiently expressed gN was shown to be modified by the addition of palmitic acid at both cysteine residues, indicating that the fatty acid modification might contribute to the functional assembly of the gM/gN complex within membrane domains destined to become the envelope of HCMV.
MATERIALS AND METHODS
Cells and viruses.
HCMV strain AD169 and recombinant viruses were propagated in primary human foreskin fibroblasts grown in minimal essential medium (Invitrogen, Karlsruhe, Germany) supplemented with 5% fetal calf serum (FCS), glutamine (100 mg/liter), and gentamicin (350 mg/liter). Virions were isolated by glycerol-tartrate gradient centrifugation as described previously (53). To prepare intracellular viral particles, cells from infected cultures were trypsinized and collected via low-speed centrifugation. The cell pellet was subjected to three freeze-thaw cycles, and cellular debris was removed by centrifugation at 1,000 × g. Supernatants were subjected to high-speed centrifugation (23,000 rpm in a Beckmann SW27 rotor) for 70 min, and the pellet was resuspended in medium and stored at −80°C. Human embryonic kidney cells expressing the simian virus 40 large T antigen (293T cells) were cultured in Dulbecco's modified Eagle's medium supplemented with 10% FCS, glutamine, gentamicin, and 50 μg/ml G418 (Invitrogen). Cos7 cells were passaged in Dulbecco's modified Eagle's medium supplemented with 10% FCS, glutamine, and gentamicin. For immunofluorescence, cells were grown on 13-mm glass coverslips in 24-well plates. For growth curves, human foreskin fibroblasts, plated in six-well dishes, were infected at a multiplicity of infection (MOI) of approximately 0.01. After adsorption of virus (4 h), the inoculum was removed and replaced with fresh medium. Supernatants were harvested at the indicated time points and stored at −80°C until use. Virus titers were determined by an indirect immunofluorescence assay using a monoclonal antibody (MAb) against the immediate early protein 1 (IE1) of HCMV as described previously (2). In some experiments, infected cell cultures were maintained in medium containing 1 mg/ml immunoglobulin (Ig) to HCMV (Cytotect; Biotest, Dreieich, Germany). At this concentration of Ig, >95% of input virus was neutralized at an MOI of 1.
Palmitoylation and immunoprecipitation.
Human embryonic kidney 293T cells were transfected with plasmids encoding full-length HCMV UL99 (pp28), full-length UL100 (gM), full-length UL73 (gN), or UL73 mutants containing the following mutations: C125S (c125), C126S (c126), and C125,126S (c125/26). All gN constructs were cotransfected with full-length gM to ensure authentic complex formation and trafficking. All constructs were cloned into the eukaryotic expression vector pcDNA3.1myc/his or pEF1myc/his (Invitrogen, Carlsbad, CA), and expressed proteins contained a Myc tag at the carboxyl terminus. Forty-eight hours after transfection, cells were washed twice in serum-free media and labeled for 2 h with 100 μCi/ml of [3H]palmitic acid. Cells from the labeling reactions were collected and processed for immunoprecipitation using magnetic beads (Miltenyi), as previously described (35). The immune precipitates were then analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), followed by fluorography.
Plasmids.
Construction of expression plasmids for gM and gN has been described previously (35). Plasmids coding for mutated forms of gN or gM were constructed by inserting the appropriate DNA fragment into the vector pcDNA3 or pcDNA3.1myc/his (Invitrogen, Karlsruhe, Germany). Mutagenesis of the coding sequence was achieved in a two-step PCR using degenerate primers (35).
BAC mutagenesis and reconstitution of recombinant viruses.
Mutagenesis of pHB5 (6) was performed using linear DNA fragments for homologous recombination. To create BACmids containing the respective UL73 mutant sequences, we used the plasmid pCPoΔUL73. This plasmid is a pCPo15 (11) derivative that contains the entire open reading frame (ORF) of UL74 (nucleotides [nt] 106095 to 107587; nomenclature according to GenBank accession number X17403) at the 3′ flanking region of the kanamycin resistance gene. PCR fragments containing the respective UL73 sequences were PCR-amplified from the plasmids described above, and the amplimer was inserted into the 5′ flanking region of the kanamycin resistance gene in pCPoΔUL73. From these plasmids, PCR fragments were generated encompassing the respective UL73-Kan-UL74 segment. Primers that were used included UL73rec5 (nt 106051 to 106067) and UL73rec3 (nt 106271 to 106251). Recombination in pHB5 was done as described previously (35). In brief, the DNA fragment was electroporated into Escherichia coli DH10B carrying the bacterial artificial chromosome (BAC) pHB5 and the plasmid pBAD for recE/T-mediated recombination (37). Bacterial colonies were selected on agar plates containing kanamycin (30 μg/ml) and chloramphenicol (30 μg/ml). To confirm the integrity of the recombined BAC, digestion of DNA with the appropriate restriction enzymes was carried out and analyzed via agarose gel electrophoresis in comparison to the parental lane pHB5. To confirm recombination at the predicted site, Southern blot analysis, PCR analysis, and DNA sequence analysis of the UL72-UL75 region were performed. To remove the kanamycin resistance gene after successful recombination, plasmid pBT340 encoding the Flp recombinase was used as described previously (11).
Reconstitution of BAC-derived virus.
MRC-5 cells (2.5 × 105 cells per well) were seeded into six-well dishes. Two days later, 5 μg of BAC DNA and 1 μg pcDNApp71tag plasmid DNA (kindly provided by B. Plachter, University of Mainz, Germany) were cotransfected using the Superfect reagent (QIAGEN, Hilden, Germany) according to the manufacturer's instructions. Twenty-four hours after transfection, the culture medium was replaced with fresh medium and the cells were cultivated for 7 days. All cells from the six-well culture were transferred to an 80-cm2 flask and cultured until a cytopathic effect was observed. Propagation of the infectious virus was either through cocultivation of infected and uninfected cells or infection of fibroblasts with the supernatant from infected cells. To test for reversion of the recombinant viruses (35), the primers 72up5 (nt 105682 to 105699) and 73rec3 (nt 106272 to 106251) were used.
Image analysis.
Cos7 cells grown on glass coverslips in 24-well plates were transfected with 0.8 μg of plasmid DNA using Lipofectamine (Invitrogen, Karlsruhe, Germany). Fibroblasts, also grown on glass coverslips in 24-well plates, were infected with the respective viruses at an MOI of 0.01. At the indicated time points, the coverslips were washed and fixed in 3.0% paraformaldehyde in phosphate-buffered saline. The fixed cells were permeabilized with 0.1% Triton X-100 containing buffer and then blocked with phosphate-buffered saline containing 1% bovine serum albumin. Primary antibodies were then added. Primary antibodies included the following: 14-16A, an IgM murine MAb specific for the gM/gN complex (34); IMP, an IgG murine MAb specific for gM (34); 41-18, an IgG murine MAb specific for HCMV pp28 (UL99); p63-27, an HCMV IE1-specific mouse MAb (2); TGN46, a polyclonal sheep antibody specific for the trans-Golgi protein TGN46 (Serotec, Dusseldorf, Germany). Following washing, antibody binding was detected with the appropriate secondary antibody conjugated with either fluorescein isothiocyanate or Cy3 (Dianova). Secondary antibodies included the following: polyclonal goat anti-mouse IgM μ-chain specific antibodies (Dianova, Hamburg, Germany); polyclonal rabbit anti-sheep IgG antibody (Dianova, Hamburg, Germany); polyclonal goat-anti mouse IgG γ-chain specific antibodies (Sigma). All antibody combinations were tested for lack of cross-reactivity. Images were collected using a Zeiss Axioplan 2 fluorescence microscope fitted with a Visitron Systems charge-coupled device camera (Puchheim, Germany). Images were processed using MetaView software and Adobe Photoshop.
EM.
For transmission electron microscopy (EM), the cells were fixed in 2.5% glutaraldehyde in 0.1 M phosphate buffer, postfixed in 2% buffered osmium tetroxide, dehydrated in a graded ethanol series, and embedded in epoxy resin according to standard protocols. Ultrathin sections were stained with uranyl acetate and lead citrate and examined with a transmission electron microscope (LEO 906E; Carl Zeiss Meditec, Oberkochen, Germany).
RESULTS
The carboxy-terminal part of gN is required for virus replication.
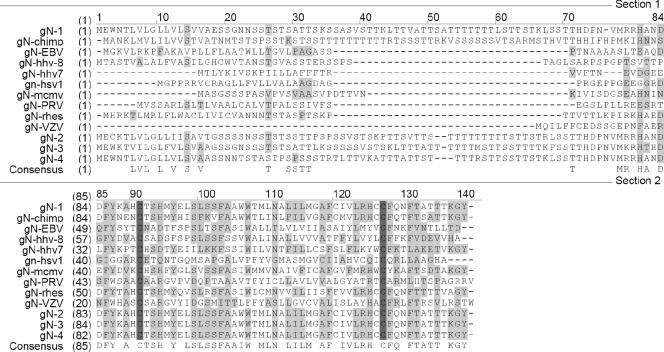
A remarkable feature of the gN molecules from different HCMV strains is the complete conservation of the amino acid sequence within the carboxy-terminal domain of the molecule starting at approximately aa 90 (numbering according to the amino acid sequence of strain AD169) despite the extreme polymorphism in the amino-terminal part of the molecule (42) (Fig. 1). An additional feature that is conserved not only between the different HCMV gNs but also in other herpesviruses are cysteine residues at positions immediately adjacent to the amino-terminal and carboxy-terminal boundaries of the putative transmembrane domain of the molecule (positions 90 and 125/126 in HCMV AD169). This perfect conservation between all herpesviruses suggests an important function of this part of the molecule and prompted us to investigate the role of this protein domain for gM/gN complex formation and viral replication. In a previous report, we have shown that the cysteine at position 90 is involved in the disulfide linkage to gM. gM/gN complex formation and viral replication in fibroblasts, however, were unaffected by a mutation of Cys 90 (35).
FIG. 1.
Alignment of gN amino acid sequences from different herpesviruses. The respective sequences were aligned using the software Vector NTi. The HCMV AD169 amino acid sequence was used as a reference. gN1 to gN4 denote prototype amino acid sequences from the different gN genotypes (42). The conserved cysteine residues are highlighted.
To investigate the role of the conserved carboxyl terminus of gN, including the cysteine residues within the C-terminal part of the molecule, in virus assembly and virus replication, we initially generated a series of HCMV BAC coding for recombinant gN molecules that contained C-terminal mutations and deletions (Fig. 2B). This represented a direct approach to begin our investigations of the function of this conserved domain of gN based on our previous findings that deletion of the gN coding region from the viral genome represented a lethal mutation (35). Recombinant BAC-UL73c125, BAC-UL73c126, and BAC-UL73125/26 harbored point mutations resulting in gN molecules with cysteine-to-serine exchanges at positions 125, 126, and 125 and 126, respectively. BAC-UL73Δ127 and BAC-UL73Δ124 encoded gN molecules that were truncated at residues 127 and 124, respectively. BAC-UL73cHSV codes for a gN molecule in which the carboxy-terminal part of HCMV gN following Cys 126 was replaced by the corresponding region of UL 49.5 (gN) from HSV-1.
FIG. 2.
Summary of mutant forms of gN that were used in this study. (A) Hydrophilicity plot of the primary amino acid sequence of the UL73 gene product. The putative signal sequence and membrane anchor are indicated by the shaded box. (B) The cartoon on the left side indicates the carboxy-terminal part of gN with the membrane anchor shaded in gray. The cysteine residues and the respective cysteine-to-serine mutations are indicated. The Myc epitope added to the very carboxy terminus of gN is indicated by the black oval.
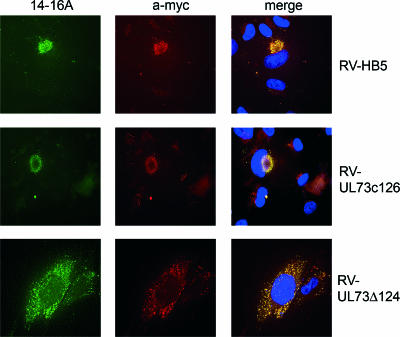
Mutations were originally constructed in BAC-HB5 of HCMV strain AD169 maintained in E. coli using a similar strategy as recently described (35). BAC DNA was then transfected into MRC-5 fibroblasts to reconstitute recombinant viruses. In several experiments involving independently derived BACs, we failed to recover infectious virus from MRC-5 cells transfected with BACs harboring gN mutations UL73c125/26, UL73cHSV, UL73Δ124, and UL73Δ127, indicating that these mutations were lethal and led to a replication-defective viral phenotype. The lack of formation of the gM/gN complex was an unlikely explanation for this defect, since we could detect reactivity with the MAb 14-16A for fibroblasts 10 to 14 days after transfection (Fig. 3 shows the results for RV-UL73Δ124 as an example). Reactivity with this antibody is a marker for complex formation between gM and gN because it has been shown to be reactive with gN only after the protein is modified by glycosylation and transported distal to the ER-Golgi-intermediate compartment in the secretory pathway (34). Coexpression of gM is prerequisite for the intracellular transport and subsequent posttranslational modifications of gN. The signal of the gN protein reactive with the 14-16A antibody nearly completely overlapped with the signal obtained by staining all gN molecules via the Myc epitope, indicating that the vast majority of the gN molecules were present in a complex with gM. In addition, the gM/gN complex also appeared to colocalize with gB in those cells (data not shown). In cells that were transfected with BACs exhibiting a replication-defective phenotype, the distribution of the gN-specific signal showed a speckled distribution over the entire cell cytoplasm (RV-UL73Δ124 in Fig. 3). This was different from cells infected with replication-competent virus which contained the characteristic juxtanuclear structure representing the viral assembly compartment (RV-HB5 and RV-UL73c126 in Fig. 3 and also below). We conclude from these results that mutations and/or deletions of the carboxy-terminal region of gN do not prevent gM/gN complex formation but can result in a replication-impaired virus.
FIG. 3.
Detection of gN in fibroblasts transfected with BAC DNA. Fibroblasts were transfected with the indicated BAC DNA and stained 14 days later by indirect immunofluorescence with antibodies specific for gN that is in complex with gM (14-16A) and total gN (a-myc). The merge picture represents an overlay of the red and green fluorescence. In the merge picture, cell nuclei are also stained blue using 4′,6′-diamidino-2-phenylindole (DAPI).
An obvious explanation for the inability to obtain replication-competent viruses from the BAC DNAs could have been a second site mutation within the genome of HCMV affecting an essential gene. To exclude this possibility, we performed a rescue experiment that repaired the mutation we had introduced into these viral genomes. To accomplish this rescue, DNA from BAC-UL73Δ124 was cotransfected with a PCR-generated DNA fragment encompassing ORFs UL72-UL74 of strain AD169. We have previously used this strategy successfully to rescue the lethal phenotype of a UL73-negative viral mutant (35). Replication-competent virus was generated using this approach, as indicated by the formation of viral plaques in the fibroblast culture 3 weeks after transfection. PCR and nucleotide sequence analysis revealed that the rescue was the result of a recombination between the UL72-UL74 DNA fragment and the BAC-UL73Δ124 DNA, giving rise to a revertant virus with the prototypic gene arrangement in the area of UL72-UL74 (data not shown).
Transfection of BAC DNA containing mutations UL73c125 and UL73c126 resulted in the recovery of infectious virus that was detected by the presence of a cytopathic effect (CPE) in the monolayer of transfected cells; however, there were profound differences in the rate of development and appearance of the CPE between the two recombinant viruses. The appearance of the CPE caused by RV-UL73c125 was comparable to the parental virus RV-HB5, i.e., an AD169-typical plaque morphology developed within 3 to 4 weeks after transfection. In contrast, the CPE caused by RV-UL73c126 took 6 to 8 weeks to develop and was reminiscent of infected cells very early after infection, i.e., rounding of individual cells exhibiting an increased contrast when observed with a light microscope. Typical plaques containing cytomegalic cells never developed (data not shown). In addition, whereas infectivity from RV-UL73c125 could be passaged using supernatant of infected cells, we could only inconsistently transfer infectivity using supernatant of RV-UL73c126-infected cells.
The extremely low to nonexistent infectivity present in the tissue culture supernatant of RV-UL73c126 made it impossible to analyze replication kinetics using extracellular virus. We therefore isolated intracellular viral particles for this assay (see Materials and Methods). These preparations contained sufficient infectious virus to perform multistep growth curves. Fibroblasts were infected with identical amounts of infectious virus from either the parental virus RV-HB5 or the mutants RV-UL73c125 and RV-UL73c126, respectively. As shown in Fig. 4A the virus yield from cells infected with RV-UL73c125 and RV-UL73c126 replication was decreased by >2 log and >3 log compared to wild-type parental virus, respectively. Quantitative real-time PCR showed that the number of HCMV genome copies in the supernatants of cells infected with the recombinant viruses were reduced in parallel to the reduction in infectious titers (>2 log for RV-UL73c126 and >1 log for RV-UL73c125). This indicated that fewer viruses were released into the supernatant by the UL73-cysteine mutant viruses (data not shown).
FIG. 4.
Replication of gN mutant viruses. (A) Fibroblasts were seeded in six-well dishes and infected with the indicated virus strains (MOI, 0.01). At the indicated days postinfection, supernatants from the infected cultures were harvested and infectious virus was titrated using indirect immunofluorescence with an antibody directed against IE1. Each data point represents the mean of results from three independent wells. (B) Fibroblasts were infected with the indicated virus strains. At the indicated time points, total DNA was extracted from the cultures and quantitative real-time PCR was performed.
To exclude the possibility that the observed replication deficit of RV-UL73c126 was the result of a second site mutation within the HCMV genome, a rescued virus, RV-UL73c126resc, was isolated as described above. This rescued virus replicated to levels similar to that of the parental virus (Fig. 4A). Interestingly, the rescue virus retained a mixed genotype with respect to ORF UL73. PCR analysis revealed that approximately 50% of extracellular viruses contained genomes exhibiting the UL73c126 genotype over several passages in tissue culture, indicating that infection of a single cell is usually with more than one genome and that gN is provided in trans (data not shown).
The lower numbers of infectious extracellular viral particles from RV-UL73c126 could result from a defect in DNA replication. To analyze this, we determined the accumulation of viral DNA during infection. Intracellular particles from RV-HB5, RV-UL73c125, and RV-UL73c126 corresponding to 2.5 × 103 infectious units/ml were used to infect fibroblasts, and DNA copy numbers were analyzed on days 4, 7, and 10 after infection by quantitative real-time PCR. As can be seen in Fig. 4B, the ratio of DNA copies to infectious particles differed considerably between the preparations (77 for RV-HB5 and 18,400 for RV-UL73c126). Although we were using intracellular particles as a source and these ratios do not reflect the DNA copy/infectious unit ratio as would be expected to exist in preparations of extracellular virus, the relative ratio of viral DNA to infectivity does suggest that a large number of DNA-containing virus particles produced by the gN recombinant viruses were noninfectious, presumably secondary to a defect in envelopment as suggested by the EM studies. After an initial drop in DNA copy numbers for RV-UL73c125 and RV-UL73c126, we observed a parallel increase in DNA concentration in cells infected with these viruses. This indicated that DNA synthesis was not inhibited in the gN recombinant viruses. Importantly, the inoculum of mutant virus RV-UL73c126 prepared from intracellular virus contained approximately 230-fold more copies (approximately 2.5 logs) of viral DNA than the wild-type virus when adjusted to the same titer of infectivity (2.5 × 103 IU). This difference in viral DNA copy number was consistent with the difference in extracellular virus yield from cells infected with the wild type compared to RV-UL73c126-infected cells. These findings, together with the EM results showing that the number of enveloped viruses is extremely small compared to immature particles in RV-UL73c126-infected cells (see below), support the presence of a defect in envelopment and not release.
gN recombinant viruses spread from cell to cell in fibroblasts.
We investigated the mode of spread of the recombinant viruses in the fibroblast cultures using an approach that would help distinguish between cell-to-cell spread versus extracellular spread of infectious virus. Fibroblasts were infected at an MOI of 0.001 with preparations from intracellular virus in the presence or absence of neutralizing IgG, and infected cells were visualized by indirect immunofluorescence at days 1, 7, and 14 after infection. In the absence of antibody, the parental virus RV-HB5 efficiently spread through the culture, and by day 14, approximately 100% of the cells were infected (Fig. 5). In the presence of antibody, the spread of virus was limited, and at day 14, infected cells were still confined to plaques. A similar picture was seen in cultures infected with RV-UL73c125, although plaques were much smaller in this case and the spread of infection to distant cells was less efficient. Plaques formed following infection with RV-UL73c126 were still smaller yet, reaching a maximum size of 20 to 30 infected cells at day 14. In contrast to the other two viruses, we detected no difference in the pattern of infection of the monolayer by RV-UL73c126 either in the presence or absence of neutralizing antibodies. Since the ability to form plaques in cell culture is generally accepted as a marker for efficient cell-to-cell spread of infectivity, we concluded from these results and those of the viral growth curves shown above, that mutations in gN resulted not only in a profound reduction in production of extracellular virus but also in a substantial decrease in the capacity of this virus to spread from cell to cell. In addition, our results indicated that the recombinant virus RV-UL73c126 spread primarily through a monolayer of permissive cells by a mechanism of cell-to-cell spread and not by release of extracellular virus.
FIG. 5.
Cell-to-cell spread of gN mutant recombinant viruses. Fibroblasts were infected with the indicated recombinant viruses at an MOI of 0.001. After 4 h of infection, the inoculum was removed and the cells were cultured in the presence (A) or absence (B) of neutralizing IgG. At days 1, 7, and 14, cells were processed for immunofluorescence by using antibodies specific for the HCMV IE1 and gB proteins (red). Cell nuclei were stained with 4′,6′-diamidino-2-phenylindole (DAPI) (blue). The purple color of the nuclei indicates IE1 staining; the red cytoplasmic staining represents gB.
The carboxy-terminal region of gN is dispensable for gM/gN complex formation.
A potential explanation for the severe reduction in production of extracellular virus by the mutant viruses could be lack of gM/gN complex formation in these viruses. To test this hypothesis, a number of expression plasmids were constructed which contained mutations in gN identical to those present in the mutant BACs (Fig. 2B). The respective DNA fragments were inserted into the vector pcDNA3.1-myc/his, allowing for the synthesis of recombinant gN proteins containing an Myc epitope at the carboxyl terminus. These plasmids were tested in transient expression assays for the formation of the gM/gN complex. As an indicator for gM/gN complex formation, we used recognition of the gN protein by the MAb 14-16A. All gN mutant proteins were recognized by MAb 14-16A when coexpressed with gM, and examples for the gNc125/26 are shown in Fig. 6. In addition, we determined the intracellular localization of the mutant gN proteins. Previous analyses have shown that, following isolated expression of gM or gN, either protein is detected mainly in the ER. When expressed together, the gM/gN complex is transported to the TGN and more distal compartments of the secretory pathway in the absence of additional viral proteins (34). The complexes of all mutant gN proteins with gM were found to colocalize with markers for the TGN (examples shown in Fig. 6). No colocalization was observed with markers for the ER, and only partial overlap with markers of the Golgi apparatus was observed (data not shown). Moreover, gM and the mutant gN proteins showed complete colocalization, indicating that mutation within the carboxy-terminal part of gN did not significantly alter the fraction of either protein within the complex (gM/gNc125/26 is shown as an example in Fig. 6). We conclude from these experiments that mutations or deletions within the carboxyl terminus of gN have no influence on the gM/gN complex formation as well as the transport of the complex to distal parts of the secretory pathway. These results confirm and extend our previous findings (35).
FIG. 6.
Intracellular localization of gM and gN mutant proteins following transient transfection. Cos7 cells were transfected with the indicated plasmids, and the intracellular localization of the individual proteins was determined by comparing the signals from the gM/gN-specific MAb 14-16A with those of antibodies specific for the trans-Golgi protein TGN46 or the gM-specific MAb IMP. Yellow indicates colocalization of the signal. In the merge panel, cell nuclei are also stained blue.
Distribution of structural proteins is unaltered in mutant infected cells.
The isolated expression of the gN mutant proteins together with gM indicated authentic complex formation and correct intracellular localization of gM/gN complexes. Whether similar complex formation and trafficking would occur in infected cells, i.e., in the presence of additional viral (glyco)proteins that could influence transport of the gM/gN complex was tested in the next series of experiments. Similar to our results from experiments using transient expression of gM and gN mutant proteins, we detected MAb 14-16A reactive protein in cells infected with either RV-UL73c125 or RV-UL73c126, indicating gM/gN complex formation (Fig. 7 and data not shown). In HCMV-infected cells, tegument and envelope glycoproteins accumulate within a cytoplasmic region, called the assembly compartment, that contains markers of the distal secretory pathway including the TGN (49). Tegument-containing capsids are proposed to be enveloped at this site. We therefore used TGN46, a marker for the TGN network, to localize the gM/gN complex within infected cells. As can be seen in Fig. 7, the gM/gN complex colocalized with TGN46 in cells infected with the parental virus RV-HB5 or the RV-UL73c126 virus. Consistent with findings from other laboratories, we noted altered morphology of the TGN within infected cells, but the morphology of the TGN was similar in cells infected with either the wild-type or mutant recombinant virus. Similarly, the tegument protein pp28 was distributed identically in cells infected with RV-HB5 and the gN mutant viruses (Fig. 7). Additional experiments using colocalization of viral envelope glycoproteins such as gB and gH with gM/gN failed to reveal differences in intracellular localization of these protein between cells infected with RV-HB5 or the mutant viruses. Also, there was no difference between RV-UL73c126 and RV-UL73c125 (data not shown). In summary, at this level of resolution, we were not able to detect obvious differences in the intracellular distribution of viral envelope or tegument proteins between wild-type virus and gN mutant viruses.
FIG. 7.
gM/gN complex formation in infected cells. Fibroblasts were infected with the indicated recombinant viruses for 72 h, and intracellular localization of the individual proteins was determined by comparing the signals from HCMV-specific MAbs with those of antibodies specific for the trans-Golgi protein TGN46. Yellow indicates colocalization of the signal. In the merge panel, cell nuclei are also stained blue. 14-16A, specific for the gM/gN complex; IMP, specific for gM (antibody IMP91-3/1); pp28, specific for the structural phosphoprotein pp28 (MAb 41-18).
Secondary envelopment is inhibited in gN mutant-infected fibroblasts.
To gain further insight into the mechanism(s) resulting in the observed phenotype of the gN mutant viruses, we performed ultrastructural analyses. Cells were infected for 120 h and processed for EM. Intracellular virus was examined only in cells with morphologically intact nuclear membranes to avoid studying late secondary cytopathic effects. In the nucleus, the three types of capsids (A, empty; B, protein scaffold containing; C, DNA containing) were found in wild-type and mutant virus-infected cells. Quantitatively, the wild-type virus and the gN mutant viruses produced similar ratios of the different capsid forms within the nucleus (data not shown). However, a dramatic difference was observed in the cytoplasm. In wild-type-infected cells we observed C-type capsids as well as complete, enveloped virions (Fig. 8). In addition, we observed capsids in the process of envelopment, indicated by the close proximity of tegumented capsids deforming electron-dense vesicles. In sharp contrast, the vast majority of the capsids were not enveloped in cells infected with RV-UL73c126. Only occasionally could we detect a complete virion in the cytoplasm of these cells (Fig. 8). Similar to the cytoplasmic capsids present in wild-type-infected cells, the capsids in RV-UL73c126-infected cells contained electron-dense material of variable intensity coating the capsid indicative of tegumentation. Thus, secondary envelopment seemed to be profoundly inhibited in cells infected with RV-UL73c126. Cells infected with RV-UL73c125 displayed an intermediate phenotype in that both tegumented capsids and enveloped viruses could readily be observed. However, the number of enveloped viruses compared to tegumented capsids was considerably lower than in wild-type-infected cells. When 200 viral particles were counted from different infected cells, the ratio of enveloped to nonenveloped particles was found to be 200 to 80 to 90 in cells infected with RV-HB5, 24 to 40 to 200 in cells infected with RV-UL73c125, and 1 to 3 to 200 in cells infected with RV-UL73c126 (Table 1).
FIG. 8.
Accumulation of virus particles in fibroblasts infected with different recombinant viruses. Cells were infected with the indicated viruses at an MOI of 0.001 and processed for EM 7 days later. Images were recorded at a magnification of ×21,560. Arrows identify enveloped virions; arrowheads identify tegumented capsids.
TABLE 1.
Ratio of enveloped virions and tegumented capsids in infected cellsa
| Particle type | Ratio in cells infected with:
|
||
|---|---|---|---|
| RV-HB5 | RV-UL73c125 | RV-UL73c126 | |
| Enveloped virions | 200 | 31 (24-40) | 2.3 (1-3) |
| Tegumented capsids | 86 (82-90) | 200 | 200 |
A total of 200 viral particles was counted, and the fraction of tegumented capsids (RV-HB5) or enveloped virions (RV-UL73c125, RV-UL73c126) was determined. Numbers represent the means of three enumerations, and ranges are given in parentheses.
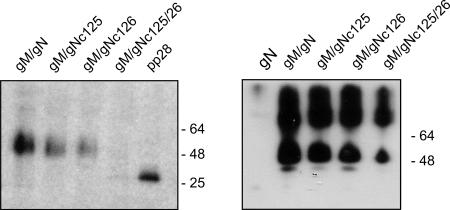
gN is modified by addition of palmitic acid.
The location of adjacent cysteine residues in a membrane-proximal location suggested the possibility that one of these residues could be covalently modified with palmitic acid, as has been observed in other viral glycoproteins (44). We investigated this possibility by transiently expressing Myc-tagged gN, gNc125, gNc126, or gNc125/26 with wild-type gM in 293T HEK cells and pulse-labeling the transfected cells with [3H]palmitic acid for 2 h. The Myc-tagged proteins were immunoprecipitated with anti-Myc beads and subjected to SDS-PAGE. We detected palmitic acid incorporation in wild-type gN and both the gNc125 and the gNc126 mutants but not in the gNc125/26 mutant (Fig. 9). Myc-tagged wild-type gN also failed to incorporate palmitic acid when it was expressed in the absence of gM, likely because, in the absence of gM, gN does not leave the ER (data not shown). When similar amounts of precipitated protein were analyzed by immunoblotting using an anti-Myc antibody to detect the Myc-tagged proteins, we found similar amounts of wild-type gN and mutant forms of gN expressed with gM (Fig. 9). In the absence of gM, only limited amounts of the unglycosylated form of gN were detected by the anti-Myc antibody. These results argued that the di-cysteines present at positions 125 and 126 could incorporate palmitic acid and suggested that mutation of these residues to serines resulted in loss of this posttranslational modification of gN and the lack of production of infectious virus when this mutation was introduced into the viral genome.
FIG. 9.
Palmitoylation of gN. (Left) Human embryonic kidney 293T cells were transfected with expression plasmids encoding full-length gM and wild-type gN or mutant forms of gN: gNc125, gNc126, or gNc125/26. As a control, HEK 293T cells were also transfected with a full-length form of UL99 (pp28). In all cases, the recombinant proteins were expressed as Myc epitope-tagged proteins. Following labeling with [3H]palmitic acid as described in Materials and Methods, the cells were lysed and precipitated using anti-Myc antibodies conjugated to magnetic beads as described. The immunoprecipitates were analyzed by SDS-PAGE and subjected to autoradiography. Note the decreased incorporation of palmitic acid in gN mutants gNc125 and gNc126 and the absence of signal following mutation of both cysteines (gNc125/26). Incorporation of palmitic acid into pp28 is shown as a control. (Right) Approximately one-half of the Myc bead-precipitated material from panel A was solubilized in SDS-PAGE sample buffer, electrophoresed by SDS-PAGE, transferred to nitrocellulose membranes, and probed with anti-Myc antibodies, followed by ECL detection of bound antibodies. These lanes served as a loading control for panel A and represent approximately the same amount of protein present in each lane of panel A. Molecular weight markers are shown on the right.
DISCUSSION
Although gN is highly conserved in all herpesviruses, a unified function of this virion protein in herpesvirus assembly has been difficult to assign. Viral mutants generated by deletion of gN in alphaherpesviruses have no readily identifiable phenotype, yet deletion of this virion glycoprotein in HCMV prevents the recovery of infectious virus. The results presented in this report further confirm the essential role of gN in the replication of HCMV in that deletion of the predicted cytoplasmic tail of gN or replacement of this region with the cytoplasmic domain of the corresponding HSV protein resulted in a null phenotype of the recombinant virus. Perhaps more importantly, our results demonstrated a seemingly essential role of gN in the secondary envelopment of the HCMV virion. Mutation of either aa 125 or 126 resulted in a dramatic alteration in the replication phenotype of the recombinant virus and a corresponding loss in the number of enveloped particles in the cytoplasm of infected cells compared to cells infected with the parental wild-type virus. Interestingly, a more pronounced replication-impaired phenotype was associated with mutation of Cys 126, the residue that is conserved between all herpesviral gNs (Fig. 1). Mutation of both Cys 125 and 126 (RV-UL73c125/26) eliminated the recovery of infectious virus, illustrating the importance of these specific amino acids in the assembly of infectious HCMV. Together, these findings extended the results from earlier studies of HSV and PRV in which only deletion of multiple envelope glycoproteins resulted in the loss of assembly of an infectious particle (7, 16, 26). These important studies were taken as further evidence of the critical role of the secondary, cytoplasmic envelopment of herpesviruses for the production of infectious virus (36). However, it should be noted that the envelopment-defective phenotype of these alphaherpesviruses was observed only after the deletion of multiple envelope glycoproteins, whereas we observed a similar phenotype in a recombinant HCMV in which a single amino acid residue within HCMV gN was mutagenized. Thus, our findings more convincingly demonstrate the requirement of gN for secondary cytoplasmic envelopment of HCMV in the assembly of an infectious particle. Yet we are also cognizant of the possibility that as yet undefined interactions between multiple envelope proteins could lead to the loss of envelopment that was observed in the RV-UL73c125/26 recombinant virus, a possibility that must also be considered when interpreting previous results from studies of HSV and PRV.
The finding that deletion or mutagenesis of the cytoplasmic tail of gN resulted in the loss of recovery of infectious HCMV from the corresponding BAC could be explained by the loss of complex formation between mutant forms of gN and gM, a protein complex that is present in the envelope of the infectious virion. Because gN must form a complex with gM to be transported from the ER, the replication-defective phenotype of recombinant viruses with mutations in the cytoplasmic tail of gN could be secondary to the loss of complex formation between these two proteins. However, we could readily demonstrate authentic complex formation between gM and gN mutants, including those mutations which failed to support replication of infectious virus when introduced into the viral genome. Complex formation has been defined by acquisition of gN reactivity with a virus-neutralizing MAb, 14-16A, a finding consistent with the observations that gN must complex with gM to acquire native structure and to localize to intracellular sites of envelopment (34). Previously, we have shown that gN complexes with gM through both covalent and noncovalent interactions, including a disulfide bond formed between Cys 44 of gM and Cys 90 of gN (35). Thus, it is not surprising that we could detect complex formation between gM and mutants that lacked the entire cytoplasmic tail of gN. These data argue that gM/gN complex formation alone is not sufficient for HCMV envelopment and production of infectious virus. Moreover, our finding argued that gN has an essential role in virion envelopment independent of its interactions with gM, a virion envelope protein that has previously been shown to be essential for envelopment. Interestingly, we have also generated recombinant viruses in which the cytoplasmic tail of gM has been deleted, and these viruses cannot replicate in permissive cells (M. Krzyzaniak, unpublished data). Together, these data support our postulate that both gM and gN could have an essential but independent role in envelopment of HCMV; however, because their structure and intracellular transport are dependent on their interactions, definitive evidence of their precise role in envelopment require further studies.
In transient-expression assays, we could demonstrate that gN was palmitoylated. Interestingly, deletion of either Cys at position 125 or 126 failed to prevent incorporation of radiolabeled palmitic acid into transiently expressed gN; however, the gN double mutant (gN C125S and C126S) did not incorporate [3H]palmitic acid. Although the presence of Cys-Cys residues immediately adjacent to the transmembrane domains of viral glycoproteins is a well-described motif in proteins that are modified by palmitoylation, experimental determination of which residue is modified is often required, as this modification is sequence context dependent and cannot be predicted from current databases (5). Thus, our data would argue that either Cys 125 or 126 or both can be modified by palmitoylation and that only when both cysteines were mutated to serines could we document a loss of this modification of gN. It is also possible that mutation of these cysteines resulted in loss of protein structure as these mutations represented nonconservative amino acid substitutions. Yet it should also be noted that this mutation did not alter complex formation with gM as detected with MAb 14-16A nor did it alter intracellular transport of the mutant gN from the ER into more distal compartments of the secretory pathway when the mutant molecule was transiently expressed as a component of the gM/gN complex. At this time, it is unclear what role palmitoylation of gN plays in the function of gN or in the gM/gN glycoprotein complex. Palmitoylation can have a number of different effects on membrane proteins, such as increasing the local concentration of the respective protein in the membrane to facilitate protein-protein interactions (52). With respect to viral infections, investigators have proposed that palmitoylation of viral glycoproteins with transmembrane domains and viral matrix protein covalently linked to membranes through myristic acid can further stabilize the membrane interactions of these proteins (5). In some cases, such as myristoylated viral matrix proteins, it appeared that palmitoylation was essential to maintain membrane association. However, since gM is a membrane protein that is anchored within the lipid bilayer by eight transmembrane domains, the function of the palmitic acid modification of gN is most likely unrelated to the membrane association of the gM/gN complex. Studies with several viruses have shown that viral envelope glycoproteins containing conventional transmembrane domains, including glycoproteins of vesicular stomatitis virus, influenza (hemagglutinin [HA]), paramxyovirus H protein, Newcastle disease virus, human immunodeficiency virus, murine leukemia virus, and Rous sarcoma virus are modified by palmitoylation (9, 10, 20, 32, 38, 39, 47, 50, 55). In some cases, palmitoylation has been reported to be required for assembly of an infectious viral particle, whereas in other cases, mutations that result in loss of this modification have no effect on the production of infectious virus (10, 21, 38, 39, 45, 47). In the case of influenza, palmitoylation of HA from H3 viruses has been suggested to be essential for several steps in the virus life cycle ranging from initial steps in entry, virus assembly, and virus budding (56, 59). The HA of influenza A virus contains three conserved cysteines at positions 555, 562, and 565. The spacing of these cysteine residues is similar to HCMV gN in that the Cys 555 is located within the membrane anchor of HA, whereas Cys 562 and Cys 565 are immediately adjacent to the transmembrane domain. Previous studies have shown that mutations of Cys 565 or a combination of Cys 562 and 565 prevented recovery of infectious virus from a reverse genetic system (59). More recently, Chen et al. have presented findings indicating that mutation of all three cysteines or cysteines 562 and 565 in combination resulted in about a 5 log decrease in virus titer (10). These authors also suggested that palmitoylation of this envelope protein likely plays a more critical role in virus assembly than HA function during entry events such as fusion.
At this time, we can only speculate on the function of the palmitic acid modification of HCMV gN during virion assembly and envelopment; however, our findings demonstrate that mutation of Cys 126 of gN can dramatically alter the replication phenotype of HCMV and significantly decrease the efficiency of secondary envelopment. These findings suggested that although gN is associated with gM, a protein predicted to have eight membrane-spanning domains, the palmitoylation modification of gN is essential for stabilization of the gN in a membrane conformation that appears to be essential for the function of the gM/gN complex. However, the mere presence of two cysteine residues at positions 125 and 126 seems insufficient for function of gN, since we could not recover infectious virus from BAC-UL73Δ127 and BAC-UL73cHSV which both contain cysteines 125 and 126. This result argued that the entire cytoplasmic tail of gN was essential for virus replication and perhaps secondary to its interaction with additional proteins. An alternative, and possibly more likely, explanation is that these specific gN mutant proteins are not palmitoylated secondary to the context dependence of the palmitoylation of membrane proteins (43).
A model for the role of gN in the envelopment of the HCMV particle can be envisioned but is highly speculative at this time, yet findings from our studies using EM point to a potential function of gN as a component of the gM/gN complex in the budding of tegumented particles into cytoplasmic vacuoles. The nature of these cytoplasmic vacuoles is incompletely defined, yet they resemble structures previously described as multivesicular bodies or late endosomes in earlier studies of the ultrastructure of HCMV in the cytoplasm of infected cells (17, 19). Our findings suggest that a defect associated with the substitution Cys→Ser at positions 125 or 126 of gN results in virus that cannot efficiently accomplish secondary envelopment. The loss of this function would suggest that gN has a major role in organization of the membrane of the cytoplasmic vacuole into which the tegumented particle ultimately buds. Because this budding process can be considered to be topologically similar to that of budding from the plasma membrane, models of RNA virus budding and envelopment at the plasma membrane could offer some insight into the function of gN. Similarly, examples of RNA envelope proteins that play critical roles in the budding of the particle from the plasma membrane, such as HA, also require posttranslational modifications, such as palmitoylation, in addition to hydrophobic transmembrane domains to successfully participate in envelopment in the particle. Although admittedly speculative at this point, gN, as part of the gM/gN complex, could play an essential role in organization of membrane domains of the cytoplasmic vacuole that eventually serve as sites of envelopment of tegumented capsids during budding into these cytoplasmic structures. Such a model is also consistent with the predicted multiple-membrane-spanning structure of gM and its abundance in the envelope of the particle. Thus, gN together with gM as a complex could serve to organize membrane domains that exclude cellular proteins but contain other, less abundant envelope glycoproteins into sites for particle envelopment.
The loss of efficient envelopment by the recombinant virus containing a mutation in Cys 126 of gN resulted in an interesting viral phenotype. This virus replicated DNA at the same rate as the parental wild-type virus but released very low numbers and, in most cases, no infectious virus into the supernatant of infected cells. Cellular monolayers infected with this virus exhibited atypical CPE, and virus spread through these cells was significantly retarded compared to wild-type virus. Together with our EM findings, these results suggested that the RV-UL73c126 recombinant virus mutated at Cys 126 had a defect in envelopment which limited the production of infectious extracellular virus but did not prevent spread from cell-to-cell. The spread of this virus between cells in a permissive monolayer with the concomitant lack of infectivity in the tissue culture supernatant suggested that cell-to-cell spread requires a very low number of enveloped virions and thus is more efficient than infection of cells with culture supernatant, a finding that was consistent with the observation of Silva et al. who demonstrated the intracellular spread of a mutant virus that lacked detectable envelope secondary to a deletion in the gene encoding the essential tegument protein, pp28 (51). Alternatively, it could also suggest that, in addition to the inhibition of secondary envelopment, gN mutant viruses have a defect in release from the infected cell.
In conclusion, we have demonstrated that the HCMV gN is an essential virion protein that appears to play a role in the secondary cytoplasmic envelopment of the virion. The cytoplasmic domain of this protein is required for the essential function(s) of gN, and our findings suggest that palmitoylation of Cys 125 and 126 represent posttranslational modifications of gN that are essential for its function during envelopment of the wild-type virus. Deletion of either one of these Cys residues results in a replication-impaired virus that exhibits a defect in production of extracellular virus, most likely secondary to a decrease in cytoplasmic envelopment. Although the role of gN and, therefore, the gM/gN complex in cytoplasmic envelopment is unknown, our findings point to a role for this glycoprotein complex late in the assembly of the infectious particle and not necessarily to a role for gM/gN in virus entry into permissive cells.
Acknowledgments
This work was supported by the Deutsche Forschungsgemeinschaft (grant MA929/6-1) and by grants from HHS, NIH, NIAID (R01 AI35602 and R01 AI50189).
Footnotes
Published ahead of print on 17 January 2007.
REFERENCES
- 1.Adams, R., C. Cunningham, M. D. Davison, C. A. MacLean, and A. J. Davison. 1998. Characterization of the protein encoded by gene UL49A of herpes simplex virus type 1. J. Gen. Virol. 79:813-823. [DOI] [PubMed] [Google Scholar]
- 2.Andreoni, M., M. Faircloth, L. Vugler, and W. J. Britt. 1989. A rapid microneutralization assay for the measurement of neutralizing antibody reactive with human cytomegalovirus. J. Virol. Methods 23:157-167. [DOI] [PubMed] [Google Scholar]
- 3.Baines, J. D., and B. Roizman. 1991. The open reading frames UL3, UL4, UL10, and UL16 are dispensable for the replication of herpes simplex virus 1 in cell culture. J. Virol. 65:938-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baines, J. D., and B. Roizman. 1993. The UL10 gene of herpes simplex virus 1 encodes a novel viral glycoprotein, gM, which is present in the virion and in the plasma membrane of infected cells. J. Virol. 67:1441-1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bijlmakers, M. J., and M. Marsh. 2003. The on-off story of protein palmitoylation. Trends Cell Biol. 13:32-42. [DOI] [PubMed] [Google Scholar]
- 6.Borst, E. M., G. Hahn, U. H. Koszinowski, and M. Messerle. 1999. Cloning of the human cytomegalovirus (HCMV) genome as an infectious bacterial artificial chromosome in Escherichia coli: a new approach for construction of HCMV mutants. J. Virol. 73:8320-8329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brack, A. R., J. M. Dijkstra, H. Granzow, B. G. Klupp, and T. C. Mettenleiter. 1999. Inhibition of virion maturation by simultaneous deletion of glycoproteins E, I, and M of pseudorabies virus. J. Virol. 73:5364-5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Browne, H., S. Bell, and T. Minson. 2004. Analysis of the requirement for glycoprotein m in herpes simplex virus type 1 morphogenesis. J. Virol. 78:1039-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chatis, P. A., and T. G. Morrison. 1982. Fatty acid modification of Newcastle disease virus glycoproteins. J. Virol. 43:342-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen, B. J., M. Takeda, and R. A. Lamb. 2005. Influenza virus hemagglutinin (H3 subtype) requires palmitoylation of its cytoplasmic tail for assembly: M1 proteins of two subtypes differ in their ability to support assembly. J. Virol. 79:13673-13684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cherepanov, P. P., and W. Wackernagel. 1995. Gene disruption in Escherichia coli: TcR and KmR cassettes with the option of Flp-catalyzed excision of the antibiotic-resistance determinant. Gene 158:9-14. [DOI] [PubMed] [Google Scholar]
- 12.Crump, C. M., B. Bruun, S. Bell, L. E. Pomeranz, T. Minson, and H. M. Browne. 2004. Alphaherpesvirus glycoprotein M causes the relocalization of plasma membrane proteins. J. Gen. Virol. 85:3517-3527. [DOI] [PubMed] [Google Scholar]
- 13.Dijkstra, J. M., V. Gerdts, B. G. Klupp, and T. C. Mettenleiter. 1997. Deletion of glycoprotein gM of pseudorabies virus results in attenuation for the natural host. J. Gen. Virol. 78:2147-2151. [DOI] [PubMed] [Google Scholar]
- 14.Dijkstra, J. M., T. C. Mettenleiter, and B. G. Klupp. 1997. Intracellular processing of pseudorabies virus glycoprotein M (gM): gM of strain Bartha lacks N-glycosylation. Virology 237:113-122. [DOI] [PubMed] [Google Scholar]
- 15.Dijkstra, J. M., N. Visser, T. C. Mettenleiter, and B. G. Klupp. 1996. Identification and characterization of pseudorabies virus glycoprotein gM as a nonessential virion component. J. Virol. 70:5684-5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farnsworth, A., K. Goldsmith, and D. C. Johnson. 2003. Herpes simplex virus glycoproteins gD and gE/gI serve essential but redundant functions during acquisition of the virion envelope in the cytoplasm. J. Virol. 77:8481-8494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fraile-Ramos, A., A. Pelchen-Matthews, T. N. Kledal, H. Browne, T. W. Schwartz, and M. Marsh. 2002. Localization of HCMV UL33 and US27 in endocytic compartments and viral membranes. Traffic 3:218-232. [DOI] [PubMed] [Google Scholar]
- 18.Hobom, U., W. Brune, M. Messerle, G. Hahn, and U. Koszinowski. 2000. Fast screening procedures for random transposon libraries of cloned herpesvirus genomes: mutational analysis of human cytomegalovirus envelope glycoprotein genes. J. Virol. 74:7720-7729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Homman-Loudiyi, M., K. Hultenby, W. Britt, and C. Soderberg-Naucler. 2003. Envelopment of human cytomegalovirus occurs by budding into Golgi-derived vacuole compartments positive for gB, Rab 3, trans-Golgi network 46, and mannosidase II. J. Virol. 77:3191-3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ivanova, L., and M. J. Schlesinger. 1993. Site-directed mutations in the Sindbis virus E2 glycoprotein identify palmitoylation sites and affect virus budding. J. Virol. 67:2546-2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jin, H., K. Subbarao, S. Bagai, G. P. Leser, B. R. Murphy, and R. A. Lamb. 1996. Palmitylation of the influenza virus hemagglutinin (H3) is not essential for virus assembly or infectivity. J. Virol. 70:1406-1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jöns, A., J. M. Dijkstra, and T. C. Mettenleiter. 1998. Glycoproteins M and N of pseudorabies virus form a disulfide-linked complex. J. Virol. 72:550-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jöns, A., H. Granzow, R. Kuchling, and T. C. Mettenleiter. 1996. The UL49.5 gene of pseudorabies virus codes for an O-glycosylated structural protein of the viral envelope. J. Virol. 70:1237-1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kari, B., and R. Gehrz. 1992. A human cytomegalovirus glycoprotein complex designated gC-II is a major heparin-binding component of the envelope. J. Virol. 66:1761-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klupp, B. G., R. Nixdorf, and T. C. Mettenleiter. 2000. Pseudorabies virus glycoprotein M inhibits membane fusion. J. Virol. 74:6760-6768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kopp, M., H. Granzow, W. Fuchs, B. Klupp, and T. C. Mettenleiter. 2004. Simultaneous deletion of pseudorabies virus tegument protein UL11 and glycoprotein M severely impairs secondary envelopment. J. Virol. 78:3024-3034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koyano, S., E. C. Mar, F. R. Stamey, and N. Inoue. 2003. Glycoproteins M and N of human herpesvirus 8 form a complex and inhibit cell fusion. J. Gen. Virol. 84:1485-1491. [DOI] [PubMed] [Google Scholar]
- 28.Lake, C. M., and L. M. Hutt-Fletcher. 2000. Epstein-Barr virus that lacks glycoprotein gN is impaired in assembly and infection. J. Virol. 74:11162-11172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lake, C. M., S. J. Molesworth, and L. M. Hutt-Fletcher. 1998. The Epstein-Barr virus (EBV) gN homolog BLRF1 encodes a 15-kilodalton glycoprotein that cannot be authentically processed unless it is coexpressed with the EBV gM homolog BBRF3. J. Virol. 72:5559-5564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lehner, R., H. Meyer, and M. Mach. 1989. Identification and characterization of a human cytomegalovirus gene coding for a membrane protein that is conserved among human herpesviruses. J. Virol. 63:3792-3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leuzinger, H., U. Ziegler, E. M. Schraner, C. Fraefel, D. L. Glauser, I. Heid, M. Ackermann, M. Mueller, and P. Wild. 2005. Herpes simplex virus 1 envelopment follows two diverse pathways. J. Virol. 79:13047-13059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li, M., C. Yang, S. Tong, A. Weidmann, and R. W. Compans. 2002. Palmitoylation of the murine leukemia virus envelope protein is critical for lipid raft association and surface expression. J. Virol. 76:11845-11852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liang, X., B. Chow, C. Raggo, and L. A. Babiuk. 1996. Bovine herpesvirus 1 UL49.5 homolog gene encodes a novel viral envelope protein that forms a disulfide-linked complex with a second virion structural protein. J. Virol. 70:1448-1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mach, M., B. Kropff, P. Dal-Monte, and W. J. Britt. 2000. Complex formation of human cytomegalovirus gylcoprotein M (gpUL100) and glycoprotein N (gpUl73). J. Virol. 74:11881-11892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mach, M., B. Kropff, M. Kryzaniak, and W. Britt. 2005. Complex formation by glycoproteins M and N of human cytomegalovirus: structural and functional aspects. J. Virol. 79:2160-2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mettenleiter, T. C. 2002. Herpesvirus assembly and egress. J. Virol. 76:1537-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muyrers, J. P., Y. Zhang, G. Testa, and A. F. Stewart. 1999. Rapid modification of bacterial artificial chromosomes by ET-recombination. Nucleic Acids Res. 27:1555-1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Naim, H. Y., B. Amarneh, N. T. Ktistakis, and M. G. Roth. 1992. Effects of altering palmitylation sites on biosynthesis and function of the influenza virus hemagglutinin. J. Virol. 66:7585-7588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ochsenbauer-Jambor, C., D. C. Miller, C. R. Roberts, S. S. Rhee, and E. Hunter. 2001. Palmitoylation of the Rous sarcoma virus transmembrane glycoprotein is required for protein stability and virus infectivity. J. Virol. 75:11544-11554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Osterrieder, N., A. Neubauer, C. Brandmuller, B. Braun, O. R. Kaaden, and J. D. Baines. 1996. The equine herpesvirus 1 glycoprotein gp21/22a, the herpes simplex virus type 1 gM homolog, is involved in virus penetration and cell-to-cell spread of virions. J. Virol. 70:4110-4115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Osterrieder, N., A. Neubauer, B. Fakler, C. Brandmuller, C. Seyboldt, O. R. Kaaden, and J. D. Baines. 1997. Synthesis and processing of the equine herpesvirus 1 glycoprotein M. Virology 232:230-239. [DOI] [PubMed] [Google Scholar]
- 42.Pignatelli, S., P. Dal Monte, G. Rossini, S. Chou, T. Gojobori, K. Hanada, J. J. Guo, W. Rawlinson, W. Britt, M. Mach, and M. P. Landini. 2003. Human cytomegalovirus glycoprotein N (gpUL73-gN) genomic variants: identification of a novel subgroup, geographical distribution and evidence of positive selective pressure. J. Gen. Virol. 84:647-655. [DOI] [PubMed] [Google Scholar]
- 43.Ponimaskin, E., and M. F. Schmidt. 1998. Domain-structure of cytoplasmic border region is main determinant for palmitoylation of influenza virus hemagglutinin (H7). Virology 249:325-335. [DOI] [PubMed] [Google Scholar]
- 44.Resh, M. D. 1999. Fatty acylation of proteins: new insights into membrane targeting of myristoylated and palmitoylated proteins. Biochim. Biophys. Acta 1451:1-16. [DOI] [PubMed] [Google Scholar]
- 45.Rose, J. K., G. A. Adams, and C. J. Gallione. 1984. The presence of cysteine in the cytoplasmic domain of the vesicular stomatitis virus glycoprotein is required for palmitate addition. Proc. Natl. Acad. Sci. USA 81:2050-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ross, J., M. Williams, and J. I. Cohen. 1997. Disruption of the varicella-zoster virus dUTPase and the adjacent ORF9A gene results in impaired growth and reduced syncytia formation in vitro. Virology 234:186-195. [DOI] [PubMed] [Google Scholar]
- 47.Rousso, I., M. B. Mixon, B. K. Chen, and P. S. Kim. 2000. Palmitoylation of the HIV-1 envelope glycoprotein is critical for viral infectivity. Proc. Natl. Acad. Sci. USA 97:13523-13525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rudolph, J., C. Seyboldt, H. Granzow, and N. Osterrieder. 2002. The gene 10 (UL49.5) product of equine herpesvirus 1 is necessary and sufficient for functional processing of glycoprotein M. J. Virol. 76:2952-2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sanchez, V., K. D. Greis, E. Sztul, and W. J. Britt. 2000. Accumulation of virion tegument and envelope proteins in a stable cytoplasmic compartment during human cytomegalovirus replication: characterization of a potential site of virus assembly. J. Virol. 74:975-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schlesinger, M. J., and C. Malfer. 1982. Cerulenin blocks fatty acid acylation of glycoproteins and inhibits vesicular stomatitis and Sindbis virus particle formation. J. Biol. Chem. 257:9887-9890. [PubMed] [Google Scholar]
- 51.Silva, M. C., J. Schroer, and T. Shenk. 2005. Human cytomegalovirus cell-to-cell spread in the absence of an essential assembly protein. Proc. Natl. Acad. Sci. USA 102:2081-2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smotrys, J. E., and M. E. Linder. 2004. Palmitoylation of intracellular signaling proteins: regulation and function. Annu. Rev. Biochem. 73:559-587. [DOI] [PubMed] [Google Scholar]
- 53.Talbot, P., and J. D. Almeida. 1977. Human cytomegalovirus: purification of enveloped virions and dense bodies. J. Gen. Virol. 36:345-349. [DOI] [PubMed] [Google Scholar]
- 54.Tischer, B. K., D. Schumacher, M. Messerle, M. Wagner, and N. Osterrieder. 2002. The products of the UL10 (gM) and the UL49.5 genes of Marek's disease virus serotype 1 are essential for virus growth in cultured cells. J. Gen. Virol. 83:997-1003. [DOI] [PubMed] [Google Scholar]
- 55.Veit, M., M. F. Schmidt, and R. Rott. 1989. Different palmitoylation of paramyxovirus glycoproteins. Virology 168:173-176. [DOI] [PubMed] [Google Scholar]
- 56.Wagner, R., A. Herwig, N. Azzouz, and H. D. Klenk. 2005. Acylation-mediated membrane anchoring of avian influenza virus hemagglutinin is essential for fusion pore formation and virus infectivity. J. Virol. 79:6449-6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wu, S. X., X. P. Zhu, and G. J. Letchworth. 1998. Bovine herpesvirus 1 glycoprotein M forms a disulfide-linked heterodimer with the U(L)49.5 protein. J. Virol. 72:3029-3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ziegler, C., F. T. Just, A. Lischewski, K. Elbers, and A. Neubauer. 2005. A glycoprotein M-deleted equid herpesvirus 4 is severely impaired in virus egress and cell-to-cell spread. J. Gen. Virol. 86:11-21. [DOI] [PubMed] [Google Scholar]
- 59.Zurcher, T., G. Luo, and P. Palese. 1994. Mutations at palmitylation sites of the influenza virus hemagglutinin affect virus formation. J. Virol. 68:5748-5754. [DOI] [PMC free article] [PubMed] [Google Scholar]