Abstract
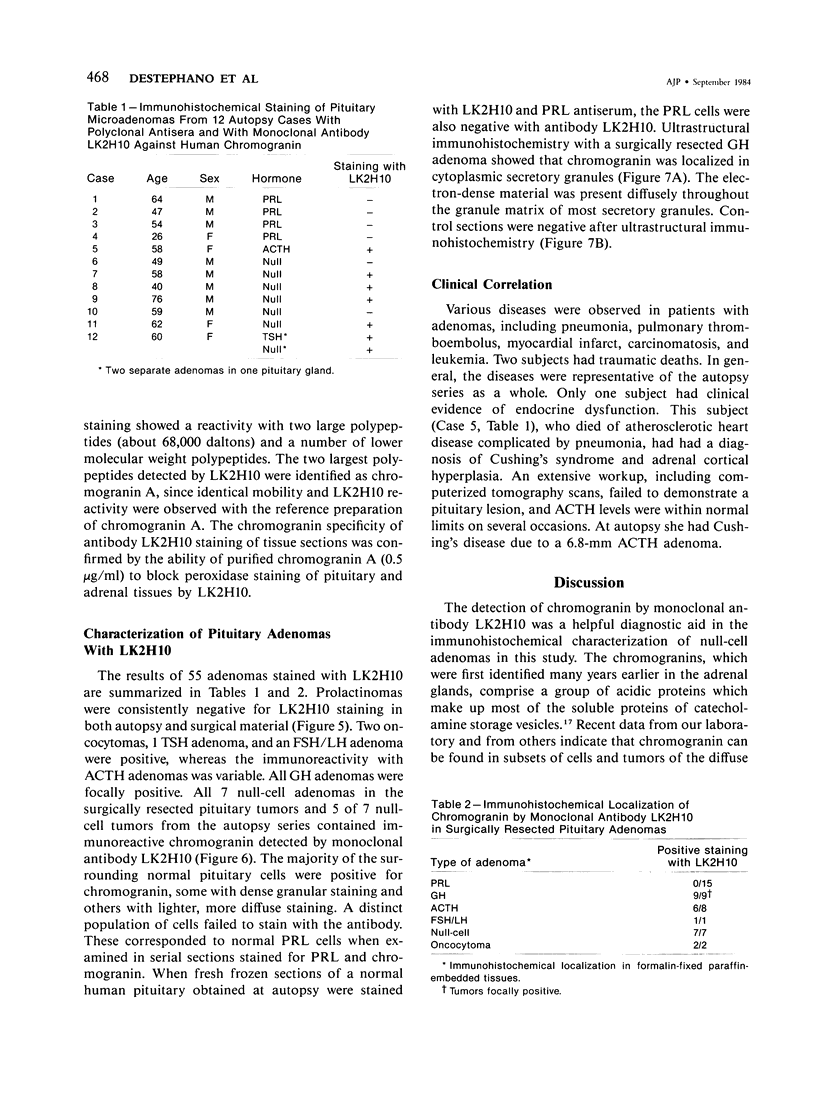
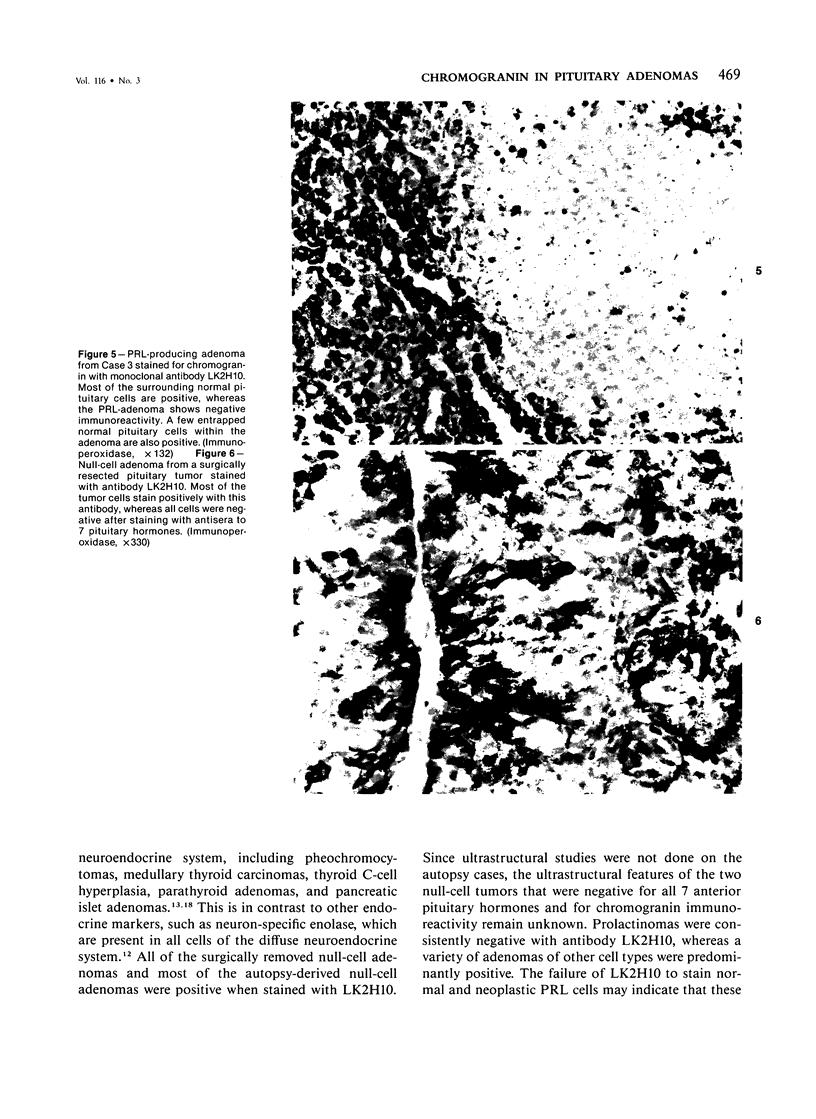
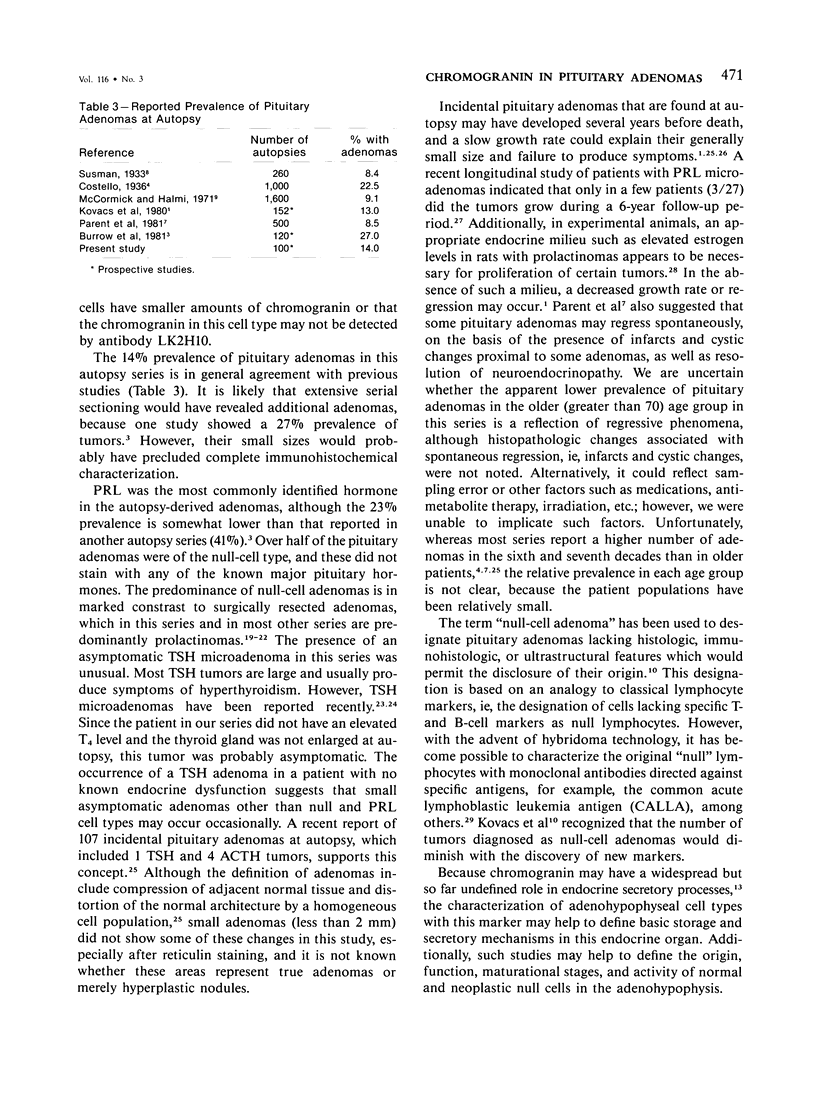
Tumors from 42 surgically resected pituitaries and from 13 autopsy cases were studied immunohistochemically with polyclonal antisera to 7 anterior pituitary hormones and with a newly developed monoclonal antibody directed against human chromogranin for evaluation of the distribution of chromogranin in normal and neoplastic pituitaries. In addition, a prospective study was done for assessment of the prevalence, morphology, and endocrine cell types of pituitary tumors in 100 autopsy subjects. When these 55 pituitary adenomas were examined with monoclonal antibody (LK2H10) directed against human chromogranin, selective staining of normal adenohypophyseal cell types and pituitary tumors was observed. Most null-cell adenomas (12/14) were positive for chromogranin, whereas all prolactin (PRL)-producing adenomas (19/19) were negative. Growth hormone (GH) adenomas were focally positive (9/9). All oncocytomas (2/2), 1 thyrotropin (TSH) adenoma, and a follicle-stimulating hormone/luteinizing hormone adenoma were positive for chromogranin. One or more adenomas were present in 14% of the autopsy cases. The tumors occurred most frequently in patients in the fifth through the seventh decades of life. Immunohistochemical staining of 13 adenomas revealed 1 TSH, 1 ACTH, and 4 PRL-producing tumors, whereas 7 other tumors, which were null-cell or undifferentiated adenomas, failed to stain for any of the seven principle pituitary hormones. These results indicate that antibody LK2H10 to human chromogranin is useful in the immunohistochemical characterization of pituitary adenomas. Incidental pituitary microadenomas from autopsy-derived pituitaries most commonly produce PRL, or they belong to the null-cell or undifferentiated tumor group.
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Burrow G. N., Wortzman G., Rewcastle N. B., Holgate R. C., Kovacs K. Microadenomas of the pituitary and abnormal sellar tomograms in an unselected autopsy series. N Engl J Med. 1981 Jan 15;304(3):156–158. doi: 10.1056/NEJM198101153040306. [DOI] [PubMed] [Google Scholar]
- Costello R. T. Subclinical Adenoma of the Pituitary Gland. Am J Pathol. 1936 Mar;12(2):205–216.1. [PMC free article] [PubMed] [Google Scholar]
- Duello T. M., Halmi N. S. Immunocytochemistry of prolactin-producing human pituitary adenomas. Am J Anat. 1980 Aug;158(4):463–469. doi: 10.1002/aja.1001580408. [DOI] [PubMed] [Google Scholar]
- Foon K. A., Schroff R. W., Gale R. P. Surface markers on leukemia and lymphoma cells: recent advances. Blood. 1982 Jul;60(1):1–19. [PubMed] [Google Scholar]
- Galfre G., Howe S. C., Milstein C., Butcher G. W., Howard J. C. Antibodies to major histocompatibility antigens produced by hybrid cell lines. Nature. 1977 Apr 7;266(5602):550–552. doi: 10.1038/266550a0. [DOI] [PubMed] [Google Scholar]
- Hsu S. M., Raine L., Fanger H. A comparative study of the peroxidase-antiperoxidase method and an avidin-biotin complex method for studying polypeptide hormones with radioimmunoassay antibodies. Am J Clin Pathol. 1981 May;75(5):734–738. doi: 10.1093/ajcp/75.5.734. [DOI] [PubMed] [Google Scholar]
- Kellett H. A., Wyllie A. H., Dale B. A., Best J. J., Toft A. D. Hyperthyroidism due to a thyrotrophin-secreting microadenoma. Clin Endocrinol (Oxf) 1983 Jul;19(1):57–65. doi: 10.1111/j.1365-2265.1983.tb00743.x. [DOI] [PubMed] [Google Scholar]
- Kovacs K., Corenblum B., Sirek A. M., Penz G., Ezrin C. Localization of prolactin in chromophobe pituitary adenomas: study of human necropsy material by immunoperoxidase technique. J Clin Pathol. 1976 Mar;29(3):250–258. doi: 10.1136/jcp.29.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs K., Horvath E., Ezrin C. Pituitary adenomas. Pathol Annu. 1977;12(Pt 2):341–382. [PubMed] [Google Scholar]
- Kovacs K., Horvath E., Ryan N., Ezrin C. Null cell adenoma of the human pituitary. Virchows Arch A Pathol Anat Histol. 1980;387(2):165–174. doi: 10.1007/BF00430697. [DOI] [PubMed] [Google Scholar]
- Kovacs K., Ryan N., Horvath E., Singer W., Ezrin C. Pituitary adenomas in old age. J Gerontol. 1980 Jan;35(1):16–22. doi: 10.1093/geronj/35.1.16. [DOI] [PubMed] [Google Scholar]
- Laemmli U. K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970 Aug 15;227(5259):680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- Landolt A. M. Ultrastructure of human sella tumors. Correlations of clinical findings and morphology. Acta Neurochir (Wien) 1975;Suppl 22:1–167. [PubMed] [Google Scholar]
- Lloyd R. V. Estrogen-induced hyperplasia and neoplasia in the rat anterior pituitary gland. An immunohistochemical study. Am J Pathol. 1983 Nov;113(2):198–206. [PMC free article] [PubMed] [Google Scholar]
- Lloyd R. V., Gikas P. W., Chandler W. F. Prolactin and growth hormone-producing pituitary adenomas. An immunohistochemical and ultrastructural study. Am J Surg Pathol. 1983 Apr;7(3):251–260. doi: 10.1097/00000478-198304000-00004. [DOI] [PubMed] [Google Scholar]
- Lloyd R. V., Wilson B. S. Specific endocrine tissue marker defined by a monoclonal antibody. Science. 1983 Nov 11;222(4624):628–630. doi: 10.1126/science.6635661. [DOI] [PubMed] [Google Scholar]
- Martinez A. J., Lee A., Moossy J., Maroon J. C. Pituitary adenomas: clinicopathological and immunohistochemical study. Ann Neurol. 1980 Jan;7(1):24–36. doi: 10.1002/ana.410070107. [DOI] [PubMed] [Google Scholar]
- McComb D. J., Ryan N., Horvath E., Kovacs K. Subclinical adenomas of the human pituitary. New light on old problems. Arch Pathol Lab Med. 1983 Sep;107(9):488–491. [PubMed] [Google Scholar]
- McCormick W. F., Halmi N. S. Absence of chromophobe adenomas from a large series of pituitary tumors. Arch Pathol. 1971 Oct;92(4):231–238. [PubMed] [Google Scholar]
- Nabarro J. D. Pituitary prolactinomas. Clin Endocrinol (Oxf) 1982 Aug;17(2):129–155. doi: 10.1111/j.1365-2265.1982.tb01573.x. [DOI] [PubMed] [Google Scholar]
- O'Connor D. T., Burton D., Deftos L. J. Immunoreactive human chromogranin A in diverse polypeptide hormone producing human tumors and normal endocrine tissues. J Clin Endocrinol Metab. 1983 Nov;57(5):1084–1086. doi: 10.1210/jcem-57-5-1084. [DOI] [PubMed] [Google Scholar]
- Parent A. D., Bebin J., Smith R. R. Incidental pituitary adenomas. J Neurosurg. 1981 Feb;54(2):228–231. doi: 10.3171/jns.1981.54.2.0228. [DOI] [PubMed] [Google Scholar]
- Parent A. D., Brown B., Smith E. E. Incidental pituitary adenomas: a retrospective study. Surgery. 1982 Nov;92(5):880–883. [PubMed] [Google Scholar]
- Saeger W., Lüdecke D. K. Pituitary adenomas with hyperfunction of TSH. Frequency, histological classification, immunocytochemistry and ultrastructure. Virchows Arch A Pathol Anat Histol. 1982;394(3):255–267. doi: 10.1007/BF00430669. [DOI] [PubMed] [Google Scholar]
- Schmechel D., Marangos P. J., Brightman M. Neurone-specific enolase is a molecular marker for peripheral and central neuroendocrine cells. Nature. 1978 Dec 21;276(5690):834–836. doi: 10.1038/276834a0. [DOI] [PubMed] [Google Scholar]
- Weiss M. H., Teal J., Gott P., Wycoff R., Yadley R., Apuzzo M. L., Giannotta S. L., Kletzky O., March C. Natural history of microprolactinomas: six-year follow-up. Neurosurgery. 1983 Feb;12(2):180–183. doi: 10.1227/00006123-198302000-00008. [DOI] [PubMed] [Google Scholar]