Abstract
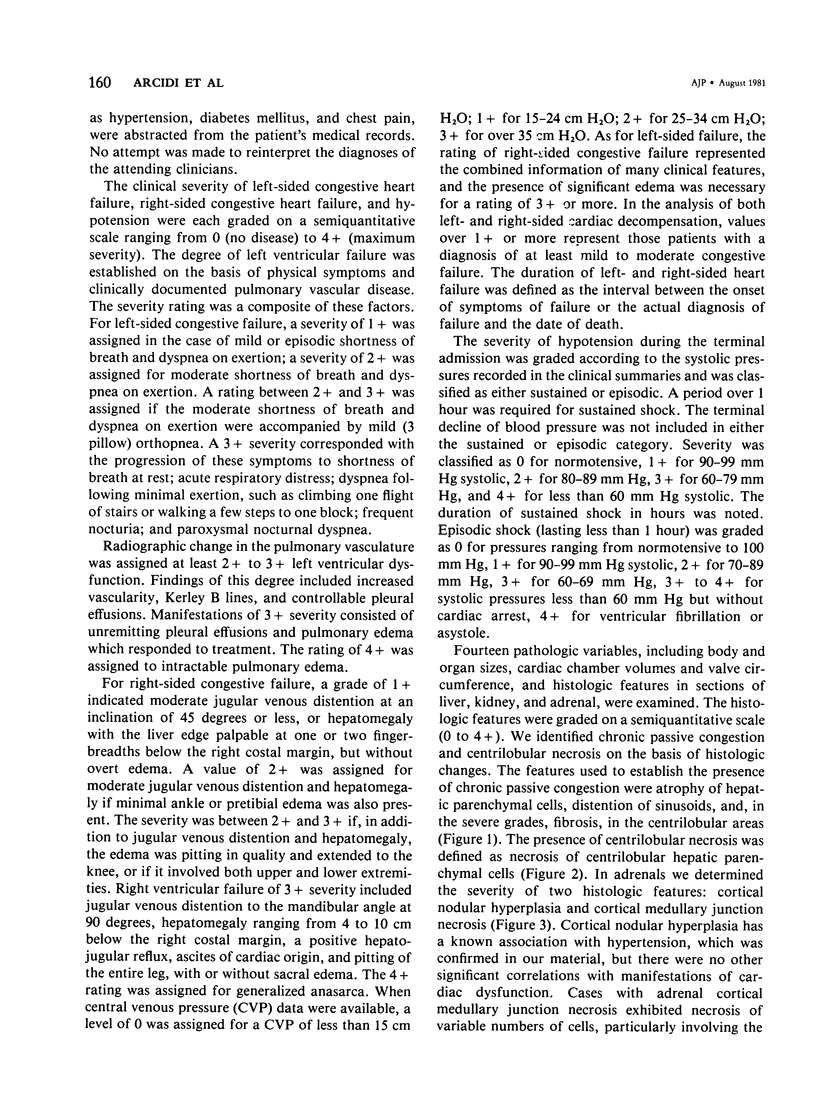
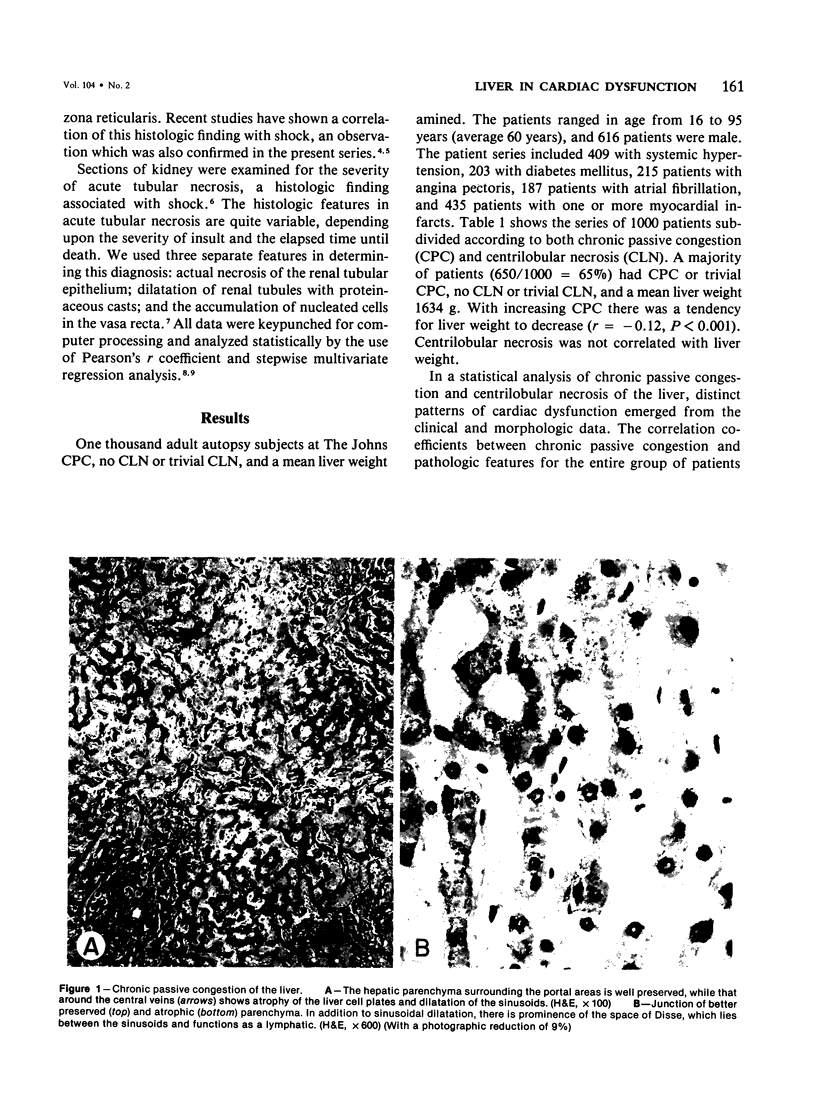
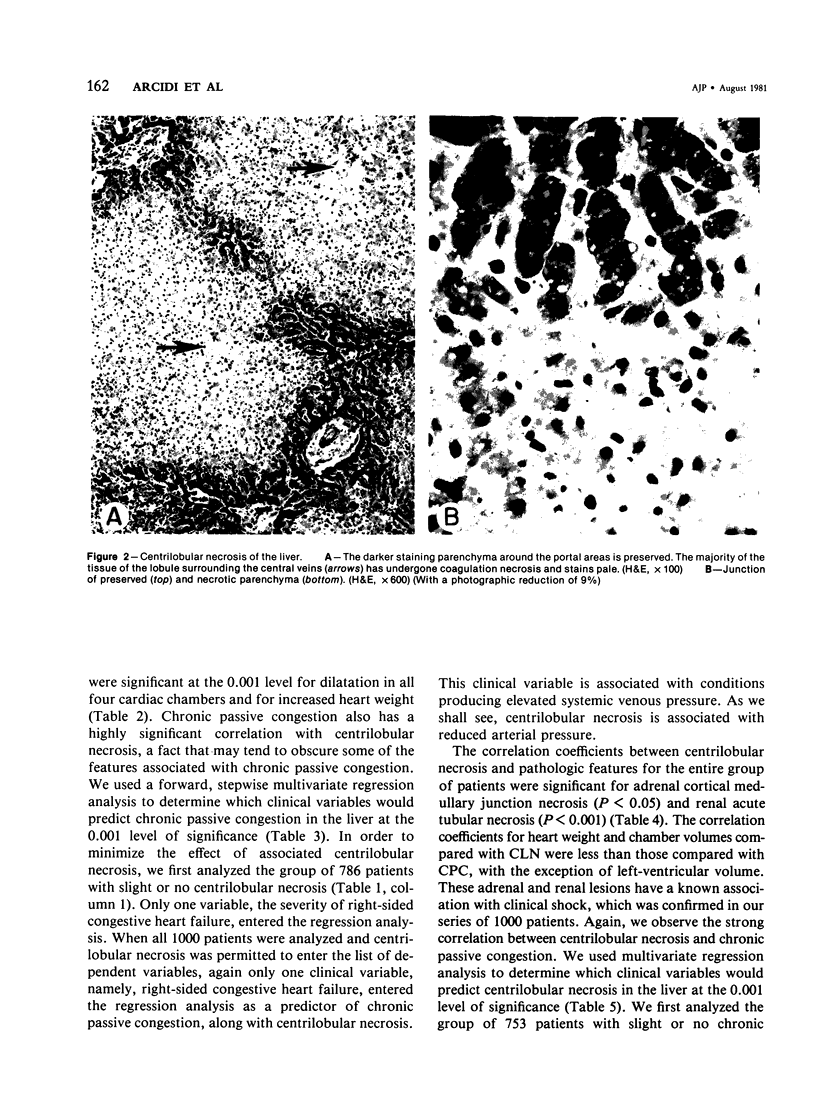
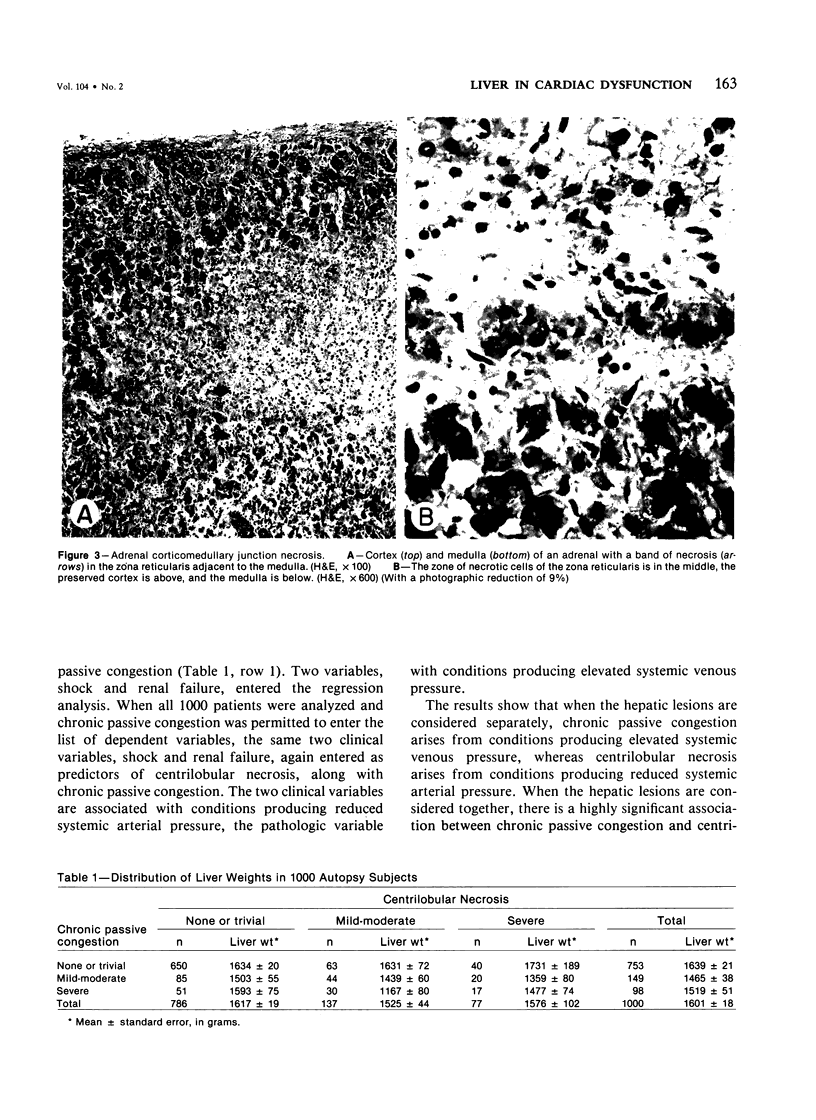
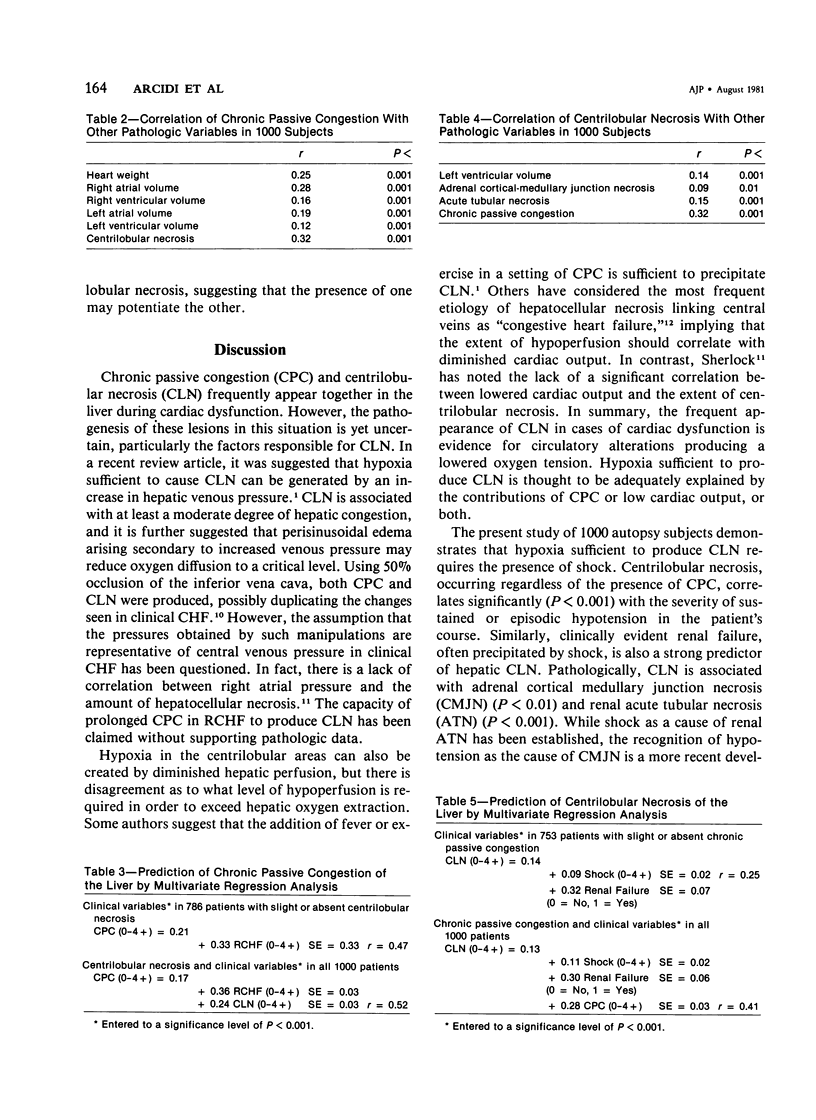
Chronic passive congestion (CPC) and centrilobular necrosis (CLN) are well recognized pathologic changes, but their exact relationship to different forms of cardiac dysfunction is uncertain. We reviewed clinical data and hepatic, renal, and adrenal morphology related to cardiac dysfunction in 1000 autopsy subjects at The Johns Hopkins Hospital whose hearts had been studied after postmortem arteriography and fixation in distention. Fourteen pathologic variables, including body and organ size, and microscopic changes graded on a semiquantitative scale, and 18 clinical variables including congestive heart failure, shock, and cardiovascular disease, were analyzed statistically. Distinct patterns of cardiac dysfunction emerged for the two spectra of hepatic morphologic change. Among patients with variable CPC, but slight or absent CLN, the amount of CPC was predicted in a multivariate analysis by severity of right-sided congestive heart failure. CPC severity correlated with cardiac weight and chamber enlargement (P less than 0.001). Among patients with variable CLN, but slight or absent CPC, CLN was predicted by profound hypotension and by renal failure. In addition, CLN, but not CPC, was significantly correlated with renal acute tubular necrosis (P less than 0.001) and adrenal cortical medullary junction necrosis (P less than 0.05), two lesions associated with shock. Among all 1000 patients CPC and CLN were highly significantly correlated (P less than 0.001). The results show that hepatic CPC arises from conditions producing elevated systemic venous pressure but that CLN arises from reduced systemic arterial pressure; and the presence of one potentiates the development of the other.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brooks S. E., Miller C. G., McKenzie K., Audretsch J. J., Bras G. Acute veno-occlusive disease of the liver. Fine structure in Jamaican children. Arch Pathol. 1970 Jun;89(6):507–520. [PubMed] [Google Scholar]
- Buhac I., Agrawal A. B., Park S. K., Lomotan A., Lowen B., Balint J. A. Jaundice and bridging centrilobular necrosis of liver in circulatory failure. N Y State J Med. 1976 May;76(5):678–682. [PubMed] [Google Scholar]
- CLARKE W. T. W. Centrilobular hepatic necrosis following cardiac infarction. Am J Pathol. 1950 Mar;26(2):249–255. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A., Kaplan M. M. Left-sided heart failure presenting as hepatitis. Gastroenterology. 1978 Mar;74(3):583–587. [PubMed] [Google Scholar]
- Cook G. C. Hepatic changes associated with shock. Int Anesthesiol Clin. 1969 Winter;7(4):883–894. doi: 10.1097/00004311-196907040-00010. [DOI] [PubMed] [Google Scholar]
- Dunn G. D., Hayes P., Breen K. J., Schenker S. The liver in congestive heart failure: a review. Am J Med Sci. 1973 Mar;265(3):174–189. doi: 10.1097/00000441-197303000-00001. [DOI] [PubMed] [Google Scholar]
- ELLENBERG M., OSSERMAN K. E. The role of shock in the production of central liver cell necrosis. Am J Med. 1951 Aug;11(2):170–178. doi: 10.1016/0002-9343(51)90102-7. [DOI] [PubMed] [Google Scholar]
- Hutchins G. M., Anaya O. A. Measurements of cardiac size, chamber volumes and valve orifices at autopsy. Johns Hopkins Med J. 1973 Aug;133(2):96–106. [PubMed] [Google Scholar]
- KILLIP T., 3rd, PAYNE M. A. High serum transaminase activity in heart disease. Circulatory failure and hepatic necrosis. Circulation. 1960 May;21:646–660. doi: 10.1161/01.cir.21.5.646. [DOI] [PubMed] [Google Scholar]
- Kanel G. C., Ucci A. A., Kaplan M. M., Wolfe H. J. A distinctive perivenular hepatic lesion associated with heart failure. Am J Clin Pathol. 1980 Feb;73(2):235–239. doi: 10.1093/ajcp/73.2.235. [DOI] [PubMed] [Google Scholar]
- Kuhajda F. J., Moore G. W., Hutchins G. M. Adrenal insufficiency secondary to massive corticomedullary junction hemorrhage following hypotension in three anticoagulated patients. Circ Shock. 1978;5(3):291–297. [PubMed] [Google Scholar]
- Kuhajda F. P., Hutchins G. M. Adrenal cortico-medullary junction necrosis: a morphologic marker for hypotension. Am Heart J. 1979 Sep;98(3):294–297. doi: 10.1016/0002-8703(79)90039-5. [DOI] [PubMed] [Google Scholar]
- Leopold J. G., Parry T. E., Storring F. K. A change in the sinusoid-trabecular structure of the liver with hepatic venous outflow block. J Pathol. 1970 Feb;100(2):87–98. doi: 10.1002/path.1711000203. [DOI] [PubMed] [Google Scholar]
- Popper H. Pathologic aspects of cirrhosis. A review. Am J Pathol. 1977 Apr;87(1):228–264. [PMC free article] [PubMed] [Google Scholar]
- SHERLOCK S. The liver in heart failure; relation of anatomical, functional, and circulatory changes. Br Heart J. 1951 Jul;13(3):273–293. doi: 10.1136/hrt.13.3.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safran A. P., Schaffner F. Chronic passive congestion of the liver in man. Electron microscopic study of cell atrophy and intralobular fibrosis. Am J Pathol. 1967 Mar;50(3):447–463. [PMC free article] [PubMed] [Google Scholar]
- Solez K., Morel-Maroger L., Sraer J. D. The morphology of "acute tubular necrosis" in man: analysis of 57 renal biopsies and a comparison with the glycerol model. Medicine (Baltimore) 1979 Sep;58(5):362–376. [PubMed] [Google Scholar]
- WHITE T. J., WALLACE R. B., GNASSI A. M., KEMP N. F., PRICE H. P., LEEVY C. M. Hepatic abnormalities in congestive heart failure; needle biopsy studies. Circulation. 1951 Apr;3(4):501–507. doi: 10.1161/01.cir.3.4.501. [DOI] [PubMed] [Google Scholar]