Abstract
Background
Methamphetamine use has been associated with rising STI/HIV transmission rates, particularly among men who have sex with men (MSM). Interventions which successfully reduce risk for HIV transmission among this population are a public health priority. This study examined the efficacy of a behavioral intervention for increasing safer sex behaviors in the context of ongoing methamphetamine use in a sample of HIV-positive, methamphetamine-using MSM.
Methods
Three-hundred forty one participants from San Diego, CA were randomly assigned to receive either a safer sex behavioral intervention (EDGE) or a time-equivalent diet-and-exercise attention-control condition. Random effects regression analyses were used to evaluate change in safer sex behaviors over a 12-month period.
Results
Participants in the EDGE intervention engaged in significantly more protected sex acts at the 8-month (p = .034) and 12-month assessment (p = 0.007). By 12-months post-baseline, a greater percentage of protected sex acts that was observed for EDGE (25.8%) vs. control participants (18.7%) (p = 0.038). There was a significant time-by-intervention interaction (p = .018) for self-efficacy for condom use, suggesting that EDGE participants’ self-efficacy demonstrated a greater increase over time compared to control participants.
Conclusions
These results suggest that it is possible to reduce high risk sexual behaviors in the context of ongoing methamphetamine use among HIV-infected MSM.
Keywords: HIV, AIDS, MSM, Safer Sex, Intervention, Methamphetamine
1. Introduction
Methamphetamine use has become widespread in the United States. In 2006, 48 percent of law enforcement officials from 500 counties in 44 states identified methamphetamine as the number one drug problem in their county (National Association of Counties; NACO, 2006). Approximately twelve million Americans are estimated to have used methamphetamine in their lifetime and 1.4 million persons use it in a given year (U.S. Dept. of Health and Human Services, 2005). Of persons using methamphetamine in the past month, the number of persons meeting criteria for stimulant abuse or dependence increased from 63,000 (10.6%) in 2002 to 130,000 (22.3%) in 2004 (U.S. Dept. of Health and Human Services, 2005). On a global level, the United Nations Office on Drugs and Crime (UNODC) estimates that amphetamine-type stimulants account for 10% of treatment demand, affecting 34 million people worldwide aged 15 and above (United Nations Office on Drugs and Crime, 2003).
Methamphetamine is the most widely used drug among men having sex with men (MSM) in the Western U.S. states, and individuals who use methamphetamine are at increased risk of acquiring HIV and other sexually transmitted infections (STIs; Clatts et al., 2005; Fernández et al., 2005; Halkitis et al., 2001; Purcell et al., 2001, Boddiger, 2005; Urbina and Jones, 2004). Methamphetamine appears to play an important role in sexual risk behaviors, particularly at the psychological level. Semple et al. (2002) reported that up to 84% of methamphetamine-using MSM engage in sexual risk behavior when high. Other studies of MSM documented strong associations between methamphetamine use and high risk sexual behaviors including unprotected insertive and receptive anal sex with casual partners, decreased use of condoms, and increased likelihood of acquiring STIs (Halkitis et al., 2001; Molitor et al., 1998; Reback and Ditman, 1997; Reback et al., 2004; Shoptaw et al., 2002). Interventions for reducing sexual risk behaviors of methamphetamine users should therefore focus on underlying motivations for drug use and unsafe sex and providing skills for practicing safer sex in the context of their methamphetamine use.
Psychosocial interventions for reducing HIV/STI risk among drug users have almost exclusively attempted to simultaneously reduce both drug use and sexual risk behaviors (Coyle et al., 1998; Metzger et al., 1998; Neaigus, 1998). In general, interventions have been more successful in reducing high risk drug-using behaviors (e.g., drug injection, multiperson reuse of syringes and needles) than sexual risk behaviors (Booth and Watters, 1994; Gibson et al., 1998). Moreover, these interventions have targeted injection drug users, most of whom are heterosexual (Kanouse, Bluthenthal, Bogart, et al., 2005). There is a paucity of HIV prevention interventions that target drug-using MSM, particularly non-injection drug users (Johnson, Hedges, & Diaz, 2006). Two studies that used data from treatment-seeking methamphetamine-using MSM demonstrated significant decreases in sexual risk behavior and increases in safer sex behavior across time (Reback et al., 2004; Shoptaw et al., 2005), supporting the notion that drug-using MSM can benefit from sexual risk reduction interventions.
This study examined the efficacy of a theory-based, psychosocial intervention for reducing sexual risk behavior among HIV-positive, methamphetamine-using MSM within the context of ongoing drug use. Our approach used motivational interviewing combined with elements from Social Cognitive Theory and the Theory of Reasoned Action (TRA) (Bandura, 1986; Bandura 1994; Azjen, 1991). Our exclusive focus on changing sexual behavior without changing drug use behavior is unique in HIV prevention research and is important for a number of reasons. First, while pharmacologic interventions to treat methamphetamine addiction are under study, such treatments are not widely available. Given the urgency of controlling the spread of HIV among methamphetamine-using MSM, and that few intervention trials designed specifically for HIV-positive individuals have been published, it is imperative to test the efficacy of programs that target sexual risk behaviors in the absence of drug abatement or reduction goals. Second, sexual risk reduction programs that do not emphasize change in drug use behavior may have a broader appeal among out-of-treatment methamphetamine users who are not ready to change their drug use but are concerned about their sexual risk behavior. Such programs, if offered through community-based organizations, could reach large numbers of methamphetamine users and help to reduce HIV/STI transmission in this high risk population.
Our intervention integrates a clinical approach (i.e., motivational interviewing) with principles from both Social Cognitive (Bandura, 1986; Bandura, 1994) and the Theory of Reasoned Action (Ajzen, 1991). Motivational interviewing is a client-centered, process-oriented, counseling approach that has been found to be very effective with alcoholics and drug users (Miller and Rollnick, 1991). It incorporates feedback on current behavior, emphasizes readiness for change and personal responsibility for change, delineates alternative strategies for changing problem behaviors, promotes counselor empathy and warmth, and reinforces self-efficacy (Miller and Rollnick, 1991). Social Cognitive Theory and the Theory of Reasoned Action use role-playing and modeling to enhance knowledge and self-efficacy for safer sex behavior (e.g., condom use, negotiation of safer sex) along with the enhancement of positive social supports. The theoretical framework for our intervention was selected on the basis of our previous intervention study which demonstrated reductions in sexual risk behaviors in a sample of mostly HIV-positive non-drug-using MSM (Patterson et al., 2003). Motivational interviewing was added to the protocol as an adjunct approach that was designed to enhance the theory-driven, positive behavior change effects that were demonstrated in our previous work.
We predicted that compared to those randomized to a general health intervention emphasizing diet and exercise, participants in the intervention condition would demonstrate a significant increase in protected sex behavior and a significant reduction in unprotected sex behaviors over the course of a 12-month randomized controlled trial. Based on a previous finding that demonstrated a strong association between self-efficacy and sexual risk behavior among HIV-positive MSM (Semple et al., 2000), we hypothesized that self-efficacy for condom use and negotiation would increase significantly over time among participants in the intervention condition who received social skills training as compared to control participants.
2. Methods
2.1. Participants
HIV-positive methamphetamine-using MSM residing in San Diego County, California, USA were recruited into the EDGE study between November 1999 and November 2004. Recruitment sources included gay organizations and groups, HIV-specialty health clinics, gay-identified venues and events, and referrals from care providers. Most participants were recruited through community-based service providers, poster media campaigns, and referrals from friends and active participants (45%, 30%, and 23%, respectively).
Due to budgetary constraints, HIV serostatus of the participant was determined by self-report. To assure a high level of accuracy regarding HIV serostatus, recruitment staff and counselors were trained to ask key questions and to remain alert to discrepancies in participants’ personal stories. No enrolled participants were suspected of falsifying their HIV serostatus. To be eligible for the study participants were required to: a) be HIV-positive, b) be male, c) be at least 18 years old, d) report having unprotected sex with at least one HIV-negative or serostatus unknown male partner during the previous four months, e) report they had snorted or smoked methamphetamine at least twice in the past 2 months and at least once in the past 30 days. Exclusion criteria included: a) unwillingness to participate in the intervention and all follow-up assessments; b) a current major psychiatric diagnosis accompanied by psychotic or suicidal symptoms; c) reporting only HIV-positive partners during the previous 4 months; d) reporting consistently protected sex with partners who were HIV-negative or were of unknown serostatus during the previous 4 months; e) not sexually active in the past 4 months; f) trying to get a partner pregnant (for bisexual men); g) have known HIV-positive serostatus for less than 4 months, and h) current enrollment in a drug treatment program. This study was registered with the NIH clinical trials registry. The IRB at the University of California San Diego approved the study and all participants signed a written, informed consent prior to enrollment.
2.2. Measures
2.2.1. Sex Practices
Participants were asked to report the number of times in the past 2 months they engaged in various sexual behaviors including anal, oral, and vaginal sex. For each sexual behavior they engaged in, a follow-up question asked the number of times these sexual acts were protected (i.e., used a condom or oral dam). Using these data, three outcome variables were established: a) Total protected sex, b) total unprotected sex, and c) percentage of total sex behaviors that were protected (i.e., ratio) by dividing protected sex behaviors by the total number of sex behaviors over the past 2 months.
2.2.2. Methamphetamine Use
Multiple indicators of methamphetamine use were utilized in the EDGE research project (Patterson et al., 2005). For the current study, a single item asked participants the amount of methamphetamine, in grams, they had used in the past 30 days.
2.2.3. Depressive Symptoms
All participants completed the 21-item Beck Depression Inventory (BDI; Beck and Steer, 1989). Higher scores indicate greater depressive symptoms.
2.2.4. Self-Efficacy for Condom Use
We asked participants to rate their confidence in performing 9 condom-related behaviors. These questions were as follows: a) “I can use a condom properly”, b) “I can use a condom every time I have penetrative sex”, c) “I can have condoms available every time I have penetrative sex”, d) “I can use a condom in any situation”, e) “I can interrupt sex to use a condom”, f) “I can use a condom without any instruction”, g) “I can use a condom for penetrative sex while under the influence of drugs or alcohol”, h) “I can delay penetrative sex if a condom is not available”, i) “I can use a condom for penetrative sex even when I am very sexually aroused”. Responses for each item ranged from 0 = “strongly disagree” to 3 = “strongly agree”. Responses to these 9 items were summed to create an overall self-efficacy score (range = 0–27). Alpha reliability for this scale was .86.
2.2.5. Self-Efficacy for Negotiating Safer Sex
All participants answered 7 questions pertaining to their self-efficacy for negotiation safer sex: a) “I can bring up the topic of safer sex with any partner”, b) “I can negotiate condom use with any partner”, c) “I could get my partner to use a condom if he/she doesn’t want to”, d) “I can convince my partner(s) that condoms are erotic”, e) “If a partner doesn’t want to use condoms, I can convince him/her to”, f) “Partners will agree to use condoms if I act hot”, and g) “I can persuade partners to try different types of condoms”. Responses to items on this scale ranged from 0 = “Strongly Disagree” to 3 = “Strongly Agree”. A total score was created by summing responses to the 7 items (range = 0–21), with higher scores representing greater self-efficacy. Alpha reliability for this scale was 0.86.
2.3. Intervention and Control Conditions
2.3.1. Common Elements of Intervention and Control Conditions
Both intervention and control conditions were manualized to ensure standardized delivery of content. Between the baseline and 4-month assessments, participants in both intervention and control conditions received 8 sessions of individual therapy. The first five intervention sessions occurred on a weekly basis with the remaining three sessions occurring every third week. Individualized counseling sessions were used for both conditions. Two Master’s level clinical psychologists served as counselors, with each counselor providing both the intervention and control conditions to ensure that each were exposed to an equal number of participants in each condition. All counselors attended a five-day training workshop that provided in-depth coverage of materials from each counseling module and booster session. The presentation for each module and booster included statement of purpose, specific aims, counseling activities, order of presentation, timetable of activities, and scripted examples of counselor-participant interactions. The training approach relied heavily upon demonstrations, role-plays, performance critiques, and corrective feedback. One day re-training workshops were conducted annually. To ensure counselor adherence to the protocol, three CDC-endorsed strategies were used: 1) Trainers observed each counselor in session once per week for a period of three weeks post-training; 2) All counseling sessions were audiotaped, with 10% of the tapes coded for accuracy of delivery by the project manager in accordance with a standardized checklist, and 3) At the end of each session, participants were asked to complete a brief checklist that queried the content of each counseling session (Kamb et al., 1996)..
2.3.2. EDGE Intervention
The intervention consisted of five weekly individual counseling sessions (90-minutes each) followed by three monthly booster sessions (90-minutes each), which were designed to reinforce behavior change. The intervention utilized a core set of constructs derived from social cognitive theory (Bandura, 1986; Bandura, 1994) and the Theory of Reasoned Action (Ajzen, 1991). Specifically, skills-training was used to help participants increase their knowledge, self-efficacy, and positive outcome expectancies in relation to a number of critical areas such as condom use, negotiation of safer sex practices (including sexual assertiveness), and disclosure of HIV serostatus to sex partners. The mechanisms of behavioral change involved observation, role modeling, skill performance (i.e., practice and rehearsal), positive feedback, reinforcement, and the development of supportive referents. The intervention was not designed to arrest or abate drug use. Instead, the focus was to reduce high risk sexual practices of methamphetamine-using HIV-positive MSM. Therefore, the behavioral strategies mentioned above were placed in the context of drug use. For example, the participant and counselor discussed how the use of methamphetamine interferes with motivation and preparedness for safer sex. Participants problem-solved ways in which they could be prepared to practice safer sex or how they could lower risk levels in the context of drug use (i.e., choosing harm reduction strategies such as seeking out HIV-positive partners, practicing oral sex instead of anal sex, limiting number and type of sex partners). The 5 modules encompassing this intervention are listed below:
1) The Context of Unsafe Sex (Triggers, Motivation, and Meaning)
This module utilized client-centered, motivational interviewing techniques to help the participant develop insights regarding motivations and triggers of unsafe sex and drug use behavior, including motivations underlying drug use behavior and unsafe sex, interactions between methamphetamine use and unsafe sex (e.g., examination of how the participant's preferences for certain types of sex acts change when using this drug), interactions among personal identities (e.g., sexual identity, HIV-positive identity, and drug user identity), drug use, and risky sex, and readiness for change. Risk reduction strategies were also introduced (e.g., discuss the feasibility of avoiding sexual settings such as bathhouses; seeking out partners who may be more likely to use condoms).
2) Condom Use
This module combined principles of motivational interviewing, social cognitive theory, and Theory of Reasoned Action. After assessing the individual's readiness for change in relation to condom use, the counselor worked with the participant to increase his awareness of current unsafe behaviors and their associated risks before proceeding with strategies on how to change his behavior. Once the participant identified motivations to change, he was actively involved in the process of problem-solving and was encouraged to come up with solutions. Counselors also began modeling safer sex behaviors and utilized role plays during this module.
3) Negotiation of Safer Sex Practices
During this module, participants learned and practiced five steps in the negotiation process; a) know what you want, b) know what you are willing to compromise, c) know as much as you can about your partner, d) have a backup plan, and e) rehearse negotiations (Dolan, 1992). Counselors modeled negotiation in the context of hypothetical sexual encounters, had the participant negotiate safer sex practices in hypothetical scenarios, provided supportive feedback on performance, and had the participant perform the task until a criterion of “strong negotiation” performance was achieved.
4) Disclosure of HIV Seropositivity to Sex Partners
During this module, the counselor and participant discussed a range of factors to be considered in relation to making the decision to disclose HIV serostatus. Modeling and role playing were used to enhance the individual's ability and confidence that he will be able to disclose to all partners without the fear of being rejected.
5) Enhancement of Social Support
The goal of this module was to help the participant enhance positive supports and minimize negative influences in relation to his safer sex goals. Problem-solving exercises were also used to help the participant: a) identify support buddies to help avoid high risk situations; b) learn ways to respond to drug-using friends who do not support safer sex goals; and c) develop a new network of friends who support safer sex goals (Rhodes and Malotte, 1996).
Following completion of these sessions, participants underwent three booster sessions at three week intervals following completion of the five core counseling modules. Booster sessions were time-equivalent (90 minutes) to the first five counseling sessions and covered the identical domains (e.g., context of sexual risk and meth use, condom use, negotiation, disclosure, social support). Sessions were focused on behavioral change experiences (e.g., new thoughts and feelings associated with change, satisfaction with outcomes, problems encountered, ambivalence experienced) and behavioral maintenance (e.g., importance and worthiness of change, strategies for staying motivated, precipitants of relapse, factors associated with success). Consistent with our theoretical framework, booster sessions used both motivational interviewing and social cognitive strategies to promote and reinforce positive behavior change and maintenance.
2.3.3. Diet-and-Exercise Intervention
The control condition was a manualized, 8-session intervention (90-minutes each) that addressed issues surrounding diet and exercise as they impact the health of HIV-positive MSM who use methamphetamine. For example, participants were taught the relationship between good nutrition and healthy immune systems, improved processing of medications taken by people with HIV, and the role of healthy diet and exercise in helping symptoms such as diarrhea, nausea, and fatigue.
2.4. Procedures and Data Collection
Study participants completed a “Sex Risk Appraisal” (SRA) and psychosocial interviews.. The SRA queried participants about their sexual behavior during the preceding two-month periods to maximize accuracy of reporting (i.e., minimize forgetfulness). Follow-up assessments were conducted at 4, 8, and 12 months post baseline. In an effort to minimize study attrition, a 4-month assessment interval was chosen for this drug-using population. Accordingly, the study was designed so that the first five counseling modules and the three booster sessions would be completed by the end of month three - allowing for a 30-day period between the completion of all intervention counseling and 4-month assessment.
Participant follow-up and tracking strategies on the EDGE project emphasized personal contact, responsiveness to special needs, flexibility in scheduling, subject payment, and special attention to the ongoing relevance and appeal of the program for HIV+ MSM. For example, we assigned study sponsors who maintained ongoing contact with participants, the acquisition of contact information for three persons, appointment reminder cards and phone calls, transportation services, mailed incentives, immediate contact following a missed appointment, a toll free project telephone line, and flexible office hours, including weeknights and weekends.
2.5. Data Analysis
Our study had three primary and two secondary outcomes. Our primary analyses assessed change in: a) total number of protected sex acts, b) total number of unprotected sex acts, and c) ratio of total protected-to-total sex acts. Our secondary analyses assessed change in self-efficacy for using condoms and self-efficacy for negotiating safer sex. Prior to conducting any analyses, the distribution of all variables was examined. Inspection of the distribution of variables indicated skewness in protected sex and unprotected sex that required log transformation; self-efficacy for condom use required square root transformation.
For all analyses, mixed (random-effects) regression analyses were used. Mixed regressions (i.e., multi-level models) allow us to estimate an intercept and slope for each participant based on all available data for that individual, augmented by the data from the entire sample. Participants were excluded if all their follow-up assessments were missing. For each outcome an initial model included fixed effects for time (i.e., coded as a linear variable whereby increments of 1 corresponded to 4-month intervals), intervention (0 = control condition; 1 = intervention), and a time squared term to test for nonlinear time effects (e.g., steeper change during the initial treatment phase with leveling off of changes between 4 and 12-months post-baseline). The time squared term was significant for two of our outcomes; i.e., unprotected sex and ratio of total protected-to-total sex acts. Therefore, for these two outcomes time squared was retained for analysis. All other outcomes (i.e., protected sex, self-efficacy for condom use, self-efficacy for negotiating safer sex) examined only the linear effect of time.
For our analysis of protected sex and both self-efficacy variables, we included main effects for time and intervention, along with a time-by-intervention interaction term. For our other two outcomes (unprotected sex and ratio of total protected-to-total sex acts), two product terms were used to test the time-by-intervention interaction: a) time-by-intervention, and b) time squared-by-intervention. A two-tailed alpha level of p=0.05 was used to determine statistical significance for all analyses.
3. Results
3.1. Participant Flow and Demographic Characteristics of the Sample
Figure 1 shows the flow of participants throughout the study. Nine hundred seventy-three participants were screened for the project over a five-year period. Three hundred forty one participants met our inclusion/exclusion criteria and completed the baseline assessment. Reasons for ineligibility were (in rank order): 1) had not used methamphetamine at least twice in the past 2 months and once in the past 30 days (35%); 2) had not had unprotected sex with an HIV negative or unknown partner in the past 2 months (20%); 3) not sexually active in the past 2 months (15%); 4) HIV-negative or unknown serostatus (15%); 5) currently enrolled in drug treatment program (8%); and 6) severe mental health problems or repeat incidents of extreme intoxication at screening (7%). Of the 340 enrolled participants, 170 were randomized to the EDGE intervention and 171 were randomized to the control (D&E) condition. A total of 262 (EDGE = 126; D&E = 136) participants (76.8%) completed at least one follow-up assessment. Compared to these 262 “completers”, participants who did not complete at least 1 follow-up were significantly younger (37.5 vs. 35.6 years; p = 0.048), but did not differ in terms of their intervention assignment, education, income, ethnicity, employment status, methamphetamine use, depressive symptoms, or sexual behavior (all p-values > 0.05). Of the full sample, approximately 61%, 57%, and 53% completed the 4-, 8-, and 12-month assessments, respectively. The two intervention conditions did not differ significantly at any follow-up in terms of retention rates (all p-values > 0.10).
Figure 1.
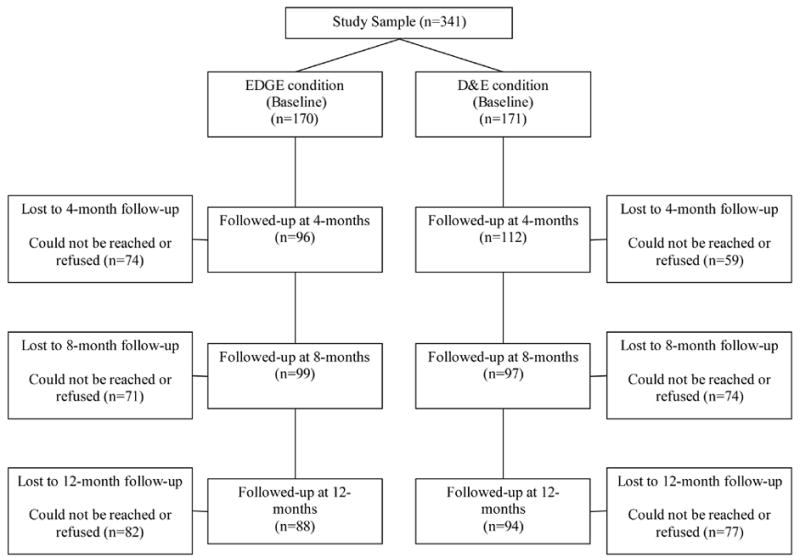
Flow of participants throughout the study. At all time points, the sum of participants who completed follow-up and those lost to follow-up equals 170 for the EDGE condition and 171 for the D&E condition because some participants who were unable to complete one follow-up were able to participate in a subsequent assessment.
Baseline characteristics of the sample can be found in Table 1. Participants had a mean age of 37 years (range = 20–61), 77% identified themselves as homosexual (n = 264), 23% (n = 77) identified as bisexual, and 57% were Caucasian (n = 195). On average, participants used 5 grams (range = 1–102) of methamphetamine over the 30 days prior to enrollment and had an average Beck depression (BDI) score of 15 (SD = 9.9). There were no significant differences between intervention conditions on any baseline characteristics.
Table 1.
Baseline Characteristics of Sample
| EDGE (n = 170) | D&E (n = 171) | t | χ2 | p | |
|---|---|---|---|---|---|
| Age, M (SD) | 37.42 (7.11) | 36.76 (7.58) | 0.82 | .413 | |
| Sexual Orientation, n (%) | 2.25 | .522 | |||
| Homosexual | 129 (76) | 135 (79) | |||
| Bisexual | 39 (23) | 31 (18) | |||
| Participant Not Sure | 2 (1) | 4 (3) | |||
| Race, n (%) | |||||
| Caucasian | 93 (55) | 101 (59) | 4.25 | .514 | |
| African American | 38 (22) | 34 (20) | |||
| Hispanic/Latino | 27 (16) | 17 (10) | |||
| Asian/Pacific Islander | 1 (1) | 1 (1) | |||
| Native American | 5 (3) | 9 (5) | |||
| Other | 6 (3) | 8 (5) | |||
| Education, n (%) | |||||
| Less than High School | 18 (11) | 27 (16) | 2.24 | .523 | |
| High School Diploma | 48 (28) | 42 (25) | |||
| Some College | 64 (38) | 62 (36) | |||
| College graduate | 40 (23) | 39 (23) | |||
| Currently Employed, n (%) | 50 (29) | 40 (23) | 1.51 | .219 | |
| Years HIV-positive, M (SD) | 7.23 (6.12) | 6.86 (5.90) | 0.56 | .577 | |
| Methamphetamine Use, past 30 days (grams), M (SD) | 5.32 (12.32) | 5.48 (10.82) | −0.13 | .899 | |
| Days of Methamphetamine Use, past 30 days, M (SD) | 10.27 (8.95) | 10.70 (9.04) | −0.44 | .664 | |
| BDI Score, M (SD) | 15.48 (10.58) | 14.98 (9.15) | 0.45 | .651 | |
| Protected Sex Behaviors, M (SD) | 5.75 (14.70) | 11.16 (59.46) | −1.15 | .251 | |
| Unprotected Sex Behaviors, M (SD) | 59.63 (73.27) | 66.96 (159.50) | −0.54 | .587 | |
| Self-Efficacy for Condom Use, M (SD) | 19.56 (5.98) | 20.86 (5.17) | −2.14 | .033 | |
| Self-Efficacy for Negotiating Safer Sex, M (SD) | 12.72 (5.05) | 12.27 (4.92) | 0.83 | .408 | |
Note. One participant in control condition refused to provide demographic data.
3.3. Adherence to Treatment Conditions
Participants randomly assigned to the EDGE intervention attended, on average, 6.32 (SD=2.37) treatment sessions, or 79% of the total possible sessions. In addition, 55% (n=94) attended all 8 sessions. Participants randomized to the D&E condition attended an average of 6.77 (SD=2.03), or 85% of treatment sessions. Sixty-four percent (n=110) of D&E participants attended all 8 sessions.
3.4. Effect of Interventions on Sex Behaviors
Results presented in text are for log transformed variables, where applicable Table 2 presents means and standard errors for the EDGE and D&E interventions at each time point. We first examined the effect of our interventions on protected sex over time. Results indicated a significant effect of time (t = −2.87, df = 620.75, p = 0.004) and a significant time-by-intervention interaction (t = 2.59, df = 623.85, p = 0.010). Post-hoc analyses for each of our assessment points indicated that EDGE participants engaged in significantly greater amounts of protected sex at 8-months (t = 2.13, df = 283.98, p = 0.034) and 12-months post-baseline (t = 2.72, df = 480.13, p =0.007).
Table 2.
Estimated means and standard errors for EDGE and D&E participants across the study.
| Assessment
|
||||
|---|---|---|---|---|
| Baseline M (SE) | 4-months M (SE) | 8-months M (SE) | 12-months M (SE) | |
| (log) Protected Sex | ||||
| D&E | 1.11 (0.09) | 1.01 (0.08) | 0.91 (0.08) | 0.81 (1.00) |
| Edge | 1.11 (1.00) | 1.14 (0.08) | 1.17 (0.08)* | 1.19 (1.00)* |
| (log) Unprotected Sex | ||||
| D&E | 3.25 (0.11) | 2.74 (0.10) | 2.52 (0.11) | 2.59 (0.11) |
| Edge | 3.25 (0.11) | 2.88 (0.10) | 2.64 (0.10) | 2.52 (0.11) |
| Ratio of total protected-to-total sex acts (%)a | ||||
| D&E | 15.11 (2.35) | 20.20 (2.15) | 21.41 (2.26) | 18.73 (2.40) |
| Edge | 14.81 (2.42) | 21.19 (2.14) | 24.85 (2.26) | 25.79 (2.40)* |
| (sqrt) SE Condom Use | ||||
| D&E | 3.05 (0.09) | 3.05 (0.08) | 3.06 (0.08) | 3.06 (0.10) |
| Edge | 2.86 (0.09) | 2.98 (0.08) | 3.09 (0.08) | 3.21 (0.10) |
| (sqrt) SE Negotiation | ||||
| D&E | 1.83 (0.09) | 1.90 (0.08) | 1.96 (0.08) | 2.02 (0.09) |
| Edge | 1.93 (0.09) | 2.03 (0.08) | 2.13 (0.08) | 2.23 (0.09) |
p < .05.
Ratio was calculated using raw (untransformed) values for sexual activity and is the percentage of total sex which was protected.
SE = Self-Efficacy.
We next examined group differences in total unprotected sex over time. Results of these analyses indicated a significant effect of time (t = −6.09, df = 689.72, p <0.001) and for time squared (t = 4.71, df = 739.96, p < 0.001), suggesting D&E participants experienced an initial decline with an eventual leveling off. In addition, there was a significant time squared-by-group interaction (t = −2.17, df = 760.48, p = .030). Examination of the data indicated that although both D&E and EDGE participants demonstrated initial declines in unprotected sex, only EDGE participants continued to decline throughout the entire 12-month study period. However, post-hoc analyses indicated EDGE and D&E participants did not differ in unprotected sex at any outcome point. Specifically, D&E participants engaged in slightly less unprotected sex at 4- and 8-month follow-ups, but slightly more unprotected sex at the 12-month follow-up (see Table 2).
Finally, we examined change in the ratio of total protected-to-total sex acts. Results demonstrated a significant main effect of time (t = 3.12, df = 683.20, p = 0.002) and time squared (t = −3.00, df = 732.85, p = 0.003), again suggesting that D&E participants demonstrated an initial increase in the ratio followed by a leveling off. The time-by-intervention and time squared-by-intervention interactions were both non-significant. Post-hoc analyses indicated that of all sex acts, EDGE participants engaged in a greater percentage of protected sex than D&E participants at the 12-month assessment. A graphical depiction of change in the ratio over time for D&E and EDGE participants is depicted in Figure 2, panel A.
Figure 2.
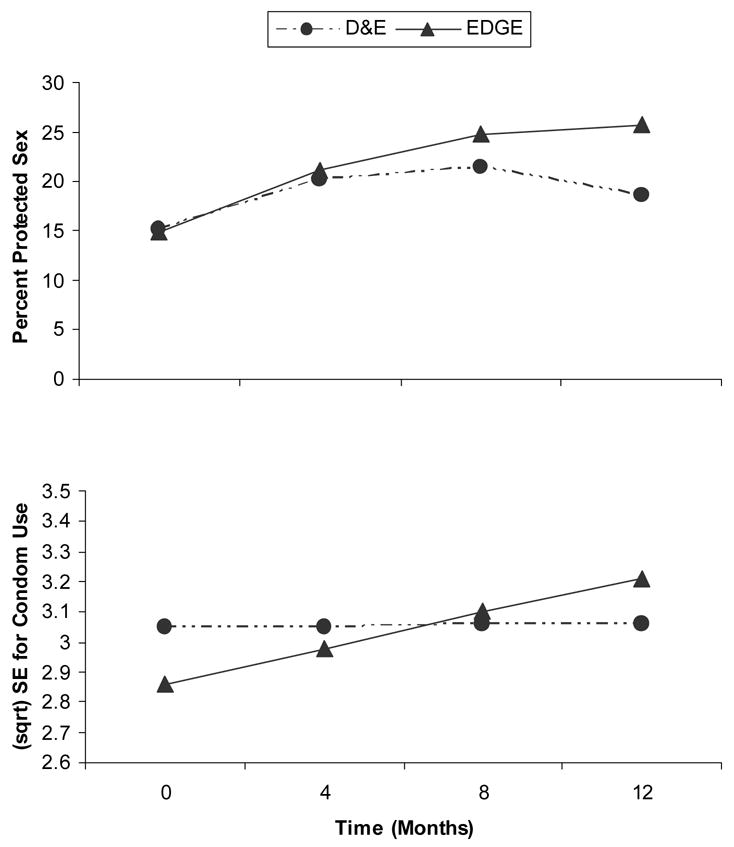
Panel A (top). Percentage of all sexual activity that was protected by treatment condition over time. Panel B (bottom). Change in Self-Efficacy for Condom Use by Treatment Condition. The slope for EDGE participants was significant (p = .001), but not for D&E participants (p = .982).
3.5. Effect of Interventions on Secondary Outcomes
Results of our random regression analysis of self-efficacy for condom use indicated a significant time-by-intervention interaction (t = 2.37, df = 721.65, p = .018), whereby the increase in self-efficacy was greater for the EDGE vs. D&E intervention. Post-hoc analyses confirmed that the within group slope for the D&E intervention was not significant (t = 0.02, df = 717.89, p = .982), whereas the slope for the EDGE intervention was significant (t = 3.39, df = 725.48, p = .001). Slopes for the two interventions are presented graphically in Figure 2, panel B.
Results for self-efficacy for negotiating safer sex indicated no significant time-by-intervention interaction (t = 0.88, df = 720.47, p = .380). Examination of within-group slopes indicated both the D&E (t = 2.01, df = 716.77, p = .045) and EDGE (t = 3.28, df = 724.24, p = .001) participants significantly increased in self-efficacy for negotiation over time. Although these slopes did not significantly differ, EDGE participants’ slopes were steeper than those of D&E participants in the expected direction.
4. Discussion
This study compared a theory-based behavioral intervention to a time-equivalent diet and exercise control condition on long-term improvements and maintenance of safer sex behaviors in a sample of HIV-positive methamphetamine-using MSM. We found that by the end of the active phase of the interventions (i.e., 4-months) the two groups did not differ in their safer sex behaviors. However, by 8-months post-baseline, participants in the EDGE intervention engaged in significantly more protected sex acts than those in the control intervention. This difference was maintained at the 12-month assessment. In addition, at the 12-month assessment, participants in the EDGE intervention engaged in a greater percentage of safer sex behaviors than control participants. Given that participants in both conditions significantly reduced their unprotected sex behaviors, these results suggest that by 12 months, EDGE participants’ risk exposure was significantly lower than that of the control participants.
The EDGE intervention was also superior to the control condition for increasing self-efficacy for condom use. Self-efficacy is very important in predicting actual success in a particular domain, as self-efficacy beliefs affect the initiation of behaviors (i.e., using a condom), how intensely behaviors are pursued, and the extent to which behaviors are maintained in the face of deterrence (Bandura, 1986; Bandura, 1997). To this end, we believe one of the strongest reasons that participants in the control intervention were not able to maintain their initial gains in safer sex behaviors (i.e., ratio of total protected-to-total sex acts) was because they had a complete absence of any change in self-efficacy for condom use. In contrast, participants in the EDGE intervention demonstrated both initial and long-term change in safer sex behaviors, likely due to their continued increase in both condom self-efficacy and self-efficacy for negotiating safer sex. These findings are important as they suggest that the EDGE intervention may aid participants in maintaining benefits over longer periods of time.
While other interventions for HIV-positive MSM have also demonstrated promise in increasing safer sex behaviors (Kelly et al., 1990; Kelly et al., 1989; Patterson et al., 2003; Peterson et al., 1996), most of these interventions were not conducted with drug users, or users of methamphetamine in particular. Recently, however, in a Los Angeles based study of treatment-seeking MSM, Reback et al (2004) demonstrated that treatment for methamphetamine use was associated with more safer sex at one-year follow-up. Participants were less “compulsive” and reported a greater capacity to reduce sexual risk behaviors such as unprotected oral and anal sex and fisting; participants also had fewer sex partners and a greater willingness to disclose their HIV-positive serostatus. In another study by the same group, Shoptaw and colleagues (2005) evaluated the efficacy of four treatment conditions designed to reduce high risk sexual behaviors and methamphetamine use in a sample of gay and bisexual men. Participants in the cognitive behavior therapy condition, which was culturally tailored to MSM lifestyles, showed significant reductions in unprotected receptive anal sex during the first four weeks of the intervention as compared to participants in the other three groups. The present study contributes to this body of literature by providing support for the long-term efficacy of a sexual risk reduction program among HIV-positive MSM. However, our intervention was unique from previous studies in that we examined the efficacy of a sexual risk reduction intervention conducted within the context of active, ongoing methamphetamine use. Our results indicate that successful long-term reductions in sexual risk behaviors within this population may be achieved, and that reductions in high risk sexual behavior among methamphetamine using MSM can be reduced through emphasis on increasing self efficacy, rather than reducing drug use.
One strength of our study was the inclusion of a time-equivalent, active control condition. Specifically, participants in the control condition were taught the importance of engaging in a healthy lifestyle through diet and nutritional choices and exercise. We believe it is likely that participants in this condition applied the message of “healthy lifestyle” to sexual behavior as well, as evidenced by a decrease in unprotected sex over the course of the study and an increase in the percentage of protected sex during the active phase of the intervention. However, we believe that the effects of our attention-control condition did not last because participants did not develop sex-specific skills (e.g., how to recognize triggers for unsafe sex and methamphetamine use; increased self-efficacy for condom use, etc.) which were targets of the EDGE intervention. Indeed, control participants demonstrated absolutely no change in their self-efficacy for condom use over the 12-months study period. In contrast, EDGE participants demonstrated increases in both self-efficacy for condom use and negotiating safer sex, and we believe participants in the EDGE intervention were able to successfully apply these skills to specific circumstances deemed to be sexually risky.
Our EDGE intervention did not actively address participants’ methamphetamine use. Recent scientific evidence suggests that among MSM, both light and heavier drug use is significantly associated with increased risk of engaging in unprotected anal sex with an HIV-positive or unknown-status partner (Colfax et al., 2005), and that risk for engaging in unprotected anal intercourse is greater when MSM use methamphetamine (Rusch et al., 2004). However, research also suggests that gay and bisexual methamphetamine users demonstrate significant decreases in sexual risk behaviors following substance abuse treatment (Reback et al., 2004). Although it is yet to be tested, an intervention combining substance abuse treatment with behavioral strategies specific to reducing sexual risk behaviors may be particularly effective for reducing risk for HIV transmission. We encourage examination of this hypothesis.
Attrition for this project was higher than one would like to see. A few observations may guide those who work with this population in the future. First, in our zeal to have a representative sample we initially enrolled individuals who had unstable housing situations. This proved to be a problematic decision since many of these individuals became homeless and were lost to follow-up across the study. Our tracking information focused primarily on family and friends. While each of these sources of information proved to be helpful, we discovered that a more detailed history of living situations and contacts with each of those situations was also needed. Not surprisingly legal problems occurred frequently in this population. However, the multitude of legal systems made it difficult to develop all of the IRB safeguards and gain approvals from each judicial system that would allow us to contact incarcerated participants.
In sum, our study demonstrates the efficacy of a behavioral skills intervention for increasing safer sex behaviors in a sample of HIV-positive methamphetamine-using MSM. Specifically, helping members of this population increase their knowledge, self-efficacy, and positive outcome expectancies for skills such as condom use, negotiation of safer sex practices, and disclosure of HIV serostatus to sex partners can produce long-term change in safer sex practices despite ongoing methamphetamine use, which in turn may reduce the transmission of HIV. Finally, it is possible that augmenting this intervention with ongoing substance abuse treatment can produce even larger gains in safer sex behaviors.
Acknowledgments
This research was supported by the National Institute on Drug Abuse award DA 012116.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ajzen I. The Theory of Planned Behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- Bandura A. Social Learning Theory. Prentice Hall; Englewood Cliffs, NJ: 1977. [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente R, Peterson J, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. Plenum Publishing Corp; New York: 1994. pp. 25–59. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. W. H. Freeman; New York: 1997. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Depression Inventory. The Psychological Corporation; San Antonio, TX: 1989. [Google Scholar]
- Boddiger D. Metamphetamine use linked to rising HIV transmission. Lancet. 2005;365:1217–1218. doi: 10.1016/S0140-6736(05)74794-2. [DOI] [PubMed] [Google Scholar]
- Booth RE, Watters JK. How effective are risk-reduction interventions targeting injecting drug users? AIDS. 1994;8:1515–1524. doi: 10.1097/00002030-199411000-00001. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Goldsamt LA, Yi H. Club drug use among young men who have sex with men in NYC: A preliminary epidemiological profile. Subst Use Misuse. 2005;40:1317–1330. doi: 10.1081/JA-200066898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, Chesney M, Vittinghoff E. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of san francisco men who have sex with men. J Urban Health. 2005;82(1):i62–70. doi: 10.1093/jurban/jti025. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle SL, Needle RH, Normand J. Outreach-based HIV prevention for injecting drug users: A review of published outcome data. Public Health Rep. 1998;113(Suppl 1):19–30. [PMC free article] [PubMed] [Google Scholar]
- Dolan JP. Negotiate Like the Pros. Perigee Books; New York: 1992. [Google Scholar]
- Fernández MI, Bowen GS, Varga LM, Collazo JB, Hernandez N, Perrino T, Rehbein A. High rates of club drug use and risky sexual practices among Hispanic men who have sex with men in Miami, Florida. Subst Use Misuse. 2005;40:1347–1362. doi: 10.1081/JA-200066904. [DOI] [PubMed] [Google Scholar]
- Gibson DR, McCusker J, Chesney M. Effectiveness of psychosocial interventions in preventing HIV risk behaviour in injecting drug users. AIDS. 1998;12:919–929. doi: 10.1097/00002030-199808000-00015. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: crystal methamphetamine drug use in relation to HIV transmission among gay men. J Homosex. 2001;41:17–35. doi: 10.1300/J082v41n02_02. [DOI] [PubMed] [Google Scholar]
- Johnson WD, Hedges LV, Diaz RM. Interventions to modify sexual risk behaviors for preventing HIV infection in men who have sex with men. Cochrane DataBase Syst Rev. 2003:CD001230. doi: 10.1002/14651858.CD001230. [DOI] [PubMed] [Google Scholar]
- Kamb M, Dillon B, Fishbein M, Willis K the project RESPECT study group. Quality assurance of HIV prevention counseling in a multi-center randomized controlled trial. Public Health Reports. 1996;111(Supp 70):503–509. [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Betts R, Brasfield TL, Hood HV. A skills-training group intervention model to assist persons in reducing risk behaviors for HIV infection. AIDS Educ Prev. 1990;2:24–35. [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Hood HV, Brasfield TL. Behavioral intervention to reduce AIDS risk activities. J Consult Clin Psychol. 1989;57:60–67. doi: 10.1037//0022-006x.57.1.60. [DOI] [PubMed] [Google Scholar]
- Kanouse DE, Bluthenthal RN, Bogart L, Iguchi MY, Perry S, Sand K, Shoptaw S. Recruiting drug-using men who have sex with men into behavioral interventions: A two-stage approach. Journal of Urban Health. 2005;82(1):i109–i119. doi: 10.1093/jurban/jti030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzger DS, Navaline H, Woody GE. Drug abuse treatment as AIDS prevention. Public Health Rep. 1998;113(Suppl 1):97–106. [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. Guilford Press; New York: 1991. [Google Scholar]
- Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med. 1998;168:93–97. [PMC free article] [PubMed] [Google Scholar]
- National Association of Counties (NACO. The meth epidemic in America. [Accessed on August 8, 2006];A 2006 survey of U.S. Counties. 2006 http://www.naco.org/Content/ContentGroups/Publications1/Surveys1/Special_Surveys/MethSurveyReport-Jul2006.pdf.
- Neaigus A. The network approach and interventions to prevent HIV among injection drug users. Public Health Rep. 1998;113(Suppl 1):140–150. [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Zians JK, Strathdee SA. Methamphetamine-using HIV-positive men who have sex with men: Correlates of polydrug use. J Urban Health. 2005;82(1 Suppl 1):i120–126. doi: 10.1093/jurban/jti031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Shaw WS, Semple SJ. Reducing the sexual risk behaviors of HIV+ individuals: Outcome of a randomized controlled trial. Ann Behav Med. 2003;25:137–145. doi: 10.1207/S15324796ABM2502_10. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Coates TJ, Catania J, Hauck WW, Acree M, Daigle D, Hillard B, Middleton L, Hearst N. Evaluation of an HIV risk reduction intervention among African-American homosexual and bisexual men. AIDS. 1996;10:319–325. doi: 10.1097/00002030-199603000-00011. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Parsons JT, Halkitis PN, Mizuno Y, Woods WJ. Substance use and sexual transmission risk behavior of HIV-positive men who have sex with men. J Subst Abuse. 2001;13:185–200. doi: 10.1016/s0899-3289(01)00072-4. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Ditman D. The social construction of a gay drug: Methamphetamine use among gay and bisexual males in Los Angeles. Los Angeles, CA: AIDS Coordinator; 1997. [Google Scholar]
- Reback CJ, Larkins S, Shoptaw S. Changes in the meaning of sexual risk behaviors among gay and bisexual male methamphetamine abusers before and after drug treatment. AIDS Behav. 2004;8:87–98. doi: 10.1023/b:aibe.0000017528.39338.75. [DOI] [PubMed] [Google Scholar]
- Rhodes F, Malotte CK. HIV risk interventions for active drug users: Experience and prospects. In: Oskamp S, Thompson S, editors. Understanding and preventing HIV risk behavior: Safer sex and drug use. Sage Publications; Thousand Oaks: 1996. pp. 207–235. [Google Scholar]
- Rusch M, Lampinen TM, Schilder A, Hogg RS. Unprotected anal intercourse associated with recreational drug use among young men who have sex with men depends on partner type and intercourse role. Sex Transm Dis. 2004;31:492–498. doi: 10.1097/01.olq.0000135991.21755.18. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. Partner type and sexual risk behavior among HIV positive gay and bisexual men: Social cognitive correlates. AIDS Educ Prev. 2000;12:340–356. [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. Motivations associated with methamphetamine use among HIV+ men who have sex with men. J Subst Abuse Treat. 2002;22:149–156. doi: 10.1016/s0740-5472(02)00223-4. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. Determinants of condom use stage of change among heterosexually-identified methamphetamine users. AIDS Behav. 2004;8:391–400. doi: 10.1007/s10461-004-7323-4. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Reback CJ, Freese TE. Patient characteristics, HIV serostatus, and risk behaviors among gay and bisexual males seeking treatment for methamphetamine abuse and dependence in Los Angeles. J Addict Dis. 2002;21:91–105. doi: 10.1300/j069v21n01_08. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, Veniegas RC, Freese TE, Hucks-Ortiz C. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol Depend. 2005;78:125–134. doi: 10.1016/j.drugalcdep.2004.10.004. [DOI] [PubMed] [Google Scholar]
- U.S. Dept. of Health and Human Services. The NSDUH Report: Methamphetamine Use, Abuse, and Dependence: 2002, 2003, and 2004. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2005. [Google Scholar]
- United Nations Office on Drugs and Crime. Global Ilicit Drug Trends. [accessed on May 30, 2006];2003 http://www.unodc.org/unodc/en/global_illicit_drug_trends.html.
- Urbina A, Jones K. Crystal methamphetamine, its analogues, and HIV infection: medical and psychiatric aspects of a new epidemic. Clin Infect Dis. 2004;38:890–894. doi: 10.1086/381975. [DOI] [PubMed] [Google Scholar]


