Abstract
Despite medical and scientific advances, racial and ethnic disparities persist in US asthma morbidity and mortality rates. Progress in the elimination of these disparities will involve disentangling the contribution of social constructs, such as race, socioeconomic status, and culture, from that of the physical environment and genetic susceptibility. One approach to reducing asthma disparities is through the traditional disease prevention stages of intervention. As such, primary prevention targets reductions in asthma incidence; secondary prevention is the mitigation of established disease and involves disease detection, management, and control; and tertiary prevention is the reduction of complications caused by severe disease. Once causative factors at each level of disease prevention are understood, this knowledge can be translated into clinical practice and public health policy.
Keywords: Asthma, racial disparities, disease prevention
The United States and other industrialized countries struggle to understand the basis for the worldwide increase in asthma and allergic disease.1,2 Researchers in the United States have a dual burden in this regard because asthma morbidity and mortality are highest among persons who are poor or of minority status.
Recent discussions concerning the concept of race in epidemiologic research are pertinent to understanding asthma disparities, which are often unexplained by adjustments for socioeconomic status (SES) and health care access.3-5 Within class strata, measures of income and education seldom translate into the same level of wealth for minorities when compared with whites.6 The consequence of this phenomenon means that a true adjustment for the minority experience in the United States using traditional demographic variables is problematic.
It is important to distinguish race as a risk marker as opposed to a risk factor.7 The former implies a collinear relationship between race and a measured variable, whereas the latter is better conceptualized as a shared ancestry, resulting in a genetic profile associated with variations in disease susceptibility.7 Failure to determine this distinction can lead to spurious associations. Progress in asthma research will involve disentangling the contribution of social constructs, such as race, SES, and culture, from that of the physical environment and genetic susceptibility.
Source material for this review included English-language articles identified from the MEDLINE and PubMed databases by using combinations of the following search terms: “racial disparity,” “ethnology,” “asthma,” “allergy (and hypersensitivity),” and “atopy.” Included were articles published from 1996 to the present, with the exception of key articles published before this time period. Articles were also identified through experts in the field and the bibliographies of pertinent studies.
ASTHMA DISPARITIES IN THE UNITED STATES
According to the 2002 estimates from the US National Center for Health Statistics, current asthma prevalence is highest for Puerto Rican Americans (13.1%), followed by Native Americans (9.9%), non-Hispanic blacks (9.5%), non-Hispanic whites (7.2%), and Mexican Americans (3.6%). Asthma attack prevalence follows a similar trend (Fig 1).8
FIG 1.
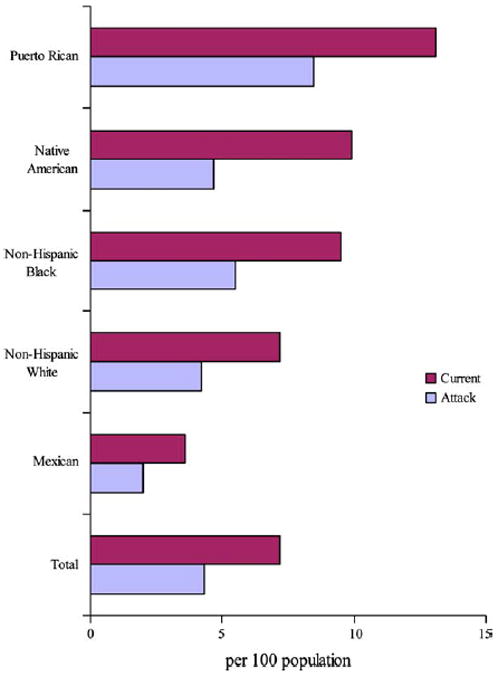
Current asthma and asthma attack prevalence, 2002. Rates are age adjusted to 2000 population. Source: Centers for Disease Control and Prevention/National Center for Health Statistics/National Hospital Ambulatory Medical Care Survey and National Hospital Discharge Survey.
Despite overall decreases in US asthma morbidity and mortality over the last decade, racial-ethnic disparities persist (Fig 2). Emergency department (ED) visit rates for 2002 for African Americans are 2 to 4 times that of whites (21.7/1000 vs 4.5/1000), as are asthma hospitalizations (11/1000 vs 3.6/1000) and deaths (3.7/100,000 vs 1.2/100,000). Age-adjusted mortality rates for US Hispanics available for 1990 through 1995 were 4.1 per 100,000 for those of Puerto Rican heritage, and 0.9 per 100,000 for Mexican Americans compared with 1.5 per 100,000 for non-Hispanic whites.9
FIG 2.
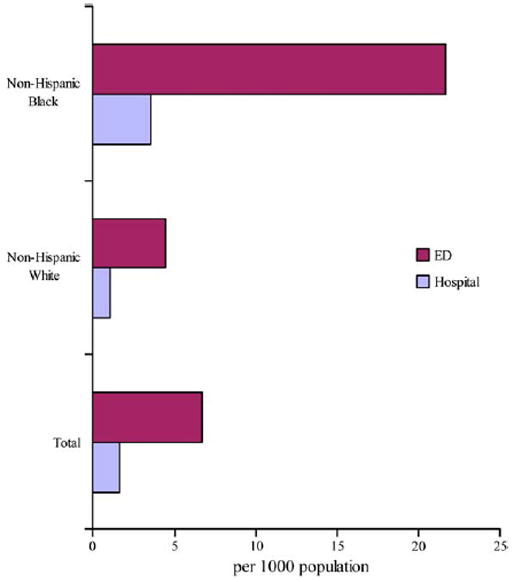
Asthma ED and hospital visits, 2002. Rates are age adjusted to 2000 population. Source: Centers for Disease Control and Prevention/National Center for Health Statistics/National Health Interview Survey.
RACE, ETHNICITY, AND ASTHMA PHENOTYPES
Phenotypically, asthma appears to vary by race and ethnicity. Differences in asthma characteristics, such as bronchial hyperresponsiveness, IgE, and allergic sensitization, might indicate different phenotypic expressions for one disease or perhaps be an indication of different diseases.
Total IgE
The pivotal role of IgE in allergic asthma is undisputed, but the clinical significance of IgE in nonallergic asthma is less understood. Recent studies suggest that among persons with asthma, the nonatopic variant is more prevalent among African Americans when compared with whites.10,11 These findings have implications for studying racial-ethnic differences in asthma because dissimilarities often center on IgE. For example, studies in the United States and Canada have shown that Hispanics, Asians, and blacks have higher cord blood IgE levels when compared with non-Hispanic whites.12,13 In a cross-sectional study of middle-class children in suburban Detroit, total IgE levels were higher for African Americans when compared with those of whites.14 Total IgE levels were not associated with asthma status among African American children, but this association was present in whites. In this study total serum IgE level was related to bronchial hyperreactivity in whites but not African Americans. A better understanding is needed of how the role of IgE in asthma might differ by race-ethnicity.
Bronchial hyperresponsiveness
Racial differences in bronchial hyperreactivity, a hallmark of asthma, have been reported. In the Michigan study of middle-class suburban children, African Americans had lower forced vital capacity and FEV1 values when compared with whites, and the former were also less likely to respond to a bronchodilator.14 Burchard et al15 have reported reduced lung function differences among Latino Americans. Puerto Ricans had significantly lower FEV1 when compared with Mexicans, although all values were within the normal range. Additionally, Puerto Ricans had, on average, 7.3% lower bronchodilator reversibility in FEV1. These results might have implications for spirometry references values, which are already adjusted for African Americans and Hispanics; however, the relationship of these differences to asthma incidence and severity should also be further explored.
Allergic sensitization
Differences in allergic sensitization by race-ethnicity have also been reported. Joseph et al14 reported a higher frequency of sensitization to bluegrass for African Americans compared with whites in the Michigan study of middle-class children. A heightened risk of sensitization to indoor (including cockroach) and outdoor allergens for Puerto Rican children was reported in a multiethnic study conducted in Hartford, Connecticut.16 In that study African Americans were also shown to have more sensitization to outdoor allergens. Litonjua et al,11 in a study of 882 female Boston residents, also noted that certain environmental allergens were significantly related to SES (eg, cockroach, mouse, and dust mite) and that sensitization to these allergens was more prevalent among African American and Hispanic females in the study when compared with non-Hispanic whites. Because race and SES were so tightly linked in these last 2 studies, the independent contribution of each to observed differences in IgE levels could not be fully assessed, despite efforts to adjust for poverty by using census-based information. Nonetheless, a heightened susceptibility to allergic sensitization might translate into increased risk or more severe disease among minorities. A case-control study conducted by Gelber et al17 of mostly whites and African Americans showed that adults who present to the ED for acute asthma were 7 times more likely to be sensitized to 3 or more allergens and have high levels of allergen in the home when compared with control subjects.
Of note is that an Australian study by Ponsonby et al18 showed that atopy is overrepresented among children with severe asthma. Thus, differences in allergic sensitization by race-ethnicity in those with allergic asthma might influence both the development of asthma and its severity once established.
RACE, ETHNICITY, AND ASTHMA GENETICS
The genetically complex nature of asthma is illustrated by the numerous polymorphisms that have been associated with asthma diagnosis, disease severity, and response to therapy.19-24 Differences in the frequency of these polymorphisms by both race and ethnicity have also been described.23,25-27 The relative contribution of these genotypic differences to asthma disparities is currently unknown. It is important to note that although there is clearly genetic variability between racial and ethnic groups, there is also substantial variability within groups.28-30 Therefore current US census categories should not be considered monolithic. For example, in a recent study of polymorphisms in the31 Β2-adrenergic receptor, Choudhry et al showed that the Arg16 allele was associated with asthma severity and bronchodilator responsiveness in Puerto Ricans but not in Mexicans, suggesting an additional gene-gene or gene-environment interaction in one of these groups.
RACIAL DISPARITIES IN THE CONTEXT OF DISEASE PREVENTION
The concept of disease prevention encompasses an understanding of the cause and consequences of disease in populations and is often described at the stage of intervention (ie, primary, secondary, and tertiary). Ways to reduce racial disparities in asthma can also be discussed in this context. As such, primary prevention targets reductions in asthma incidence through the identification and elimination of exposure to risk factors that are more common among minorities. Secondary prevention is the mitigation of established disease and involves disease detection, management, and control, all of which might be suboptimal in minority populations. Tertiary prevention, the reduction of disease complications, involves identifying race differences in the treatment and control of severe disease and factors related to asthma mortality. Reducing racial disparities in asthma will require that contributing factors at each level of disease prevention are understood and that this knowledge be translated into clinical practice and public health policy.
PRIMARY PREVENTION: ELIMINATION OR REDUCTION OF FACTORS RELATED TO ASTHMA INCIDENCE
Race, ethnicity, and asthma incidence
Few US studies specifically provided detailed asthma incidence rates and none by race.32-35 Beckett et al35 used data from a large multicenter study on coronary artery risk to evaluate weight gain and, in this case, cumulative incidence of asthma. Among the 4547 young adults aged 18 to 30 years, the 10-year cumulative incidence of asthma was 6.7%, 10.5%, 5.4%, and 9.7% for black males, black females, white males, and white females, respectively. The Children’s Health Study, a prospective study of 3792 fourth through tenth graders did report an overall incidence rate of asthma (2.5/100 person-years) but not race-specific rates.33 Compared with non-Hispanic whites, the relative risk of new-onset asthma was 1.05 (95% CI, 0.70–1.57) for Hispanics and 1.53 (95% CI, 0.77–3.02) for blacks, although the latter made up less than 6% of the study population.33 A recent study of lead exposure used claims and encounter databases for 4634 managed care enrollees (70% African American) and reported incidence rates by race. The incidence rate of asthma for African American children was 3.0 per 100 person-years versus 1.2 per 100 person-years for white children (P < .01). Adjusting for birth weight, sex, and SES did not alter this difference.5 Clearly, basic knowledge regarding racial differences in asthma incidence rates is lacking.
Race, ethnicity, and risk factors for asthma
Risk factors prevalent in minority populations, such as obesity and low birth weight, might affect asthma risk. It has been suggested that obesity might be directly related to the development of asthma through histologic changes in lungs, alterations of hormonal patterns and immune function, or mechanical stress on the respiratory system, such as decreased airway caliber or pulmonary vascular congestion.35-38 Obesity is more prevalent among African American and Latino populations when compared with non-Hispanic whites. According to recent data, almost 50% of US African American women are obese.39 Indirectly, obesity might be associated with a sedentary lifestyle, leading to an increase in exposure to indoor allergens.36 Prospective studies in US populations are consistent in finding an interaction between obesity and asthma risk by sex but do not agree on whether the risk is higher in female or male subjects.32,33,35 As a modifiable risk factor, the role of obesity in asthma incidence warrants exploration and might provide further insight into racial-ethnic disparities. To date, no studies of racial differences in the relationship of obesity to asthma have been conducted.
Low birth weight is more prevalent among African Americans and is also a risk factor for asthma. Results of 2 different analyses found that low birth weight accounted for 30% to 68% of the racial differences in asthma observed in the populations studied.40,41
Residential segregation has the potential to shape socioeconomic conditions that can influence the risk of asthma development, including community-level and individual-level exposures.42-44 Outdoor pollution has not been associated consistently with incident asthma, although it has been associated with increased symptoms among prevalent cases and is more often a problem in areas where people of less means reside.45 The built environment, defined as the physical environment humans have constructed,46 might also have an effect. For example, if one’s surrounding provides little opportunity for physical activity, this might in turn result in increased obesity and an increased incidence of asthma. Children from poor areas have been shown to spend less time outdoors because of a lack of playgrounds and recreational programs and concerns about safety.47
Individual-level exposures have been investigated in urban and nonurban settings. For example, in some studies early exposure to pets or some related factor have been found to be protective for the development of persistent allergic sensitization or asthma.48-50 Pet keeping, however, has been found to be less common among African Americans.51 Cockroach exposure has been associated with an increased risk for incident disease, with cockroaches found to a higher degree in urban areas compared with suburban areas, as are rodents.52
SECONDARY PREVENTION: EARLY DETECTION AND REDUCTION OF MORBIDITY
Early detection
Presumably, early detection of asthma symptoms will facilitate treatment and curb disease progression. Screening programs identifying children with asthma symptoms but no formal diagnosis (“undiagnosed asthma”) might provide an opportunity for treatment and a reduction in morbidity. In a population-based study of more than 122,000 schoolchildren, factors independently related to undiagnosed frequent wheeze included African American race or Hispanic ethnicity (25% to 35% increase in risk) and low SES (50% increased risk) but not urban residence (odds ratio, 0.91; 95% CI, 0.89–0.96).53 Children with undiagnosed frequent wheeze reported less health care and lower self-rated health status. In contrast, a recent study using data from the 1999 National Health Interview Survey found that after adjusting for disease severity, minority children were actually more likely to be given diagnoses than non-Hispanic whites.54 Regardless of race, the prevalence of undiagnosed asthma is not easily compared across studies because estimates in the literature range from 5.3% to 20% depending on the symptoms, criteria, or both used.55-57
Do those without a diagnosis benefit from treatment? A positive-intervention effect was reported in phase II of the National Cooperative Inner-City Asthma Study, which involved a randomized trial to evaluate the effectiveness of an asthma counselor in reducing asthma-related morbidity among children with and without diagnoses.58 In another randomized trial of Open Airways, an asthma management program for school-aged children, subanalyses showed that children with undiagnosed asthma also benefited from treatment when compared with control subjects.59 A caveat in interpreting the results of these studies is the lack of information on persons categorized as having undiagnosed asthma. For example, in one study 8.4% of those without a diagnosis reported being prescribed asthma medications for symptoms.59 In light of evidence that treatment delays might prevent improvements in quality of life and other health outcomes, such as missed work or school, further exploration of early detection as a means of reducing asthma morbidity in minorities is warranted, accompanied by consistent definitions and phenotypic classifications of asthma for use in epidemiologic studies.
Culture, attitudes, and beliefs
Establishing or maintaining optimal functioning in persons with physician-diagnosed asthma requires that health care providers understand how culture, attitudes, and beliefs influence disease management. Mistrust of the medical care system is still voiced by African Americans.60,61 Among Latino communities, variations in family structure (eg, extended families), as well as health beliefs and coping mechanisms, are likely to influence disease management.62,63 The same is true for other minority groups. In a study of 310 Hispanic and African American parents of children with asthma, 89% of the parents had treated their child in the past year with some form of complementary or alternative medicine, most without telling the child’s physician.64 Of these, 59% believed the alternative therapy was at least as effective as pharmacologic therapy, and many used the alternative therapy first for acute attacks. Ford et al65 found that compared with whites, African Americans had lower scores in asthma knowledge but were less likely to believe asthma was best managed by a health care professional. Apter et al66 found that attitudes toward inhaled corticosteroids, such as fear of adverse effects and doubts in the benefit of these drugs, although significantly higher for African Americans compared with whites, did not entirely explain the relationship between race and adherence in multivariate models. These findings illustrate cultural differences toward standard medical care and emphasize the need for a better understanding of factors that influence its use.
Language barriers, in addition to cultural barriers, can undermine quality asthma care. Chan et al67 reported that deficiencies in asthma management skills and knowledge about asthma were associated with a Spanish-speaking home.43,44,59 These limitations were related to a higher frequency of adverse outcomes among children from Spanish-speaking families relative to English-speaking Latino, African American, and non-Hispanic white families. Language barriers might contribute to disparities in asthma morbidity through direct hampering of communication, collaboration, and education.
The residential environment also plays a key role in observed disparities in asthma morbidity related to environmental management.43,44 Crowding and substandard housing translate into an inability to regulate indoor temperature and humidity and increased exposure to indoor and outdoor allergens and irritants. Moreover, prolonged exposure to allergens might in turn prevent adequate asthma control.68-70 Other environmental exposures, such as tobacco smoke, have been associated with ED visits for asthma and with school absenteeism in children with asthma.71-73 In 2 studies of urban children with asthma, the prevalence of smoking among caregivers in the home was approximately 60%.56 However, interventions must take into account that tobacco is a coping strategy for individuals dealing with the stress and deprivation of economically disadvantaged settings and perhaps from the added stress of caring for a family member with asthma.74
Obesity
Because obesity is more prevalent among African American and Latino populations when compared with whites, reducing differences in adiposity might mitigate racial disparities in asthma control. Obesity has been associated with severity and persistence of symptoms from childhood into adolescence.32 National Cooperative Inner-City Asthma Study findings suggest that clinical management of asthma might be more difficult in urban obese children.75 Randomized trials of weight reduction and exercise in persons with asthma suggest these measures can improve asthma control, and although sample sizes are small, results are fairly consistent.76,77
Stress and violence
Stress is higher among residents of economically disadvantaged neighborhoods.78 Parental stress was found to be a significant predictor of infant wheeze in a prospective study of infants with a family history of asthma, allergy, or both.79 In support of this concept, experiences of racial discrimination are significant predictors of preterm and low-birth-weight deliveries and other adverse health outcomes.80 Stress can be linked to asthma exacerbations through several pathways, including the upregulation of mediators of the allergic response.42 Research on the association of chronic exposure to violence and asthma morbidity is emerging. Using data from the Inner-City Asthma Study, Wright et al81 found a significant gradient increase in symptomatology with increasing exposure to violence after adjusting for SES and negative life events.
Access and health care delivery
Disparities in access to and receipt of quality asthma care are well documented. These include but are not limited to less prescribing of inhaled corticosteroids, less follow-up of acute exacerbations, and less availability of pharmacy resources in urban communities.82 The importance of health care coverage should also be underscored. In New Jersey, extension of a safety-net program to poor families who did not qualify for Medicaid resulted in significant increases in asthma diagnosis and treatment in a predominantly Latino community.73 Access to health care does not always explain these trends because disparities in care have also been documented among insured individuals.83,84
TERTIARY PREVENTION: MITIGATING DISEASE COMPLICATIONS
Whether differences by race-ethnicity reflect different phenotypes as opposed to variations in disease incidence, prevalence, or severity is not clear. Putative markers of severity (eg, ED use) might also be influenced by culture, access, and behavior, such that distinguishing use patterns from actual disease severity can be difficult. There is general consensus in the literature that severe asthma, as indicated by frequency of hospitalization or by the rate of asthma deaths, is higher among minorities. A study from Charleston, South Carolina, showed that over the interval from 1956 through 1997, African Americans experienced a 20-fold increase in the rate of hospital discharge for asthma compared with a 5-fold increase for whites.85 In another large multicenter study of ED visits by adults, asthma management did not vary by race in the ED; however, blacks and Hispanics were twice as likely to be hospitalized for their asthma episode and to experience symptoms 2 weeks after hospital discharge.86 These findings suggest either that the asthma episodes are more severe in African Americans and Hispanics by the time they arrive in the ED or that their asthma is less responsive to treatment. McConnochie et al87 studied all asthma hospitalizations in Rochester, New York, occurring in a 5-year period. Asthma hospitalization rates were 5.21 per 1000 (95% CI, 4.83–5.58) and 1.05 per 1000 (95% CI, 0.98–1.13) for “inner-city” versus suburban areas, respectively. Asthma severity was determined by arterial oxygen saturation, nebulized treatment frequency, and length of stay. Results indicated a higher incidence of hospitalization for severe acute asthma among inner-city residents compared with residents from other areas. The authors concluded that higher hospitalization rates in these areas signaled a greater morbidity burden, as opposed to excess use.
Recent studies on racial and ethnic variations in response to asthma medication underscore the importance of extricating disease management from disease severity in asthma. Results of the National Jewish Medical and Research Center study suggested that African American patients with asthma have a diminished response to glucocorticoids, as determined by the amount of dexamethesone needed to suppress in vitro T-lymphocyte activation.88 Also relevant are the results of Choudhry et al,31 discussed earlier, regarding a differential response to bron-chodilators between Puerto Ricans and Mexicans. Clearly, more research in this area is needed, but results suggest that racial and ethnic differences in response to medication must be considered, along with management, behavior, and access, as a potential contributor to disparities in asthma severity.
SUMMARY
Concepts of disease prevention can be applied to the elimination of racial-ethnic disparities in asthma. Asthma primary prevention will require continued advances in research on factors related to incidence, the ability to disentangle effects caused by race-ethnicity from those caused by SES and related factors, and the ability to perform successful interventions. Although genetic differences might be important in learning more about the natural history of asthma, the potential for modification is low. A possible exception is the tailoring of treatment regimens on the basis of the patient’s predisposition to respond to therapy.
Disease management would seem an area most amenable to changes that could reduce asthma morbidity in US minorities and ultimately mitigate disparities. Recent reports of continued discrimination, unequal treatment, and poor access for many poor and minority US citizens, despite major advances in science and medicine, demand a renewed focus. Understanding the biologic and social concepts driving disparities is central to their elimination.
Abbreviations used
- ED
Emergency department
- SES
Socioeconomic status
References
- 1.Centers for Disease Control and Prevention (CDC) Asthma prevalence and control characteristics by race/ethnicity—United States, 2002. MMWR Morb Mortal Wkly Rep. 2004;53:145–8. [PubMed] [Google Scholar]
- 2.Hartert TV. Epidemiology of asthma: the year in review. Curr Opin Pulm Med. 2000;6:4–9. doi: 10.1097/00063198-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–30. doi: 10.2105/ajph.90.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant EN, Lyttle CS, Weiss KB. The relation of socioeconomic factors and racial/ethnic differences in US asthma mortality. Am J Public Health. 2000;90:1923–5. doi: 10.2105/ajph.90.12.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joseph CL, Havstad S, Ownby DR, Peterson EL, Maliarik M, McCabe MJ, Jr, et al. Blood lead level and risk of asthma. Environ Health Perspect. 2005;113:900–4. doi: 10.1289/ehp.7453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14. [DOI] [PubMed] [Google Scholar]
- 7.Osborne NG, Feit MD. The use of race in medical research. JAMA. 1992;267:275–9. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. National Center for Health Statistics, Health E-Stats. Hyattsville (MD): U.S. Department of Health and Human Services, National Center for Health Statistics; [Accessed September 2005.]. Available at: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/asthma/asthma.htm. [Google Scholar]
- 9.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990–1995. Am J Respir Crit Care Med. 2000;161:504–9. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 10.Chen JT, Krieger N, Van Den Eeden SK, Quesenberry CP. Different slopes for different folks: socioeconomic and racial/ethnic disparities in asthma and hay fever among 173,859 U.S. men and women. Environ Health Perspect. 2002;110(suppl 2):211–6. doi: 10.1289/ehp.02110s2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Litonjua AA, Celedon JC, Hausmann J, Nikolov M, Sredl D, Ryan L, et al. Variation in total and specific IgE: effects of ethnicity and socioeconomic status. J Allergy Clin Immunol. 2005;115:751–7. doi: 10.1016/j.jaci.2004.12.1138. [DOI] [PubMed] [Google Scholar]
- 12.Halonen M, Stern D, Lyle S, Wright A, Taussig L, Martinez FD. Relationship of total serum IgE levels in cord and 9-month sera of infants. Clin Exp Allergy. 1991;21:235–41. doi: 10.1111/j.1365-2222.1991.tb00836.x. [DOI] [PubMed] [Google Scholar]
- 13.Johnson CC, Maliarik M, McCabe MJ, Jr, Peterson E, Wegienka G, Smolarek LK, et al. Cord blood stimulated T-cell interferon γ production varies by race in a birth cohort. J Allergy Clin Immunol. 2005;115:S229. [Google Scholar]
- 14.Joseph CL, Ownby DR, Peterson EL, Johnson CC. Racial differences in physiologic parameters related to asthma among middle-class children. Chest. 2000;117:1336–44. doi: 10.1378/chest.117.5.1336. [DOI] [PubMed] [Google Scholar]
- 15.Burchard EG, Avila PC, Nazario S, Casal J, Torres A, Rodriguez-Santana JR, et al. Lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma. Am J Respir Crit Care Med. 2004;169:386–92. doi: 10.1164/rccm.200309-1293OC. [DOI] [PubMed] [Google Scholar]
- 16.Celedon JC, Sredl D, Weiss ST, Pisarski M, Wakefield D, Cloutier M. Ethnicity and skin test reactivity to aeroallergens among asthmatic children in Connecticut. Chest. 2004;125:85–92. doi: 10.1378/chest.125.1.85. [DOI] [PubMed] [Google Scholar]
- 17.Gelber LE, Seltzer LH, Bouzoukis JK, Pollart SM, Chapman MD, Platts-Mills TA. Sensitization and exposure to indoor allergens as risk factors for asthma among patients presenting to hospital. Am Rev Respir Dis. 1993;147:573–8. doi: 10.1164/ajrccm/147.3.573. [DOI] [PubMed] [Google Scholar]
- 18.Ponsonby AL, Gatenby P, Glasgow N, Mullins R, McDonald T, Hurwitz M. Which clinical subgroups within the spectrum of child asthma are attributable to atopy? Chest. 2002;121:135–42. doi: 10.1378/chest.121.1.135. [DOI] [PubMed] [Google Scholar]
- 19.Silverman ES, Palmer LJ, Subramaniam V, Hallock A, Mathew S, Vallone J, et al. Transforming growth factor-{beta}1 promoter polymorphism C-509T is associated with asthma. Am J Respir Crit Care Med. 2004;169:214–9. doi: 10.1164/rccm.200307-973OC. [DOI] [PubMed] [Google Scholar]
- 20.Eder W, Klimecki W, Yu L, von ME, Riedler J, Braun-Fahrlander C, et al. Toll-like receptor 2 as a major gene for asthma in children of European farmers. J Allergy Clin Immunol. 2004;113:482–8. doi: 10.1016/j.jaci.2003.12.374. [DOI] [PubMed] [Google Scholar]
- 21.Zambelli-Weiner A, Ehrlich E, Stockton ML, Grant AV, Zhang S, Levett PN, et al. Evaluation of the CD14/-260 polymorphism and house dust endotoxin exposure in the Barbados Asthma Genetics Study. J Allergy Clin Immunol. 2005;115:1203–9. doi: 10.1016/j.jaci.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Lim S, Crawley E, Woo P, Barnes PJ. Haplotype associated with low interleukin-10 production in patients with severe asthma. Lancet. 1998;352:113. doi: 10.1016/S0140-6736(98)85018-6. [DOI] [PubMed] [Google Scholar]
- 23.Burchard EG, Silverman EK, Rosenwasser LJ, Borish L, Yandava C, Pillari A, et al. Association between a sequence variant in the IL-4 gene promoter and FEV(1) in asthma. Am J Respir Crit Care Med. 1999;160:919–22. doi: 10.1164/ajrccm.160.3.9812024. [DOI] [PubMed] [Google Scholar]
- 24.Israel E, Drazen JM, Liggett SB, Boushey HA, Cherniack RM, Chinchilli VM, et al. The effect of polymorphisms of the beta(2)-adrenergic receptor on the response to regular use of albuterol in asthma. Am J Respir Crit Care Med. 2000;162:75–80. doi: 10.1164/ajrccm.162.1.9907092. [DOI] [PubMed] [Google Scholar]
- 25.Ness RB, Haggerty CL, Harger G, Ferrell R. Differential distribution of allelic variants in cytokine genes among African Americans and White Americans. Am J Epidemiol. 2004;160:1033–8. doi: 10.1093/aje/kwh325. [DOI] [PubMed] [Google Scholar]
- 26.Choudhry S, Avila PC, Nazario S, Ung N, Kho J, Rodriguez-Santana JR, et al. CD14 tobacco gene-environment interaction modifies asthma severity and immunoglobulin E levels in Latinos with asthma. Am J Respir Crit Care Med. 2005;172:173–82. doi: 10.1164/rccm.200409-1232OC. [DOI] [PubMed] [Google Scholar]
- 27.Lazarus R, Vercelli D, Palmer LJ, Klimecki WJ, Silverman EK, Richter B, et al. Single nucleotide polymorphisms in innate immunity genes: abundant variation and potential role in complex human disease. Immunol Rev. 2002;190:9–25. doi: 10.1034/j.1600-065x.2002.19002.x. [DOI] [PubMed] [Google Scholar]
- 28.Burchard EG, Ziv E, Coyle N, Gomez SL, Tang H, Karter AJ, et al. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348:1170–5. doi: 10.1056/NEJMsb025007. [DOI] [PubMed] [Google Scholar]
- 29.Cooper RS, Kaufman JS, Ward R. Race and genomics. N Engl J Med. 2003;348:1166–70. doi: 10.1056/NEJMsb022863. [DOI] [PubMed] [Google Scholar]
- 30.Bamshad M. Genetic influences on health: does race matter? JAMA. 2005;294:937–46. doi: 10.1001/jama.294.8.937. [DOI] [PubMed] [Google Scholar]
- 31.Choudhry S, Ung N, Avila PC, Ziv E, Nazario S, Casal J, et al. Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med. 2005;171:563–70. doi: 10.1164/rccm.200409-1286OC. [DOI] [PubMed] [Google Scholar]
- 32.Castro-Rodriguez JA, Holberg CJ, Morgan WJ, Wright AL, Martinez FD. Increased incidence of asthmalike symptoms in girls who become overweight or obese during the school years. Am J Respir Crit Care Med. 2001;163:1344–9. doi: 10.1164/ajrccm.163.6.2006140. [DOI] [PubMed] [Google Scholar]
- 33.Gilliland FD, Berhane K, Islam T, McConnell R, Gauderman WJ, Gilliland SS, et al. Obesity and the risk of newly diagnosed asthma in school-age children. Am J Epidemiol. 2003;158:406–15. doi: 10.1093/aje/kwg175. [DOI] [PubMed] [Google Scholar]
- 34.Milner JD, Stein DM, McCarter R, Moon RY. Early infant multivitamin supplementation is associated with increased risk for food allergy and asthma. Pediatrics. 2004;114:27–32. doi: 10.1542/peds.114.1.27. [DOI] [PubMed] [Google Scholar]
- 35.Beckett WS, Jacobs DR, Jr, Yu X, Iribarren C, Williams OD. Asthma is associated with weight gain in females but not males, independent of physical activity. Am J Respir Crit Care Med. 2001;164:2045–50. doi: 10.1164/ajrccm.164.11.2004235. [DOI] [PubMed] [Google Scholar]
- 36.Nieman DC, Henson DA, Nehlsen-Cannarella SL, Ekkens M, Utter AC, Butterworth DE, et al. Influence of obesity on immune function. J Am Diet Assoc. 1999;99:294–9. doi: 10.1016/S0002-8223(99)00077-2. [DOI] [PubMed] [Google Scholar]
- 37.Litonjua AA, Sparrow D, Celedon JC, DeMolles D, Weiss ST. Association of body mass index with the development of methacholine airway hyperresponsiveness in men: the Normative Aging Study. Thorax. 2002;57:581–5. doi: 10.1136/thorax.57.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sood A. Does obesity weigh heavily on the health of the human airway? [published erratum appears in J Allergy Clin Immunol. 2005;116:55] J Allergy Clin Immunol. 2005;115:921–4. doi: 10.1016/j.jaci.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 39.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 40.Joseph CL, Ownby DR, Peterson EL, Johnson CC. Does low birth weight help to explain the increased prevalence of asthma among African-Americans? Ann Allergy Asthma Immunol. 2002;88:507–12. doi: 10.1016/S1081-1206(10)62390-3. [DOI] [PubMed] [Google Scholar]
- 41.Brooks AM, Byrd RS, Weitzman M, Auinger P, McBride JT. Impact of low birth weight on early childhood asthma in the United States. Arch Pediatr Adolesc Med. 2001;155:401–6. doi: 10.1001/archpedi.155.3.401. [DOI] [PubMed] [Google Scholar]
- 42.Wright RJ, Steinbach SF. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ Health Perspect. 2001;109:1085–9. doi: 10.1289/ehp.011091085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brown P, Mayer B, Zavestoski S, Luebke T, Mandelbaum J, McCormick S. The health politics of asthma: environmental justice and collective illness experience in the United States. Soc Sci Med. 2003;57:453–64. doi: 10.1016/s0277-9536(02)00375-1. [DOI] [PubMed] [Google Scholar]
- 45.Lwebuga-Mukasa JS, Wojcik R, Dunn-Georgiou E, Johnson C. Home environmental factors associated with asthma prevalence in two Buffalo inner-city neighborhoods. J Health Care Poor Underserved. 2002;13:214–28. doi: 10.1353/hpu.2010.0519. [DOI] [PubMed] [Google Scholar]
- 46.Brisbon N, Plumb J, Brawer R, Paxman D. The asthma and obesity epidemics: the role played by the built environment—a public health perspective. J Allergy Clin Immunol. 2005;115:1024–8. doi: 10.1016/j.jaci.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (CDC) Neighborhood safety and the prevalence of physical inactivity—selected states, 1996. MMWR Morb Mortal Wkly Rep. 1999;48:143–6. [PubMed] [Google Scholar]
- 48.Ownby DR, Johnson CC, Peterson EL. Exposure to dogs and cats in the first year of life and risk of allergic sensitization at 6 to 7 years of age. JAMA. 2002;288:963–72. doi: 10.1001/jama.288.8.963. [DOI] [PubMed] [Google Scholar]
- 49.Remes ST, Castro-Rodriguez JA, Holberg CJ, Martinez FD, Wright AL. Dog exposure in infancy decreases the subsequent risk of frequent wheeze but not atopy. J Allergy Clin Immunol. 2001;108:509–15. doi: 10.1067/mai.2001.117797. [DOI] [PubMed] [Google Scholar]
- 50.Nafstad P, Magnus P, Gaarder PI, Jaakkola JJK. Exposure to pets and atopy-related diseases in the first 4 years of life. Allergy. 2001;56:307–12. doi: 10.1034/j.1398-9995.2001.00881.x. [DOI] [PubMed] [Google Scholar]
- 51.Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, et al. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109:857–65. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 52.Litonjua AA, Carey VJ, Burge HA, Weiss ST, Gold DR. Exposure to cockroach allergen in the home is associated with incident doctor-diagnosed asthma and recurrent wheezing. J Allergy Clin Immunol. 2001;107:41–7. doi: 10.1067/mai.2001.111143. [DOI] [PubMed] [Google Scholar]
- 53.Yeatts K, Davis KJ, Sotir M, Herget C, Shy C. Who gets diagnosed with asthma? Frequent wheeze among adolescents with and without a diagnosis of asthma. Pediatrics. 2003;111:1046–54. doi: 10.1542/peds.111.5.1046. [DOI] [PubMed] [Google Scholar]
- 54.Akinbami LJ, Rhodes JC, Lara M. Racial and ethnic differences in asthma diagnosis among children who wheeze. Pediatrics. 2005;115:1254–60. doi: 10.1542/peds.2004-0897. [DOI] [PubMed] [Google Scholar]
- 55.Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein RE. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics. 1994;94:356–62. [PubMed] [Google Scholar]
- 56.Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio M, et al. Issues in identifying asthma and estimating prevalence in an urban school population. J Clin Epidemiol. 2002;55:870–81. doi: 10.1016/s0895-4356(02)00451-1. [DOI] [PubMed] [Google Scholar]
- 57.Yawn BP, Wollan P, Scanlon PD, Kurland M. Outcome results of a school-based screening program for undertreated asthma. Ann Allergy Asthma Immunol. 2003;90:508–15. doi: 10.1016/S1081-1206(10)61844-3. [DOI] [PubMed] [Google Scholar]
- 58.Evans R, III, Gergen PJ, Mitchell H, Kattan M, Kercsmar C, Crain E, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr. 1999;135:332–8. doi: 10.1016/s0022-3476(99)70130-7. [DOI] [PubMed] [Google Scholar]
- 59.Joseph CL, Havstad S, Anderson EW, Brown R, Johnson CC, Clark NM. Effect of asthma intervention on children with undiagnosed asthma. J Pediatr. 2005;146:96–104. doi: 10.1016/j.jpeds.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 60.George M, Freedman TG, Norfleet AL, Feldman HI, Apter AJ. Qualitative research-enhanced understanding of patients’ beliefs: results of focus groups with low-income, urban, African American adults with asthma. J Allergy Clin Immunol. 2003;111:967–73. doi: 10.1067/mai.2003.1459. [DOI] [PubMed] [Google Scholar]
- 61.Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97:951–6. [PMC free article] [PubMed] [Google Scholar]
- 62.Lara M, Morgenstern H, Duan N, Brook RH. Elevated asthma morbidity in Puerto Rican children: a review of possible risk and prognostic factors. West J Med. 1999;170:75–84. [PMC free article] [PubMed] [Google Scholar]
- 63.Pachter LM, Cloutier MM, Bernstein BA. Ethnomedical (folk) remedies for childhood asthma in a mainland Puerto Rican community. Arch Pediatr Adolesc Med. 1995;149:982–8. doi: 10.1001/archpedi.1995.02170220048007. [DOI] [PubMed] [Google Scholar]
- 64.Braganza S, Ozuah PO, Sharif I. The use of complementary therapies in inner-city asthmatic children. J Asthma. 2003;40:823–7. doi: 10.1081/jas-120023574. [DOI] [PubMed] [Google Scholar]
- 65.Ford ME, Havstad SL, Tilley BC, Bolton MB. Health outcomes among African American and Caucasian adults following a randomized trial of an asthma education program. Ethn Health. 1997;2:329–39. doi: 10.1080/13557858.1997.9961842. [DOI] [PubMed] [Google Scholar]
- 66.Apter AJ, Boston RC, George M, Norfleet AL, Tenhave T, Coyne JC, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it’s not just black and white. J Allergy Clin Immunol. 2003;111:1219–26. doi: 10.1067/mai.2003.1479. [DOI] [PubMed] [Google Scholar]
- 67.Chan KS, Keeler E, Schonlau M, Rosen M, Mangione-Smith R. How do ethnicity and primary language spoken at home affect management practices and outcomes in children and adolescents with asthma? Arch Pediatr Adolesc Med. 2005;159:283–9. doi: 10.1001/archpedi.159.3.283. [DOI] [PubMed] [Google Scholar]
- 68.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336:1356–63. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 69.Leaderer BP, Belanger K, Triche E, Holford T, Gold DR, Kim Y, et al. Dust mite, cockroach, cat, and dog allergen concentrations in homes of asthmatic children in the northeastern United States: impact of socioeconomic factors and population density. Environ Health Perspect. 2002;110:419–25. doi: 10.1289/ehp.02110419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Findley S, Lawler K, Bindra M, Maggio L, Penachio MM, Maylahn C. Elevated asthma and indoor environmental exposures among Puerto Rican children of East Harlem. J Asthma. 2003;40:557–69. doi: 10.1081/jas-120019028. [DOI] [PubMed] [Google Scholar]
- 71.Huss K, Rand CS, Butz AM, Eggleston PA, Murigande C, Thompson LC, et al. Home environmental risk factors in urban minority asthmatic children. Ann Allergy. 1994;72:173–7. [PubMed] [Google Scholar]
- 72.Freeman NC, Schneider D, McGarvey P. Household exposure factors, asthma, and school absenteeism in a predominantly Hispanic community. J Expo Anal Environ Epidemiol. 2003;13:169–76. doi: 10.1038/sj.jea.7500266. [DOI] [PubMed] [Google Scholar]
- 73.Freeman NC, Schneider D, McGarvey P. The relationship of health insurance to the diagnosis and management of asthma and respiratory problems in children in a predominantly Hispanic urban community. Am J Public Health. 2003;93:1316–20. doi: 10.2105/ajph.93.8.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Flint AJ, Novotny TE. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983–1993: the independent risk of being poor. Tob Control. 1997;6:14–8. doi: 10.1136/tc.6.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Belamarich PF, Luder E, Kattan M, Mitchell H, Islam S, Lynn H, et al. Do obese inner-city children with asthma have more symptoms than nonobese children with asthma? Pediatrics. 2000;106:1436–41. doi: 10.1542/peds.106.6.1436. [DOI] [PubMed] [Google Scholar]
- 76.Lucas SR, Platts-Mills TA. Physical activity and exercise in asthma: relevance to etiology and treatment. J Allergy Clin Immunol. 2005;115:928–34. doi: 10.1016/j.jaci.2005.01.033. [DOI] [PubMed] [Google Scholar]
- 77.Ford ES. The epidemiology of obesity and asthma. J Allergy Clin Immunol. 2005;115:897–909. doi: 10.1016/j.jaci.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 78.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75:3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- 79.Wright RJ, Cohen S, Carey V, Weiss ST, Gold DR. Parental stress as a predictor of wheezing in infancy: a prospective birth-cohort study. Am J Respir Crit Care Med. 2002;165:358–65. doi: 10.1164/ajrccm.165.3.2102016. [DOI] [PubMed] [Google Scholar]
- 80.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. Am J Public Health. 2004;94:2125–31. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94:625–32. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Warman KL, Jacobs AM, Silver EJ. If we prescribe it, will it come? Access to asthma equipment for Medicaid-insured children and adults in the Bronx, NY. Arch Pediatr Adolesc Med. 2002;156:673–7. doi: 10.1001/archpedi.156.7.673. [DOI] [PubMed] [Google Scholar]
- 83.Zoratti EM, Havstad S, Rodriguez J, Robens-Paradise Y, Lafata JE, McCarthy B. Health service use by African Americans and Caucasians with asthma in a managed care setting. Am J Respir Crit Care Med. 1998;158:371–7. doi: 10.1164/ajrccm.158.2.9608039. [DOI] [PubMed] [Google Scholar]
- 84.Lozano P, Connell FA, Koepsell TD. Use of health services by African-American children with asthma on Medicaid. JAMA. 1995;274:469–73. [PubMed] [Google Scholar]
- 85.Crater DD, Heise S, Perzanowski M, Herbert R, Morse CG, Hulsey TC, et al. asthma hospitalization trends in Charleston, South Carolina, 1956 to 1997: twenty-fold increase among black children during a 30-year period. Pediatrics. 2001;108:e97. doi: 10.1542/peds.108.6.e97. [DOI] [PubMed] [Google Scholar]
- 86.Boudreaux ED, Emond SD, Clark S, Camargo CA., Jr Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status. Chest. 2003;124:803–12. doi: 10.1378/chest.124.3.803. [DOI] [PubMed] [Google Scholar]
- 87.McConnochie KM, Russo MJ, McBride JT, Szilagyi PG, Brooks AM, Roghmann KJ. Socioeconomic variation in asthma hospitalization: excess utilization or greater need? Pediatrics. 1999;103:e75. doi: 10.1542/peds.103.6.e75. [DOI] [PubMed] [Google Scholar]
- 88.Federico MJ, Covar RA, Brown EE, Leung DYM, Spahn JD. Racial differences in T-lymphocyte response to glucocorticoids. Chest. 2005;127:571–8. doi: 10.1378/chest.127.2.571. [DOI] [PubMed] [Google Scholar]


