Abstract
Plasmid DNA expressing the major outer membrane protein (MOMP) of an avian Chlamydia psittaci serovar A strain has been tested for its ability to raise an immune response and induce protection against challenge with the same serovar. A combined parenteral (intramuscular injection) and mucosal route (DNA drops administered to the nares) of DNA inoculation was compared with gene gun-based immunization. The gene gun delivery of pcDNA1/MOMP as well as the intramuscular–intranasal DNA delivery primed both T-helper and B cell memory, although rMOMP-expressing cells did not induce high antibody responses. Evidence for the priming of the memory was provided by the fact that the pcDNA1/MOMP inoculations raised antibodies belonging to the IgG and not IgM isotype. However, in response to challenge only five out of 15 vaccinated turkeys showed four-fold increases in serum IgG after challenge. By contrast, evidence for the priming of T cell memory in response to challenge was found in all vaccinated turkeys, as shown by the significantly heightened proliferative responses of peripheral blood lymphocytes following vaccination. Both immunization methods produced similar serological and lymphocyte proliferative responses. Notwithstanding the immunization method, a significant level of protection was observed in all pcDNA1/MOMP-immunized turkeys. The efficacy of MOMP-based DNA vaccination as a means of preventing severe clinical signs, lesions and chlamydia excretion in a turkey model of C. psittaci infection was demonstrated.
Keywords: chlamydia, vaccination, turkeys
INTRODUCTION
Chlamydia psittaci, a Gram-negative obligate intracellular bacterium, is an important turkey pathogen causing infections of mucosal epithelial cells and macrophages of the respiratory tract, followed by septicaemia and localization in epithelial cells and macrophages in various organs [1]. Chlamydial infections in turkeys present significant economical losses, but public health is also a consideration, since veterinary surgeons and poultry workers are at risk of becoming infected by this zoonotic agent. Chlamydia vaccines are non-existent, although considerable efforts have been made [2–7].
The important host defence mechanisms against Chlamydia remain incompletely defined. An ongoing controversy is the relative contribution of humoral versus cell-mediated immunity in the host resistance against chlamydiae. The potential effectors of anti-chlamydial T cell-mediated immunity are the CD4+ T helper type 1 (Thl), CD8+ T cells, mononuclear phagocytes and cytokines secreted by these cells [8–14].
Regarding the probable role of CD8+ T cells in conjunction with CD4+ Th1 cells, gene vaccination or the use of antigen encoding DNAs to vaccinate offers a new exciting method to develop chlamydia subunit vaccines. Gene vaccination provides a stable and long-lived source of immunogenic protein (reviewed in [15,16]). Unlike conventional vaccines, DNA vaccination leads to antigen processing and loading onto both MHC class I and II molecules, and in this respect might resemble more closely a natural chlamydia infection. This leads to an immune response characterized by the generation of MHC class I-restricted cytotoxic T cells, as well as helper T cells of the Th1 phenotype secreting predominantly interferon-gamma (IFN-γ). The type of response that is induced may be determined by non-coding immunostimulatory sequences (ISS) within the plasmid backbone, which are centred around unmethylated CpG base pairs. These motifs rapidly stimulate the innate immune system, leading to production of IFN-γ by natural killer (NK) cells and IFN-α and IFN-β, IL-12 and IL-18 by macrophages. Moreover, bacterial DNA, through its mitogenic effect on B cells and synergistic effect with antigen receptor cross-linking, could lead to the early production of low-affinity opsonizing antibodies. Furthermore, the cytokine milieu that is generated by the bacterial DNA favours the differentiation of naive Th cells to the Th1 phenotype on encounter with antigen. Secretion of IFN-γ by Th1 cells then favours immunoglobulin class switching to the IgG2a isotype and activation of cytotoxic T lymphocytes.
The only protective chlamydial antigen which has been unambiguously identified is the major outer membrane protein (MOMP). This protein, identified independently by two groups in the USA [17,18] and one in the UK [19], represents the majority of the surface exposed proteins of the species C. psittaci. It is a protein of around 40 kD characterized by four variable regions (VS I to IV) and five intervening constant regions of conserved structure and function. MOMP is an immunodominant protein carrying genus-, species- and interestingly serovar-specific epitopes eliciting neutralizing antibodies [20,21]. Chlamydial recombinant MOMP (rMOMP) expressed by plasmid DNA assembles into a native conformation in eukaryotic cells and is localized to the host cell membrane [22]. In the present study, plasmid DNA expressing the C. psittaci serovar A MOMP has been tested for its ability to raise immunity in specific pathogen-free (SPF) turkeys against challenge with the homologous chlamydia strain. The effect of the route of inoculation on DNA vaccination was evaluated in a turkey C. psittaci model.
MATERIALS AND METHODS
Chlamydia psittaci strain
In this study, C. psittaci strain 84/55, isolated from the lungs of a diseased parakeet, was used. The strain was previously characterized using serovar-specific MoAbs and by restriction fragment length analysis of the omp1 gene. Strain 84/55 was classified as an avian serovar A and genotype A strain [23]. The strain was grown in Buffalo Green Monkey (BGM) cells as previously described [24].
Vaccine DNA
Plasmid pcDNA1/MOMP was constructed by sticky-end ligation of the outer membrane protein 1 (omp1) gene of strain 84/55 into the Eco R1 site of pcDNA1. A construct in the correct orientation to express the omp1 gene under the control of the cytomegalovirus immediate early promotor was identified by both restriction endonuclease digestions of plasmid mini-preparations and polymerase chain reaction (PCR) clone analysis using Sp6 and T7 primers. The sequences of the omp1 inserts were determined by the dideoxynucleotide chain termination method using pcDNA1 T7 (5′) and Sp6 (3′) priming sites and thereafter specific 18- and 23-mer oligonucleotides at approximately 300-bp intervals in both the 3′ and 5′ directions. Expression of MOMP was confirmed by indirect immunofluorescent staining of both transiently transfected COS7 cells and turkey skeletal muscle injected with pcDNA1/MOMP [22]. pcDNA1 was used as control plasmid. DNAs were grown in Escherichia coli MC1061/P3 bacteria and purified by use of the Qiagen Tip 2500 plasmid preparation method (Qiagen GmbH, Hilden, Germany). DNA concentration was determined by optical density (OD) at 260 nm and confirmed by comparing intensities of ethidium bromide-stained EcoRI restriction endonuclease fragments with standards of known concentration. DNA was stored at −20°C in 1 mm Tris pH 7.8, 0.1 mm EDTA. For injections DNA was diluted in saline (0.9% NaCl).
Vaccination trial
SPF turkeys (CNEVA, Ploufragan, France) were divided in four groups, each reared in negative pressure isolators on wired floors. Turkeys of group 1 (n = 10) (IM + IN vaccinated group) were immunized by a combined parenteral and mucosal route of DNA inoculation including intramuscular injection and DNA drops administered to the nares. Turkeys of group 2 (n = 5) (gene gun-vaccinated group) were immunized by DNA-coated gold particles (1.0 μm) delivered into the abdominal skin with the Helios Gene Gun System (BioRad, Nazareth, Belgium), which employs a helium pulse as motive force. Group 1 as well as group 2 received two DNA inoculations, one at time 0 and the second 3 weeks later. Turkeys of group 1 received 100 μg of pcDNA1/MOMP in 100 μl of saline per inoculation site, while turkeys of group 2 received 2.0 μg pcDNA1/MOMP precipitated onto gold micro carriers. Chlamydia psittaci serovar A challenge was administered by aerosol at 14 days after the second DNA inoculation. The challenge consisted of 108.5 TCID50 of chlamydia strain 84/55. A control group (group 3) (placebo-vaccinated-challenged group) of six pcDNA1-vaccinated SPF turkeys was similarly infected. A second control group (group 4) (placebo-vaccinated-unchallenged group) of five pcDNA1-vaccinated SPF turkeys remained unchallenged. All control turkeys received pcDNA1 intramuscularly and intranasally.
Samples
All turkeys were observed daily for clinical signs. Nasal and cloacal swabs were taken every other day. Blood samples were collected for the detection of anti-MOMP-specific antibodies immediately prior to each DNA inoculation, immediately prior to the experimental infection and at 8 and 18 days after the challenge infection. Blood samples were stored overnight at room temperature, centrifuged (325 g, 10 min, 4°C) and afterwards serum was collected and frozen at −20°C until tested. At the time of euthanasia, 18 days post-challenge, proliferative responses in peripheral blood lymphocytes were examined. All euthanized turkeys were examined for macroscopic lesions. Cryostat tissue sections of the abdominal and thoracic air sacs, the lungs, pericardium, spleen and liver were examined for the presence of chlamydia antigen.
Chlamydia isolation
Nasal and cloacal swabs were examined for the presence of viable chlamydiae by isolation in BGM cells, as previously described [24].
Direct immunofluorescence staining
Cryostat tissue sections were examined by IMAGEN direct immunofluorescence staining, as previously described (Novo Nordisk Diagnostics, Cambridge, UK) [24]. The number of cells with chlamydial inclusions was counted in five microscopic fields (× 500). The results are presented as a score ranging from − to +++. Score − indicated no antigen present. Score +, ++ and +++ were given when a mean of 1–5, 5–10 and > 10 inclusion-positive cells per field were present, respectively.
Antibody responses
ELISAs were performed on turkey sera being pretreated with kaolin to remove background activity [25]. Anti-MOMP antibody titres and turkey antibody isotypes were determined by two different indirect ELISAs using standard protocols and microwell plates coated with recombinant MOMP (rMOMP). Recombinant MOMP was produced in pcDNA1/MOMP-transfected COS7 cells as described previously [22]. For the determination of antibody titres, 1:4000 and 1:2000 dilutions of biotinylated anti-chicken/turkey IgG (H+L) antibody and peroxidase-conjugated streptavidin, respectively, were used. Anti-MOMP immunoglobulin titres were presented as the reciprocal of the highest serum dilution that gave an optical density (OD405) above the cut-off value. The cut-off value (0.100) was the mean OD of seronegative turkeys ± twice the s.d.
Anti-MOMP isotype-specific antibodies were determined using 1:500 dilutions of cross-reactive anti-chicken IgG- or IgA-specific peroxidase-conjugated polyclonal antibodies (Bethyl Labs, Montgomery, TX) and a 1:1000 dilution of a cross-reactive anti-chicken IgM-specific MoAb (B. Kaspers, Institute for Animal Physiology, University of Munich, Germany). The results for each isotype were presented as the mean OD405 measured at a serum dilution of 1/32 ± the s.d. The cut-off values for the different isotypes were 0.102 (IgM), 0.114 (IgG) and 0.117 (IgA).
Lymphocyte proliferative responses
Peripheral blood leucocytes (PBL) were isolated from heparinized blood samples obtained by venepuncture from each turkey of groups 1–4, at 18 days after challenge. Macrophage-like adherent cells were removed from cell suspensions by treatment of heparinized blood with carbonyl iron powder as described by Sjöberg et al. [26]. Subsequently, turkey PBL were isolated over a Lymphoprep density gradient (Life Technologies) and most remaining macrophages were removed by adherence to plasma-coated polystyrene culture plates. The non-adherent cells were cultured in duplicate in 96-well microtitre plates at 6 × 106 cells in 150 μl of Dulbecco's modified Eagle's medium (DMEM) supplemented with 20% heat-inactivated fetal calf serum (FCS; Integro, Zaandam, The Netherlands), 1% non-essential amino acids (Life Technologies), 1% sodium pyruvate (Life Technologies), 1% l-glutamine (Life Technologies), 1% gentamycin (Life Technologies) and 5 × 10−5 mβ-mercaptoethanol (β-ME; Life Technologies). For antigen-induced proliferation, 10 μg of recombinant MOMP were added to individual wells. Controls included cells stimulated with either medium or 10 μg concanavalin A (Con A). Cells were incubated at 39.5°C in a humidified incubator with 5% CO2. Con A- or antigen-induced proliferation was measured by incorporation of 3H-thymidine (1 μCi/well) during the last 16 h of culture, at days 2 and 8, respectively. Cultures were harvested onto glassfibre filter strips with a cell harvester (Skatron, Lier, Norway). Filters were placed in 2 ml Lumasave LSC cocktail (Lumac, Groningen, The Netherlands) and counted in a Beckman β-scintillation counter (Beckman, Gent, Belgium). The stimulation index (SI) was defined as the ratio of ct/min of stimulated on medium-only cultures.
Statistical analysis
The two-tailed Student's t-test was employed for all statistical analyses. Results were considered significantly different at the level of P < 0.05.
RESULTS
Protection against C. psittaci challenge
Following two inoculations with pcDNA1/MOMP or pcDNA1, SPF turkeys were challenged with a very high experimental infective dose of the homologous chlamydia strain. Severe clinical signs and lesions were only observed in the non-vaccinated challenged control group. Turkeys of this group showed depression, anorexia, conjunctivitis, head shaking, respiratory distress and diarrhoea. At necropsy, conjunctivitis, rhinitis, sinusitis, pneumonia, airsacculitis, pericarditis, hepatosplenomegaly and congestion of the kidneys were observed. In two out of 10 turkeys of the IM+IN vaccinated group, only head shaking was observed while turkeys of the gene gun-vaccinated group showed no clinical signs. However, in all vaccinated turkeys lesions were present in the abdominal air sacs. In the abdominal air sacs one or two small fibrin cloths were unilaterally present. No other lesions were observed in the vaccinated groups.
Results of the cloacal and nasal cultures obtained at 2-daily intervals during 18 days following challenge are shown in Tables 1 and 2, respectively. A significant level of protection was observed in all turkeys immunized with pcDNA1/MOMP. Turkeys immunized by the combined intranasal–intramuscular route seemed equally protected as the intra-epidermal-immunized turkeys. All turkeys of the non-vaccinated challenged control group had a positive cloacal culture during the 18 days of observation, while 93% (14 of 15) of the vaccinated turkeys had no cloacal shedding during these 18 days. All control turkeys as well as all vaccinated turkeys excreted chlamydia nasally. However, the period of shedding was significantly shorter in vaccinated turkeys. At 18 days post-challenge, 66% (four of six) of the control turkeys still excreted chlamydia nasally, while in vaccinated turkeys, nasal excretion was observed no longer than 8 days post-challenge. In addition, at day 6 post-challenge, the control turkeys shed a higher number of infectious chlamydiae than did the pcDNA1/MOMP-immunized groups. All the turkeys in the sham-immunized non-challenged group remained chlamydia-negative throughout the experiment.
Table 1.
Results of nasal cultures
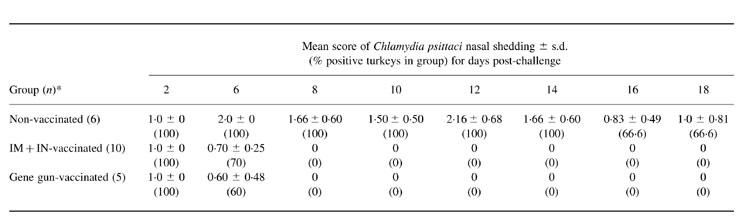
*Number of turkeys per group.
Table 2.
Results of cloacal cultures
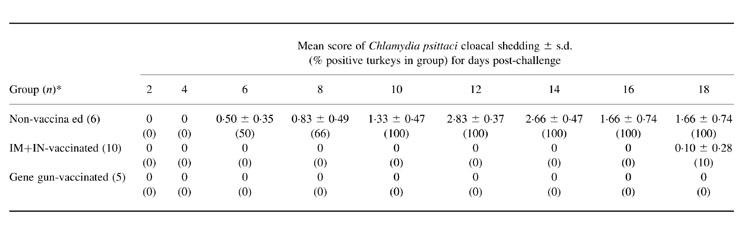
*Number of turkeys per group.
Immunofluorescence staining of tissues of the control turkeys, euthanized 18 days post-challenge, revealed strong chlamydia replication in air sacs, lungs and liver, and weak replication in pericardium and spleen (Table 3). Regarding chlamydia replication, there were no significant differences in protection provided by the combined intramuscular–intranasal or intra-epidermal routes of DNA administration. In these vaccinated challenged animals, only a weak replication was observed in lung tissues of five out of 15 turkeys, in air sacs of all and in pericardium of two out of 15 turkeys.
Table 3.
Chlamydia replication in tissues of turkeys, 18 days post-challenge determined by direct immunofluorescence staining
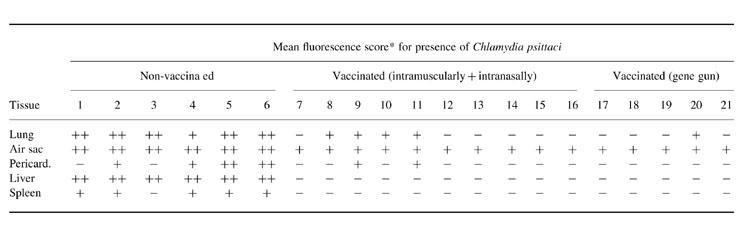
*−, No antigen present; +, an average of 1–5 inclusion-positive cells; ++, an average of 5–10 inclusion-positive cells; +++, an average of > 10 inclusion-positive cells.
Antibody responses
Turkeys were immunized by a combined intramuscular (100 μg)–intranasal (100 μg) route or intra-epidermal (2.0 μg) route using the Helios Gene Gun. Three weeks following the first immunization with pcDNA1/MOMP, anti-MOMP serum antibodies were observed in five out of 10 IM+IN-vaccinated turkeys and in all gene gun-vaccinated turkeys (Table 4). Following the second immunization anti-MOMP antibodies also appeared in the five seronegative IM+IN-vaccinated turkeys. However, the antibody responses as determined in an ELISA with homologous rMOMP were weak. Following challenge, only four out of 10 IM+IN-vaccinated turkeys and one of five gene gun-vaccinated turkeys displayed four-fold increase in antibody titres, indicating the occurrence of a secondary antibody response. In all control turkeys, a primary antibody response was observed after the infection. Protection occurred in all vaccinated turkeys that had detectable anti-MOMP antibody titres before challenge. The best protection occurred in turkeys which had not displayed secondary antibody responses. All non-vaccinated non-infected turkeys showed undetectable anti-MOMP antibody activity in the lowest serum dilution (1:32) used.
Table 4.
Major outer membrane protein (MOMP)-specific antibody titres following DNA vaccination and subsequent challenge with the homologous Chlamydia psittaci strain
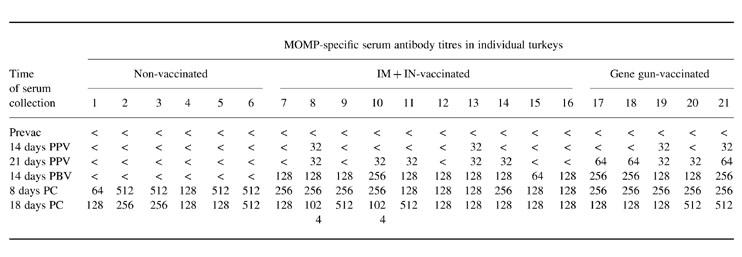
Prevac, Bleed at hatching, before DNA vaccination; PPV, post-primovaccination; PBV, post-booster vaccination; PC, post-challenge; <, no antibodies detected at serum dilution used (1:32).
The isotype-specific ELISAs demonstrated that both immunization methods induced low IgM, IgG and IgA responses (Fig. 1). Indeed, 14 days after the second DNA inoculation, all IM+IN-vaccinated turkeys as well as all gene gun-vaccinated turkeys showed for all isotypes low mean OD values of 0.1–0.2 and 0.2–0.3, respectively, above those of sera of turkeys immunized with the control plasmid. Eighteen days after challenge, these marginal IgM, IgG and IgA levels had increased, with IgG dominating the immune response. However, for both immunization methods, increased levels of IgG were not significantly correlated with higher levels of protection. In non-vaccinated turkeys the IgG and IgA antibody levels following infection were lower in comparison with the levels in post-challenge sera of vaccinated turkeys.
Fig. 1.
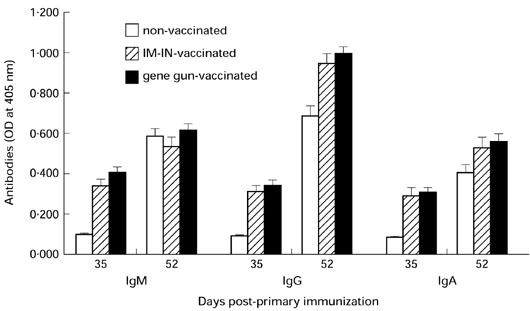
Major outer membrane protein (MOMP)-specific IgG, IgM and IgA antibodies induced by intramuscular–intranasal or intra-epidermal immunization with pcDNA1/MOMP. Each column represents the mean optical density (OD) measured at a serum dilution of 1:32 ± 1 s.d.
Antigen-specific lymphocyte proliferation
Proliferative responses to rMOMP of PBL of pcDNA1/MOMP (group 1 + 2) or pcDNA1-immunized control turkeys were determined 18 days following challenge with the homologous chlamydia strain. The PBL of pcDNA1/MOMP-immunized turkeys displayed significantly higher proliferative responses (Table 5) than the PBL of the controls. In addition, PBL responses in gene gun-immunized turkeys were comparable to the responses in intramuscularly–intranasally-immunized turkeys. The PBL responses of challenged controls were comparable to responses of non-challenged controls.
Table 5.
Proliferative response of peripheral blood lymphocytes of immunized and non-immunized turkeys to recombinant major outer membrane protein (rMOMP) day 18 post-challenge
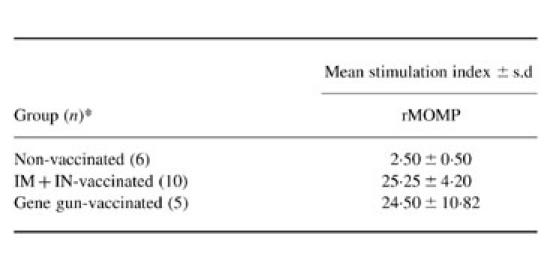
*Number of turkeys per group.
DISCUSSION
In the present study, the eukaryotic expression vector pcDNA1/MOMP, encoding the major outer membrane protein of an avian C. psittaci serovar A strain, was used to assess the potential of DNA-mediated immunization of turkeys against challenge with the homologous chlamydia strain. The chlamydial recombinant MOMP (rMOMP) expressed by pcDNA1/MOMP, assembled into a native conformation in COS7 cells and turkey muscle tissue and was expressed in the cytoplasm and on the host cell membrane [22]. The efficacy of combined intramuscular–intranasal administration of plasmid DNA in saline and of gene gun delivery of plasmid DNA-coated gold particles to the skin was evaluated. The intramuscular–intranasal inoculation method combines unusually efficient transfection in the muscle and a less efficient transfection in the nose. However, the latter tissue is the natural route of entrance for C. psittaci and epithelial cells of the respiratory tract have a high turnover, so that recombinant MOMP is available in high concentration for MHC I and II presentation to CD8+ and CD4+ T cell activation. Gene gun vaccination theoretically reflects efficient biolistic transfection together with efficient antigen presentation by cells of the bird's skin-associated lymphoid tissue.
In the present study, pcDNA1/MOMP vaccination protected all turkeys against severe clinical signs and lesions following C. psittaci challenge. Both immunization methods gave comparable protection levels. In all aerosol-infected turkeys, chlamydiae could still replicate in epithelial cells and macrophages of the respiratory tract, resulting in nasal excretion for 6 days following challenge. Possibly, the protection level at the respiratory tract would have been higher if a less severe challenge had been chosen. Notwithstanding the severe challenge used, chlamydia replicated outside the respiratory tract in only two out of 15 pcDNA1/MOMP-vaccinated turkeys. By contrast, in all control turkeys chlamydia replicated intensively outside the respiratory tract, resulting in positive cloacal cultures throughout the observation period. Chlamydia isolation from the pericardium of two vaccinated turkeys might result from contamination by the surrounding infected air sacs, rather than from septicaemia, as chlamydia replicated not in the liver and the spleen, and all cloacal cultures remained negative throughout the observation period.
Gene gun delivery of small amounts (2.0 μg) of pcDNA1/MOMP as well as intramuscular–intranasal DNA delivery did prime both Th and B cell memory, although rMOMP-expressing cells did not induce high antibody responses. Following the pcDNA1/MOMP inoculations, rising titres of antibodies belonging to the IgG isotype evidenced the priming of memory. IgG is produced by differentiated plasma cells that have undergone immunoglobulin rearrangements in response to T cell help. Evidence for the mobilization of B cell memory in response to challenge was found in all vaccinated turkeys, as IgG levels where significantly higher than IgM levels. Mobilization of T cell memory in response to challenge was evidenced in all vaccinated turkeys by the significantly higher PBL proliferative responses following challenge compared with the non-vaccinated turkeys.
The best protection occurred in turkeys which upon challenge did not demonstrate secondary antibody responses. In these turkeys, chlamydia replicated only weakly in the air sacs, whereas in turkeys with secondary serum antibody responses chlamydia replicated also in the lungs. There was no correlation between titres and protection, nor between immunoglobulin isotype and protection. These data support recent studies in mice showing that antibody, including mucosal IgA, is not an absolute requirement for relatively successful defence against chlamydia [8,12,14]. However, these studies did not exclude a role for local antibodies in protection. Moreover, one must be aware that protection data in mice do not necessarily apply to other animal species, such as birds. For instance, guinea pigs may rely more heavily on local antibody production than mice do [27]. Therefore, further DNA vaccination experiments in turkeys will examine the effect of local antibodies or local antibody-producing cells on protection. Regarding this, an ELISPOT assay for the quantification of mucosal antibody-producing cells is currently being evaluated (Vanrompay et al., unpublished results).
Proliferative responses in PBL stimulated in vitro with rMOMP indicated that only intramuscular–intranasal and gene gun DNA-immunized turkeys induced strong responses. It is our intention to determine the percentage of CD4+ and CD8+ T cells using anti-chicken CD4 and CD8 MoAbs cross-reactive with turkey lymphocytes or anti-turkey CD4 and CD8 MoAbs.
Gene gun delivery of DNA into the epidermis was the most efficient immunization method, since it required 100 times less DNA than the saline inoculations (2.0 μg as opposed to 200 μg of DNA). This is in agreement with earlier studies comparing different DNA immunization methods [28]. Therefore, the Helios Gene Gun system obviously represents a very effective transfection method. When the avian epidermis is transfected, antigens probably become subject to immune surveillance by lymphoid foci present in the bird's skin. As in mammals, these lymphoid foci are rich in antigen-presenting cells (Langerhans cells) being transported to the spleen, where they can activate naive T cells.
Recently, Zhang et al. [29] reported that a MOMP-based DNA vaccine could reduce lung titres of C. trachomatis mouse pneumonitis (MoPn) organisms following intranasal challenge in the presence of a poor serological response. Strugnell et al. [30] also observed poor serological responses to MOMP-based DNA, comparing the immunogenicity in mice of a C. trachomatis MOMP-DNA with that of DNA vaccines expressing influenza nucleoprotein or haemagglutinin. Moreover, notwithstanding the better resistance to lethal challenge, all mice became ill and were killed.
In conclusion, the present results demonstrate the efficacy of DNA vaccination as a means of preventing severe clinical signs, lesions and chlamydia excretion in a turkey model of C. psittaci infection. Further studies need to define the immune mechanism(s) for the protection observed. Identification of these mechanisms might allow an increase in the efficacy of the current chlamydia DNA vaccine, e.g. by using cytokine fusion constructs or by co-inoculating vectors encoding either cytokines or co-stimulatory molecules.
Acknowledgments
The Fund for Scientific Research (FWO) Flanders, The Flemish Institute for the Promotion of Scientific-Technological Research in the Industry (IWT) and the Flemish Scientific Foundation (VWS), supported D.V. E. Defoor, K. Meylemans, D. Slos and M. Voet are acknowledged for technical assistance.
REFERENCES
- 1.Vanrompay D, Mast J, Ducatelle R, Haesebrouck F, Goddeeris BM. Chlamydia psittaci infections in turkeys: pathogenesis of infections in avian serovar A, B and D. Vet Microbiol. 1995;47:245–56. doi: 10.1016/0378-1135(95)00125-5. [DOI] [PubMed] [Google Scholar]
- 2.Anderson IE, Tan TW, Jones GE, Herring AJ. Efficacy against ovine enzootic abortion of an experimental vaccine containing purified elementary bodies of Chlamydia psittaci. Vet Microbiol. 1990;24:21–27. doi: 10.1016/0378-1135(90)90047-y. [DOI] [PubMed] [Google Scholar]
- 3.Tan TW, Herring AJ, Anderson IE, Jones GE. Protection of sheep against Chlamydia psittaci infection with a subcellular vaccine containing the major outer membrane protein. Infect Immun. 1990;58:3101–8. doi: 10.1128/iai.58.9.3101-3108.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuffrey M, Alexander F, Conlan W, Woods C, Ward M. Heterotypic protection of mice against chlamydial salpingitis and colonization of the lower genital tract with a human serovar F isolate of Chlamydia trachomatis by prior immunization with recombinant serovar L1 major outer membrane protein. J Gen Microbiol. 1992;138:1707–15. doi: 10.1099/00221287-138-8-1707. [DOI] [PubMed] [Google Scholar]
- 5.Sturgess CP, Gruffydd-Jones TJ, Harbour DA, Feilden HR. Studies on the safety of Chlamydia psittaci vaccination in cats. Vet Rec. 1995;137:668–9. [PubMed] [Google Scholar]
- 6.Sandbulte J, TerWee J, Wigington K, Sabara M. Evaluation of Chlamydia psittaci subfraction and subunit preparations for their protective capacities. Vet Microbiol. 1996;48:269–82. doi: 10.1016/0378-1135(95)00166-2. [DOI] [PubMed] [Google Scholar]
- 7.Pal S, Theodor L, Peterson EM, de la Maza LM. Immunization with an acellular vaccine consisting of the outer membrane protein complex of Chlamydia trachomatis induces protection against a genital challenge. Infect Immun. 1997;65:3361–9. doi: 10.1128/iai.65.8.3361-3369.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cotter TW, Meng Q, Shen Z-L, Zhang Y-X, ¤¤..¤¤su H, Caldwell HD. Protective efficacy of major outer membrane protein-specific immunoglobulin A (IgA) and IgG monoclonal antibodies in a murine model of Chlamydia trachomatis genital tract infection. Infect Immun. 1995;63:4704–14. doi: 10.1128/iai.63.12.4704-4714.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su H, Caldwell HD. CD4+ T cells play a significant role in adoptive immunity to Chlamydia trachomatis infection of the mouse genital tract. Infect Immun. 63:3302–8. doi: 10.1128/iai.63.9.3302-3308.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beatty PR, Rasmussen SJ, Stephens RS. Cross-reactive cytotoxic T-lymphocyte-mediated lysis of Chlamydia trachomatis and Chlamydia psittaci-infected cells. Infect Immun. 1997;65:951–6. doi: 10.1128/iai.65.3.951-956.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cotter TW, Ramsey KH, Miranpuri GS, Poulsen ChE, Byrne GI. Dissemination of Chlamydia trachomatis chronic genital tract infection in gamma interferon gene knockout mice. Infect Immun. 1997;65:2145–52. doi: 10.1128/iai.65.6.2145-2152.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johansson M, Schön K, Ward M, Lycke N. Genital tract infection with Chlamydia trachomatis fails to induce protective immunity in gamma interferon receptor-deficient mice despite a strong local immunoglobulin A response. Infect Immun. 1997;65:1032–44. doi: 10.1128/iai.65.3.1032-1044.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Su H, Feilzer K, Caldwell HD, Morrison RP. Chlamydia trachomatis genital tract infection of antibody-deficient gene knockout mice. Infect Immun. 1997;65:1993–9. doi: 10.1128/iai.65.6.1993-1999.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams DM, Grubbs BG, Pack E, Kelly K, Rank RG. Humoral and cellular immunity in secondary infection due to murine Chlamydia trachomatis. Infect Immun. 1997;65:2876–82. doi: 10.1128/iai.65.7.2876-2882.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donelly JJ, Ulmer JB, Shiver JW, Liu MA. DNA vaccines. Annu Rev Immunol. 1997;15:617–48. doi: 10.1146/annurev.immunol.15.1.617. [DOI] [PubMed] [Google Scholar]
- 16.Tighe H, Corr M, Roman M, Raz E. Gene vaccination: plasmid DNA is more than just a blueprint. Immunol Today. 1998;19:89–97. doi: 10.1016/s0167-5699(97)01201-2. [DOI] [PubMed] [Google Scholar]
- 17.Hatch TP, Vance DW, Al-Hossainey E. Identification of a major envelope protein in Chlamydia spp. J Bacteriol. 1981;146:426–9. doi: 10.1128/jb.146.1.426-429.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caldwell HD, Kromhout J, Schachter J. Purification and partial characterization of the major outer membrane protein of Chlamydia trachomatis. Infect Immun. 1981;31:1161–76. doi: 10.1128/iai.31.3.1161-1176.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salari SH, Ward ME. Polypeptide composition of Chlamydia trachomatis. J Gen Microbiol. 1981;123:197–207. doi: 10.1099/00221287-123-2-197. [DOI] [PubMed] [Google Scholar]
- 20.Lucero ME, Kuo CC. Neutralization of Chlamydia trachomatis cell culture infection by serovar-specific monoclonal antibodies. Infect Immun. 1985;50:595–7. doi: 10.1128/iai.50.2.595-597.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Y-X, Stewart S, Joseph T, Taylor HR, Caldwell HD. Protective monoclonal antibodies recognize epitopes located on the major outer membrane protein of Chlamydia trachomatis. J Immunol. 1987;138:575–81. [PubMed] [Google Scholar]
- 22.Vanrompay D, Cox E, Mast J, Goddeeris BM, Volckaert G. High-level expression of the Chlamydia psittaci major outer membrane protein in COS cells and in turkey muscle cells. Infect Immun. 1998;66:5494–500. doi: 10.1128/iai.66.11.5494-5500.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vanrompay D, Butaye P, Sayada Ch, Ducatelle R, Haesebrouck F. Characterization of European avian Chlamydia psittaci strains using omp1 gene restriction mapping and serovar-specific monoclonal antibodies. Res Microbiol. 1997;148:327–33. doi: 10.1016/S0923-2508(97)81588-4. [DOI] [PubMed] [Google Scholar]
- 24.Vanrompay D, Van Nerom A, Ducatelle R, Haesebrouck F. Evaluation of five immunoassays for detection of Chlamydia psittaci in cloacal and conjunctival specimens from turkeys. J Clin Microbiol. 1994;32:1470–4. doi: 10.1128/jcm.32.6.1470-1474.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Novak M, Moldoveanu Z, Schafer DP, Mestecky J, Compans RW. Murine model for evaluation of protective immunity to influenza virus. Vaccine. 1993;11:55–60. doi: 10.1016/0264-410x(93)90339-y. [DOI] [PubMed] [Google Scholar]
- 26.Sjöberg O, Andersson L, Möller G. Requirement for adherent cells in the primary and secondary immune response in vitro. Eur J Immunol. 1972;2:123–9. doi: 10.1002/eji.1830020206. [DOI] [PubMed] [Google Scholar]
- 27.Rank RG, Batteiger BE. Protective role of serum antibody in immunity to chlamydial genital infection. Infect Immun. 1989;57:299–301. doi: 10.1128/iai.57.1.299-301.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fynan EF, Webster RG, Fuller DH, Haynes JR, Santoro JC, Robinson HL. DNA vaccines: protective immunizations by parenteral, mucosal, and gene-gun inoculations. Proc Natl Acad Sci USA. 1993;90:11478–82. doi: 10.1073/pnas.90.24.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang D, Yang X, Berry J, Shen C, McClarty G, Brunham RC. DNA vaccination with the MOMP gene induces acquired immunity to Chlamydia trachomatis(mouse pneumonitis) infection. Infect Immun. 1997;176:1035–40. doi: 10.1086/516545. [DOI] [PubMed] [Google Scholar]
- 30.Strugnell RA, Drew D, Mercieca J, Di Natale S, Firez N, Dunstan SJ, Simmons CP, Vadolas J. DNA vaccines for bacterial infections. Immunol Cell Biol. 1997;75:364–9. doi: 10.1038/icb.1997.57. [DOI] [PubMed] [Google Scholar]


