Abstract
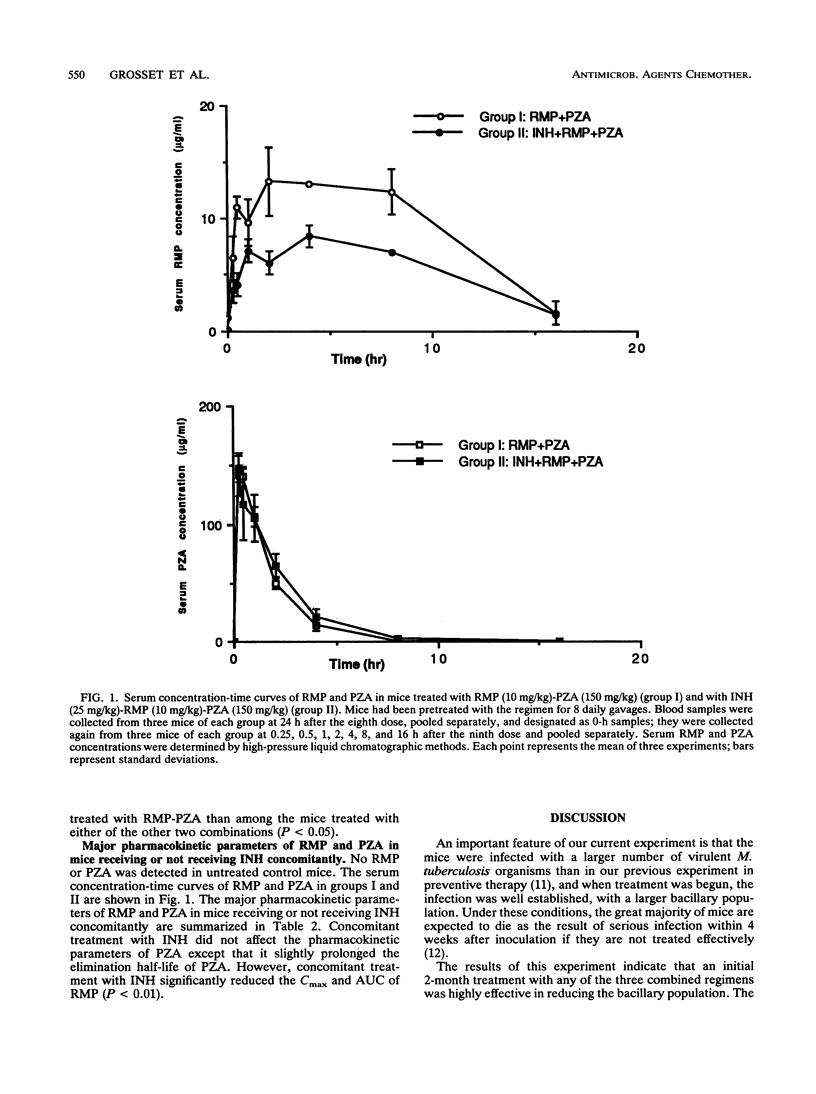
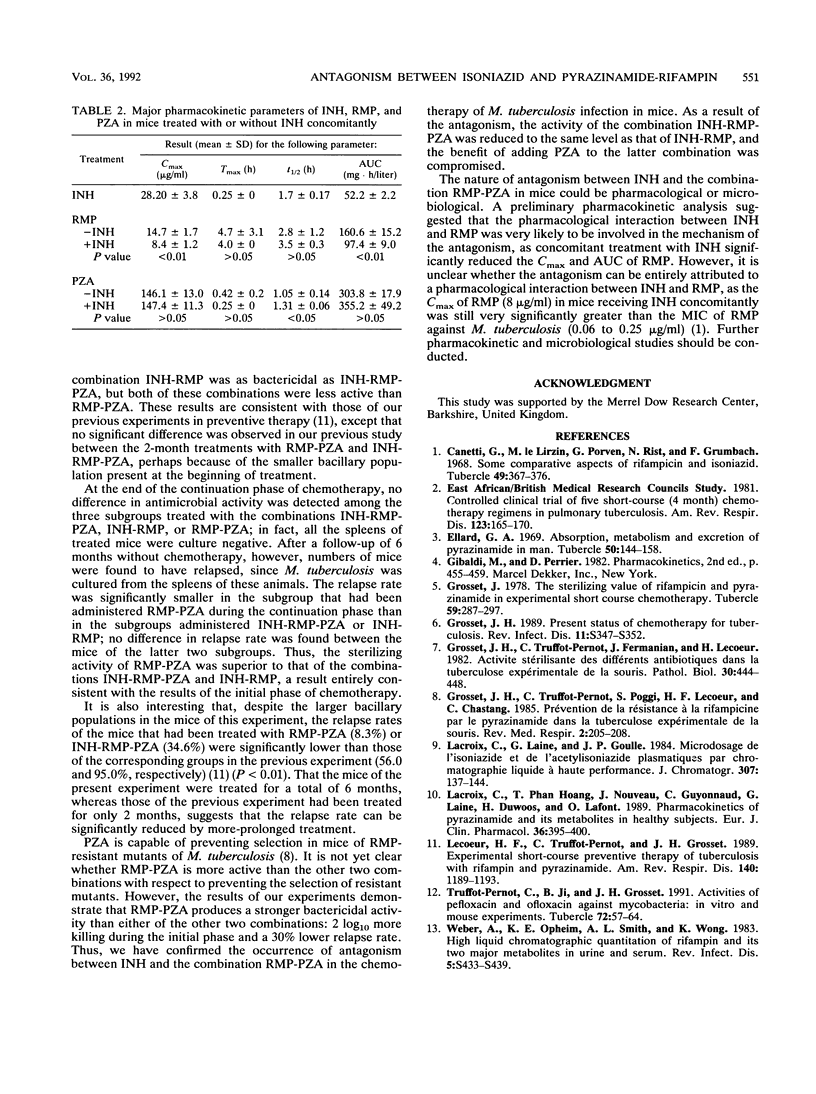
Mice that had been inoculated intravenously with 6.30 log10 Mycobacterium tuberculosis H37Rv 14 days earlier were administered one of three combinations of drugs, i.e., isoniazid (INH)-rifampin (RMP)-pyrazinamide (PZA), INH-RMP, and RMP-PZA, during an initial 2-month period to mimic the initial phase of chemotherapy for human tuberculosis and during a later 4-month period to mimic the continuation phase of chemotherapy. At the end of the initial phase, all three combined regimens were found to have been highly effective in terms of the number of CFUs in the spleens of infected mice. The bactericidal activities of INH-RMP-PZA and INH-RMP were similar, whereas that of RMP-PZA was significantly greater. The spleens of all of the mice that had been treated initially with INH-RMP-PZA were culture negative by the end of 6 months of treatment, regardless of the regimen employed during the continuation phase. However, after an additional period of 6 months without treatment, the proportion of spleen culture positivity, or relapse rate, was significantly smaller in the subgroup treated with RMP-PZA during the continuation phase than in the subgroups treated with INH-RMP-PZA or INH-RMP; the relapse rate did not differ significantly between the latter two subgroups. These results suggest that antagonism occurs between INH and the combination RMP-PZA during both the initial and continuation phases of chemotherapy, compromising the benefit conferred by the addition of PZA to the combined regimen.The preliminary pharmacokinetic analysis suggested that the pharmacological interaction between INH and RMP was very likely to be involved in the mechanism of antagonism, as concomitant treatment with INH had significantly reduced the peak serum level and the area under the serum concentration-time curve of RMP in mice.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Canetti G., Le Lirzin M., Porven G., Rist N., Grumbach F. Some comparative aspects of rifampicin and isoniazid. Tubercle. 1968 Dec;49(4):367–376. doi: 10.1016/s0041-3879(68)80017-0. [DOI] [PubMed] [Google Scholar]
- Ellard G. A. Absorption, metabolism and excretion of pyrazinamide in man. Tubercle. 1969 Jun;50(2):144–158. doi: 10.1016/0041-3879(69)90020-8. [DOI] [PubMed] [Google Scholar]
- Grosset J. H. Present status of chemotherapy for tuberculosis. Rev Infect Dis. 1989 Mar-Apr;11 (Suppl 2):S347–S352. doi: 10.1093/clinids/11.supplement_2.s347. [DOI] [PubMed] [Google Scholar]
- Grosset J., Truffot-Pernot C., Poggi S., Lecoeur H., Chastang C. Prévention de la résistance à la rifampicine par le pyrazinamide dans la tuberculose expérimentale de la souris. Rev Mal Respir. 1985;2(4):205–208. [PubMed] [Google Scholar]
- Grosset J., Truffot C., Fermanian J., Lecoeur H. Activité stérilisante des différents antibiotiques dans la tuberculose expérimentale de la souris. Pathol Biol (Paris) 1982 Jun;30(6):444–448. [PubMed] [Google Scholar]
- Lacroix C., Hoang T. P., Nouveau J., Guyonnaud C., Laine G., Duwoos H., Lafont O. Pharmacokinetics of pyrazinamide and its metabolites in healthy subjects. Eur J Clin Pharmacol. 1989;36(4):395–400. doi: 10.1007/BF00558302. [DOI] [PubMed] [Google Scholar]
- Lacroix C., Laine G., Goulle J. P., Nouveau J. Microdosage de l'isoniazide et de l'acetylisoniazide plasmatiques par chromatographie liquide à haute performance. J Chromatogr. 1984 Apr 13;307(1):137–144. [PubMed] [Google Scholar]
- Lecoeur H. F., Truffot-Pernot C., Grosset J. H. Experimental short-course preventive therapy of tuberculosis with rifampin and pyrazinamide. Am Rev Respir Dis. 1989 Nov;140(5):1189–1193. doi: 10.1164/ajrccm/140.5.1189. [DOI] [PubMed] [Google Scholar]
- Truffot-Pernot C., Ji B., Grosset J. Activities of pefloxacin and ofloxacin against mycobacteria: in vitro and mouse experiments. Tubercle. 1991 Mar;72(1):57–64. doi: 10.1016/0041-3879(91)90025-n. [DOI] [PubMed] [Google Scholar]
- Weber A., Opheim K. E., Smith A. L., Wong K. High-pressure liquid chromatographic quantitation of rifampin and its two major metabolites in urine and serum. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S433–S439. doi: 10.1093/clinids/5.supplement_3.s433. [DOI] [PubMed] [Google Scholar]


