Tuberculosis (TB) remains one of the leading infectious causes of illness and death world-wide and, even though it has been declared a Global Emergency by the World Health Organization [1], the annual number of cases continues to escalate. A principal reason for our failure to control this disease is the lack of a vaccine that is effective in all regions of the world and which can be given safely to those already infected by tubercle bacilli, thereby preventing them from developing post-primary, transmissible, pulmonary disease [2].
Despite many attempts to develop new immunizing agents [3,4], bacille Calmette–Guérin (BCG), a living attenuated derivative of a bovine tubercle bacillus (Mycobacterium bovis), is the only available vaccine against TB. The choice of this species rather than M. tuberculosis itself for the development of a vaccine strain was influenced by Robert Koch's dubious assertion that bovine tubercle bacilli are of low virulence in humans and by the equally dubious Marfan's Law which stated that children who recovered from non-pulmonary manifestations of TB of bovine origin were protected against the more severe pulmonary TB in adult life [5]. Accordingly, Albert Calmette (Fig. 1) and Camille Guérin attempted to attenuate their strain by the random process of subculturing it 230 times on slices of potato soaked in bile and glycerol over a 13-year period, until extensive animal inoculations convinced them that the strain was irreversibly attenuated [6]. It was first administered to neonates born to mothers with open TB and who were thus at high risk of developing the disease. It was given orally, to mimic milk-borne infection by M. bovis, and appeared to give 90% protection [7].
Fig. 1.
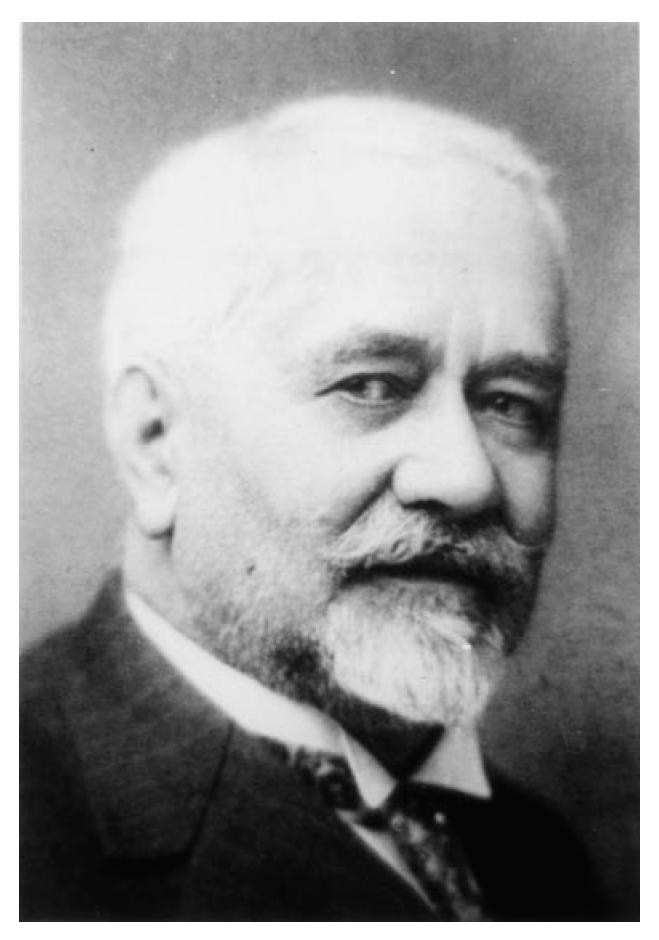
Albert Calmette (1863–1933), the pioneer of vaccination against tuberculosis.
The BCG strain was then distributed to many centres world-wide and propagated locally for use as an oral vaccine but, in 1930, a tragedy occurred in the North German city of Lübeck where, owing to a labelling accident, the children of that city were vaccinated with a virulent strain of M. tuberculosis instead of BCG and over 70 died [8]. As a result, BCG was subsequently prepared in special production plants and freeze-dried for intradermal injection and, principally after the Second World War, attempts were made to determine its safety and protective efficacy by means of extensive clinical trials.
Two important findings emerged from these trials. First, the protective efficacy of BCG varies considerably from region to region—from around 80% protection to none at all [9]. Indeed, in some regions BCG vaccination may well have had a detrimental effect on protection [10,11]. Second, where a beneficial effect was observed, BCG protected neonates and children against serious but principally non-infectious forms of primary disease such as tuberculous meningitis, but afforded little or no protection against infectious, post-primary, pulmonary TB in adolescents and adults [12].
Thus, BCG is a two-edged sword—protecting in some circumstances but failing to protect or even predisposing to active TB in others [11]. This raises the question of whether, despite the lengthy process of attenuation to which it was subjected, BCG retains determinants that are associated with immunopathology and virulence, as indeed Calmette's early critics claimed [13].
In contrast to several other bacterial pathogens, notably highly toxigenic bacteria such as Corynebacterium diphtheriae that have single clearly defined virulence determinants, the virulence of M. tuberculosis is poorly understood and is almost certainly multifactorial [14]. A further problem is that infection by a tubercle bacillus may induce either protective immunity or tissue-destroying hypersensitivity reactions that lead to progressive disease. Ever since Clemens von Pirquet introduced the tuberculin test in 1907 as an indicator of past infection by the tubercle bacillus [15], there has been controversy as to whether protective immunity and tissue-destroying hypersensitivity reactions in TB are quite distinct reactions or differ only in intensity [16]. This issue has been largely resolved by the demonstration in recent years that the two types of reaction are mediated by different cytokines. Thus there is evidence that protective reactions are mediated by type 1 immune responses, while a superimposed type 2 response leads to immunopathology [17,18]. Of the several explanations that have been advanced to account for the regional variation in the protective efficacy of BCG, the most generally accepted one is that, while neonatal BCG vaccination confers protection and induces a type 1 immune response [19], older children and adults are primed for either protective or tissue-necrotizing immune responses by prior contact with various populations of saprophytic mycobacteria in the environment, and that BCG vaccination boosts the preselected response [20,21].
There is therefore a need for a vaccine against TB which is not adversely affected by environmental factors and is thus of universal efficacy. Fortunately the time has now arrived when, thanks to the characterization of the entire genome of M. tuberculosis [22], and the availability of techniques for transferring genes between mycobacterial species, it is possible to examine the role of the many antigens and other constituents of this bacillus in the various immune responses and to determine whether any factors have the potential to interfere with the induction of protective immunity by BCG.
In this edition, Yeremeev and colleagues report their continuing studies on the 19-kD antigen which is present in members of the M. tuberculosis complex, including BCG, and some other slowly growing mycobacteria, but not in the rapidly growing species M. vaccae and M. smegmatis [23]. Yeremeev and colleagues confirm the findings of previous workers that, at a suitable concentration, a strain of M. vaccae confers protection against experimental TB in mice [24], and they also show that the same strain expressing the 19-kD antigen fails to protect. It is thus postulated that, by lacking a determinant antagonistic to protection, a laboratory-selected mutant strain of BCG unable to express the 19-kD antigen would have improved protective efficacy.
In considering the mechanism by which the 19-kD antigen exerts its adverse effect, it is noteworthy that a strong type 1 immune response specifically to the 19-kD antigen alone did not have a detrimental effect on protective immunity. It was therefore postulated that the observed detrimental activity of this antigen is the result of its effect on immune recognition of other antigens in the vaccinating strain. In support of this, vaccination with M. smegmatis or M. vaccae expressing the 19-kD antigen significantly reduced dermal responses to PPD, which consists principally of antigens common to all mycobacteria, following infection by M. tuberculosis.
In this context, it is noteworthy that skin testing surveys have revealed that, in contrast to healthy infected persons, patients with active leprosy or TB have a reduced ability to respond to those antigens common to all mycobacteria [25,26]. Intriguingly, a similar reduction in dermal responses to shared mycobacterial antigens has been demonstrated in Chagas' disease which, like mycobacterial diseases, is characterized by intracellular parasitism [27]. This raises the possibility that an important determinant of virulence of at least some intracellular parasites is their ability to down-regulate immune recognition of widely distributed antigens, notably the stress-related proteins, such as the 65-kD heat shock protein which is able to evoke protective immunity against TB [28]. This ‘immunological blindness’ could compromise the induction of apoptosis of pathogen-laden cells, a process shown to have a deleterious effect on such parasites [29].
Another factor requiring consideration is the evidence from studies of patients with TB that M. vaccae exerts its protective effect by down-regulating type 2 immune responses responsible for immunopathology, and by enhancing protective type 1 responses [30]. It is thus possible that the 19-kD antigen directly or indirectly interferes with this beneficial immunoregulatory effect. If this is the case, a vaccine lacking this antigen might be able to down-regulate adverse immune responses that are thought to compromise the protective efficacy of BCG vaccination in some regions.
Whatever the mechanism of action, the studies on the 19-kD antigen by Yeremeev and colleagues point to a novel class of virulence determinants that may occur, possibly in structurally diverse forms, in a wide range of intracellular pathogens. More importantly, these studies herald a shift from the hit-and-miss attenuation procedures pioneered by Louis Pasteur and utilized by Calmette and Guérin to a much more rational selection of mutants or genetically engineered modifications of mycobacteria for use as anti-tuberculosis vaccines. This in turn holds out hope for the eventual conquest of a disease which for far too long has been the ‘Captain of all of these Men of Death’.
REFERENCES
- 1.World Health Organization. TB—a global emergency. Geneva: World Health Organization; 1994. [Google Scholar]
- 2.Fine PE. Vaccines, genes and trials. Novartis Found Symp. 1998;217:57–69. doi: 10.1002/0470846526.ch5. discussion 69–72. [DOI] [PubMed] [Google Scholar]
- 3.Grange JM. Vaccination against tuberculosis: past problems and future hopes. Semin Respir Crit Care Med. 1997;18:459–70. [Google Scholar]
- 4.Orme IM. New vaccines against tuberculosis. The status of current research. Infect Dis Clin North Am. 1999;13:169–85. doi: 10.1016/s0891-5520(05)70049-0. [DOI] [PubMed] [Google Scholar]
- 5.Savage WG. The prevention of human tuberculosis of bovine origin. London: MacMillan; 1929. [Google Scholar]
- 6.Guérin C. The history of BCG: early history. In: Rosenthal SR, editor. BCG vaccination against tuberculosis. London: Churchill; 1953. [Google Scholar]
- 7.Weil-Hallé B, Turpin R. Premiers essais de vaccination antituberculeuse de l'enfant par le bacille Calmette-Guérin (BCG) Bull Mem Soc Med Hôp Paris. 1925;14:1589. [Google Scholar]
- 8.Calmette A. Epilogue de la catastrophe de Lübeck. Presse Med. 1931;2:17. [Google Scholar]
- 9.Colditz GA, Berkey CS, Mosteller F, et al. The efficacy of bacillus Calmette–Guérin vaccination of newborns and infants in the prevention of tuberculosis: meta-analyses of the published literature. Pediatrics. 1995;96:29–35. [PubMed] [Google Scholar]
- 10.Ponnighaus JM, Fine PE, Sterne JA, et al. Efficacy of BCG vaccine against leprosy and tuberculosis in northern Malawi. Lancet. 1992;339:636–9. doi: 10.1016/0140-6736(92)90794-4. [DOI] [PubMed] [Google Scholar]
- 11.Springett VH, Sutherland I. A re-examination of the variations in the efficacy of BCG vaccination against tuberculosis in clinical trials. Tubercle Lung Dis. 1994;75:227–33. doi: 10.1016/0962-8479(94)90013-2. [DOI] [PubMed] [Google Scholar]
- 12.Styblo K, Meijer J. Impact of BCG vaccination programmes in children and young adults on the tuberculosis problem. Tubercle. 1976;57:17–43. doi: 10.1016/0041-3879(76)90015-5. [DOI] [PubMed] [Google Scholar]
- 13.Petroff SA. A new analysis of the value and safety of protective immunization with BCG (bacille Calmette–Guérin) Am Rev Tuberc. 1929;20:275–96. [Google Scholar]
- 14.Gordon S, Andrew PW. Mycobacterial virulence factors. J Appl Bacteriol. 1996;81(Suppl.):10S–22S. [PubMed] [Google Scholar]
- 15.von Pirquet C. Demonstration zur Tuberculindiagnose durch Hautimpfung. Berl Klin Wochenschr. 1909;481:699. [Google Scholar]
- 16.Bothamley GH, Grange JM. The Koch phenomenon and delayed hypersensitivity 1891–1991. Tubercle. 1991;72:7–12. doi: 10.1016/0041-3879(91)90018-n. [DOI] [PubMed] [Google Scholar]
- 17.Dlugovitzky D, Torres-Morales A, Rateni L, Farroni MA, Largacha C, Molteni O, Bottasso O. Circulating profile of Th1 and Th2 cytokines in tuberculosis patients with different degrees of pulmonary involvement. FEMS Immunol Med Microbiol. 1997;18:203–7. doi: 10.1111/j.1574-695X.1997.tb01046.x. [DOI] [PubMed] [Google Scholar]
- 18.Surcel H-M, Troyer-Blomberg M, Paulie S, Andersson G, Moreno C, Pasvol G, Ivanyi J. Th1/Th2 profiles in tuberculosis based on proliferation and cytokine response of blood lymphocytes to mycobacterial antigens. Immunology. 1994;81:171–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Marchent A, Goetghebuer T, Ota MO, et al. Newborns develop a Th1-type immune response to Mycobacterium bovis bacillus Calmette–Guérin vaccination. J Immunol. 1999;163:2249–55. [PubMed] [Google Scholar]
- 20.Stanford JL, Shield MJ, Rook GAW. Hypothesis 1. How environmental mycobacteria may predetermine the protective efficacy of BCG. Tubercle. 1981;62:55–62. doi: 10.1016/0041-3879(81)90037-4. [DOI] [PubMed] [Google Scholar]
- 21.Fine PE. Variation in protection by BCG: implications of and for heterologous immunity. Lancet. 1995;346:1339–45. doi: 10.1016/s0140-6736(95)92348-9. [DOI] [PubMed] [Google Scholar]
- 22.Cole ST, Brosch R, Parkhill J, et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature. 1998;393:537–44. doi: 10.1038/31159. [DOI] [PubMed] [Google Scholar]
- 23.Yeremeev VV, Lyadova IV, Nikonenko BV, et al. The 19-kD antigen and protective immunity in a murine model of tuberculosis. Clin Exp Immunol. 2000;120:274–9. doi: 10.1046/j.1365-2249.2000.01212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hernandez-Pando R, Pavon L, Arriaga K, Orozco H, Madrid-Marina V, Rook G. Pathogenesis of tuberculosis in mice exposed to low and high doses of an environmental mycobacterial saprophyte before infection. Infect Immun. 1997;65:3317–27. doi: 10.1128/iai.65.8.3317-3327.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stanford JL, Nye PM, Rook GAW, Samuel N, Fairbank A. A preliminary investigation of the responsiveness or otherwise of patients and staff of a leprosy hospital to groups of shared or specific antigens of mycobacteria. Lepr Rev. 1981;52:321–7. doi: 10.5935/0305-7518.19810043. [DOI] [PubMed] [Google Scholar]
- 26.Kardjito T, Beck JS, Grange JM, Stanford JL. A comparison of the responsiveness to four new tuberculins among Indonesian patients with pulmonary tuberculosis and healthy subjects. Eur J Respir Dis. 1986;69:142–5. [PubMed] [Google Scholar]
- 27.Bottasso OA, Ingledew N, Keni M, Morini J, Pividori JF, Rook GA, Stanford JL. Cellular immune response to common mycobacterial antigens in subjects seropositive for Trypanosoma cruzi. Lancet. 1994;344:1540–1. doi: 10.1016/s0140-6736(94)90351-4. [DOI] [PubMed] [Google Scholar]
- 28.Lowrie DB, Silva CL, Colston MJ, Ragno S, Tascon RE. Protection against tuberculosis by a plasmid DNA vaccine. Vaccine. 1997;15:834–8. doi: 10.1016/s0264-410x(97)00073-x. [DOI] [PubMed] [Google Scholar]
- 29.Molloy A, Laochumroonvorapong P, Kaplan G. Apoptosis, but not necrosis, of infected monocytes is coupled with killing of intracellular bacillus Calmette–Guérin. J Exp Med. 1994;180:1499–509. doi: 10.1084/jem.180.4.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dlugovitzky D, Bottasso O, Dominino JC, et al. Clinical and serological studies of tuberculosis patients in Argentina receiving immunotherapy with Mycobacterium vaccae (SRL 172) Respir Med. 1999;93:557–62. doi: 10.1016/s0954-6111(99)90155-5. [DOI] [PubMed] [Google Scholar]


