Abstract
The purpose of this study was to compare fat-free mass (FFM) and percent body fat determined by two bio-electrical impedance analysis (BIA) instruments against criterion estimates determined by dual-energy x-ray absorptiometry (DXA) in a multi-racial/ethnic sample of adolescent girls. BIA was assessed in 151 girls (n=51 African-American; n=45 Hispanic; n=55 Caucasian; age 12.2 ± 1.2 yr) using the RJL Quantum II and the American Weights and Measures Body-Comp Scale (BCS). Percent body fat determined by BIA was significantly related to that determined by DXA (R2=0.87, SEE=2.8% for RJL vs DXA, P<0.0001; R2=0.71, SEE=4.4% for BCS vs DXA, P<0.0001). The agreement between DXA and BIA for FFM was also significant (R2=0.91, SEE=0.03 kg for RJL, P <0.0001; R2=0.79, SEE=0.04 kg for BCS, P <0.0001). The BCS overestimated FFM by 2.7 kg (P<0.0001) and underestimated percent body fat by over 4% (P<0.001). There were no differences in percent body fat between DXA and the RJL, and although the RJL significantly overestimated FFM, the absolute difference was <1 kg. Within each ethnic group, the RJL instrument more closely estimated FFM and percent body fat than did the BCS. Although both BIA instruments compared favorably with DXA, the RJL had better stability and accuracy than the BCS, for both the total sample and for the three ethnic groups. Considering its relatively low cost and minimal time required for technical training, BIA is a useful and appropriate technique for assessing body composition in adolescent girls.
Keywords: body composition, body fat, children, ethnicity
Introduction
As the prevalence of childhood and adolescent obesity continues to rise in the US, the need for behavioral interventions to prevent and reduce this public health burden becomes more evident. Health care professionals and fitness specialists working with children and adolescents in field settings need accurate, reliable, and inexpensive techniques to monitor the effectiveness of behavioral interventions targeted to favorably alter body composition in this population.
At present there is a host of methods and devices available for assessing body composition. Bioelectrical impedance analysis (BIA) and skinfold assessments are two techniques used frequently by personal trainers and other fitness professionals to measure percent body fat and fat-free mass (FFM). Research on BIA showed that more accurate estimates of body composition could be obtained in adolescents by using prediction equations that included anthropometric and impedance measurements, rather than impedance alone [1]. However, the improved accuracy with anthropometric measurements was very small. Because BIA requires less technical skill than skinfold assessments, quality control for BIA may be easier to maintain, especially in fitness centers that employ a large number of instructors/trainers and/or have a high staff turnover rate, and in schools where training opportunities may be limited.
The BIA technique is a two-compartment model based on the principle that an electric current flows more rapidly through tissues with higher water and electrolyte content than through tissue less hydrated. Due to the greater electrolyte content of FFM, it offers less resistance to electric current compared to fat tissue. Thus, resistance, or impedance to electric current, directly relates to the amount of FFM. Fat mass is then calculated by subtracting FFM from total body mass. Skinfold equations, on the other hand, provide estimates of body density or percent body fat, from which FFM can then be derived.
The accuracy and reliability of BIA has been reported in both adults [2–5] and in children and adolescents [6–14], sometimes in studies with small sample sizes [7, 9]. Although some BIA validity studies have employed participants representing ethnic minorities [6, 8, 11–14], few differentiated the results by race. Thus, it is unclear whether BIA devices yield similar results across different ethnic groups. The present study was conducted to determine the accuracy of two BIA instruments for measuring body composition in a multiethnic sample of adolescent girls with a wide range of body mass index (BMI). We compared body fatness and fat-free mass determined by the RJL and American Weights & Measures Body Comp Scales to that determined by dual energy x-ray absorptiometry (DXA).
Subjects and methods
Subjects
This report presents results from a substudy of the multi-site Trial of Activity for Adolescent Girls (TAAG) study. Prior to initiating the main study, a multi-ethnic sample of girls of the same age group as that targeted in the main trial was recruited to determine an appropriate method for assessing the body composition of participants in the main trial. Approval for the sub-study was obtained by the respective IRB at each of three study sites (San Diego State University, Tulane University and the University of Arizona) participating in this substudy. Written parental consent and participant written assent were obtained for all participants.
Participants
The recruitment goal was 180 girls, distributed evenly among three race/ethnic groups (n=60 each: African-American, non-Black Hispanic, non-Hispanic White (Caucasian)). One hundred sixty-nine girls were recruited and measured. Fifteen of the 169 girls self-reported mixed ethnicity; rather than arbitrarily assigning those girls to one of the three groups, they were excluded from data analyses. Another three girls were excluded due to missing DXA values. Thus, the final sample size of the present study was 151. Approximately one-third of the sample was measured at each geographic site. Additional inclusion criteria included girls in grade 6 or 8, age 10–15 years, with a wide range of values for BMI. These criteria were selected to be consistent with those for the main trial. Although physical activity was not assessed in the present study, by recruiting girls with a wide range of BMI we expected our sample to be heterogeneous in terms of physical activity and fitness, and therefore representative of the target population. Girls were screened to include approximately 50 percent in each age group with a BMI above the age-specific median (50th percentile) BMI.
Methods
All measurements were conducted during a single visit to each site’s laboratory. The girls were asked to wear clothing free of metal and hard plastic, and to remove their shoes, jewelry, and hair clips.
Height and weight
Standing height was measured in stocking feet on a Schorr Height board (Schorr Productions, Olney, Maryland), and body weight was obtained on a portable digital scale (Seca Corporation, Hanover, Maryland). Calibration of the Seca scale was obtained before each testing session using a 5 kg weight. Body weight was recorded to the nearest 0.1 kg; height was recorded to the nearest 0.1 cm.
Dual energy x-ray absorptiometry (DXA)
The criterion estimate of fat-free mass was obtained from whole-body densitometry using dual energy x-ray absorptiometry (Lunar/GE DPX-NT or DPX-IQ, Software version 6.8). All scans were conducted and analyzed by the same technician at each site. The densitometers were calibrated daily against the manufacturer’s standard calibration block. Precision (%CV) of fat-free mass values for the three machines used in the study ranged from 0.6–0.94%.
Participants were positioned according to the standard manufacturer’s instructions for whole body scans, which require them to lie supine with their arms by their sides, palms down, and their knees and ankles held together with Velcro straps. They were instructed to lie still and not talk during the scanning process. Total scan time was approximately 10 minutes. Scans were analyzed using the manual mode, following the manufacturer’s standard procedures for defining regions of interest (ROIs) for each body region.
Bioelectric impedance
Determinations of resistance (R) and reactance (Xc) were made using two BIA instruments, and percent body fat and FFM were estimated from the manufacturers’ equations. The first was the RJL Quantum II, which is a four terminal single frequency (800 mA at 50 kHz) impedance plethysmograph (Valhalla Scientific Model 1990B, Clinton Twp., MI) (RJL). The calibration procedure uses an internal calibration system.
Participants wore light clothing and were barefoot (or removed the shoe and sock from the right foot). The subject reclined in a supine position on a measuring table or a floor mat with arms adjacent to, but not touching the body, palms flat against the table, and legs adjacent to each other but not touching. Four surface self-adhesive spot electrodes were placed on the dorsal surface (top) of the right hand and on the dorsal surface of the right foot. Prior to placement of electrodes the skin was wiped with alcohol at the 4 locations for electrode placement. Resistance (R) and reactance (Xc) values were determined on the right side of the body. Two trials were performed and recorded for each subject. The mean of these two trials was used in the calculations. The time required to complete this procedure was approximately 4–5 minutes.
The second BIA instrument (American Weights and Measures Body-Comp Scale (BCS), Rancho Santa Fe, CA) requires the subject to stand on a scale while grasping handles at approximately chest-height. The current is passed through the body from hand to hand. Accuracy of the scale can be determined by comparing a subject’s weight obtained on the Seca Scale with the weight measured on the BCS. This determination was made on each measurement morning. If the BCS did not provide an accurate weight, it was calibrated according to the manufacturer’s instructions using a 5 kg weight. Because the BCS was a newer instrument and reliability had not been reported previously, we recorded three trials for each subject, and the mean of the three trials was used for statistical analysis.
Statistical analysis
Data were analyzed using the Statistical Analytic Software (SAS Institute, Cary, NC) Descriptive statistics (means and SD) were computed for the total sample and for African-American, Caucasian and Hispanic girls separately. Linear regression analysis was used to determine relationships between the BIA instruments and DXA for FFM and percent body fat. Dependent t-tests were used to compare each of the two BIA instruments to DXA on percent body fat and FFM for the total sample. ANOVA with post-hoc pair-wise comparisons were used to determine possible ethnic differences in body composition. Bland-Altman analysis was conducted to assess the agreement between the two BIA instruments and DXA in determining percent body fat [15].
Results
Demographics
The physical characteristics of the participants are shown in Table 1. Eighty-five percent of the girls were aged 11–13 years. The mean age (± SD) of the total sample was 12.1 ± 1.2 years. Body stature was similar among the three ethnic groups (P>0.05). Body weight and BMI were significantly greater in African-American girls compared to both other groups (P<0.05). There were no significant differences in weight or BMI between Caucasian and Hispanic girls.
Table 1.
Physical characteristics of participants.
| Characteristic | African American (n=51) | Hispanic (n=45) | Cuacasian (n=55) | Total 3 groups (n=151) |
|---|---|---|---|---|
| Age (y) | 12.0 ± 1.1 | 12.3 + 1.1 | 12.1 ± 1.3 | 12.1 ± 1.2 |
| Height (cm) | 155.8 ± 7.7 | 153.8 ± 7.9 | 154.0 ± 8.9 | 154.6 ± 8.2 |
| Weight (kg) | 56.4 ± 18.4* | 52.1 ± 14.9 | 50.0 ± 14.3 | 52.8 ± 16.1 |
| BMI (kg·m−2) | 23.1 ± 6.4* | 21.8 ± 5.3 | 20.6 ± 4.8 | 21.8 ± 5.6 |
Values shown are mean ± SD.
P<0 .05 compared to Caucasian girls.
Stability of BIA instruments
Consistent measurements were obtained on 151 girls. For the RJL instrument, for which two trials were conducted, the differences between trials ranged from 0–5 Ohms, with 94% of the sample less than 3 Ohms. Expressed as a percent of the average resistance, the difference between trials was less than 1%. For the BCS scale, resistance was measured three times, as this is a newer instrument, and reliability across trials had not been previously reported. Differences across the three trials ranged from 0 to 233 Ohms. These differences exceeded 50 Ohms, or 5% of the overall mean, in 44% of the sample, however, the differences were as great as 200 Ohms (21% of the overall mean) in 3% of the sample.
Comparison of BIA to DXA
Linear regression analyses are reported in Table 2. FFM and percent body fat determined by both BIA instruments were highly related to that determined by DXA. For the RJL instrument, the R2 for FFM was 0.91 (SEE=0.03 kg), whereas for the BCS, the R2 was 0.79 (SEE=0.04 kg). The R2 for percent body fat estimated by the RJL was 0.87, SEE=2.8% fat, whereas for the BCS, R2 =0.71, with a SEE of 4.4% fat.
Table 2.
Linear regression analysis of BIA and DXA.
| R2 | SEE | P-value | ||||
|---|---|---|---|---|---|---|
| FFM | Percent body fat | FFM (kg) | Percent body fat | FFM | Percent body fat | |
| RJL vs DXA | 0.91 | 0.87 | 0.03 | 2.76 | <0.0001 | <0.0001 |
| BCS vs DXA | 0.79 | 0.71 | 0.04 | 4.40 | <0.0001 | <0.0001 |
Dependent t-test comparisons of DXA to BIA on percent body fat and FFM for the total sample are reported in Table 3. Compared to DXA, percent body fat was not different for the RJL instrument (P>0,05), whereas the BCS instrument underestimated percent body fat by over 4% (P <0.001). Fat-free mass was overestimated by both the RJL and BCS instruments (P <0.0001), but the absolute difference between the RJL and DXA was only 0.8 kg, whereas the difference between the DCS and DXA was 2.7 kg. Bland-Altman plots of the difference in percent body fat between DXA and each BIA instalment (DXA minus BIA) vs the mean of DXA and BIA are shown in Figs 1 and 2 for the RJL and BCS, respectively. With the RJL instrument, the limits of agreement (±2 SD) ranged from approximately −7% to +7% fat, with the average difference within 1% fat. However, the limits of agreement for the BCS ranged from approximately −7% to +16% fat, with an average difference of 4% fat.
Table 3.
Dependent t-test comparisons of DXA to BIA on percent body fat and FFM for the total sample.
| Measurement | DXA | RJL | BCS | DXA vs RJL | DXA vs BCS | ||
|---|---|---|---|---|---|---|---|
| Mean ± SD (n=163) | t-value | P-value | t-value | P-value | |||
| Percent body fat | 27.6 ± 10.4 | 27.2 ± 11.4 | 23.1 ± 11.2 | 1.36 | 0.176 | 7.96 | <0.001 |
| FFM (kg) | 35.9 ± 7.0 | 36.7 ± 5.5 | 38.5 ± 8.0 | −4.79 | <0.0001 | −7.99 | <0.0001 |
Figure 1.
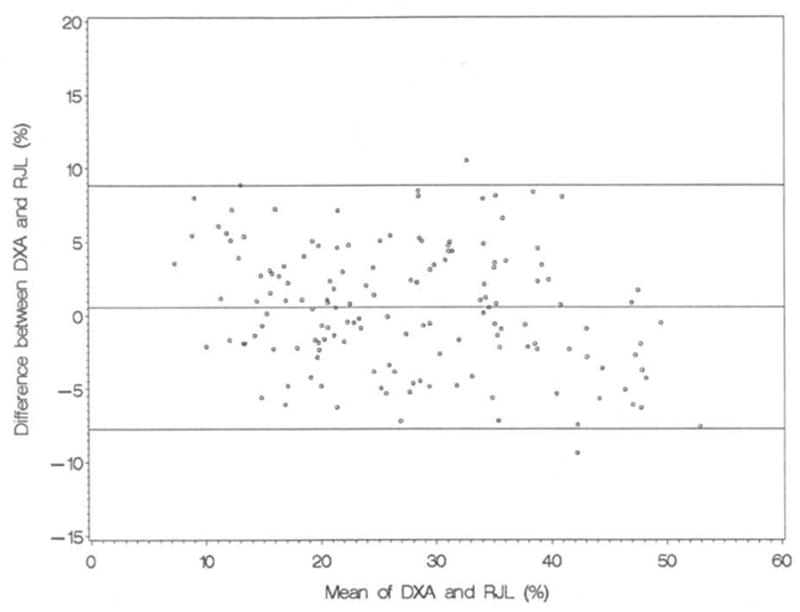
Bland-Altman plot of limits of agreement in percent body fat between DXA and RJL. Parallel lines indicate the mean difference ± 2 SD.
Figure 2.
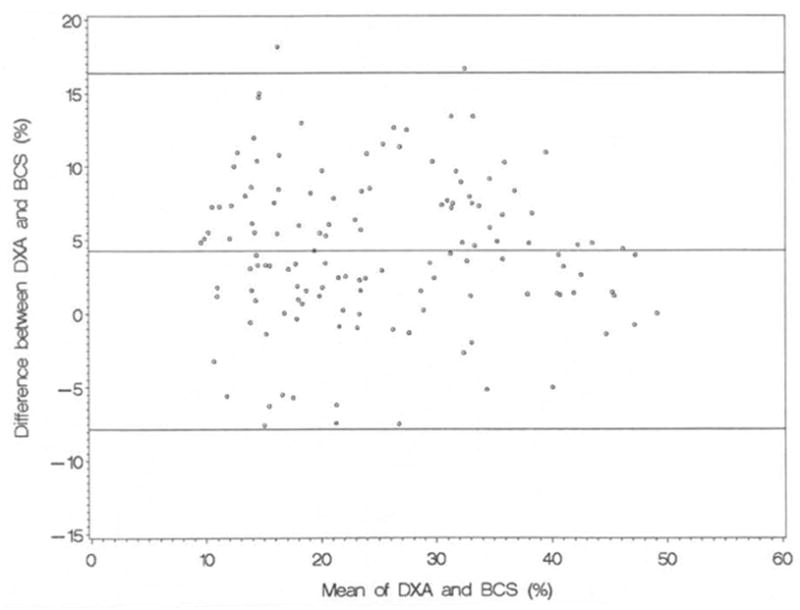
Bland-Altman plot of limits of agreement in percent body fat between DXA and BCS. Parallel lines indicate the mean difference ± 2 SD.
Comparisons by race/ethnicity
Body composition (FFM and %fat) determined by the three techniques is shown for each race/ethnicity in Table 4. Using DXA as the criterion measure, ANOVA with post-hoc pair-wise comparisons showed that African-American girls had significantly greater FFM compared to both Caucasian (P =0.01) and Hispanic (P =0.005) girls. However, neither the RJL or the BCS detected these racial differences in FFM (P >0.05), although the RJL showed a trend (P=0.06) for African-Americans vs Hispanic girls.
Table 4.
Comparison by race of mean ± SD FFM and percent body fat determined by each instrument, shown as P scores
| method | Measure | Mean values by race | ANOVA (P) | African-American vs Caucasian (P) | Hispanic v. Caucasian (P) | Hispanic vs African-American (P) | ||
|---|---|---|---|---|---|---|---|---|
| African-American (n=51) | Hispanic (n=45) | Caucasian (n=55) | ||||||
| DXA | FFM (kg) | 38.3 ± 7.1 | 34.3 ± 6.1 | 34.9 ± 6.8 | 0.007 | 0.010 | 0.692 | 0.005 |
| Percent fat | 27.2 ± 11.2 | 29.5 ± 10.8 | 26.4 ± 9.1 | 0.304 | 0.675 | 0.132 | 0.277 | |
| BCS | FFM (kg) | 39. 5 ± 8.4 | 38.9 ± 7.5 | 37.6 ± 7.7 | 0.473 | 0.231 | 0.447 | 0.747 |
| Percent fat | 24.7 ± 12.5 | 24.5 ± 10.9 | 20.5 ± 9.8 | 0.120 | 0.062 | 0.104 | 0.954 | |
| RJL | FFM (kg) | 38.0 ± 5.5 | 35.9 ± 5.3 | 36.3 ± 5.6 | 0.128 | 0.111 | 0.717 | 0.061 |
| Percent fat | 29.0 ± 12.3 | 28.3 ± 11.6 | 24.6 ± 10.1 | 0.103 | 0.047 | 0.105 | 0.762 | |
There were no differences among the three groups in percent body fat measured by DXA, whereas the RJL instrument produced marginally significant (P=0.047) differences in percent body fat between African-American and Caucasian girls. Percent body fat estimates by the BCS tended to be different (P=0.06) in African-Americans vs Caucasians.
Table 5 shows the overall calculated bias (mean difference and standard error of the difference) in FFM and percent body fat for the total sample and for each of the three ethnic groups. The limits of agreement between DXA and the RJL across the three ethnic groups ranged from −1.6 to 0.3 kg FFM, and from −1.8 to 2.0 % fat, whereas between DXA and the BCS they ranged from −3.8 to −1.2 kg FFM, and from 2.6 to 5.2 %fat.
Table 5.
Mean ± SE differences in FFM and percent body fat by race/ethnicity.
| Comparison | Measure | African-American (A-A) |
Hispanic | Caucasian | Total Sample | ANOVA | A-A vs Caucasian |
Hispanic vs Caucasian |
Hispanic vs A-A |
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SE | Mean ± SE | Mean ± SE | Mean ± SE | P-value | P-value | P-value | P-value | ||
| DXA minus BCS | FFM | −1,2 ± 0.6 | −3.8 ± 0.4 | −2.9 ± 0.5 | −2.5 ± 0.3 | 0.002 | 0.014 | 0256 | <0.001 |
| Percent body fat | 2.6 ± 1.0 | 5.1 ± 0.8 | 5.2 ± 0.8 | 4.2 ± 0.5 | 0.055 | 0.028 | 0.893 | 0.063 | |
| DXA minus RJL | FFM | 0.3 ± 0.4 | −1.5 ± 0.3 | −1.6 ± 0.3 | −0.9 ± 0.2 | <0.001 | <0.001 | 0.927 | <0.001 |
| Percent body fat | −1.8 ± 0.5 | 1.2 ± 0.5 | 2.0 ± 0.6 | 0.5 ± 0.3 | <0.001 | <0.001 | 0.340 | <0.001 | |
ANOVA with pair-wise post-hoc comparisons showed no differences between Hispanic and Caucasian girls for either FFM or percent body fat when comparing DXA to either BIA instrument (P>0.05). However, significant differences between African-Americans and Caucasians, were found for both FFM and percent body fat comparisons between DXA and both the RJL and BCS instruments (P<0.028 to 0.001). Also, significant differences between African-American and Hispanic girls were found for FFM comparisons between DXA and both instruments, whereas for percent body fat only the comparison between DXA and the RJL instrument was significant (P <0.001). The mean difference in FFM for the RJL (DXA minus RJL) was smallest (0.3 kg) in African-American girls and similar (approximately 1.5 kg) in Caucasian and Hispanic girls. The mean difference in percent body fat estimated by the RJL was similar across the three groups. For the BCS instrument, the mean difference in FFM was smallest in African-Americans, and largest in Hispanics. The mean difference in percent body fat was smallest in African-Americans (2.6%) and over twice as large in both Caucasian and Hispanic girls.
Discussion
BIA is a simple, relatively inexpensive technique for estimating body composition, which unlike DXA, emits no radiation to the subject. Because it requires minimal technical training for assessment, and only a few minutes for participant measurement and analysis, it has potential for use in a variety of settings with large numbers of individuals. The results of the present study indicate that the RJL Quantum II instrument compared more favorably with DXA than did the American Weights Body Composition Scale. Furthermore, the resistance measures showed more stability across trials when measured with the RJL analyzer compared to the BCS. In the total sample, fat-free mass derived from the RJL instrument differed from DXA by only 0.8 kg, whereas FFM estimated by the BCS was 2.7 kg higher than that determined by DXA.
A possible explanation for the lower accuracy of the BCS is that within the manufacturer’s equations used to predict FFM and fat mass, resistance (ohms) has limited influence; other variables, including height and weight are more important determinants of FFM and fat mass. The lower accuracy of the BCS may also be related to the degree of separation of the arms from the trunk while holding the handles during measurement with the BCS. Schell & Gross [16] have shown that resistance increases as the arms are more abducted from the trunk. Since participants varied tremendously in body size and weight, smaller girls may have had to abduct their arms more than larger girls to grasp the handles. This could have resulted in artificially increasing their resistance scores, which in turn would lead to underestimation of FFM and over-estimation of body fat.
Although the resistance measures are not directly comparable between the two analyzers, percent body fat derived from the two instruments correlated highly (r = 0.89, P <0.0001). The differences between the BCS and RJL may be due, at least in part, to the electrical conduction path of the two instruments. The RJL is a tetrapolar device and thus measures resistance and reactance through both the upper and lower body, whereas with the BCS the conduction path is from hand to hand. Variations in cross-sectional area of body segments affect resistance, which is larger for body parts with smaller circumferences [17]; thus, assumptions of the variability in the cross-sectional area of body segments may not be met in children of different ethnicities or those with a wide range of BMI.
In general, our results are consistent with those reported in several other studies [1, 3, 7, 10, 12]. First, correlation or regression coefficients of the relationships between BIA and DXA in adults and children in other studies were similar to those in the present study [3, 7–10, 12]. Second, compared to DXA, BIA tended to underestimate percent body fat and overestimate FFM [3, 7, 14]. However, in obese children of similar age, the differences in percent body fat between DXA and BIA were significant for boys, but not for girls [7].
Among the three racial/ethnic groups, the mean differences in FFM and percent body fat between DXA and the other two devices were not significant for Caucasians vs. Hispanics. However, significant differences were observed between African-American and Hispanic girls, and between African-American and Caucasians for both the RJL and BCS. In those few studies that directly compared African-American and Caucasian children or adolescents [12, 13, 18], prediction equations for FFM and/or percent body fat were not generalizable to both groups. As we also found, the mean differences for percent body fat and FFM were significant for African-Americans vs Caucasians [13]. Within each ethnic group as well as for the total sample, compared to DXA, the RJL instrument more closely estimated FFM and percent body fat than did the BCS. The largest errors in estimates of percent body fat with the BCS instrument were seen in Caucasian and Hispanic girls, whereas for the RJL instrument, the error was relatively similar among the three groups, and smaller overall compared to the BCS.
In conclusion, these data indicate that BIA provides reasonable estimates of body composition in female adolescents. However, estimates of FFM and percent body fat by the RJL and BCS instruments cannot be generalized across the three racial/ethnic groups reported here; separate equations should be developed for that purpose. BIA is a useful and appropriate technique for assessing body composition in adolescent girls because of its low cost and reduced training requirements compared to DXA. For the total sample, as well as the three racial/ethnic groups reported here, the RJL impedance analyzer provided more accurate and stable estimates of FFM and percent body fat than the BCS.
Footnotes
This study was funded by NIH - NHLBI HL66856.
References
- 1.Houtkooper LB, Lohman TG, Going SB, et al. Validity of bioelectric impedance for body composition assessment in children. J Appl Physiol. 1989;66(2):814–21. doi: 10.1152/jappl.1989.66.2.814. [DOI] [PubMed] [Google Scholar]
- 2.Andreoli A, Melchiorri G, De Lorenzo A, et al. Bioelectrical impedance measures in different position and vs dual-energy X-ray absorptiometry (DXA) J Sports Med Phys Fitness. 2002;42(2):186–9. [PubMed] [Google Scholar]
- 3.Bolanowski M, Nilsson BE. Assessment of human body composition using dual-energy x-ray absorptiometry and bioelectrical impedance analysis. Med Sci Monit. 2001;7(5):1029–33. [PubMed] [Google Scholar]
- 4.Houtkooper LB, Going SB, Sproul J, et al. Comparison of methods for assessing body-composition changes over 1 y in postmenopausal women. Am J Clin Nutr. 2000;72(2):401–6. doi: 10.1093/ajcn/72.2.401. [DOI] [PubMed] [Google Scholar]
- 5.Malavolti M, Mussi C, Poli M, et al. Cross-calibration of eight-polar bioelectrica! impedance analysis versus dual-energy X-ray absorptiometry for the assessment of total and appendicular body composition in healthy subjects aged 21–82 years. Ann Hum Biol. 2003;30(4):380–91. doi: 10.1080/0301446031000095211. [DOI] [PubMed] [Google Scholar]
- 6.Bray GA, DeLany JP, Volaufova J, et al. Prediction of body fat in 12-y-old African American and white children: evaluation of methods. Am J Clin Nutr. 2002;76(5):980–90. doi: 10.1093/ajcn/76.5.980. [DOI] [PubMed] [Google Scholar]
- 7.Eisenkolbl J, Kartasurya M, Widhalm K. Underestimation of percentage fat mass measured by bioelectrical impedance analysis compared to dual energy X-ray absorptiometry method in obese children. Eur J Clin Nutr. 2001;55(6):423–9. doi: 10.1038/sj.ejcn.1601184. [DOI] [PubMed] [Google Scholar]
- 8.Ellis KJ. Measuring body fatness in children and young adults: comparison of bioelectric impedance analysis, total body electrical conductivity, and dual-energy X-ray absorptiometry. Int J Obes Relat Metab Disord. 1996;20(9):866–73. [PubMed] [Google Scholar]
- 9.Fuller NJ, Fewtrell MS, Dewit O, et al. Segmental bioelectrical impedance analysis in children aged 8–12 y: 2. The assessment of regional body composition and muscle mass. Int J Obes Relat Metab Disord. 2002;26(5):692–700. doi: 10.1038/sj.ijo.0801989. [DOI] [PubMed] [Google Scholar]
- 10.Houtkooper LB, Going SB, Lohman TG, et al. Bioelectrical impedance estimation of fat-free body mass in children and youth: a cross-validation study. J Appl Physiol. 1992;72(1):366–73. doi: 10.1152/jappl.1992.72.1.366. [DOI] [PubMed] [Google Scholar]
- 11.Lohman TG, Caballero B, Himes JH, et al. Body composition assessment in American Indian children. Am J Clin Nutr. 1999;69(4 Suppl):764S–766S. doi: 10.1093/ajcn/69.4.764S. [DOI] [PubMed] [Google Scholar]
- 12.Morrison JA, Guo SS, Specker B, et al. Assessing the body composition of 6–17-year-old Black and White girls in field studies. Am J Hum Biol. 2001;13(2):249–54. doi: 10.1002/1520-6300(200102/03)13:2<249::AID-AJHB1035>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 13.Sun SS, Chumlea WC, Heymsfield SB, et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr. 2003;77(2):331–40. doi: 10.1093/ajcn/77.2.331. [DOI] [PubMed] [Google Scholar]
- 14.Treuth MS, Butte NF, Wong WW, et al. Body composition in prepubertal girls: comparison of six methods. Int J Obes Relat Metab Disord. 2001;25(9):1352–9. doi: 10.1038/sj.ijo.0801731. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10. [PubMed] [Google Scholar]
- 16.Schell B, Gross R. The reliaility of bioelectrical impedance measurements in the assessment of body composition in healthy adults. Nutr Rep Int. 2000;36:449–59. [Google Scholar]
- 17.Baumgartner RN, Chumlea WC, Roche AF. Estimation of body composition from bioelectric impedance of body segments. Am J Clin Nutr. 1989;50(2):221–6. doi: 10.1093/ajcn/50.2.221. [DOI] [PubMed] [Google Scholar]
- 18.Wong WW, Stuff JE, Butte NF, et al. Estimation of body fat in Caucasian and African-American girls: total-body electrical conductivity methodology versus a four-component model. Int J Obes Relat Metab Disord. 2000;24(9):1200–1206. doi: 10.1038/sj.ijo.0801369. [DOI] [PubMed] [Google Scholar]


