INTRODUCTION
Kuhn1 used the term ‘crisis’ for the chaotic situation provoked by an unresolved anomaly (i.e. a finding not explainable by a prevailing scientific paradigm). As a crisis evolves, the rules by which the old paradigm are applied to new findings become increasingly blurred. Kuhn's description of a paradigm in crisis1 applies accurately to recent discussions of the cardiovascular risks of the coxibs.2,3 Recognition of paradigm crises is problematic in all scientific fields; however, in medical science, failure to recognize and resolve an ongoing crisis can put lives at risk by delaying a necessary paradigm shift.
There had been a ‘working paradigm’, reviewed by Antman et al.2 in a paper that aptly presents the current crisis. Their account of the ‘tsunami of events’ following withdrawal of rofecoxib in 2004 suggests an ongoing paradigm crisis. By the early 1990s, the prevailing paradigm involved ‘the recognition that there are two different cyclooxygenases (COXs), which ‘led to the straightforward view that COX-2 is responsible for the adverse pro-inflammatory effects of prostanoids and that non-specific COX inhibitors cause bleeding by inhibiting COX-1 in platelets’.2 The paradigm encouraged development of COX-2 selective inhibitors to isolate an assumed anti-inflammatory mechanism of aspirin from the mechanism causing haemorrhage.
Which of the direct and indirect effects of long-term aspirin use is responsible for cardioprotection remains fundamentally a matter of speculation. There is no reliable proof that the mechanisms under most intense discussion are responsible for prevention of coronary events with regular use. The ‘working paradigm’2 has been overtaken by a paradigm crisis. The mechanism of benefit could be an unexpected effect of aspirin or it could be hidden within one of the known harmful effects of aspirin.
A COMPETING PARADIGM
The hazard of gastrointestinal bleeding obscured the possibility that bleeding might have a cardiovascular benefit. In 1982, I proposed cumulative iron loss from occult bleeding as one mechanism by which long-term use of aspirin protects against heart disease.4 The suggestion is a corollary to the ‘iron hypothesis’ that proposed a primary cardioprotective effect of sustained iron depletion.5-8
Cumulative iron losses from occult bleeding associated with daily use of aspirin can have the same impact on iron storage levels as typical cumulative menstrual iron losses. The traditional upper limit of normal for menstrual bleeding is 60 mL/month. Normal menstrual blood loss is therefore <0.72 L/year. A modestly increased blood loss of 1 mL/day with aspirin use, though imperceptible to the patient, would cause a cumulative loss of 0.37 L/year, well within the range of typical menstrual losses. Whole blood contains approximately 0.5 g/L of elemental iron. Cumulative loss of a litre of blood over the period of a year or two would be expected to cause the loss of a significant proportion of the 1.0 g load of stored iron of a typical middle-aged male.
Use of aspirin was associated with lower serum ferritin levels in the Danish DAN-MONICA 10 survey,9 in a group of postmenopausal women who had participated in the Nurses' Health Study,10 and in elderly participants in the Framingham Heart Study.11 A smaller study on the interactions of Helicobacter pylori and aspirin use in elderly subjects reported that low-dose aspirin use was not associated with diminished ferritin;12 however, subjects with evidence of iron deficiency were excluded, eliminating an unknown proportion of iron depleted aspirin users and potentially biasing the results against finding an effect of aspirin use.
Regular, long-term use of aspirin is a weak protective factor in terms of absolute risk. ISIS-2 reported a small survival benefit in patients with suspected acute myocardial infarction randomized to receive aspirin therapy for one month.13 In absolute terms, approximately 2.6% fewer deaths were recorded in the first 35 days among those allocated to oral aspirin. Iron loss from a brief period of aspirin use would not substantially lower typical iron storage loads. However, this does not rule out a primary or secondary cardioprotective effect of iron losses from prolonged exposure to aspirin. The efficacy of cardioprotective aspirin regimens may be lower than expected because sustained iron depletion is rarely achieved. The degree of iron depletion seen in practice with regular aspirin use is highly variable.9-12 Iron loss is not a goal of conventional cardioprotective aspirin regimens.
In light of the risks of coxibs, the global effect of regular aspirin use might derive from the net impact of competing mechanisms: an antithrombotic action in coronary arteries, a cardioprotective effect of iron loss, and an opposing cardiovascular risk-enhancing transformation in association with long-term inhibition of COX-2. There remains uncertainty over the optimal dosage of aspirin for cardioprotection. Differing dose dependencies of competing effects could result in a complex dose dependence for the net cardioprotective effect.
Drugs such as the coxibs, which share some of the effects of aspirin, offer the opportunity for new insight into the mechanism(s) involved in cardioprotection. Future trials on selective COX-2 inhibitors may help to dissect competing mechanisms of native aspirin. A prospective trial of the primary cardioprotective effects of aspirin, a COX-2 inhibitor, placebo, or sustained iron depletion would be useful. Absent chronic bleeding, aspirin may be less cardioprotective, indeed, the possibility of an underlying disease-promoting action and cardiovascular risk transformation of long-term aspirin use is raised by emerging findings on COX-2 inhibitors.
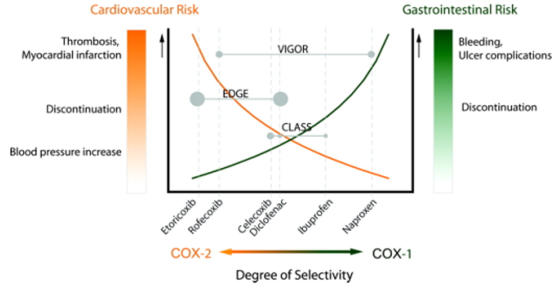
A recent scientific statement from the American Heart Association demonstrates the limits of the prevailing paradigm on the effects of COX inhibition on cardiovascular risk.14 In particular, the differential effects of varying COX-1/COX-2 selectivity on cardiovascular and gastrointestinal risks was displayed graphically (Figure 1). The Figure is an interpretation based largely on three trials: VIGOR (Vioxx Gastrointestinal Outcomes Research),15 EDGE (Etoricoxib versus Diclofenac sodium Gastrointestinal tolerability and Effectiveness trial, part of the larger MEDAL program),16 and CLASS (Celecoxib Long-Term Arthritis Safety Study).17 A conclusion that may be drawn from these trials is that cardiovascular risk is inversely proportional to gastrointestinal risk. Given the striking correlation shown in Figure 1, it is plausible that cardioprotection may be dependent on the degree of gastrointestinal risk. A potential causal relationship between cardiovascular and gastrointestinal risks is not addressed by the AHA scientific statement. The authors specifically endorse the use of proton pump inhibitors to decrease the possibility of bleeding.14 The fundamental questions raised by the present essay are: is cardiovascular protection by long-term aspirin use dependent on its gastrointestinal hazard? And does engineering out the gastrointestinal bleeding side effect of COX inhibition cancel the cardiac benefit of long-term aspirin use?
Figure 1.
Implications of the relative degrees of selectivity of COX inhibition for cardiovascular and gastrointestinal risks. Reproduced from Antman et al.14 Reprinted with permission from Circulation. [In colour online.]
IMPACT OF ASPIRIN-INDUCED IRON DEFICIENCY ON THE OTHER EFFECTS OF ASPIRIN
Lowering stored iron level by long-term aspirin use could modify the known acute effects of aspirin. A key component of anti-inflammatory and antioxidant effects of iron depletion appears to be restriction of the availability of redox-active iron in vivo.8 It has been recently demonstrated that the low molecular weight iron (LMWI) concentration within human atherosclerotic plaques is directly proportional to storage iron level as measured by serum ferritin.18 Effects of iron depletion/deficiency on iron dependent enzymes involved in inflammation and antioxidant defence have also been proposed as a general mechanism by which iron depletion could protect against ischemic heart disease.6 Anti-inflammatory effects after aspirin-induced iron deficiency may differ qualitatively and quantitatively from the initial acute effects of aspirin exposure.
MAGNITUDE OF IRON REDUCTION IN THE FEAST TRIAL VERSUS THE EFFECTS OF REGULAR ASPIRIN USE
The possibility that progressively increasing benefit is associated with greater levels of iron loss in long-term use must be assessed in future experiments. Previous studies on disease prevention by aspirin have not included assessments of the impact of treatment on iron levels in the individual participants and therefore do not address the possibility that those who experience the greatest iron losses could have the greatest degree of protection.
The findings of a first randomized trial of mild iron reduction therapy in elderly patients with established peripheral vascular disease (PAD) have been recently published.19 The FeAST trial provides indirect but strong support for the possibility that the cumulative amount of aspirin-induced iron losses can have a cardioprotective effect. The trial assessed the effect of mild iron reduction therapy in secondary prevention of cardiovascular disease. It was therefore not a fully valid test of primary prevention as postulated by the iron hypothesis. Iron deficiency or complete iron depletion was carefully avoided, as stipulated by the study design. No overall cardiovascular benefit was found. Nonetheless, the youngest age quartile randomized to iron reduction had a 53% reduction in total mortality (P=0.019), the primary endpoint, and a 57% reduction in death plus nonfatal myocardial infarction and stroke (P<0.001), the secondary endpoint, compared to control patients.
The mortality benefit in the youngest quartile was seen in association with a phlebotomy-induced reduction in serum ferritin from a mean entry value of 122.5 ng/mL to 79.7 ng/mL at the end of the study, a 35% decrease. The decrease in serum ferritin in association with regular aspirin use in observational studies is of the same order of magnitude achieved in the FeAST subjects. In the Framingham Study,11 mean serum ferritin was lower in association with regular aspirin use by 21-50%, depending on the state of health of the subjects and the amount of aspirin consumed. In an earlier study of a Danish population by Milman et al.,9 aspirin users were found to have serum ferritin values 20% lower than non-users. In the Nurses' Health Study,10 postmenopausal women who used aspirin 15-30 times per month had a 19% lower mean serum ferritin value than non-users. The fact that the magnitude of serum ferritin lowering observed with aspirin use is of the same order of magnitude as the phlebotomy induced iron reduction in the FeAST trial indirectly supports iron loss as a mechanism of cardioprotection by aspirin. Iron reduction of this order of magnitude was shown in the FeAST trial to lower mortality by more than 50% in younger patients with PAD. Taken together, these findings suggest that storage iron reduction is a sufficient mechanism for the demonstrated benefits of aspirin use in patients with PAD.20
CONCLUDING COMMENT
The possibility that iron loss may have a beneficial effect on cardiovascular risk and also treat inflammation should be fully explored. Without appropriate measurements of the impact of aspirin use on iron status in clinical trials, a pattern of greater benefit among subjects with the greatest degree of iron loss may have been overlooked. The impact of non-selective non-steroidal anti-inflammatory drugs and coxibs on iron balance should also be assessed. The findings of the FeAST trial of secondary prevention of cardiovascular disease by iron reduction therapy impart new urgency to future studies that address the role of sustained iron depletion in protection against cardiovascular diseases, as well as cancer and other disorders.8 It is clear that long-term, regular aspirin use can lower storage iron level, in some subjects by a substantial degree. It cannot be simply concluded, relying on application of the assumptions of an earlier paradigm and without new studies, that this known effect has no impact on cardiovascular risk.
Competing interests None declared.
Acknowledgments I thank Dr Stuart D Katz for his useful suggestions.
References
- 1.Kuhn TS. The Structure of Scientific Revolutions. 2nd edition. Chicago: University of Chicago Press, 1970
- 2.Antman EM, DeMets D, Loscalzo J. Cyclooxygenase inhibition and cardiovascular risk. Circulation 2005;112: 759-70 [DOI] [PubMed] [Google Scholar]
- 3.Topol EJ. Arthritis medicines and cardiovascular events—‘House of Coxibs’. JAMA 2005;293: 366-8 [DOI] [PubMed] [Google Scholar]
- 4.Sullivan JL. Iron, aspirin, and heart disease risk [letter]. JAMA 1982;247: 751. [PubMed] [Google Scholar]
- 5.Sullivan JL. Iron and the sex difference in heart disease risk. Lancet 1981;1: 1293-4 [DOI] [PubMed] [Google Scholar]
- 6.Sullivan JL. The iron paradigm of ischemic heart disease. Am Heart J 1989;117: 1177-88 [DOI] [PubMed] [Google Scholar]
- 7.Sullivan JL. Stored Iron and Vascular Reactivity. Arterioscler Thromb Vasc Biol 2005;25: 1532-5 [DOI] [PubMed] [Google Scholar]
- 8.Sullivan J. Is stored iron safe? J Lab Clin Med 2004;144: 280-4 [DOI] [PubMed] [Google Scholar]
- 9.Milman N, Ovesen L, Byg K, Graudal N. Iron status in Danes updated 1994. I: prevalence of iron deficiency and iron overload in 1332 men aged 40-70 years. Influence Of blood donation, alcohol intake, and iron supplementation. Ann Hematol 1999;78: 393-400 [DOI] [PubMed] [Google Scholar]
- 10.Liu JM, Hankinson SE, Stampfer MJ, Rifai N, Willett WC, Ma J. Body iron stores and their determinants in healthy postmenopausal US women. Am J Clin Nutr 2003;78: 1160-7 [DOI] [PubMed] [Google Scholar]
- 11.Fleming DJ, Jacques PF, Massaro JM, D'Agostino RB Sr, Wilson PW, Wood RJ. Aspirin intake and the use of serum ferritin as a measure of iron status. Am J Clin Nutr 2001;74: 219-26 [DOI] [PubMed] [Google Scholar]
- 12.Kaffes A, Cullen J, Mitchell H, Katelaris PH. Effect of Helicobacter pylori infection and low-dose aspirin use on iron stores in the elderly. J Gastroenterol Hepatol 2003;18: 1024-8 [DOI] [PubMed] [Google Scholar]
- 13.Baigent C, Collins R, Appleby P, Parish S, Sleight P, Peto R. ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomized comparison of intravenous streptokinase, oral aspirin, both, or neither. BMJ 1998;316: 1337-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of Nonsteroidal antiinflammatory drugs. An update for clinicians. A scientific statement from the American Heart Association. Circulation 2007;115:[DOI: 10.1161/CIRCULATIONAHA.106.181424] [DOI] [PubMed]
- 15.Dobson R. NEJM ‘failed its readers’ by delay in publishing its concerns about VIGOR trial. BMJ 2006;333: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cannon CP, Curtis SP, Bolognese JA, Laine L. Clinical trial design and patient demographics of the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) study program: cardiovascular outcomes with etoricoxib versus diclofenac in patients with osteoarthritis and rheumatoid arthritis. Am Heart J 2006;152: 237-45 [DOI] [PubMed] [Google Scholar]
- 17.Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: A randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA 2000;284: 1247-55 [DOI] [PubMed] [Google Scholar]
- 18.Lapenna D, Pierdomenico SD, Ciofani G, et al. Association of body iron stores with low molecular weight iron and oxidant damage of human atherosclerotic plaques. Free Radical Biol Med 2007;42: 492-8 [DOI] [PubMed] [Google Scholar]
- 19.Zacharski LR, Chow BK, Howes PS, et al. Reduction of iron stores and cardiovascular outcomes in patients with peripheral arterial disease: a randomized controlled trial. JAMA 2007;297: 603-10 [DOI] [PubMed] [Google Scholar]
- 20.CLIPS Group. Prevention of serious vascular events by aspirin amongst patients with peripheral arterial disease: randomized, double-blind trial. J Intern Med 2007;261: 276-84 [DOI] [PubMed] [Google Scholar]