Abstract
The objective of this study was to investigate the relationship between peripheral blood CD4+ T cell subsets and routine viro-immunological markers in vertically HIV-1-infected children undergoing highly active antiretroviral therapy (HAART). CD4+ and CD8+ T cell subsets were examined by three-colour flow cytometry. Plasma viraemia was quantified by a standardized molecular assay. A negative correlation between the %CD4+ T cells and both viral load and the %CD8+ T cells was observed. A strong positive correlation between the %CD4 T cells and naïve, CD38+ and non-activated CD4+ T cell subsets was found, whereas the %CD4 T cells correlated negatively with the numbers of memory, activated and memory-activated CD4+ T cell subsets. Elevated percentages of CD8 T cells were associated with increased memory and CD4+ CD62L-T cell subsets, whereas the naïve and CD4+ HLA-DRCD38+ subsets negatively correlated with the CD8%. Co-expression of CD62L on memory CD4+ cells and high expression of HLA-DR (but not of CD38) were associated with high viral load. No association between viral load and naïve CD4+ T cells was observed. Specific CD4+ T cell subsets may be more informative than routine surrogate markers in defining the evolution of HIV infection and immune reconstitution in children.
Keywords: CD4 subsets, children, highly active antiretroviral therapy, HIV immune reconstitution, surrogate markers
Introduction
HIV-1 infection causes both a decrease in CD4+ T cell numbers and activation of the immune system [1,2]. In adults, immune activation correlates with an increase in CD4+ T cells co-expressing the activation markers CD38 and HLA-DR [1,2]. However, in children the CD38+ marker is a maturation, rather than an activation marker since 75% of all CD4+ T cells and 50% of CD8+ T cells normally co-express CD38 in children [3]. A decrease in immature T cells over the years is accompanied by decreasing percentages of CD38 cells to normal adult values of around 30% [4–7]. This fact may contribute to misinterpretation of this marker in children, since these cells can be either immature and/or activated [4,8]. An increased expression of HLA-DR on T cells has also been proposed as a progression marker of HIV-1 infection in both adults [9] and children [10].
Other T cells, such as naïve and memory CD4+ and CD8+ T cell subsets, have been used in HIV-1-infected adults for prognostic purposes. Activation of the immune system by HIV-1 infection enhances the maturation of naïve T cells into memory T cells (CD4+ CD45RO+) that are a main target for viral infection [11–13]. Cells that escape from death circulate in peripheral blood with a CD45RO+ phenotype. In neonates, more than 80% of T cells are CD4+ CD45RA+ naïve cells, while less than 20% are memory T cells [14,15]. Naïve cells are continuously recycling between peripheral blood and secondary lymphoid organs, and this traffic is highly dependent on the expression of l-selectin (CD62L) [16].
Highly active antiretroviral therapy (HAART) has had a tremendous impact on the treatment of HIV infection [17,18], resulting in an important suppression of viral load (VL) and recovery of CD4 T cell numbers, with a dramatic reduction in the occurrence of opportunistic infections [18]. However, a complete recovery of CD4 T cell counts and functionality is not achieved [19–21], contrary to that expected after halting the destruction of CD4 cells. In turn, HAART in adults induces a reduction in the activation status of memory cells as detected by activation markers [22,23], an increase in memory T cell numbers which is followed later by a gradual and sustained increase in naïve T cell numbers [19–21].
In children, however, the effects of HAART on naïve and memory T cells have not been well studied. Therefore, the main goal of our study was to determine the relationship between the most commonly used immunological (CD4+ and CD8+ T cells) and virological (VL) markers to monitor HIV-1 infection [24,25] and memory, naïve and activated CD4+ T cell subsets in children undergoing HAART therapy.
Materials and methods
Patients and control subjects
Thirty-nine infants born to HIV-1-infected mothers were recruited in a cross-sectional study between July and September 1999 at the Paediatric Departments of the University General Hospital ‘Gregorio Marañón’ in Madrid and ‘Virgen del Rocío’ Hospital in Seville, Spain. All infants were diagnosed as HIV-1-infected on the basis of positive results in both DNA PCR and virus culture assays, as described previously [26], and all were treated with potent antiretroviral therapy. Clinical classification was based on the 1994 revised guidelines of the Center for Disease Control and Prevention (CDCP) [27]. The study was conducted according to the Declaration of Helsinki and approved by the Ethical Committee. Drugs were prescribed by the treating physician according to CDCP guidelines [28] upon obtaining written informed consent from parents or legal guardians.
Quantification of the percentages of CD3+ CD4+ and CD3+ CD8+ T cells in whole blood
The technique employed for quantifying the percentages of CD4+ and CD8+ T cells in peripheral blood was the TRUCOUNTTM (Becton-Dickinson Immunocytometry Systems, San José, CA, USA) in whole blood, whereby lymphocytes were selected by means of an SSC gate against anti-CD45 [29], following the manufacturer's instructions. The acquisition was carried out in a FACSCalibur cytometer (Becton-Dickinson) using the CELLQuest (Becton-Dickinson) acquisition program immediately after cell staining. TRUCOUNTTM Control Beads were used routinely as a quality control.
Quantification of CD4+ T cell subsets
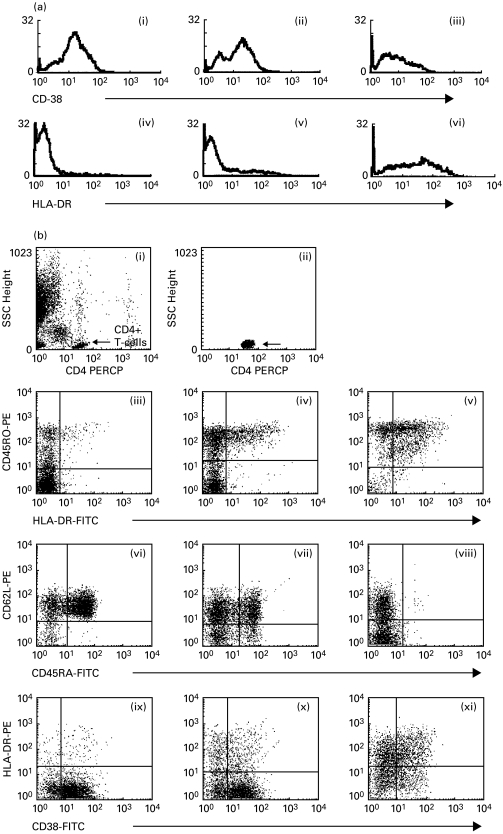
For the analysis of CD4+ T cell subsets, we used a combination of the monoclonal antibodies shown in Table 1. T cell subsets were analysed by three-colour multi-parametric flow cytometry in whole blood, lysed and washed [30]. Data acquisition was performed in a FACScan (Becton-Dickinson) cytometer using the Lysis II acquisition program (Becton-Dickinson) within 2 h of cell staining. The optimal parameters for acquisition (detector sensitivity, detector amplification and compensation) were determined using Calibrite as a reagent (Becton-Dickinson) and the AutoComp (Becton-Dickinson) program periodically. Five thousand events were compiled using a collection gate for CD4+ T-lymphocytes. The gate was defined using the low SSC and high expression of CD4 [29]. Data were analysed using the Lysis II analysis program (Becton-Dickinson). Appropriate isotypic controls (IgG1-FITC; IgG1-PE) were used to evaluate non-specific staining, which was deducted from the remaining results. We measured HLA-DR and CD38 relative fluorescence intensities (RFI) as the mean RFI using single-parameter histograms with no cursor sets. Figure 1 shows a typical FACS plot illustrating the T cell subsets.
Table 1.
Monoclonal antibodies used for the phenotypic characterization of CD4+ T cell subsets
| Tube | FITC | PE | PerCP | Analysed subsets |
|---|---|---|---|---|
| 1 | Anti-IgG1 | Anti-IgG1 | anti-CD4 | CD4+ T cells |
| 2 | Anti-HLA-DR | anti-CD45RO | anti-CD4 | Memory/activated CD4 |
| 3 | Anti-CD45RA | anti-CD62L | anti-CD4 | Naïve CD4 |
| 4 | Anti-CD38 | Anti-HLA-DR | anti-CD4 | CD4 activated |
Naïve cells were defined as CD62L+ and CD45RA+ bright cells (CD4+ CD45RAhi/CD62L+). Memory CD4+ T cells were defined as CD4+ CD45RO+ or CD4+ CD45RA. Activated CD4+ T cells were defined as CD4+ HLA-DR+ and CD4+ HLA-DR+ CD38+ 0. FITC: fluorescein-isotyocianate; PE: phycoeritrin; PerCP: peridinin chloropyll protein.
Fig. 1.
(a) RFI of CD38 and HLA-DR CD4+ T cells. (i, iv) Asymptomatic patient. (ii, v) Mild-symptomatic patient. (iii, vi) Patient in category (iii). RFI of activation markers, especially HLA-DR, were strongly elevated in symptomatic patients, whereas the RFI of CD38 was not. (b) Analysis of CD4+ T cell subsets. (i, ii) Gating of CD4+ T cells. The acquisition gate was defined using low SSC and high expression of CD4 to exclude monocytes. (iii, vi, ix) Asymptomatic patient. (iv, vii, x) Mild-symptomatic patient. (v, viii, xi) Patient in clinical category (iii). (iii, iv, v) Analysis of memory and memory-activated CD4+ T cells. In HIV-infected children we found a progressive increase in memory and memory-activated T cell numbers correlating with the progression of the immunodeficiency. (iii, iv, v) Analysis of naive CD4+ T cells. Naive cells were defined as cells with bright expression of CD45RA and positive for CD62-L. In HIV-infected children we found a progressive decrease in naive cell numbers and an increase in CD62L cells correlating with the progression of the immunodeficiency. (vi, vii, viii) Analysis of activated CD4+ T cells. In HIV+ children we found elevated levels of CD4+ CD38+ HLA-DR+ cells. Most cells in asymptomatic patients expressed CD38 at low intensities but these cells did not co-express HLA-DR. These cells are mostly naive cells.
Quantitative HIV-1 RNA assay
Blood samples were collected in EDTA tubes, separated within 4 h and plasma stored at −70°C. HIV-1 RNA was measured in 200 µl plasma using a quantitative reverse transcriptase PCR (RT-PCR) assay (Amplicor Monitor, Roche Diagnostic Systems).
Statistics
In all analyses, VL was transformed to log10-scale in order to normalize the distribution. The relationship between variables was investigated using a partial correlation coefficient, which describes the linear relationship between two variables while controlling for the effects of age. Values of both range between −1 (a perfect negative relationship) and +1 (a perfect positive relationship). A value of 0 indicates no linear relationship.
Differences in characteristics between infants were analysed using multiple linear regression analysis. Factor variables used to divide the population into groups were 25% CD4+ T cells, and 4·5 log10 VL (copies/ml), including the effects of age as covariates. Since the %CD4+ and CD8+ changes with age in children, a multiple linear regression analysis was performed for all children collectively and age-matched to compensate for differences among groups. We confirmed that virtually all the CD4+ CD45RA+ CD62L+ T cells expressed CD38, as reported previously [31]. The subset of CD4+ CD45RO+ CD38+ T cells was calculated by subtracting the subset CD4+ CD45RA+ CD62L+ from the CD4+ CD38+ subset.
Results
Demographics and clinical characteristics of the HIV-1-infected children
Clinical, immunological and virological characteristics, as well as the antiretroviral therapy regimens of the 39 vertically HIV-1-infected children are shown in Table 2. In this paediatric population, the %CD4+ T cells correlated negatively with both log10 VL (r = − 0·39; P < 0·05), and %CD8+ T cells (r = − 0·67; P < 0·001).
Table 2.
Immunological and virological characteristics of the children included in the study
| Characteristics | Values |
|---|---|
| No. HIV-1 children | 39 |
| Age (years)* | 7·6 ± 0·54 (3·0; 15·6) |
| Clinical category | |
| A | 10 (25·6%) |
| B | 9 (23·1%) |
| C | 20 (51·3%) |
| Lymphocyte subsets | |
| % CD4+ T* | 25·9 ± 1·90 (2·0; 46·2) |
| % CD8+ T* | 47·3 ± 2·21 (30·4; 79·4) |
| CD4+ T/mm3* | 952 ± 146 (35; 3779) |
| CD8+ T/mm3* | 1455 ± 133 (267; 4276) |
| Viral load (VL) | |
| log10 VL (log10 copies/ml)* | 3·89 ± 0·20 (1·30; 5·80) |
| Antiretroviral treatment | |
| 2 NA + indinavir | 3 (7,69%) |
| 2 NA + nelfinavir | 19 (48,72%) |
| 2 NA + saquinavir | 3 (7,69%) |
| 2 NA + amprenavir | 2 (5,13%) |
| 2 NA + ritonavir | 1 (2,56%) |
| 2 NA + nelfinavir + ritonavir | 1 (2,56%) |
| 2 NA + nelfinavir + efavirenz | 2 (5,13%) |
| 2 NA + nelfinavir + saquinavir | 1 (2,56%) |
| 2 NA + nelfinavir + nevirapina | 6 (15,38%) |
| 1 NA + nelfinavir + ritonavir + | 1 (2,56%) |
| efavirenz | |
Values are expressed as mean ± s.e.m. (min; max). VL, viral load. NA, nucleoside analogue.
Relationship between the %CD4+ T cell subsets and laboratory markers
We studied the relationship between the percentage of several CD4+ T cell subsets and viro-immunological markers used in clinical practice (i.e. %CD4+, CD8+ T cells and VL) by using a partial correlation analysis adjusted by age. Surprisingly, when analysing the association between VL and the different CD4+ T cell subsets, we found a positive correlation only with the CD4+ CD45RA-CD62L+ T cell subset (Table 3).
Table 3.
Summary of the correlation coefficients of %CD4+ and %CD8+T cells and log10 viral load (copies/ml) with the different CD4+ T cell subsets, expressed as %CD4+ T cells
| Correlation coefficients | ||||
|---|---|---|---|---|
| Phenotype | Values (min; max) mean ±s.e.m. | % CD4+ | % CD8+ | log10 VL |
| Memory/naive | ||||
| CD4+ CD45RO+ DR+ | 8·7 ± 1·80 (1·4; 51·3) | − 0·53** | − 0·29 | 0·27 |
| CD4+ CD45RO DR+ | 1·3 ± 0·25 (0·1; 7·3) | − 0·13 | 0·28 | 0·27 |
| CD4+ CD45RO+ DR | 32·8 ± 2·61 (13·2; 82·0) | − 0·37* | 0·25 | 0·04 |
| CD4+ CD45RO− DR | 57·2 ± 3·56 (6·1; 79·5) | 0·57** | − 0·36 | − 0·19 |
| CD4+ CD45RO+ CD38+ | 27·3 ± 2·27 (6·5; 74·2) | − 0·56** | 0·34* | 0·29 |
| CD4+ CD45RO+ | 41·6 ± 3·60 (15·9; 93·2) | − 0·56** | 0·34* | 0·17 |
| CD4+ CD45RA+ CD62L+ | 56·0 ± 3·39 (5·6; 83·7) | 0·71** | − 0·40* | − 0·26 |
| CD4+ CD45RACD62L+ | 31·0 ± 2·35 (12·4; 70·8) | − 0·48** | 0·08 | 0·36* |
| CD4+ CD45RA+ CD62L | 1·5 ± 0·42 (0·1; 11·8) | − 0·33* | 0·44** | 0·01 |
| CD4+ CD45RACD62L | 11·5 ± 1·84 (0·9; 49·9) | − 0·56** | 0·46** | 0·03 |
| CD4+ CD62L+ | 87·0 ± 2·11 (38·3; 97·4) | 0·54** | − 0·49** | 0·03 |
| CD4+ CD45RA+ | 57·5 ± 3·28 (5·8; 84·8) | 0·71** | − 0·36* | − 0·27 |
| Activated | ||||
| CD4+ DR+ CD38+ | 6·9 ± 1·46 (1·3; 52·4) | − 0·47** | 0·33 | 0·33 |
| CD4+ DR CD38+ | 75·3 ± 2·44 (35·7; 9) | 0·70** | − 0·42** | − 0·17 |
| CD4+ DR+ CD38 | 3·3 ± 0·59 (0·6; 15·9) | − 0·47** | 0·16 | 0·07 |
| CD4+ DR CD38 | 14·5 ± 1·35 (4·9; 36·3) | − 0·54** | 0·33 | − 0·14 |
| CD4+ HLA-DR+ | 10·0 ± 1·88 (1·9; 58·7) | − 0·52** | 0·31 | 0·29 |
| CD4+ CD38+ | 82·2 ± 1·74 (50·2; 94·0) | 0·58** | − 0·30 | 0·08 |
| RFI CD4+ HLA-DR+ | 15·6 ± 2·39 (3·8; 73·2) | − 0·45** | 0·16 | 0·31 |
| RFI CD4+ CD38+ | 49·5 ± 1·87 (26·4; 76·4) | 0·30 | − 0·51** | 0·19 |
RFI, relative fluorescence intensities. Level of significance
P < 0·05
P < 0·01. VL, viral load.
We found a positive correlation between %CD4+ T cells and both naïve (CD4+ CD45RA+ CD62L+) and CD4+ HLA-DRCD38+ cells (most of them naïve cells) (Table 3). Conversely, a negative correlation between %CD4+ T cells and all memory T cell subsets (CD4+ CD45RA+ CD62L, CD4+ HLA-DR+ and CD4+ HLA-DR+ CD38+ T cells) was found (Table 3). We also found a negative correlation between %CD4+ T cells and the level of HLA-DR expressed on the CD4 cell surface as measured by RFI (Table 3).
We found a positive correlation between %CD8+ T cells and memory T cell subsets (CD4+ CD45RO+, CD4+ CD45RO+ CD38+, CD4+ CD45RA+ CD62L and CD4+ CD45RA-CD62L) (Table 3). Conversely, we found a negative correlation between %CD8+ and naïve (CD4+ CD45RA+ CD62L+), CD4+ CD62L+ and CD4+ HLA-DRCD38+ T cells (Table 3). We also found a negative correlation between %CD8+ T cells and CD38 RFI (Table 3).
Differences between CD4+ T cell subsets according to the cut-off levels of 25% CD4 T cells and 4·5 log10 of viral load
Previously, we have reported that the cut-off level of 4·5 log10 VL copies/ml is indicative of high plasma viraemia [32]. Children having <4·5 log10 VL (copies/ml) showed statistically significant lower percentages of the CD4+ HLA-DR+ CD38+ subset (P < 0·05) indicating that the lower the VL, the lower the immune activation.
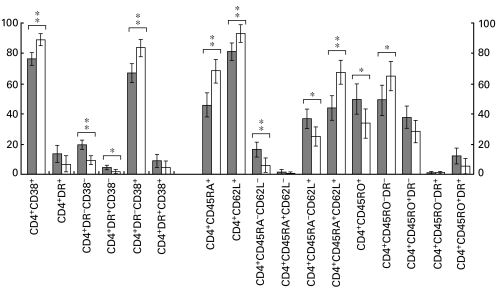
Similarly, we have reported that the cut-off level of 25% total CD4+ T cells is indicative of a preserved immunological status [24]. Children with >25% CD4+ T cells showed significantly higher percentages of naïve cells (CD4+ CD45RA+ CD62L+), CD4+ CD38+, CD4+ HLA-DRCD38+, CD4+ CD45RA+, CD4+ CD62L+ and CD4+ CD45RO-DR T cells subsets (Fig. 2). Conversely, we found lower percentages of CD4+ HLA-DRCD38, CD4+ HLA-DR+ CD38and all memory subsets in children with >25% CD4+ (Fig. 2). Thus, the more preserved the immune status, the higher the levels of naïve T cells.
Fig. 2.
Differences in the percentages of activated, memory and naïve CD4+ T cell subsets, expressed as %CD4+ T cells, in HIV-1-infected children stratified according to the 25% CD4+ T cells cut-off level. □, ≫25% CD4+ □, ≪25% CD4+.
Differences in the laboratory markers according to CD38 and HLA-DR expression
HIV-infected children were classified according to the expression of CD38 and HLA-DR in CD4 T cells, respectively. High expression of CD38 (CD38hi) was defined by CD38 RFI values >75th percentile (54·2) plus %CD4+ CD38+ cells >75th percentile (89·3); conversely, low expression (CD38lo) was defined by the <75th percentile of both RFI and %CD4+ CD38+ 0. Similarly, children were rated according to high expression of HLA-DR (HLA-DRhi) by HLA-DR RFI > 75th percentile (14·7) plus the %CD4+ HLA-DR+ cells, also the >75th percentile (8·2); and children with a low expression (HLA-DRlo) by the <75th percentile of both parameters. Interestingly, HIV-1-infected children with HLA-DRhi had higher values of VL and lower values of CD4+ T cells but we did not find any differences with respect to the expression of CD38 (Table 4). Therefore, in children, HLA-DRhi seems to be a better activation marker for CD4+ T cells than CD38hi.
Table 4.
Mean values of %CD4+, %CD8+ T cells and viral load in the infected children, according to the high or low expression level of CD38 and HLA-DR
| HLA-DRhi | HLA-DRlo | P | CD38hi | CD38lo | P | |
|---|---|---|---|---|---|---|
| %CD4+ | 14·6 ± 3·5 | 29·9 ± 1·8 | 0·001 | 26·2 ± 2·0 | 29·8 ± 5·7 | n.s. |
| %CD8+ | 51·2 ± 4·3 | 44·87 ± 2·2 | n.s. | 46·1 ± 2·1 | 47·8 ± 6·0 | n.s. |
| log10 VL | 4·70 ± 0·43 | 3·66 ± 0·22 | 0·040 | 3·86 ± 0·22 | 4·13 ± 0·63 | n.s. |
| (copies/ml) | ||||||
Values expressed as mean ± s.e.m.; VL, viral load; P, level of significance.
Discussion
HIV induces a chronic activation of CD4+ and CD8+ T lymphocytes, and predominantly destroys CD4+ T lymphocytes. Homeostatic mechanisms take place to counteract the fall of CD4+ T cells caused by HIV infection in the organism. HAART therapy, by inhibiting the chronic activation induced by HIV, allows the recovery of CD4+ lymphocyte numbers and, at least partially, their function [18]. Information on immune reconstitution is particularly scarce in HAART-treated children [33,34], and is focused mainly on the HIV-1-specific response. Thus, the study of the contribution of the different CD4+ subsets to this phenomenon may add very valuable information.
In our study, we did not find any association between CD4+ CD38+ subsets and VL. This is in agreement with the fact that the surface expression of CD38 in CD4 T cells is a marker of immaturity in children [8,10]. However, the co-expression of the memory marker CD45RO and the activation markers HLA-DR or CD38 plus HLA-DR in CD4+ T cells correlated negatively with %CD4+ T cells. Higher VL values in children correlated with increased co-expression of HLA-DR, measured both as a higher percentage of cells expressing HLA-DR as well as by the higher number of HLA-DR molecules per cell (RFI), and with higher percentages of CD4+ HLA-DR+ CD38+ cells. In contrast, the percentages of activated (CD4+ CDHLA-DR+, CD4+ CD38+ HLA-DR+) or memory-activated (CD4+ CD45RO+ HLA-DR+ CD4+ CD45RO+ CD38+) T cells did not correlate with VL. This lack of correlation may reflect the effect of ART in reducing CD4+ T cell activation. Moreover, we found a strong association between the CD4+ HLA-DRCD38+ cell subset and high %CD4+ T cells, comparable to the correlation between naïve CD4+ T cells and total CD4 cells. This indicates that CD4+ CD38+ numbers could be used in children as a marker of preserved immune status and its decrease is associated with immunodeficiency. Our data also indicate that naïve CD4+ T cells express CD38, confirming previously described data [10]. Therefore, we feel this marker should not be used as an activation marker for CD4 T cells, since it behaves in a completely different way to HLA-DR on CD4+ cells [10].
Our results suggest that the naïve CD4+ T cell subset can also be considered as a good marker of immune reconstitution in children, taking into account the strong correlation with the %CD4+0. Moreover, a strong association between naïve CD4 and naïve CD8 lymphocytes was observed [35], which either indicates a relatively preserved immune system or parallel immune reconstitution for both T cell subsets in response to HAART. Our data can be interpreted to mean that HAART somehow prevented HIV-replication in T cell progenitors, which would be in agreement with a previous report indicating that CD4+ CD8+ T cells progenitors can be infected and thereby die before emigrating from the thymus [36]. Available data in adults indicate that the thymus does not contribute significantly to the immune recovery induced by HAART, which may in fact result from the release of sequestered cells from lymph nodes [20]. From birth until around 20 years of age, more than 80% of the thymus is composed of lymphoid tissue, and this proportion continuously declines until it reaches 5% from the age of 40 onwards [37]. Although HAART therapy in children is not completely effective at inhibiting viral replication, only 20% of HIV-infected children had VL < 1000 copies/ml, and around 38% had VL > 30 000 copies/ml. Moreover, we have observed high percentages of naïve CD4+ T cells after HAART. However, we did not find any differences in the absolute naïve CD4+ T cell counts when stratifying our children by VL (data not shown). In this regard, our study is in agreement with those reported by other authors that describe substantial immune reconstitution in children on HAART, despite repeated virological failures [34]. Our data suggest that the thymus capacity to regenerate naïve T cells after HAART is probably much higher in infants and young children than in adults [38].
It has been described that the recovery of CD4+ T cells induced by HAART in adults is limited to memory and naïve lymphocytes that co-express CD62L, CD38 and low levels of CD44 [31]. The contribution of the memory CD4+ T cells (particularly cells co-expressing CD62L) to the immune reconstitution induced by HAART has been shown to be very important in HIV-infected adults [20,39]. In our children, CD4+ CD45RACD62L+ cells correlated negatively with %CD4 T cells. In addition, we found a negative correlation between the percentages of other memory CD4+ T cell subsets (CD4+ CD62L, CD4+ CD45RACD62L- and CD4+ CD38, regardless of co-expression of HLA-DR) with %CD4+ cells. Therefore, our data discount such an important role for memory T cells in children, suggesting a small contribution of those T cells to the immune reconstitution after HAART. Thus, naïve T cells CD45RA+ CD62L+ correlate with preserved immune status (high %CD4) whereas memory T cells correlate with immunodeficiency (low %CD4) even in the context of therapy that suppresses VL. These results may reflect the level of immunodeficiency even in the context of therapy.
Interestingly enough, we found a positive correlation between memory T cells co-expressing CD62L (CD4+ CD45RA CD62L+) and VL. This could indicate that this subset is the main target for HIV infection within CD4+ T cells. On the other hand, some subsets of memory CD4+ T cells have been described to be inherently resistant to HIV replication [40]. In our cohort of children we did not find any correlation between CD4+ CD62L and CD4+ CD38 subsets with VL. We hypothesize that these subsets could be less susceptible to HIV infection than cells co-expressing CD38 and CD62L.
HIV infection in children follows a different course than in adults and there are no data in the literature reporting the association of CD4 and CD8 subsets with the routine prognostic markers of progression in HAART-treated HIV-infected children. Our data indicate clearly a strong association between chronic activation of CD4+ T cells, severe immunological deterioration and high viral replication. Although this is a cross-sectional study, it indicates that in children the co-expression of CD38 on CD4+ T cells is neither a reliable marker of cellular activation nor of worse prognosis. One of the most important differences among HIV infection in children and adults is that children always have higher viral loads than adults [24], even after HAART therapy. Therefore, complete control of viral replication is often not achieved in children [34]. However, despite higher VL in children, we observed normal percentages of naïve cells, indicating a good immune reconstitution after HAART. Although the series of children studied is rather large, it would be necessary to perform follow-up studies not only to confirm these data but also to ascertain clues as to the pathogenesis of the HIV infection in children.
Acknowledgments
We thank Dolores García Alonso for her excellent technical assistance. This work was funded by grants of the Foundation for Research and Prevention of AIDS in Spain (FIPSE 3008/99), of the National Health Research Development Program (SAF 99–0022), the Community of Madrid and Bristol-Myers, S.A. Grupo Bristol-Myers Squibb.
References
- 1.Levacher M, Hulstaert F, Tallet S, et al. The significance of activation markers on CD8 lymphocytes in human immunodeficiency syndrome: staging and prognostic value. Clin Exp Immunol. 1992;90:376–82. doi: 10.1111/j.1365-2249.1992.tb05854.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phillips AN, Sabin CA, Elford J, et al. CD8 lymphocyte counts and serum immunoglobulin A levels early in HIV infection as predictors of CD4 lymphocyte depletion during 8 years of follow-up. AIDS. 1993;7:975–80. doi: 10.1097/00002030-199307000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Jackson DG, Bell JI. Isolation of a cDNA encoding the human CD38 (T10) molecule, a cell surface glycoprotein with an unusual discontinuous pattern of expression during lymphocyte differentiation. J Immunol. 1990;144:2811–5. [PubMed] [Google Scholar]
- 4.Mocroft A, Bofill M, Lipman M, et al. CD8+,CD38+ lymphocyte percent: a useful immunological marker for monitoring HIV-1-infected patients. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;14:158–62. doi: 10.1097/00042560-199702010-00009. [DOI] [PubMed] [Google Scholar]
- 5.Plaeger-Marshall S, Spina CA, Giorgi JV, et al. Alterations in cytotoxic and phenotypic subsets of natural killer cells in acquired immune deficiency syndrome (AIDS) J Clin Immunol. 1987;7:16–23. doi: 10.1007/BF00915420. [DOI] [PubMed] [Google Scholar]
- 6.Ibegbu C, Spira TJ, Nesheim S, et al. Subpopulations of T and B cells in perinatally HIV-infected and noninfected age-matched children compared with those in adults. J Acquir Immune Defic Syndr. 1994;7:340–8. doi: 10.1006/clin.1994.1047. [DOI] [PubMed] [Google Scholar]
- 7.Schlesinger M, Peters V, Jiang JD, et al. Increased expression of activation markers on CD8 lymphocytes in children with human immunodeficiency virus-1 infection. Pediatr Res. 1995;38:390–6. doi: 10.1203/00006450-199509000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Plaeger-Marshall S, Isacescu V, O'Rourke S, et al. T cell activation in pediatric AIDS pathogenesis: three-color immunophenotyping. Clin Immunol Immunopathol. 1994;71:27–32. doi: 10.1006/clin.1994.1046. [DOI] [PubMed] [Google Scholar]
- 9.Kestens L, Vanham G, Vereecken C, et al. Selective increase of activation antigens HLA-DR and CD38 on CD4+ CD45RO+ T lymphocytes during HIV-1 infection. Clin Exp Immunol. 1994;95:436–41. doi: 10.1111/j.1365-2249.1994.tb07015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Martino M, Rossi ME, Azzari C, et al. Different meaning of CD38 molecule expression on CD4+ and CD8+ cells of children perinatally infected with human immunodeficiency virus type 1 infection surviving longer than five years. Pediatr Res. 1998;43:752–8. doi: 10.1203/00006450-199806000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Clement LT, Yamashita N, Martin AM. The functionally distinct subpopulations of human CD4+ helper/inducer T lymphocytes defined by anti-CD45R antibodies derive sequentially from a differentiation pathway that is regulated by activation-dependent post-thymic differentiation. J Immunol. 1988;141:1464–70. [PubMed] [Google Scholar]
- 12.Schnittman SM, Lane HC, Greenhouse J, et al. Preferential infection of CD4+ memory T cells by human immunodeficiency virus type 1: evidence for a role in the selective T cell functional defects observed in infected individuals. AIDS. 1990;4:879–82. doi: 10.1073/pnas.87.16.6058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sleasman JW, Aleixo LF, Morton A, et al. CD4+ memory T cells are the predominant population of HIV-1-infected lymphocytes in neonates and children. AIDS. 1996;10:1477–84. doi: 10.1097/00002030-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Bradley LM, Bradley JS, Ching DL, et al. Predominance of T cells that express CD45R in the CD4+ helper/inducer lymphocyte subset of neonates. Clin Immunol Immunopathol. 1989;51:426–35. doi: 10.1016/0090-1229(89)90041-x. [DOI] [PubMed] [Google Scholar]
- 15.De Paoli P, Battistin S, Santini GF. Age-related changes in human lymphocyte subsets: progressive reduction of the CD4 CD45R (suppressor inducer) population. Clin Immunol Immunopathol. 1988;48:290–6. doi: 10.1016/0090-1229(88)90022-0. [DOI] [PubMed] [Google Scholar]
- 16.Picker LJ, Treer JR, Ferguson-Darnell B, et al. Control of lymphocyte recirculation in man. I. Differential regulation of the peripheral lymph node homing receptor l-selection on T cells during the virgin to memory cell transition. J Immunol. 1993;150:1105–21. [PubMed] [Google Scholar]
- 17.Carpenter CC, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1997. Updated recommendations of the International AIDS Society-USA panel. JAMA. 1997;277:1962–9. [PubMed] [Google Scholar]
- 18.Powderly WG, Landay A, Lederman MM. Recovery of the immune system with antiretroviral therapy: the end of opportunism? JAMA. 1998;280:72–7. doi: 10.1001/jama.280.1.72. [DOI] [PubMed] [Google Scholar]
- 19.Autran B, Carcelain G, Li TS, et al. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. J Med Chem. 1997;40:2164–76. doi: 10.1126/science.277.5322.112. [DOI] [PubMed] [Google Scholar]
- 20.Pakker NG, Notermans DW, de Boer RJ, et al. Biphasic kinetics of peripheral blood T cells after triple combination therapy in HIV-1 infection: a composite of redistribution and proliferation. Nat Med. 1998;4:208–14. doi: 10.1038/nm0298-208. [DOI] [PubMed] [Google Scholar]
- 21.Kelleher AD, Sewell WA, Cooper DA. Effect of protease therapy on cytokine secretion by peripheral blood mononuclear cells (PBMC) from HIV-infected subjects. Clin Exp Immunol. 1999;115:147–52. doi: 10.1046/j.1365-2249.1999.00761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kelleher AD, Carr A, Zaunders J, et al. Alterations in the immune response of human immunodeficiency virus (HIV)-infected subjects treated with an HIV-specific protease inhibitor, ritonavir. J Infect Dis. 1996;173:321–9. doi: 10.1093/infdis/173.2.321. [DOI] [PubMed] [Google Scholar]
- 23.Bohler T, Walcher J, Holzl-Wenig G, et al. Early effects of antiretroviral combination therapy on activation, apoptosis and regeneration of T cells in HIV-1-infected children and adolescents. Am J Public Health. 1999;89:947–8. doi: 10.1097/00002030-199905070-00006. [DOI] [PubMed] [Google Scholar]
- 24.Resino S, Gurbindo MD, Bellón JM, et al. Predictive markers of clinical outcome in vertically HIV-1 infected infants. A prospective longitudinal study. Pediatr Res. 2000;47:509–15. doi: 10.1203/00006450-200004000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Gurbindo D, Resino S, Sánchez-Ramón S, et al. Correlation of viral load and CD8 T-lymphocyte with development of neurological manifestations in vertically HIV-infected infants. A prospective longitudinal study. Neuropediatrics. 1999;30:197–204. doi: 10.1055/s-2007-973490. [DOI] [PubMed] [Google Scholar]
- 26.Munoz-Fernandez MA, Obregon E, Navarro J, et al. Relationship of virologic, immunologic, and clinical parameters in infants with vertically acquired human immunodeficiency virus type 1 infection. Pediatr Res. 1996;40:597–602. doi: 10.1203/00006450-199610000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Center for Diseases Control Prevention (CDCP) Revised classification system for HIV-1 infection in children less than 13 years of age. MMWR. 1994;43:1–13. [Google Scholar]
- 28.Center for Diseases Control Prevention (CDCP) Guidelines for use of antiretroviral agents in pediatric HIV infection. MMWR. 1998;47:RR–4. [PubMed] [Google Scholar]
- 29.Nicholson JK, Hubbard M, Jones BM. Use of CD45 fluorescence and side-scatter characteristics for gating lymphocytes when using the whole blood lysis procedure and flow cytometry. Cytometry. 1996;26:16–21. doi: 10.1002/(SICI)1097-0320(19960315)26:1<16::AID-CYTO3>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 30.Nicholson J, Kidd P, Mandy F, et al. Three-color supplement to the NIAID DAIDS guideline for flow cytometric immunophenotyping. Cytometry. 1996;26:227–30. doi: 10.1002/(SICI)1097-0320(19960915)26:3<227::AID-CYTO8>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 31.Hengel RL, Jones BM, Kennedy MS, et al. Markers of lymphocyte homing distinguish CD4 T cell subsets that turn over in response to HIV-1 infection in humans. J Immunol. 1999;163:3539–48. [PubMed] [Google Scholar]
- 32.Resino S, Bellón JM, Gurbindo D, et al. Prognostic markers of progression to AIDS in infants vertically infected by human immunodeficiency virus type-1. Med Clin (Barc) 2000;115:564–7. doi: 10.1016/s0025-7753(00)71626-5. [DOI] [PubMed] [Google Scholar]
- 33.Luzuriaga K, McManus M, Catalina M, et al. Early therapy of vertical human immunodeficiency virus type 1 (HIV-1) infection: control of viral replication and absence of persistent HIV-1- specific immune responses. J Virol. 2000;74:6984–91. doi: 10.1128/jvi.74.15.6984-6991.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Essajee SM, Kim M, Gonzalez C, et al. Immunologic and virologic responses to HAART in severely immunocompromised HIV-1-infected children. AIDS. 1999;13:2523–32. doi: 10.1097/00002030-199912240-00005. [DOI] [PubMed] [Google Scholar]
- 35.Rabin L, Hincenbergs M, Moreno MB, et al. Use of standardized SCID-hu Thy/Liv mouse model for preclinical efficacy testing of anti-human immunodeficiency virus type 1 compounds. Pediatr Infect Dis J. 1996;15:197–203. doi: 10.1128/aac.40.3.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bonyhadi ML, Rabin L, Salimi S, et al. HIV induces thymus depletion in vivo. Nature. 1993;363:728–32. doi: 10.1038/363728a0. [DOI] [PubMed] [Google Scholar]
- 37.Rodewald HR. The thymus in the age of retirement. Nature. 1998;396:630–1. doi: 10.1038/25251. [DOI] [PubMed] [Google Scholar]
- 38.Franco JM, Leon-Leal JA, Leal M, et al. CD4+ and CD8+ T lymphocyte regeneration after anti-retroviral therapy in HIV-1-infected children and adult patients. Clin Exp Immunol. 2000;119:493–8. doi: 10.1046/j.1365-2249.2000.01152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walker RE, Carter CS, Muul L, et al. Peripheral expansion of pre-existing mature T cells is an important means of CD4+ T cell regeneration HIV-infected adults. Nat Med. 1998;4:852–6. doi: 10.1038/nm0798-852. [DOI] [PubMed] [Google Scholar]
- 40.Wallace DL, Matear PM, Davies DC, et al. CD7 expression distinguishes subsets of CD4(+) T cells with distinct functional properties and ability to support replication of HIV-1. Eur J Immunol. 2000;30:577–85. doi: 10.1002/1521-4141(200002)30:2<577::AID-IMMU577>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]