Abstract
Anticancer drugs are generally plagued by toxic manifestations at doses necessary for control of various forms of cancer. Incorporating such drugs into liposomes not only reduces toxicity but also enhances the therapeutic index. Some antioxidants and potent immunomodulators have also been shown to impart significant antitumor activity presumably by nonspecific activation of the host immune system. In the present study, we evaluated augmentation of the antitumor activity of etoposide (ETP) by the immunomodulator tuftsin in Swiss albino mice with fibrosarcoma. The efficacies of the free form of ETP, liposomized ETP (Lip-ETP), and tuftsin-bearing liposomized ETP (Tuft-Lip-ETP) formulations were evaluated on the basis of tumor regression, effect on expression level of p53wt and p53mut, and survival of the treated animals. Tuft-Lip-ETP, when administered at a dosage of 10 mg/kg body weight/day for five days, significantly reduced tumor volume, delayed tumor growth, and also up-regulated the expression of p53wt. In contrast, although Lip-ETP delayed tumor growth, it did not decrease tumor size. The results of the present study suggest that tuftsin incorporation in drug-loaded liposomes is a promising treatment strategy for various forms of cancers, including fibrosarcoma.
INTRODUCTION
Etoposide (ETP), a derivative of podophyllotoxin, has been successfully employed as an antineoplastic agent against various forms of cancer. It causes cell death by forming a ternary complex with topoisomerase II and DNA ensuing breakage of DNA (1) and is active against multiple cell lines such as L929 fibroblasts, HL-60, K562, A549 human lung carcinoma cells (2–4). It is a part of the first-line therapy for small-cell lung carcinoma (5), malignant lymphoma (6), and drug-resistant testicular cancer (7). Unfortunately, ETP causes dose-limiting hematological (8) as well as gastrointestinal toxicity when administered orally (9). Furthermore, the lipophilic nature of ETP poses difficulty in development of drug formulations; as a consequence different solubilizers are generally used as co-additives to develop suitable ETP formulations (10). These additives are often associated with adverse effects such as hypotension, anaphylaxis, and bronchospasm (8,11).
Taking into consideration toxicity constraints associated with most of the available chemotherapeutic agents, including ETP, many workers have successfully used liposome-based delivery systems to circumvent these problems (12, 13–17). The higher lipophilicity of ETP offers better intercalation in lipid-based liposomal formulations (18,19). Liposomes accumulate in the tumors in a gradual passive fashion due to increased “leakiness” of the tumor vasculature (20). In particular, antineoplastic agents encapsulated in long circulating pegylated liposomes have been found to attain higher concentrations in tumor interstitium, ultimately eliminating tumors with great efficiency (21). Similarly, the encapsulation of certain anticancer agents into cationic liposomes was also found to enhance their antitumor potential. However, cost factors, cumbersome preparation methods, and more importantly, intrinsic toxic manifestations of cationic lipids limit their usefulness as suitable drug vehicles.
The immunomodulator tuftsin is a tetra peptide (Thr-Lys-Pro-Arg) that binds specifically to macrophages, monocytes, and polymorphonuclear leukocytes and stimulates them to evoke immunomodulatory activity in the host. Many reports have also described anti-tumor activity of tuftsin against experimental tumors in animal models (22,23). Because of tuftsin’s intrinsic antitumor properties and its possible role in activation and infiltration of tumoricidal macrophages, administration of tuftsin in combination with a potent antitumor agent can successfully suppress various forms of cancers.
Earlier attempts have demonstrated usage of liposomized ETP (Lip-ETP) in delaying tumor progression, but such treatment failed to regress tumor in model animals (19,24). In the present study, we evaluated tuftsin-mediated augmentation of the antitumorogenic potential of ETP against fibrosarcoma induced in Swiss albino mice by the carcinogen benzo (a) pyrene. Development of tumor was ascertained by measurement of tumor volume and confirmed by histopathological examination of the tissues. The tumor-bearing animals were treated with free-form as well as liposomal formulation of ETP with or without tuftsin. The efficacy of various formulations was ascertained on the basis of tumor volume and survival, as well as expression of p53wt and p53mut in the tumor tissues of the animals.
MATERIALS AND METHODS
Chemicals
All the reagents used in the study were of the highest purity available. Egg PC was isolated and purified from hen egg yolk according to published procedure (25). Cholesterol was bought from Centron Research Laboratory, Mumbai, India, and used after crystallizing three times with methanol. Tuftsin was modified at the C-terminus by attaching a sufficiently long hydrocarbon fatty acyl residue to the C-terminus through an ethylenedi-amine spacer arm (Thr-Lys-Pro-Arg-NH-(CH2)2-NH-CO-C15H31), which permits almost quantitative incorporation into liposomes, following the procedure standardized in our lab (26). Anti-p53 antibody specific for wild-type (wt) protein (clone PAb 1620, Ab-5) and anti-p53mut (clone PAb 240) were purchased from Merck India, Ltd. The horseradish peroxidase-conjugated isotypes were obtained from Bangalore Genei (Bangalore, India).
Animals
Female Swiss albino mice weighing 18 ± 2 g were used in the whole study. The animals were given a standard pellet diet (Hindustan Lever Ltd.) and water ad libitum. Animals were checked daily for their mortality and morbidity prior to commencement of the study, and only healthy animals were included in the experiment. The techniques used for bleeding and injection as well as killing of animals were performed strictly according to mandates approved by the institute’s Animal Ethics Committee (Committee for the purpose of control and supervision of Experiments on Animals, Government of India).
Liposome Preparation
Etoposide-bearing unilamellar liposomes were prepared from egg PC (49 μmol) and cholesterol (21 μmol) with or without tuftsin (6.66 mol % of PC) following the published procedure (25). Briefly, the solution of egg PC and ETP (in a ratio of 40:1 w/w) along with cholesterol and tuftsin in chloroform was reduced to a thin dry film with a slow jet of N2 gas. The dried lipid film was hydrated with 150-mM sterile normal saline, followed by sonication for 1 h at 4 ° C under N2 atmosphere in a bath-type sonicator. The sonicated preparation was centrifuged at 10,000 g for 1 h at 4 ۜ°C to remove undispersed lipid. Finally, the liposomal preparation was extensively dialyzed against saline for 24 h at 4 °C in the dark to remove the free form of the drug from the liposomal preparations. Both tuftsin-free and tuftsin-bearing liposomal preparations were found to be of unilamellar type, with a size range of 80 ± 10 nm, as revealed by electron microscopy (data not shown).
ESTIMATION OF LIPOSOME INTERCALATED ETP
The intercalation efficiency of ETP in the liposomes was estimated by an HPLC method (27). Briefly, specific volumes of standard drug solution of an isocratic were injected onto a Hypersil octyldecylsilane (5 μm particle size) analytical column (150 × 4.6 mm). Detection of ETP was accomplished with a UV-visible-light detector set at 254 nm. A standard curve of ETP was plotted by calibrating peak area versus amount of the drug injected into the column. The elution buffer consisted mixture of 0.005 M EDTA and methanol (2: 8 v/v). The flow rate was kept at 1.2 mL/min, and retention time was found to be 4.5 min. Finally a known volume of liposomal formulation was injected and the amount present in the sample was determined by the area under the curve. The intercalation efficiency of ETP, both in plain egg PC and tuftsin-bearing liposomes, was found out to be of the same order of magnitude (90% ± 4%).
Estimation of Liposome Intercalated Tuftsin
The amount of tuftsin entrapped in the drug-containing liposomes was estimated by the BCA method, as modified in our lab (28). Briefly, the liposomes (given volume) were lysed with a Triton X-100 solution and incubated with the mixture of solutions A and B of BCA reagent. The absorbance of the colored complex formed was measured at 600 nm, and tuftsin content was determined using a standard curve of tuftsin plotted in the presence of Triton X-100. The incorporation of tuftsin was found out to be ~98% for both sham as well as ETP-containing tuftsin-bearing liposomes.
In Vitro Drug Release Assay
Drug release from tuftsin-bearing ETP liposomes into surrounding phosphate buffered saline (PBS; pH 7.4) was determined by the HPLC method, following a standardized protocol as described above (27). The vials containing Lip-ETP and tuftsin-bearing liposomized ETP (Tuft-Lip-ETP) were incubated with PBS at 37 °C under continuous shaking. An aliquot was withdrawn at two different time points (24 h and 48 h) and the mixture was ultracentrifuged at 100,000g for 15 min. The resulting supernatant was analyzed by HPLC method as described earlier. The percentage of in vitro release was calculated with respect to the total drug content in liposomes.
ETP-Mediated Lysis of Human Erythrocytes
The human red blood cells (RBCs) were diluted to 50% hematocrit with isotonic buffer. ETP (free as well as Lip-ETP) was added at a concentration of 10 μg/mL to erythrocyte suspension. The free form of the drug was dissolved in 50 mL of DMSO, and the final volume was made up to 1 mL with PBS (5% DMSO). To study hemolysis, a suspension of RBCs was incubated with 1 mL of free as well as liposomized drug (10 μg/mL) at 37 °C for 1 h and centrifuged at 1500g; then the supernatant was analyzed for the released hemoglobin by measuring the absorbance at 576 nm. The percentage hemolysis was determined by following equation:
where Abs = absorbance of the sample,
Abs0 = Absorbance of negative control (erythrocytes in 5% DMSO) with no ETP
Abs100 = Absorbance of positive control (erythrocytes in 1% Triton X-100) in the presence of 10 μg/mL ETP.
Maximum Tolerated Dose
The maximum tolerated dose (MTD) for the tuftsin bearing liposomal formulation administered intravenously was determined in healthy Swiss albino mice. Doses were escalated in increments starting with 0, 10, 20 40, 100, 200, 400, and 500 mg/kg body weight daily for five days. After completing the preliminary experiments, we defined the approximate MTD using eight groups consisting of 9 mice of each. The drug effects were determined by careful surveillance of weight changes and survival of the experimental animals. The highest nonlethal dose of ETP causing > 10% weight loss within 1 week of cessation from start of the dosing schedule was defined as the MTD. Of the 9 animals in each group, 3 mice received free drug, 3 were given Lip-ETP, and the remaining 3 were given Tuft-Lip-ETP.
Hematological Toxicity Tests
Swiss albino mice were used to analyze the changes in hematological parameters after administration of Tuft-Lip-ETP, Lip-ETP, and the free form of ETP, with respect to time and dose. The mice were randomized into 4 groups. Group I served as controls and received vehicle treatment, and group II, group III, and group IV mice were treated with free ETP, Lip-ETP, and Tuft-Lip-ETP formulations, respectively, at a dosage of 10 mg/kg body weight/day for 5 days. Drugs were administered through the tail vein. On day seven after the last treatment dose of the analysis, the animals were killed by cervical dislocation while under anesthesia, and blood was withdrawn by cardiac puncture. Total and differential leukocyte and platelet counts were determined using a Sysmex cell counter.
In Vivo Tumor Model
Solid fibrosarcoma was induced in mice according to the published method, with slight modification (29). Briefly, a single dose of benzo (a) pyrene (250 μg/animal) was administered subcutaneously into the flanks of the left hind limbs. The mice were observed daily for any change along the dimensions of the two hind limbs. The mice that developed palpable tumors at 90 to 100 d of administration of benzo (a) pyrene were included in the study.
Treatment Schedule and Efficacy-Assessment Parameters
The animals were divided into seven groups of 20 animals each. The animals in group I were used as untreated controls (normal healthy) and did not receive any treatment. The tumor-bearing mice were pooled and randomized into 6 groups (group II–VII) (Table 1). The tumors were measured regularly with a Vernier caliper until they reached a volume of 200 mL. At this juncture the mice were treated with 10 mg/kg body weight/day of ETP for five consecutive days, and the first day of treatment was considered day 0. The drug and vehicle were slowly injected into the tail vein. The tumors were measured regularly after treatment, and antitumor activity was assessed by calculating the tumor volume according to the formula:
Table 1.
Treatment Groups of Tumor-Bearing Mice
| Groups | Treatment |
|---|---|
| Group I | Untreated control (normal) |
| Group II | PBS (vehicle control) |
| Group III | Sham liposomes (vehicle control) |
| Group IV | Empty tuftsin liposome without ETP (Sham-Tuft-Lip) |
| Group V | Free drug (ETP) |
| Group VI | Liposomal ETP (Lip-ETP) |
| Group VII | Tuftsin-bearing liposomal ETP (Tuft-Lip-ETP) |
where V = tumor volume, D = biggest dimension, and d = smallest dimension.
Using the median day of death (MDD), we calculated the percentage increase in host life span according to a previously described formula (30):
Percentage increase in host life span = MDD (treated mice) − MDD (tumor-bearing control mice) × 100 MDD (tumor-bearing control mice)
Histopathological Examinations
To assess the development of tumor, three mice were killed by cervical dislocation and fixed in 10% formaldehyde solution. Subsequently, tumor tissues were excised, and sections were prepared using conventional paraffin sections and hemotoxylineosin staining.
Preparation of Nuclear Fraction
On day 25 after the administration of the first dose of various forms of ETP, the skin/tumor tissues were removed from experimental mice with sharp scalpel blades. The tissue samples were placed on ice and fat was scrapped off before further processing. Finally, the samples were homogenized and the nuclear fraction was prepared according to a published method (31).
WESTERN BLOTTING
Using a Western blotting method (32), we analyzed the nuclear fraction for the presence of p53wt and p53mut. Briefly, protein content of the homogenate was estimated by the routine method using BSA as a standard (33). Proteins (30–50 μg) were resolved under nondenaturing conditions on PAGE for p53wt and on 10% SDS-PAGE gels for p53mut and electro-blotted onto nitrocellulose membranes. The blots were probed with appropriate antibodies [i.e., anti-p53wt (clone PAb 1620) and anti-p53mut (clone PAb 240)]. Immunoblots were detected by horse-radish peroxidase-conjugated anti-mouse IgG using 3, 3′-diaminobenzidine tetra-hydrochloride chromogen. To quantify equal loading, membranes were reprobed with β-actin antibody. Data were presented as the relative pixel density of each of the bands normalized to band of β-actin. The intensity of the bands was quantitated using Alpha Image Analysis software on an Alpha Image Gel Documentation System.
Statistics
All the data were evaluated with SPSS/10.0 software. Multiple groups at the same time points were compared using ANOVA followed by Dunnett’s post hoc test. P values <0.05 were considered statistically significant.
RESULTS
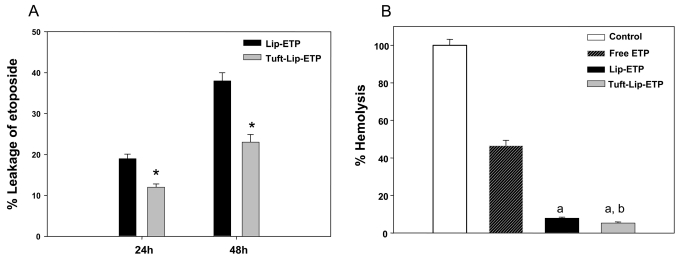
When a novel formulation of a given therapeutic agent is developed, it is desirable to have some information about its in vitro stability profile. In this investigation, kinetic studies of in vitro drug release revealed that incubation of Lip-ETP in PBS resulted in slow release of the drug. After 24 h and 48 h, respectively, leakage of ETP from tuftsin-bearing ETP liposomes was 12% and 23%, whereas drug release of Lip-ETP was 19% and 38% (Figure 1a).
Figure 1.
(A) Leakage of ETP from liposomized formulations in surrounding PBS buffer. Liposomized formulations of ETP were incubated in PBS for 24 h and 48 h. Aliquots were taken from the supernatant to determine released ETP by HPLC as described in Materials and Methods. Data are mean ± SD of 3 independent experimental values. *P < 0.001 (Tufts-Lip-ETP) versus Lip-ETP at 24 h and 48 h. (B) Hemolysis of human erythrocytes induced by various formulations of ETP. Human erythrocytes were incubated with free ETP, Lip-ETP, and Tuft-Lip-ETP for 1 h at 37 °C as described in Materials and Methods. Data are mean ± SD of 3 independent experimental values. Various groups were compared by one-way ANOVA followed by Dunnett’s post hoc test. aP < 0.001 versus free ETP; bP < 0.001 versus Lip-ETP.
Toxicity study results suggest that incorporation of ETP in liposomes markedly lowers its toxicity to erythrocytes. Among various formulations, free ETP was found to show maximum toxicity, resulting in significant hemolysis of erythrocytes. The incorporation of ETP in conventional as well as tuftsin-bearing liposomes resulted in surprising diminution of its toxicity. The Tuft-Lip-ETP formulation imparts less toxicity to erythrocytes (~7% hemolysis) than does conventional liposomal preparation (~12% hemolysis) of the same drug (Figure 1b).
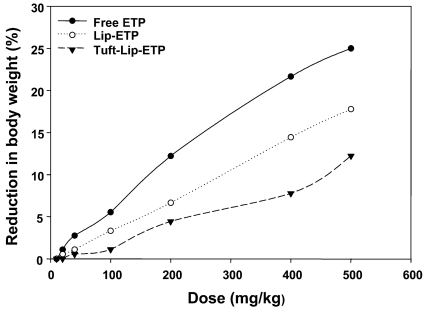
Loss of body weight in response to the administration of the antineoplastic agent ETP was used as another parameter to assess its toxicity. As shown in Figure 2, the maximum tolerated doses (MTD) for free ETP, Lip-ETP, and Tuft-Lip-ETP were found to be 165.53, 279.77, and 413.25 mg/kg, respectively (P < 0.001 for Lip-ETP vs free ETP and for Tuft-Lip-ETP vs Lip-ETP).
Figure 2.
Effect of increasing doses of ETP on body weight of the treated animals. The Swiss mice were treated with free ETP, Lip-ETP, and Tuft-Lip-ETP. The dose resulting in the loss of more than 10% body weight is identified as the MTD. Lip-ETP had a significantly higher MTD than free ETP, and Tuft-Lip-ETP had a significantly higher MTD than Lip-ETP. Data shown are means of three individual animals at each dose point.
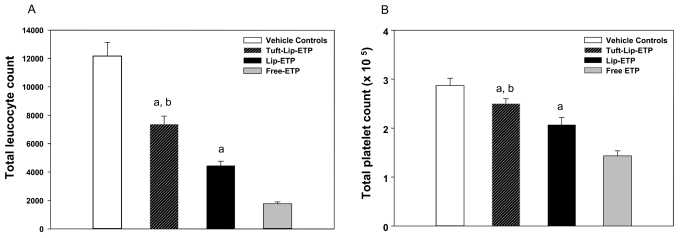
Hematological tests were performed to evaluate the effect of Lip-ETP on rapidly proliferating hematopoietic cells. The immune cell depletion was significantly greater in the free ETP treated group than in the Lip-ETP treated group, with mean total leukocyte counts of 1764/mm3 vs 4457/mm3 counts, respectively, (P < 0.001) on day 7 from the last dose. Myelosuppression was significantly lower in the group of animals treated with Tuft-Lip-ETP (mean total leukocyte count 7364/mm3) compared with groups of animals treated with free (P < 0.001) or Lip-ETP (P < 0.001). Control healthy mice had a total leukocyte count of 12,160/mm3 at the same time point (Figure 3a). After therapy, however, no substantial change was observed in the differential leukocyte profile, a finding that suggests that the proliferation of all the components was equally suppressed. A reduction in platelet count was also observed on day 7 in drug-treated groups compared with controls. The mean platelet counts in the free ETP, Lip-ETP, and Tuft-Lip-ETP treated groups were 1.4 × 105/mm3 (P < 0.001 vs control), 2.1 × 105/mm3 (P < 0.001 vs free ETP), and 2.5 × 105/mm3 (P < 0.001 vs free as well as Lip-ETP), respectively. Vehicle-treated control animals had a mean platelet count of 2.8 × 105/mm3 (Figure 3b).
Figure 3.
Effects of ETP chemotherapy on leukocyte and platelet counts of the treated animals. Experimental animals were treated with various formulations of ETP. The blood samples of the treated animals were analyzed for their lymphocyte and platelet counts. (A) Free ETP significantly reduced the total leukocyte count (P < 0.001) compared with controls. Lip-ETP caused lesser myelosuppression compared with free ETP (P < 0.001). Tuft-Lip-ETP depleted fewer leucocytes compared with free ETP (P < 0.001) and Lip-ETP (P < 0.001). (B) A similar effect was observed on platelet counts as seen for total leukocyte count after treatment with free ETP (P < 0.001). The Lip-ETP group had significantly higher mean platelet counts (P < 0.001) than the free ETP group. The Tuft-Lip-ETP group had even higher platelet counts than the free (P < 0.001) and Lip-ETP (P < 0.001) groups. Data are means ± SD with n = 5 per group. aP < 0.001 versus free ETP; bP < 0.001 versus Lip-ETP.
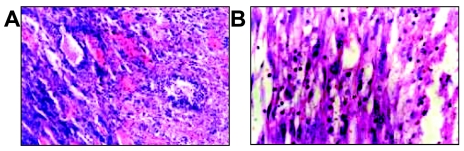
To evaluate in vivo efficacy of various ETP formulations against experimental fibrosarcoma, tumors were developed in model animals. After treatment with benzo (a) pyrene, 90% of the treated animals developed tumors within 90–100 days. The establishment of the tumors was confirmed by histopathological examinations of the tissues. The fibrosarcoma was found to be accompanied by increased vascularization and large pleomorphic, hyperchromatic spindle-shaped cells with anisonucleosis and irregularly dispersed chromatin (Figure 4a and 4b).
Figure 4.
Establishment of fibrosarcoma by exposure of animals to benzo (a) pyrene. Administration of benzo (a) pyrene (250 μg/animal, subcutaneously) into the flanks of the animals resulted in successful tumor induction in at least 90 % of the animals and no tumor development in 10 % of the animals. The tumor-bearing animals were killed by cervical dislocation and fixed in 10 % formaldehyde solution. Subsequently tissues were excised and sections were prepared after standard HE staining of 12-mm-thin sections. (A) Photomicrograph from tumor showing zone of necrosis, increased vascularization and hemorrhage. Large numbers of hyperchromatic mesenchymal cells with features of fibrosarcoma are present. Some hyperchromatic cells are arranged in glandular form. (B) Photomicrograph from tumor showing soft tissue sarcoma with large pleomorphic, hyperchromatic spindle-shaped cells with anisonucleosis and irregularly dispersed chromatin. Some inflammatory cells can also be seen.
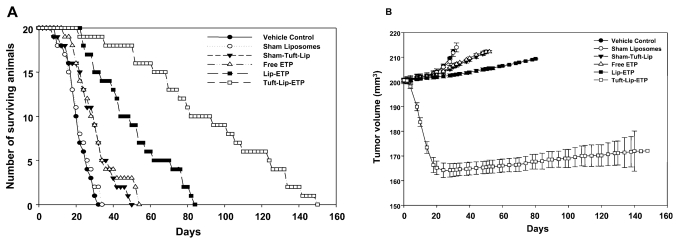
Among various formulations, Tuft-Lip-ETP was found to be more effective that tuftsin-free Lip-ETP or free ETP in treatment of fibrosarcoma. Treatment of the animals with Lip-ETP was started when the tumors attained the size of approximately 200 mm3. Mice treated with chemotherapy with Tuft-Lip-ETP at a dose of 10 mg/kg body weight/day for five days showed significantly reduced tumor growth compared with mice treated with Lip-ETP (P < 0.001), free ETP (P < 0.001), and Sham-Tuft-Lip (P < 0.001) as well as controls treated with sham liposomes (no tuftsin) and PBS (P < 0.001). Lip-ETP delayed tumor growth and was superior to the free form of ETP and sham tuftsin liposomes but did not cause significant tumor regression. On the other hand, tuftsin-bearing ETP liposomes reduced growth up to 165.7 ± 2.63 mm3 from 200 mm3 within 52 d after the initiation of chemotherapy (Figure 5a).
Figure 5.
(A) Effects of chemotherapy with various formulations of ETP on tumor development in Swiss mice. Treatment of tumor-bearing animals was started when the tumor size reached a volume of approximately 200 mm3. Free ETP and sham tuftsin liposomes significantly delayed tumor growth (P < 0.05) as compared with controls (PBS and Sham liposomes). Liposomal ETP was superior to free ETP in delaying tumor growth (P < 0.001). The regressions of tumors were recorded only in the group of animals treated with Tuft-Lip-ETP. Data are values ± SD (n = 20 at initiation of therapy, the number varies at later time points due to mortality). (B) Effects of ETP chemotherapy on the survival of tumor-bearing mice. The fibrosarcoma was induced by exposure to benzo (a) pyrene. The treatment of tumor-bearing animals was started at the time point when tumor size reached a volume of approximately 200 mm3. All the treated mice received a dose of 10 mg/kg body weight/day for 5 d with various formulations of the drug. Free ETP significantly enhanced the life span of the mice compared with the control group (PBS and sham liposomes) (P < 0.01). Lip-ETP was superior to free ETP in increasing the lifespan (P < 0.001). The best therapeutic effect was recorded in the group of animals treated with Tuft-Lip-ETP (P < 0.001). Data shown are the number of mice surviving at the given time points.
Mortality was seen in all mice with benzo (a) pyrene induced tumors, but animals treated with appropriate chemotherapy had comparatively longer life spans. Table 2 shows the median day of death in each group. Tumor-bearing mice treated with the free form of ETP lived longer than those treated with PBS or with sham liposomes (P < 0.001). Tumor-bearing mice treated with Lip-ETP lived longer than those treated with the free form of ETP or with Sham-Tuft-Lip (P < 0.001) (Figure 5b), and tumor-bearing mice treated with Tuft-Lip-ETP lived longer than those treated with Sham-Tuft-Lip-ETP or with Lip-ETP (P < 0.001).
Table 2.
Effect of Chemotherapy with Various Formulations on the Progression of Benzo (a) Pyrene-Induced Fibrosarcomaa
| Treatment | MDD | Increase in life span % |
|---|---|---|
| PBS (Vehicle Control) | 22 | — |
| Sham liposomes (Vehicle Control) | 23 | — |
| Sham-Tuft-Lip | 31 | 40.90 |
| Free Drug (ETP) | 29 | 31.81 |
| Lip-ETP | 50 | 127.27 |
| Tuft-Lip-ETP | 88 | 300.00 |
All the ETP-treated mice received 10 mg/kg body weight/day for 5 d of drug as a suspension in PBS. The formulations were diluted in PBS so the total volume of administration was always 100 μL. Vehicle-treated groups received only PBS (100 μL), or sham liposomes in PBS (100 μL). Percentage increase in host life span was calculated by the formula as described in Materials and Methods.
Exposure to the carcinogenic agent benzo (a) pyrene followed by treatment with ETP resulted in transient weight loss in treated animals. The treatment with liposomized ETP mitigated weight loss to varying levels depending on the ETP formulation used for the treatment (data not shown).
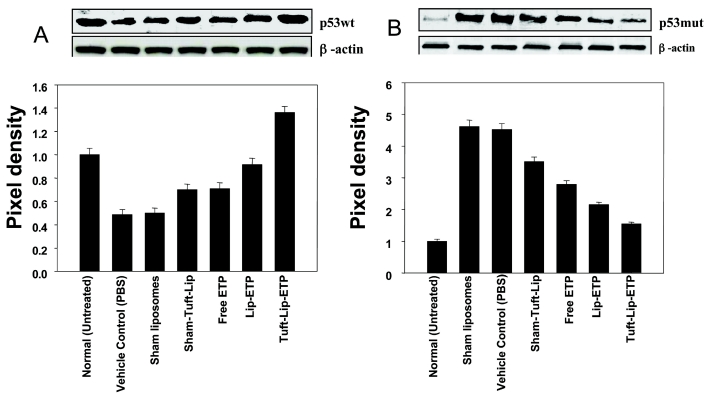
Because p53 is crucial for regulating growth and death of cells, its presence was used as a parameter to study the antitumoricidal effect of the tuftsin. The levels of p53wt protein were significantly reduced in fibrosarcoma-bearing animals, which were treated with PBS and sham liposomes (vehicle controls), compared with untreated healthy controls (Figure 6a, lanes 1, 2 and 3). A comparatively high expression level of p53wt protein was recorded in the animals treated with various formulations of ETP. Compared with the animals treated with vehicle, p53wt expression increased 179 % in animals treated with Tuft-Lip-ETP, 88 % in animals treated with Lip-ETP, 45 % in animals treated with the free form of ETP, and 44 % in animals treated with sham tuftsin liposomes (Figure 6a) indicating that tuftsin-bearing liposomal ETP replenished the expression of p53wt protein and abolished benzo (a) pyrene–induced neoplastic changes.
Figure 6.
(A) Effect of various formulations on the expression of p53wt in mouse fibrosarcoma. Skin/tumor lysates were prepared as described in Materials and Methods and 30–50 μg protein was used for Western blot analysis. A diminutive expression of p53wt was recorded in the animals treated with vehicle controls. Treatment with various formulations was found to replenish the p53wt expression in fibrosarcoma. Lane 1, untreated (Normal); lane 2, vehicle control (PBS); lane 3, sham egg PC liposomes; lane 4, Sham-Tuft-Lip; lane 5, free ETP; lane 6, Lip-ETP; and lane 7, Tuft-Lip-ETP. (B) Effect of various formulations on the expression of mutp53 in mouse fibrosarcoma. Skin/tumor lysates were prepared as described in Materials and Methods and proteins (30–50 μg) were employed for Western blots. The expression of p53mut was induced significantly in the animals treated with vehicle controls; however, treatment with various formulations against fibrosarcoma resulted in a decrease in p53mut expression. Lane 1, untreated (normal); lane 2, vehicle control (PBS); lane 3, sham liposomes; lane 4, Sham-Tuft-Lip; lane 5, free ETP; lane 6, Lip-ETP; and lane 7, Tuft-Lip-ETP.
Mice treated with tuftsin-bearing liposomal ETP showed a low level of p53mut similar to that of the healthy mice not exposed to benzo (a) pyrene, whereas up-regulation of p53mut occurred in animals exposed to benzo (a) pyrene and subsequently treated with vehicle controls (Figure 6b, lanes 1, 2, 3 and 7). As depicted in Figure 6b, 85 % down-regulation in the expression level of p53mut occurred in the animals treated with Tuft-Lip-ETP compared with the animals treated with vehicle only (PBS and sham liposomes). In the group of animals treated with Lip-ETP, the reduction was 68 %, and 50 % down-regulation occurred in the animals treated with the free form of ETP and 30 % in the animals treated with Sham-Tuft-Lip. These results clearly demonstrate ETP-mediated down-regulation of p53mut, which was more marked upon its intercalation along with tuftsin in the liposomes used in the present study (Figure 6b).
DISCUSSION
Drugs used in cancer treatment generally have severe toxic manifestations and undesirable side effects. The use of most of the anticancer drugs, including ETP, is also limited by an ever-increasing trend of multidrug resistance by cancerous cells. This resistance is mainly due to the drug efflux mediated by an array of transporters, p-glycoproteins such as p-gp4, and other multidrug resistance proteins, chiefly MRP1, MRP2, and MRP3 (34–36). Thus ongoing development of newer formulations of ETP with less toxicity that also can circumvent the problem of drug resistance is crucial. One possible solution is the use of drug delivery systems that can specifically deliver anticancer drugs solely to tumor tissues. ETP entrapped in liposomes has been found to be an effective application of this method (19,24). Liposomes are lipid-based vesicles that enable efficient and targeted delivery of drugs to the desired site (15,17). Moreover, liposomized anti-cancer formulations can circumvent drug efflux and achieve adequate drug concentrations in the target cells to enable tumor cell killing, because liposome-mediated disposition interacts well with drug efflux mediated by p-glycoprotein transporters (37–41).
We attempted to further enhance the therapeutic efficacy of liposomal ETP by the incorporation of the immunomodulator tuftsin. Immunomodulators are biological response modifiers and can also exert antitumor effects by improving host defense mechanisms against the tumor. Tuftsin has been shown to have antiproliferative effects on tumor cells and also enhance the ability of the host to tolerate damage by toxic chemicals that may be used to destroy the cancer cells (42,43). Immunomodulatory therapy could thus provide an alternative to conventional chemotherapy for a variety of disease conditions, especially when host defense mechanisms are impaired and need appropriate activation. To suppress tumors in vivo, macrophages must first infiltrate to the desired site. It is well documented that the presence of inflammatory macrophages in growing tumors is maintained through recruitment of circulating monocytes (44–47) and in certain tumors, the proliferation of mononuclear phagocytes (48). Activated macrophages can destroy syngeneic, allogeneic, and xenogeneic tumor cells but leave normal nontumorigenic cells unharmed, suggesting that histocompatibility and tumor-specific antigens are not involved in this recognition (49). In addition, differences in metastatic potential, chromosome number, resistance to chemotherapeutic agents, or the antigenic properties of tumor cells did not appear to be important factors for macrophage recognition of tumor cells (50,51). Successful treatment of metastases by the intravenous injection of liposomes containing immunomodulators has been reported for several tumor-host models, including mouse fibrosarcoma (52–55), melanomas (56,57), lung carcinoma (58), and colon carcinoma (59). Macrophages are believed to migrate to local regions of inflammation and the sites of tumor growth, where they induce further immune reactivity against tumor cells. The treatment of tumors could be achieved by first delivering the drug to the RES and concomitant activation of their components (eg, macrophages) for their tumoricidal activity by a desirable immunomodulator. Being particulate in nature, liposomes are avidly taken up by macrophages that act as secondary depots of the drug. After reaching the tumor site these macrophages release the drug and thereby bring about tumor cell death. At the outset, we speculated that our novel formulation comprising the immunomodulator tuftsin grafted on the surface of liposomes along with ETP would be able to eliminate fibrosarcoma in Swiss albino mice.
In our previous studies, we have demonstrated that pretreatment with liposomized tuftsin led to the successful elimination of a range of pathogens in leukopenic mice (27,60,61). The antitumor activity of tuftsin has long been recognized, but no evaluation has been made of the therapeutic potential of its liposomized form or a tuftsin-bearing liposomal preparation of any anticancer agent. In the present study, we evaluated the anticancer potential of Tuft-Lip-ETP against experimental fibrosarcoma because ETP has cytotoxic properties and the immunomodulator tuftsin possesses both antitumor and immunomodulatory properties to coactivate immune system. Our results are well in agreement with our hypothesis, because this novel formulation of liposomized ETP with tuftsin grafted on the surface was found to be more effective than its free form. MDD studies also demonstrated increased life span in animals treated with Tuft-Lip-ETP. More importantly, significant tumor regression was also found in the animals treated with Tuft-Lip-ETP. Enhanced efficacy of tuftsin-bearing ETP liposomes might be due to the fact that tuftsin helps in specific targeting to macrophages that will subsequently infiltrate to the tumor site. Treatment with free ETP and Sham-Tuft-Lip were not very effective in killing tumor cells.
The tumor suppressor gene p53 is regarded as a key factor in maintaining the balance between cell growth and cell death (62,63) and is reported to be mutated in ~80% of all human malignancies (64). Because of its role in regulation of the cell cycle, alterations in p53 are critical events in carcinogenesis. Normally, in response to toxic insults p53wt triggers a chain of cell cycle regulatory events to check the proliferation of altered cells and repair or minimize damage (62,63). In tumors, loss of p53wt prevents the activation of this growth control pathway (65). The failure to induce transcription-ally active p53wt plays a role in the unregulated growth of tumors and also in the failure to respond to chemotherapeutic agents, which normally trigger p53wt, and regulates cell cycle arrest or cell death (66). The balance between p53wt and p53mut determines the fate of the cell, and many chemotherapeutic agents are known to exert their anticancer effects by modulating p53wt and p53mut expression levels (67–69). The results of the present study showed increased up-regulation of p53wt and down-regulation of p53mut by liposomal formulations of ETP. ETP acts intrinsically by modulating the balance between p53wt and p53mut protein expression, suppressing p53mut and enhancing tumor suppressor p53wt (2–4,68). As evident from the present study, the effect of ETP on p53wt enhanced and reduced p53mut upon its liposomization along with tuftsin (Figure 6a and 6b).
On the basis of the data of the present study, we conclude that Tuft-Lip-ETP is an effective formulation for treatment of fibrosarcoma and can pave the way for treatment of other forms of cancer. Moreover it is imperative to speculate that formulation of tuftsin-bearing liposomes in combination with other anticancer drugs may be equally effective against various form of cancer.
ACKNOWLEDGMENTS
We thank our coordinator, Professor M Saleemuddin, for his support and encouragement throughout the study. We are also thankful to the ITRC director, Dr. C M Gupta, and Dr. Y Shukla for their help in the initial phase of the study. Arif Khan acknowledges ICMR for a Senior Research Fellowship.
Footnotes
Online address: http://www.molmed.org
REFERENCES
- 1.Hande KR. Etoposide: four decades of development of a topoisomerase II inhibitor. Eur J Cancer. 1998;34:1514–21. doi: 10.1016/s0959-8049(98)00228-7. [DOI] [PubMed] [Google Scholar]
- 2.Spurgers KB, Gold DL, Coombes KR, et al. Identification of cell cycle regulatory genes as principal targets of p53-mediated transcriptional repression. J Biol Chem. 2006;281(35):25134–42. doi: 10.1074/jbc.M513901200. [DOI] [PubMed] [Google Scholar]
- 3.Natalie OK, Tafani M, Rothman RJ, Russo MA, Farber JL. The course of etoposide-induced apoptosis from damage to DNA and p53 activation to mitochondrial release of cytochrome c. J Biol Chem. 2002;277:16547–52. doi: 10.1074/jbc.M110629200. [DOI] [PubMed] [Google Scholar]
- 4.Huang Y, Chan AML, Liu Y, Wang X, Holbrook NJ. Serum withdrawal and etoposide induce apoptosis in human lung carcinoma cell line A549 via distinct pathways. Apoptosis. 1997;2:199–206. doi: 10.1023/a:1026420616484. [DOI] [PubMed] [Google Scholar]
- 5.Smit EF, Carney DN, Harford P, Sleijfer DT, Postmus PE. A phase II study of oral etoposide in elderly patients with small cell lung cancer. Thorax. 1989;44:631–3. doi: 10.1136/thx.44.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dollery C. Etoposide. In: Dollery C, editor. Therapeutic Drugs. London, UK: Churchill Livingstone; 1999. pp. E103–E108. [Google Scholar]
- 7.Williams SD, Birch R, Einhorn LH, Irwin L, Greco FA, Loehrer PJ. Treatment of disseminated germ-cell tumors with cisplatin, bleomycin, and either vinblastine or etoposide. N Engl J Med. 1987;316:1435–40. doi: 10.1056/NEJM198706043162302. [DOI] [PubMed] [Google Scholar]
- 8.Sinkule JA. Etoposide: a semisynthetic epipodophyllotoxin. Chemistry, pharmacology, pharmacokinetics, adverse effects and use as an antineoplastic agent. Pharmacotherapy. 1984;4:61–73. doi: 10.1002/j.1875-9114.1984.tb03318.x. [DOI] [PubMed] [Google Scholar]
- 9.Postmus PE, Mulder NH, Sleijfer DT, Meinesz AF, Vriesendorp R, de Vries EG. High-dose etoposide for refractory malignancies: A phase I study. Cancer Treat Rep. 1984;68:1471–4. [PubMed] [Google Scholar]
- 10.Hande KR. Etoposide pharmacology. Semin Oncol. 1994;19(13):3–9. [PubMed] [Google Scholar]
- 11.O’Dwyer PJ, Weiss RB. Hypersensitivity reactions induced by etoposide. Cancer Treat Rep. 1984;68:959–61. [PubMed] [Google Scholar]
- 12.Marina NM, Cochrane D, Harney E, et al. Dose escalation and pharmacokinetics of pegylated liposomal doxorubicin (doxil) in children with solid tumors: a pediatric oncology group study. Clin Cancer Res. 2002;8:413–8. [PubMed] [Google Scholar]
- 13.Batist G, Ramakrishnan G, Rao CS, et al. Reduced cardiotoxicity and preserved antitumor efficacy of liposome-encapsulated doxorubicin and cyclophosphamide compared with conventional doxorubicin and cyclophosphamide in a randomized, multicenter trial of metastatic breast cancer. J Clin Oncol. 2001;19:1444–54. doi: 10.1200/JCO.2001.19.5.1444. [DOI] [PubMed] [Google Scholar]
- 14.Chidiac T, Budd GT, Pelley R, et al. Phase II trial of liposomal doxorubicin (Doxil) in advanced soft tissue sarcomas. Investig New Drugs. 2000;18:253–9. doi: 10.1023/a:1006429907449. [DOI] [PubMed] [Google Scholar]
- 15.Gabizon A, Martin F. Polyethylene glycol-coated (pegylated) liposomal doxorubicin: rationale for use in solid tumours. Drugs. 1997;54:15–21. doi: 10.2165/00003495-199700544-00005. [DOI] [PubMed] [Google Scholar]
- 16.Gabizon A. Selective tumor localization and improved therapeutic index of anthracyclines encapsulated in long-circulating liposomes. Cancer Res. 1992;52:891–6. [PubMed] [Google Scholar]
- 17.Vaage J, Mayhew E, Lasic D, Martin F. Therapy of primary and metastatic mouse mammary carcinomas with doxorubicin encapsulated in long circulating liposomes. Int J Cancer. 1992;5:942–8. doi: 10.1002/ijc.2910510618. [DOI] [PubMed] [Google Scholar]
- 18.Tyagi P, Sengupta S, Velpandian T, Gupta YK, Kochupillai V, Gupta SK. Evaluations of the antitumour activity of liposomal formulations of etoposide against choriocarcinoma xenograft in Balb/c nu/nu mice. Pharm Pharmacol Commun. 1999;5:595–8. [Google Scholar]
- 19.Sengupta S, Velpandian T, Sapra P, Sanyal M, Gupta SK. Etoposide encapsulated long circulating liposomes: improved antitumour efficacy with reduced adverse effects. Naunyn Schmeideberg’s Arch Pharmacol. 1998;358:R531. [Google Scholar]
- 20.Yuan F, Leunig M, Huang SK, Berk DA, Papahadjopoulos D, Jain RK. Microvascular permeability and interstitial penetration of sterically stabilized (stealth) liposomes in a human tumor xenograft. Cancer Res. 1994;54:3352–6. [PubMed] [Google Scholar]
- 21.Papahadjopoulos D, Allen TM, Gabizon A, et al. Sterically stabilized liposomes: Improvements in pharmacokinetics and antitumor therapeutic efficacy. Proc Natl Acad Sci US A. 1991;88:11460–4. doi: 10.1073/pnas.88.24.11460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nishioka K, Amoscato AA, Babcock GF. Tuftsin: a hormone-like tetrapeptide with antimicrobial and antitumor activities. Life Sci. 1981;28:1081–90. doi: 10.1016/0024-3205(81)90684-6. [DOI] [PubMed] [Google Scholar]
- 23.Nishioka K, Babcock GF, Phillips JH, Banks RA, Amoscato AA. In vivo and in vitro antitumor activities of tuftsin. Ann N Y Acad Sci. 1983;419:234–41. doi: 10.1111/j.1749-6632.1983.tb37109.x. [DOI] [PubMed] [Google Scholar]
- 24.Sengupta S, Tyagi P, Chandra S, Kochupillai V, Gupta SK. Encapsulation in cationic liposomes enhances antitumour efficacy and reduces the toxicity of etoposide, a topoisomerase II inhibitor. Pharmacology. 2001;62:163–71. doi: 10.1159/000056090. [DOI] [PubMed] [Google Scholar]
- 25.Owais M, Krishnakumar B, Jain RK, Bachhawat BK, Gupta CM. Tuftsin bearing liposomes as drug vehicles in the treatment of experimental aspergillosis. FEBS Lett. 1993;326:56–8. doi: 10.1016/0014-5793(93)81760-w. [DOI] [PubMed] [Google Scholar]
- 26.Gupta CM, Puri A, Jain RK, Bali A, Anand N. Protection of mice against P. berghei infection by a tuftsin derivative. FEBS Lett. 1986;205:351–4. doi: 10.1016/0014-5793(86)80927-9. [DOI] [PubMed] [Google Scholar]
- 27.Khan MA, Faisal SM, Haque W, Owais M. Immunomodulator tuftsin augments antifungal activity of amphotericion B against experimental murine candidiasis. J Drug Target. 2002;10(3):185–92. doi: 10.1080/10611860290022615. [DOI] [PubMed] [Google Scholar]
- 28.Owais M, Gupta CM. Liposome mediated cytosolic delivery of macromolecules and its possible use in vaccine development. Eur J Biochem. 2000;267:3946–56. doi: 10.1046/j.1432-1327.2000.01447.x. [DOI] [PubMed] [Google Scholar]
- 29.Faiderbe S, Chagnaud JL, Geffard M. Identification and characterization of a specific autoantiphosphatidylinositol immune response during the time course of benzo (a) pyrene-induced malignant tumors in female Sprague-Dawley rats. Cancer Res. 1992;52:2862–5. [PubMed] [Google Scholar]
- 30.Corbett TH, Roberts BJ, Leopold WR, Peckham JC, Wilkoff LJ, Griswold DP, Jr, Schabel FM., Jr Induction and chemotherapeutic response of two transplantable ductal adenocarcinomas of the pancreas in C57BL/6 mice. Cancer Res. 1984;44:717–26. [PubMed] [Google Scholar]
- 31.Serpi R, Piispala J, Jarvilehto M, Vahakangas K. Thapsigargin has similar effect on p53 protein response to benzo (a) pyrene DNA adducts as TPA in mouse skin. Carcinogenesis. 1999;20:1755–60. doi: 10.1093/carcin/20.9.1755. [DOI] [PubMed] [Google Scholar]
- 32.Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci U S A. 1979;76:4350–4. doi: 10.1073/pnas.76.9.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lowry OH, Rosenbrough NK, Farr AL, Randall RJ. Protein measurement with folin phenol reagent. J Biol Chem. 1951;193:265–75. [PubMed] [Google Scholar]
- 34.Borst P, Evers R, Kool M, Wijnholds J. A family of drug transporters: the multidrug resistance-associated proteins. J Nat Cancer Inst. 2000;92(16):1295–302. doi: 10.1093/jnci/92.16.1295. [DOI] [PubMed] [Google Scholar]
- 35.Zelcer N, Saeki T, Reid G, Beijnen JH, Borst P. Characterization of drug transport by the human multidrug resistance protein 3 (ABCC3) J Biol Chem. 2001;276(49):46400–7. doi: 10.1074/jbc.M107041200. [DOI] [PubMed] [Google Scholar]
- 36.Guo A, Marinaro W, Hu P, Sinko PJ. Delineating the contribution of secretory transporters in the efflux of etoposide using Madin-Darby canine kidney (MDCK) cells over-expressing P-glycoprotein (Pgp), multidrug resistance-associated protein (MRP1), and canalicular multispecific organic anion transporter (cMOAT) Drug Metab Dispos. 2002;30(4):457–63. doi: 10.1124/dmd.30.4.457. [DOI] [PubMed] [Google Scholar]
- 37.Candoni A, Michelutti A, Simeone E, Damiani D, Baccarani M, Fanin R. Efficacy of liposomal daunorubicin and cytarabine as reinduction chemotherapy in relapsed acute lymphoblastic leukemia despite expression of multidrug resistance related proteins. Eur J Haematol. 2006;77:293–9. doi: 10.1111/j.1600-0609.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 38.Sadava D, Coleman A, Kane SE. Liposomal daunorubicin overcomes drug resistance in human breast, ovarian and lung carcinoma cells. J Liposome Res. 2002;12:301–9. doi: 10.1081/lpr-120016196. [DOI] [PubMed] [Google Scholar]
- 39.Lo YL, Liu FI, Yang JM, Cherng JY. Reversal of multidrug resistance to epirubicin by cyclosporin A in liposomes or intralipid. Anticancer Res. 2001;21:445–50. [PubMed] [Google Scholar]
- 40.Lawrence DM, Jennifer AS. The role for liposomal drug delivery in molecular and pharmacological strategies to overcome multidrug resistance. Cancer Metastasis Rev. 2001;20:87–93. doi: 10.1023/a:1013108524062. [DOI] [PubMed] [Google Scholar]
- 41.Poujol S, Tilleul P, Astre C, Martel P, Fabbro M, Pinquet F. Effect of mitoxantrone liposomes on multidrug-resistant breast cancer cells. Anticancer Res. 1999;19:3327–31. [PubMed] [Google Scholar]
- 42.Knyszynski A, Gottilieb B, Fridkin M. Inhibition by tuftsin of Rauscher virus leukemia development in mice. J Nat Cancer Inst. 1983;71:87–90. [PubMed] [Google Scholar]
- 43.Noyes RD, Babcock GF, Nishioka K. Antitumor activity of tuftsin on murine melanoma in vivo. Cancer Treat Rep. 1981;65:673–5. [PubMed] [Google Scholar]
- 44.Bugelski PJ, Cotwon SP, North SM, Kirsh R, Nicolson GM, Poste G. Macrophage content of spontaneous metastases at different stages of growth. Cancer Res. 1987;47:4141–7. [PubMed] [Google Scholar]
- 45.Bugelski PJ, Kirsh R, Ruscarmo C, Cotwin SP, Poste G. Recruitment of exogeneous macrophages into metastases at different stages of tumor growth. Cancer mmunol Immunother. 1987;24:93–8. doi: 10.1007/BF00205584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Evans R, Cullen RT. In situ proliferation of intratumor macrophages. J Leuk Biol. 1984;35:561–8. doi: 10.1002/jlb.35.6.561. [DOI] [PubMed] [Google Scholar]
- 47.Normann SJ. Macrophage infiltration and tumor progression. Cancer Metastasis Rev. 1985;4:277–91. doi: 10.1007/BF00048093. [DOI] [PubMed] [Google Scholar]
- 48.Mantovani A. Tumor-associated macrophages. Curr Opin Immunol. 1990;2:689–94. doi: 10.1016/0952-7915(90)90031-b. [DOI] [PubMed] [Google Scholar]
- 49.Fidler IJ, Schroit AJ. Recognition and destruction of neoplastic cells by activated macrophages: discrimination of altered self. Biochim Biophys Acta. 1988;948:151–73. doi: 10.1016/0304-419x(88)90009-1. [DOI] [PubMed] [Google Scholar]
- 50.Killion JJ, Radinsky RR, Dong Z, Fishbeck R, Whitworth P, Fidler IJ. The immunogenic properties of drug resistant murine tumor cells do not correlate with expression of the MDR phenotype. Cancer Immunol Immunother. 1993;36:381–6. doi: 10.1007/BF01742254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pak CC, Fidler IJ. Activated macrophages distinguish undifferentiated-tumorigenic from differentiated-nontumorgenic murine erythroleukemia cells. Differentiation. 1989;41:49–55. doi: 10.1111/j.1432-0436.1989.tb00731.x. [DOI] [PubMed] [Google Scholar]
- 52.Fidler IJ. Optimization and limitations of systemic treatment of murine melanoma metastasis with liposomes containing muramyl tripeptide phosphatidylethanolamine. Cancer Immunol Immunother. 1986;21:169–73. doi: 10.1007/BF00199357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Deodhar SD, James K, Chiang T, Barna BP. Inhibition of lung metastasis in mice bearing a malignant fibrosarcoma by treatment with liposomes containing human C-reactive protein. Cancer Res. 1982;42:5084–91. [PubMed] [Google Scholar]
- 54.Eppstein DA, Vander Pas MA, Fraser-Smith EB. Liposome-encapsulated muramyl dipeptide analogue enhances non-specific host immunity. Int J Immunother. 1986;2:115–26. [Google Scholar]
- 55.Lopez-Berestein G, Milas L, Hunter N, Mehta E, Eppstein D, Vander Pas MA, Mathews TR, Hersh EM. Prophylaxis and treatment of experimental lung metastases in mice after treatment with liposome-encapsulated 6-0-steroyl-N-acetylmuramyl-L-amino-butryl-D-isoglutamine. Clin Exp Metastasis. 1984;2:366–7. doi: 10.1007/BF00052413. [DOI] [PubMed] [Google Scholar]
- 56.Phillips NC, Mora ML, Chedid L, Lefrancier P, Bernard JM. Activation of tumoricidal activity and eradication of experimental metastases by freeze-dried liposomes containing a new lipophilic muramyl dipeptide derivative. Cancer Res. 1985;39:2582–90. [PubMed] [Google Scholar]
- 57.Phillips NC, Tsao MS. Inhibition of experimental liver tumor growth in mice by liposomes containing a lipophilic muramyl dipeptide derivative. Cancer Res. 1989;49:936–9. [PubMed] [Google Scholar]
- 58.Brodt P, Blore J, Philips NC, Munzer JS, Rioux JD. Inhibition of murine hepatic tumor growth by liposomes containing a lipophilic muramyl dipeptide. Cancer Immunol Immunother. 1989;28:54–60. doi: 10.1007/BF00205801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thrombe P, Deodhar SD. Inhibition of liver metastasis in murine colon adenocarcinoma by liposomes containing human C-reactive protein or crude lymphokine. Cancer Immunol Immunother. 1984;16:145–50. doi: 10.1007/BF00205420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Khan MA, Arif K, Owais M. Prophylactic use of liposomized tuftsin enhances the susceptibility of Candida albicans to fluconazole in leukopenic mice. FEMS Immunol Med Microbiol. 2005;46(1):63–9. doi: 10.1111/j.1574-695X.2005.00014.x. [DOI] [PubMed] [Google Scholar]
- 61.Khan MA, Nasti TH, Khanam S, et al. Coadministration of immunomodulator tuftsin and liposomisednystatin can combat less susceptible Candida albicans infection in temporarily neutropenic mice. FEMS Immunol Med Microbiol. 2004;41:249–58. doi: 10.1016/j.femsim.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 62.Agarwal ML, Taylor WR, Chernov MV, Chernova OB, Stark GR. The p53 network. J Biol Chem. 1998;273:1–4. doi: 10.1074/jbc.273.1.1. [DOI] [PubMed] [Google Scholar]
- 63.Mowat MR. p53 in tumor progression: life, death and everything. Adv Cancer Res. 1993;74:25–48. doi: 10.1016/s0065-230x(08)60764-2. [DOI] [PubMed] [Google Scholar]
- 64.Hollstein M, Sidransky D, Vogelstein B, Harris CC. p53 mutations in human cancers. Science. 1991;253:49–53. doi: 10.1126/science.1905840. [DOI] [PubMed] [Google Scholar]
- 65.Burns PA, Kemp CJ, Gannon JV, Lane DP, Bremmer R, Balmain A. Loss of heterozygosity and mutational alterations of the p53 gene in skin tumors of interspecific hybrid mice. Oncogene. 1991;6:2363–9. [PubMed] [Google Scholar]
- 66.El-Deiry WS, Harper JW, O’Connor PM, et al. WAFI/CIPI is induced in p53 mediated G1 arrest and apoptosis. Cancer Res. 1994;54:1169–74. [PubMed] [Google Scholar]
- 67.Skvortsova I, Poper BA, Akvortsov S, et al. Pretreatment with Rituximab enhances radiosensitivity of non-Hodgkin’s lymphoma cells. J Radiation Res. 2005;46:241–8. doi: 10.1269/jrr.46.241. [DOI] [PubMed] [Google Scholar]
- 68.Takimoto R, Wang W, Dicker DT, Rastinejad F, Lyssikatos J, El-Deiry WS. The mutant p53-conformation modifying drug, CP-31398, can induce apoptosis of human cancer cells and can stabilize wild-type p53 protein. Cancer Biol Ther. 2002;1:47–55. doi: 10.4161/cbt.1.1.41. [DOI] [PubMed] [Google Scholar]
- 69.Bunz F, Hwang PM, Torrance C, et al. Disruption of p53 in human cancer cells alters the responses to therapeutic agents. J Clin Invest. 1999;104:263–9. doi: 10.1172/JCI6863. [DOI] [PMC free article] [PubMed] [Google Scholar]