Abstract
The iron status of African-American infants continues to be subject to debate. We characterized the iron status of 198 9-month-old inner-city infants (94% fed iron-fortified formula) using a comprehensive panel of measures and assessing lead and inflammation markers. The proportion with iron deficiency was calculated based on three approaches (≥ 2 abnormal iron measures with or without anemia for MCV model—NHANES II, ferritin model—NHANES III, or Sweden/Honduras study) and a promising new measure—body iron, calculated from ferritin and transferrin receptor (TfR). There were no sex differences for any iron measure. Hb < 110 g/l was observed in 25%; Hb ≤ 105 g/l in 10.1%. Free erythrocyte protoporphyrin (FEP) values were elevated without elevated lead concentrations or an inflammatory response: mean FEP = 86.6 μg/dl red blood cells [75.5 μmol/mol heme]; 52.3% were > 80 μg/dl (1.42 μmol/l), almost half of which were accompanied by a second abnormal iron measure. The estimated prevalence of iron deficiency was 14.4, 5.3, and 2.5% for the MCV model, ferritin model, and Sweden/Honduras cutoffs, respectively, and 4.1% for body iron < 0 mg/kg. Regulation of iron storage is immature at < 1 year of age, making estimates of iron deficiency that depend on ferritin, including body iron, suspect in this age period. Thus, the “true” prevalence of iron deficiency could not be established with confidence due to major differences in the results, depending on the guidelines used. Functional indicators of poor iron status in young infants are urgently needed.
Keywords: iron deficiency, anemia, infants, African-American, erythrocyte protoporphryrin, body iron
INTRODUCTION
There is no doubt that the iron status of US infants and toddlers has improved in the last several decades [1–5]. For instance, in the latest published national survey (National Health and Nutrition Examination Survey III or NHANES III, 1988–1994) [6], the prevalence of iron deficiency anemia and iron deficiency overall (with or without anemia) in 1- to 2-year-olds was quite low (3 and 9%, respectively).
Despite dramatic improvement, iron deficiency is more common among some groups. Further analysis of NHANES III data showed a higher nationwide prevalence of iron deficiency with or without anemia among poor or minority toddlers or both, compared with that among non-poor whites (Ogden cited in Ref. 7) [8]. A study that focused specifically on such children reported iron deficiency anemia in 10% of 1- to 3-year-olds drawn from a cross-section of pediatric practices in the New York City area, with an ethnically mixed population (primarily black and Hispanic) [9]. Another study among 9- to 30-month-old predominantly black infants in inner-city Baltimore reported iron deficiency anemia in 8% [10]. However, direct comparisons across these and other studies are problematic, as the models to define iron deficiency often differ between studies.
To try to clarify the iron status of inner-city black infants, a recent study in Baltimore examined response to iron therapy [11], because an increase in hemoglobin (Hb) following iron supplementation or therapy can confirm iron deficiency [5,12]. Even though anemia (defined as Hb < 110 g/l) was observed in 25% of the infants, there was little or no response to iron therapy. One interpretation is that the anemia was not due to iron deficiency. Another is that the definition of “anemia” was inappropriate, since Hb concentrations are somewhat lower, on average, among blacks than whites, [13–16] which could result in “nonresponders” who were really not anemic to begin with. However, the study noted serious limitations (e.g., administration of iron therapy was unmonitored, only 36% were reassessed within 3 months, etc.). Thus, failure to respond could be due to methodologic and not substantive issues.
In addition to issues specific to African-Americans, identifying individuals with iron deficiency continues to present a number of challenges, especially in infants. Despite general agreement with the concepts that iron deficiency exists when the iron supply is inadequate for normal synthesis of essential iron compounds or hemoglobin increases in response to iron therapy [17,18], detecting iron deficiency is not straightforward. Commonly utilized measures of iron status index iron storage pools (ferritin), iron transport (serum iron, transferrin saturation), or adequacy of delivery of iron to bone marrow (Hb, MCV, RDW, FEP, TfR). They must be considered in combination in order to have a strong predictive value in the diagnosis of iron deficiency [19], and some may be affected by other factors such as time of day, inflammation, thalassemia trait, or other hemoglobinopathies, etc. [5,20–24], as well as age and gender. For the past 2 decades or so, it has been common practice in research studies to define iron deficiency as two or more iron measures in the deficient range. However, consensus guidelines do not agree about the combination of measures or cutoffs [6,15,25,26], and few address definitions of iron sufficiency or insufficiency in infants < 1 year of age.
Highlighting this point, the Committee on Nutrition of the European Society of Pediatric Gastroenterology, Hepatology, and Nutrition noted that “more appropriate cutoff values to define anemia in infants and young children are necessary and that current prevalence data must be interpreted with caution” [27]. Others have concurred [28]. Domellöf et al. further challenged existing guidelines, using data from 9- to 12-month-old breast-fed infants in Sweden and Honduras to argue that available cutoffs are incorrect for such babies [29].
A relatively new iron status indicator—body iron—promises to improve detection of iron deficiency by capturing the full spectrum of iron status across individuals and at the population level. This index, proposed by Cook et al. [30], is based on a quantitative evaluation of how ferritin and TfR changed in adults as known amounts of iron were removed from their bodies by phlebotomy [31]. However, its use with infants has been reported in only one study to date [32].
Our study focused on iron deficiency among African-American infants under 1 year of age from an economically-stressed inner-city population. Based on a comprehensive panel of iron status indicators, including such newer measures as transferrin receptor (TfR) and body iron, we used different guidelines to characterize the iron status of 9-month-old infants—at the beginning of the recommended window for anemia screening [33]. Due to widespread participation in the Women, Infants, and Children (WIC) program, we expected that iron deficiency would be uncommon in the population at this age.
MATERIALS AND METHODS
Subjects
Nine-month-old infants presenting for a health maintenance visit at the General Pediatric Clinic of Children’s Hospital of Michigan, Wayne State University, Detroit were contacted in the course of an ongoing study of the effects of iron deficiency on brain and behavior (protocol approved by the Institutional Review Boards at Wayne State University and University of Michigan). Signed informed consent was obtained separately for the screening phase of the project, which consisted of a brief questionnaire and an extra tube of blood for additional iron status measures, obtained at the time of the baby’s routine blood sample. Over a 12-month period (2002–2003), the mothers/caregivers of 316 infants in this age range were contacted on their routine health maintenance visit. Ninety percent (n = 285) agreed to screening. In some cases, technical difficulties prevented the blood sample from being obtained or analyzed, and in others, the child’s health care provider did not order blood drawn at the visit. As a result, blood samples were available for 232 infants. There were no differences between the infants with blood work and the 53 babies without in terms of gender, birth weight, gestational age, birth by Cesarean section or maternal age, education, and marital status. However, infants without blood work had been hospitalized somewhat more often and their mothers had more children (P values < 0.05).
Children were excluded from this analysis if they had received medicinal iron drops (n = 15), had a lead concentration ≥ 10 μg/dl (0.5 μmol/l) (n = 2), or a major congenital anomaly (n = 1), were not African-American (n = 20), or were in foster care (n = 7). The sample was restricted to African-Americans because over 90% of the clinic population was black and the remainder varied widely in ethnic origin. Infants in foster care were excluded since details of the infant’s medical and feeding history were unknown. These exclusions resulted in a final sample for analysis consisting of 198 infants. Infants with HIV/AIDS, sickle cell disease, or other major hemoglobinopathies received care in specialty clinics and were not part of the sample.
Characteristics of the final sample are shown in Table I. Infants weighed 3.26 kg at birth, on average, with 12% < 2.50 kg. Eighteen percent had been born by Cesarean section. All but 6 births (3%) were singleton; four of the twins were low birth weight or premature. Almost all babies (94%) were fed formula with iron, although mothers of 33% of the infants reported at least some breastfeeding (18 weeks on average). None of the mothers reported having started their infants on unmodified cow milk. Mothers averaged 25 years of age, and only 9 (4.5%) were <18. Virtually all mothers and infants participated in the WIC program. The infants were covered primarily by Medicaid insurance, and most of the mothers were single (85%). Almost half the mothers had some education beyond high school, often vocational courses or other training.
TABLE I.
Sample Description
| Infant characteristics | |
| Gender (female) | 54% (107) |
| Birth weight (kg) | 3.26 ± 0.73 |
| Premature (<37 weeks) | 10% (20) |
| Low birth weight (<2.5 kg) | 12% (23) |
| Cesarean section | 18% (36) |
| Formula with iron | 94% (185) |
| Some breast feeding | 33% (66) |
| If breast fed, duration (weeks) | 18.5 ± 12.9 |
| Family characteristics | |
| Mother’s age (years) | 25.3 ± 5.9 |
| Teen birth (<18 years) | 4.5% (9) |
| Number of children | 1.8 ± 1.0 |
| Marital status (married) | 15% (29) |
| Mother’s education (years) | 12.8 ± 1.5 |
| Type of insurance (Medicaid) | 87% (172) |
Values are percent (number) for categorical variables and mean ± SD for continuous variables.
Procedures
A 10-min questionnaire was administered to the mother/caregiver in the examination room as families waited to see the doctor. Questions covered demographics, birth history, dietary history, and medical history.
An experienced clinic phlebotomist obtained up to 5 ml of venous blood. Routine blood tests included a complete blood count with red cell indices, lead, and free erythrocyte protoporphyrin (FEP) or zinc protoporphyrin/heme ratio (ZPP/H) or both. An extra tube of blood was obtained whenever possible, promptly centrifuged and frozen at −20°C for subsequent determination of serum transferrin saturation, ferritin, transferrin receptor (TfR) and biochemical markers of inflammation (α1-acid glyco-protein [AGP] and quantitative C-reactive protein [CRP]) in the laboratory of John Beard, Pennsylvania State University. Because blood collection occurred in conjunction with routine clinic visits, samples varied in time of day.
All measures assessed iron status except for CRP, AGP, and lead. These were obtained to assess factors that can alter iron status measures in the absence of iron deficiency. For instance, inflammation/infection can be accompanied by decreased Hb and increased ferritin. CRP rises rapidly in response to inflammation and decreases toward normal within 36–48 hr, whereas both ferritin and AGP may remain elevated for as long as 5–10 days after the onset of an acute inflammatory response [34,35]. Lead concentrations above 15–18 μg/dl can impair red cell production, reflected in elevated FEP values [36].
The Detroit Medical Center University Laboratories performed the hematologic and lead assays. Complete blood counts were performed with a Beckman Coulter Max-M instrument or a Sysmex SE-900 automated counter. Cell counters were calibrated daily with normal clinical quality controls. The agreement between cell counters was 0.99 for the variables of interest. Lead was measured by atomic absorption using a graphite furnace [37]. ARUP Laboratories, Salt Lake City, UT performed the FEP determinations; specimens were immediately wrapped in foil to prevent heme degradation by light and preserved at −20°C until analysis. FEP was assayed by extraction followed by fluorometric measurement. Part-way through the study, it became possible to perform ZPP/H determinations on site (ZP Hematofluorometer, Model 206D, AVIV Associates, NJ). Both FEP and ZPP/H were determined for the remainder of the year. As in NHANES II and III, red cells were not washed. All laboratories maintained strict quality control using internal and external standards.
Serum ferritin measurement was based on radioimu-nometric assay (Dipontics Corporation, Los Angeles, CA). Combined measurement of ferritin, soluble transferrin receptor, and C-reactive protein was performed by a sandwich enzyme-linked immunosorbent assay technique [38]. AGP was measured by a quantitative immunodiffusion assay (Kent Laboratories, Bellingham, WA). The external standard for ferritin consisted of the IBS standard diluted to 19.2 μg/l ferritin. The coefficient of variation for within assay-variation was <4.5% for all ELISA assays, with a between-batch coefficient of variation of 6.2–7.4%. For AGP and CRP, within-batch variation was <3% and between batches, it was <5%.
All infants had data for Hb, MCV (mean cell volume), and RDW (red cell distribution width). Eighty-seven per cent (172/198) had determinations for FEP. ZPP/H was available for 128 infants, 120 of whom also had FEP. Combined, 180 infants had FEP or ZPP/H or both. In reporting results, we focus on FEP due to the higher number of assessments and its use in NHANES. However, FEP results in μg/dl red blood cells are also expressed as μmol/mol heme for ease of consideration in relation to ZPP/H, which is currently recommended [39]. Values for transferrin saturation, ferritin, TfR, and body iron were available for 141–147 infants (71–74%). A total of 132 infants had complete data for the measures used to determine iron status in NHANES II or III (i.e., Hb, MCV, FEP, transferrin saturation, and ferritin). Missing data were due to technical problems, such as trouble obtaining sufficient blood. Children with missing values had somewhat lower MCV and higher RDW values than children with a full set of measures (P values < 0.05).
Quantitative CRP and AGP data were available for 139 and 142 infants, respectively. AGP > 130 mg/l or CRP > 3 mg/l or both were considered to indicate inflammation.
Describing Iron Status
Iron status was examined in three ways.
Hb and iron measures were described as continuous variables and compared with data for African-American infants in NHANES III. From the NHANESIII database [40], we extracted data for infants most similar to those in our sample. Specifically, we selected African-American infants 12–23 months of age with lead concentrations < 10 μg/dl (n = 178).
The prevalence of iron deficiency and iron deficiency anemia among study infants was determined according to three different expert sources with different recommendations for measures and cutoffs: MCV model—NHANES II [25], ferritin model—NHANES III [6], and the Sweden/Honduras study [29]. The following strategy was employed: the percentage of infants with values indicative of iron deficiency was calculated for each parameter based on the cutoffs for a given source; the number of abnormal iron measures was determined for each infant for each set of cutoffs; and the proportion of the sample with two or more abnormal iron measures (our criterion for iron deficiency) was calculated. A lower cutoff for defining anemia among blacks is sometimes recommended [14,41]. Therefore, we calculated the prevalence of anemia and iron deficiency anemia at both Hb < 110 g/l and lower concentrations (<105 g/l or < 100 g/l). Anemia was defined as Hb below cutoff and iron deficiency anemia as the combination of a low Hb concentration and two or more abnormal iron measures. It should be noted that infants in our study were younger than the 1- to 2-year age range covered by NHANES surveys. However, we considered NHANES cutoffs to be applicable, since previous research has shown little or no differences in the 6- to 24-month age range for Hb, MCV, FEP, transferrin saturation, or ferritin [42–44].
The final approach was to compute the body iron content in mg iron/kg of body weight based on the algorithm published by Cook et al. [30]. We then computed the cumulative distribution of body iron and utilized body iron < 0 mg/kg as another definition of “iron deficiency” in assessing prevalence.
Statistics
The Student t test was used to test for differences between the Detroit sample and African-American 1-year-olds in NHANES III. This statistic was also used to test for differences in iron status measures related to gender or other conditions that might affect iron status or iron measures or both. The Chi square test was used to test differences in dichotomous variables. In light of missing data for some iron measures, proportions were calculated with the denominator being the number with available data for a given parameter. All statistical analyses were performed using SAS for Windows, version 9.1 (SAS Institute, Cary, NC).
RESULTS
The mean, standard deviation, and range for Hb and iron measures are shown in Table II. The severity of anemia was generally mild, with the lowest Hb being 95 g/l and a prevalence of anemia of 25.3, 10.1, or 1.5 at cutoffs < 110 g/l, 105 g/l, or 100 g/l, respectively. Erythrocyte protoporphyrin values were generally elevated. The mean FEP was 86.6 μg/dl red blood cells (75.5 μmol/mol heme), well above the cutoff of 80 μg/dl red blood cells (1.42 μmol/l) considered by NHANES and the Centers for Disease Control (CDC) to be the upper limit of normal for age [6,25,26]. ZPP/H values were also high. The mean ZPP/H was 82.5 μmol/mol heme (94.6 μg/dl red blood cells). Higher values for ZPP/H were expected, since these were determined in fresh whole blood within 1–2 days, whereas specimens for FEP were frozen and shipped. Nonetheless, the correlation between FEP and ZPP/H was 0.79 for the 120 infants with both assessments, indicating good agreement despite freezing and shipping. Lead concentrations averaged 2.6 μg/dl (0.12 μmol/l), and, by entrance criteria, all values were <10 μg/dl. There were no gender differences on any iron measure, with or without control for birth weight (all P values > 0.12). Comparing infants born prematurely and/or with birth weight < 2.5 kg (n = 20) to the rest of the sample, there were no differences on any iron status measure.
TABLE II.
Hematologic and Biochemical Measures: Detroit Sample vs. African-American 1-Year-Olds in NHANES III
| Detroit sample | NHANES III subsample | |||
|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | |
| Hb (g/l) | 198 | 116.2 ± 9.1 (95.0–137.0)a | 178 | 116.6 ± 8.0 (92.5–143.0)a |
| MCV (fl) | 198 | 77.3 ± 4.6 (63.3–88.2) | 178 | 77.1 ± 5.4 (61.9–90.5) |
| RDW (%)* | 198 | 13.2 ± 1.1 (11.0–20.0) | 178 | 13.5 ± 1.3 (11.2–18.2) |
| FEP (μg/dl red blood cells)** [μmol/mol heme] | 172 | 86.6 ± 32.0 (27–218) [75.5 ± 27.9 (24–190)] | 178 | 61.5 ± 28.3 (27–204) [53.6 ± 24.7 (24–178)] |
| ZPP/H μmol/mol heme | 82.5 ± 29.9 (22–222) | NA | ||
| Transferrin saturation (%)** | 141 | 23.6 ± 9.1 (6.1–52.6) | 178 | 15.6 ± 8.0 (3.0–44.1) |
| Ferritin (μg/l)* | 147 | 37.0 ± 25.3 (2.5–152.4) | 178 | 29.3 ± 37.1 (3–369) |
| TfR (mg/l) | 145 | 5.3 ± 1.7 (2.0–11.2) | NA | |
| Body iron (mg/kg) | 147 | 5.0 ± 2.8 (±6.82–14.25) | NA | |
| AGP (mg/l) | 142 | 76.6 ± 32.8 (26.3–187.1) | NA | |
| CRP (mg/l) | 139 | 0.9 ± 2.0 (0–16.5) | NA | |
| Lead (μg/dl)*** | 167 | 2.6 ± 1.6 (0–8.0) | 178 | 4.8 ± 2.1 (0.7–9.8) |
Significance levels of differences between the Detroit sample and 12- to 23-month-old African-American infants in NHANES III are based on the Student t test.
Values in parentheses indicate range.
P < 0.05,
P < 0.001. NA, not available.
As shown in Table II, the Detroit sample was similar to African-American 1-year-olds (12–23 months) in NHANES III with respect to Hb and MCV. FEP values were 25 μg/dl higher in the Detroit sample (86.6 vs. 61.5 μg/dl red blood cells, P < 0.001). RDW, transferrin saturation, ferritin, and lead were worse in the NHANES subsample (P values 0.03 to <0.001)
The prevalence of iron deficiency was estimated based on the proportion of infants with two or more iron measures in the “abnormal” range as defined by different sources (Table III). The MCV model utilized in NHANES II (FEP, transferrin saturation, and MCV) yielded an estimate of 14.4% iron deficiency overall. The ferritin model utilized in NHANES III (FEP, transferrin saturation, and ferritin) resulted in a considerably lower estimate of 5.3% iron deficiency overall. Corresponding estimates of iron deficiency with anemia were 6.1 and 2.3%, respectively, using Hb < 110 g/l, the cutoff in NHANES II and III. The approach recommended in the Sweden/Honduras study of breast-fed infants at 9–12 months of age, with more stringent cutoffs given for five iron status measures and Hb, yielded prevalence estimates of 2.5% for iron deficiency and 1.5% for iron deficiency anemia. There are as yet no established norms for TfR in infants, but the Sweden/Honduras study considered “abnormal” TfR > 11 mg/l. Only one infant in our study had a value above this cutoff.
TABLE III.
Percent Abnormal in Detroit Sample by Different Iron Status Criteria
| NHANES II
|
NHANES III
|
Sweden/Honduras
|
|||||
|---|---|---|---|---|---|---|---|
| n | Cutoff | % Abnormal (n) | Cutoff | % Abnormal (n) | Cutoff | % Abnormal (n) | |
| Individual iron measures | |||||||
| Hb (g/l) | 198 | <110 | 25.3 (50)a | <110 | 25.3 (50)a | <100 | 1.5 (3)a |
| MCV (fl)b | 198 | <74 | 23.2 (46) | NA | <71 | 8.6 (17) | |
| FEP (μg/dl red blood cells) [μmol/mol heme] | 172 | >80 [>69] | 52.3 (90) | >80 [>69] | 52.3 (90) | >103 [>90] | 23.3 (40) |
| Transferrin saturation | 141 | <12 | 7.8 (11) | <10 | 5.0 (7) | NA | |
| Ferritin (μg/l) | 147 | NA | <10 | 4.8 (7) | <5 | 1.4 (2) | |
| TfR (mg/l) | 145 | NA | NA | >11 | 0.7 (1) | ||
| Iron deficiency/iron deficiency anemia (n) | 132c | 132c | 198 | ||||
| Iron deficiency (≥2 abnormalities) | 14.4 (19) | 5.3 (7) | 2.5 (5) | ||||
| Anemia + iron deficiency | 6.1 (8) | 2.3 (3) | 1.5 (3) | ||||
Values in parentheses indicate number of cases.
As recommended by the CDC (26), the MCV cut-off was 74 fl (instead of 73 fl) to reflect changes in methods for determining hematocrit and possibly red cell counts.
The n for estimating the proportion with iron deficiency or iron deficiency anemia using NHANES criteria was based on infants with complete data for Hb, MCV, FEP, transferrin saturation, and ferritin.
Values for the new body iron index (mg/kg body weight) were normally distributed. The 50th percentile was 5.3 mg/kg, with 4.1% of values < 0 mg/kg (“iron deficient”) (Fig. 1). There was no greater prevalence of low Hb or MCV or elevated FEP in infants with body iron < 0, compared with those between 0 and 1 or between 1 and 2 mg iron/kg (data not shown). Body iron was highly correlated with ferritin (r values = 0.87 for serum ferritin and 0.99 for log ferritin). Among the other iron measures, body iron was modestly related only to Hb and RDW (r values = −0.17 and −0.21, respectively, P < 0.05). Table IV provides correlations among all iron status measures.
Fig. 1.
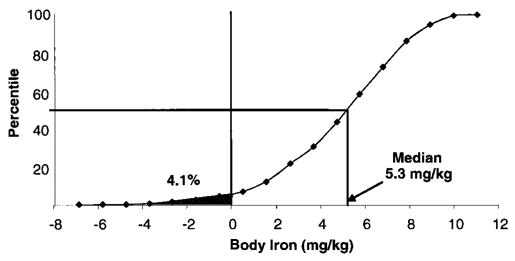
Cumulative distribution plot of body iron in African-American 9-month-old infants. The median body iron (5.3 mg/kg) is shown, along with the proportion with body iron < 0 mg/kg (shaded area), indicating iron deficiency in 4.1%.
TABLE IV.
Correlations (n) Among Measures of Infant Iron Status
| MCV | RDW | Transferrin saturation | Log ferritin | TFR | Body iron | ZPP/H | FEP | |
|---|---|---|---|---|---|---|---|---|
| Hb | 0.29*** (198) | −0.16* (198) | 0.12 (141) | −0.17* (147) | −0.23** (145) | −0.17* (147) | −0.25** (128) | −0.19* (172) |
| MCV | −0.46*** (198) | 0.05 (141) | <0.001 (147) | −0.14 (145) | 0.01 (147) | −0.30*** (128) | −0.13a (172) | |
| RDW | −0.13 (141) | −0.19* (147) | 0.25** (145) | −0.21* (147) | 0.53*** (128) | 0.42*** (172) | ||
| Transferrin saturation | 0.07 (141) | −0.19* (140) | 0.06 (141) | −0.16 (100) | −0.16a (132) | |||
| Log ferritin | −0.05 (145) | 0.99*** (147) | −0.23* (103) | −0.29*** (138) | ||||
| TFR | −0.07 (145) | 0.50*** (101) | 0.30*** (136) | |||||
| Body iron | −0.26*** (103) | −0.29*** (138) | ||||||
| ZPP/H | 0.79*** (120) |
Suggestive trend, p < 0.10.
P < 0.05,
P < 0.01,
P < 0.001.
FEP stands out among the indicators of iron status as showing a high prevalence of values in the range consistent with iron deficiency. As shown in Table IV, FEP (and ZPP/H to an even greater degree) significantly correlated with all iron status measures except transferrin saturation. Correlations with Hb, MCV, log ferritin, and body iron were moderate (r magnitude 0.19–0.30); those for RDW and TfR were considerably higher (r magnitude 0.30–0.53). Over half the infants (52.3%) had values above the NHANES cutoff of 80 μg/dl red blood cells (69 μmol/mol heme), and 23.3% were above the Sweden/Honduras cutoff of 103 μg/dl red blood cells (90 μmol/mol heme). Infants with FEP > 80 μg/dl red blood cells, compared with those with values below cutoff, had lower values for Hb (114 vs. 117 g/l, P < 0.05) and higher values for RDW (13.3 vs. 12.8%, P < 0.001) and TfR (5.6 vs. 5.0 mg/l, P < 0.05). In 44% of them, a second iron measure also indicated iron deficiency (MCV, ferritin, or transferrin saturation per NHANES cutoffs or RDW > 14% per Centers for Disease Control cutoff [26]). However, there was no relationship to ferritin at any concentration.
We also considered a possible role for inflammation/infection. Biochemical evidence of an inflammatory response was present in only 18 infants (8 with AGP > 130 mg/l, 8 with CRP > 3 mg/l, and 2 with both parameters altered). These values constituted 7.0 and 7.2% of the available AGP and CRP specimens, respectively. Infants with elevated AGP or CRP values or both did not have higher FEP or ZPP/H values than the rest of the sample, and those with high FEP values did not have higher AGP or CRP. However, infants with evidence of inflammation showed lower transferrin saturation (24.4% vs. 17.7%) and higher ferritin concentrations (52.4 μg/l vs. 34.7 μg/l) (P values < 0.01).
DISCUSSION
In this sample of 9-month-old African-American infants in inner-city Detroit, we expected iron deficiency to be uncommon, since virtually all infants received iron-fortified formula. The proportion with Hb concentrations < 110 g/l was about 25%, like that reported in other impoverished African-American populations [11,45,46]. In keeping with the use of iron-fortified formula, the proportion meeting NHANES III criteria for iron deficiency (5.3%) was lower than the national average for older infants and toddlers (9%) [6]. However, the proportion meeting criteria for iron deficiency was considerably higher using NHANES II criteria—14.4%, indicating that inclusion of MCV as a criterion measure, rather than ferritin as in NHANES III, substantially altered the estimate of iron deficiency. Thus, estimates of the prevalence of iron deficiency varied substantially, depending on the approach used.
An elevated erythrocyte protoporphyrin concentration is considered a good indicator of iron deficiency [47–50], as it can reflect the functionally significant condition of inadequate iron for hemoglobin synthesis. In fact, several investigators conclude that hemoglobin is no longer the preferred way to screen for iron deficiency in US infants [51–53]. In the current study, average FEP (and ZPP/H) values were unexpectedly high. The overall mean FEP of 86.6 μg/dl red blood cells (75 μmol/mole heme) was substantially higher than that of African-American 12- to 23-month-olds in NHANES III (61 μg/dl red blood cells), US national averages for 1- to 2-year-olds in NHANES II and III (63–69 μg/dl red blood cells) [6,25], and average ZPP/H values in 9-month-old infants (47–56 μmol/mol heme) in more recent studies [29,54]. Laboratory error is unlikely to account for the differences. FEP determinations were performed by ARUP Laboratories, a national reference laboratory at the University of Utah that maintains rigorous standards and is utilized by over half the university teaching hospitals and children’s hospitals in the US. High ZPP/H values were also observed as a hematofluorometer became available to the project. Thus, two different laboratories, utilizing different equipment and different techniques, obtained elevated values. We found no evidence that inflammation accounted for the high values. A newborn screening program has not identified higher than usual prevalence of hemoglobinopathies in this population. That iron deficiency contributes to the high FEP and ZPP/H concentrations is supported by the modest to substantial correlations between FEP and ZPP/H with other measures of iron status and the fact that almost 50% of infants with an elevated FEP had another iron measure in the abnormal range. Nonetheless, this interpretation cannot be proved with the available data, and our observation of high erythrocyte protoporphyrin concentrations in these young inner-city African-American infants warrants further investigation.
The study’s comprehensive panel of iron status indicators included a relatively new measure—total body iron, which depends on both ferritin and TfR. The estimated prevalence of iron deficiency using body iron (4.1%) was quite similar to that in the ferritin model (NHANES III). The body iron calculation has been reported in young children in only one previous study (in Bolivia) [32]. In that analysis, body iron < 0 mg/kg was associated with some hematologic changes indicating inadequate delivery of iron to bone marrow. We found no relationship between body iron < 0 mg//kg and indicators of inadequate delivery. However, our results cannot be directly compared with the Bolivia study, because the above analysis was not reported separately for infants < 1 year of age. Iron fortification/supplementation was not routine in the Bolivia study, whereas it was close to universal in the Detroit sample. In our sample, body iron was so highly correlated with ferritin (whether or not log transformed) that it added little or no information about iron status. Thus, despite the promise of this new index, its usefulness in young infants is unclear.
Regulation of iron absorption and storage is not fully mature in young infants [55–57], making it difficult to interpret measures connected to iron storage, such as ferritin and body iron. The phlebotomy studies in adults that established the progression from iron sufficiency to iron deficiency [58,59] and were used to calculate body iron [31] may not apply to young infants. In phlebotomized adults, for instance, FEP does not become elevated until iron stores are depleted [19]. Yet in the present study, most infants with elevated FEP had normal ferritin values, and there was no level of ferritin at which FEP was consistently high. If the high FEP values reflect inadequate iron for normal erythropoiesis, as other findings in the study indicate, this would imply that the progression of changes in iron status measures is different in young infants. Other research suggests this is the case. For instance, Lind et al. concluded that iron regulation is dynamic in infancy, with dietary iron channeled to red cell production in the 1st year of life and not to storage until the 2nd year [57]. Thus, it seems imperative to confirm which iron status indicators show functional limitations of available iron in young infants and be cautious about applying approaches based on phlebotomized adults.
Turning to other results, we found no differences between male and female infants on any individual iron measure or the proportion meeting criterion for iron deficiency with or without anemia. These results are in contrast to the gender differences observed in some other studies [60–62]. Although the explanation for the differing findings is not readily apparent, iron supplementation may play an important role. In a recent analysis of a large Chilean sample [63], we found that male infants were not at increased risk for iron deficiency under conditions of iron supplementation. Taken together with results in the Detroit sample, where infants were also on iron-fortified formula, the findings indicate that gender-specific standards for iron measures in infancy should not be adopted without further research among infants of different ethnic origin and in different circumstances regarding iron supplementation.
Limitations
The data were collected in the course of identifying infants for a study of brain and behavior in early iron deficiency. Thus, there was no mechanism for monitoring iron therapy or hematologic response to iron or both in the clinic population in general. Dietary information was not collected prospectively or in detail. Our results may underestimate the prevalence of iron deficiency among inner-city African-American infants and toddlers. At 9 months, study infants were still consuming iron-fortified formula and were just entering the age period at highest risk for iron deficiency. It seems reasonable to expect lower iron stores and more iron-deficient erythropoiesis as infants switch from iron-fortified formula to unmodified cow milk. Our results may also be conservative because infants with the complete panel of iron status measures seemed to have better iron status than infants missing the extra blood work. Despite these limitations, the study provides current data on a comprehensive set of iron status indicators in young inner-city black infants.
In sum, Hb < 110 g/l was observed in about a quarter of this sample of 9-month-old African-American infants in inner-city Detroit. FEP and ZPP/H concentrations were considerably higher than generally observed in US infants and toddlers. The high values did not appear to be due to laboratory error or inflammation. Associations with other iron status measures suggested iron deficiency as a possible cause. However, the true prevalence of iron deficiency with or without anemia could not be established with confidence due to differences in the estimates, depending on the approach and whether or not measures related to iron storage were criterion measures. The regulation of iron storage is not mature in the first year of life, and hence, the utility of serum ferritin and the calculated body iron measure is uncertain. Functional definitions of iron deficiency in young infants are urgently needed but remain elusive.
Acknowledgments
We are grateful for the dedicated efforts of William Neeley, M.D., Medical Director, Detroit Medical Center University Laboratories, the laboratory staff at the Detroit Medical Center and Pennsylvania State University, and the clinic’s skilled phlebotomists (Shirhon Robinson and Stephanie Smith). Offie Soldin, Ph.D., Cancer Genetics and Epidemiology, Georgetown University School of Medicine, generously shared ZPP/H data specifically for 8- to 10-month-old infants. The entire group of investigators participating in the Brain and Behavior in Early Iron Deficiency Program Project (Betsy Lozoff, Principal Investigator) contributed to our thinking about the iron status of the study population. The families’ cooperation is deeply appreciated.
Footnotes
Preliminary results were presented at the Pediatric Academic Society meetings, Seattle, 2003.
Contract grant sponsor: NIH; Contract grant number: P01 HD39386.
References
- 1.Vasquez-Seoane P, Windom R, Pearson HA. Disappearance of iron-deficiency anemia in a high-risk infant population given supplemental iron. New Engl J Med. 1985;313:1239–1240. doi: 10.1056/NEJM198511073131936. [DOI] [PubMed] [Google Scholar]
- 2.Yip R, Binkin NJ, Fleshood L, Trowbridge FL. Declining prevalence of anemia among low-income children in the United States. JAMA. 1987;258:1619–1623. [PubMed] [Google Scholar]
- 3.Yip R, Walsh KM, Goldfarb MG, Binkin NJ. Declining prevalence of anemia in childhood in a middle-class setting: A pediatric success story? Pediatrics. 1987;80:330–334. [PubMed] [Google Scholar]
- 4.Sherry B, Bister D, Yip R. Continuation of decline in prevalence of anemia in low-income children: The Vermont experience. Arch Pediatr Adolesc Med. 1997;151:928–930. doi: 10.1001/archpedi.1997.02170460066011. [DOI] [PubMed] [Google Scholar]
- 5.Dallman PR. Changing characteristics of childhood anemia. J Pediatr. 1989;114:161–164. doi: 10.1016/s0022-3476(89)80625-0. [DOI] [PubMed] [Google Scholar]
- 6.Looker AC, Dallman P, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997;277:973–976. doi: 10.1001/jama.1997.03540360041028. [DOI] [PubMed] [Google Scholar]
- 7.McLoyd V, Lozoff B. Racial and ethnic trends in children’s behavior and development. In: Smelser N, Wilson WJ, Mitchell F, editors. National Research Council. America Becoming: Racial Trends and Their Consequences. Washington, DC: National Academy Press; 2000. pp. 311–350. [Google Scholar]
- 8.Brotanek JM, Halterman J, Auinger P, Flores G, Weitzman M. Iron deficiency, prolonged bottle-feeding, and racial/ethnic disparities in young children. Arch Pediatr Adolesc Med. 2005;159:1038–1042. doi: 10.1001/archpedi.159.11.1038. [DOI] [PubMed] [Google Scholar]
- 9.Eden AN, Mir MA. Iron deficiency in 1-to-3-year-old children. Arch Pediatr Adolesc Med. 1997;151:986–988. doi: 10.1001/archpedi.1997.02170470020003. [DOI] [PubMed] [Google Scholar]
- 10.Bogen D, Duggan A, Dover G, Wilson M. Screening for iron deficiency anemia by dietary history in a high-risk population. Pediatrics. 2000;105:1254–1259. doi: 10.1542/peds.105.6.1254. [DOI] [PubMed] [Google Scholar]
- 11.Bogen DL, Krause JP, Serwint JR. Outcome of children identified as anemic by routine screening in an inner-city clinic. Arch Pediatr Adolesc Med. 2001;155:366–371. doi: 10.1001/archpedi.155.3.366. [DOI] [PubMed] [Google Scholar]
- 12.Driggers DA, Reeves JD, Lo EYT, Dallman PR. Iron deficiency in one-year-old infants: Comparison of results of a therapeutic trial in infants with anemia or low-normal hemoglobin values. Pediatrics. 1981;98:753–758. doi: 10.1016/s0022-3476(81)80836-0. [DOI] [PubMed] [Google Scholar]
- 13.Perry GS, Byers T, Yip R, Margen S. Iron nutrition does not account for hemoglobin differences between blacks and whites. J Nutr. 1992;122:1417–1424. doi: 10.1093/jn/122.7.1417. [DOI] [PubMed] [Google Scholar]
- 14.Dallman PR, Barr GD, Allen CM, Shinefield HR. Hemoglobin concentration in white, black, and oriental children: Is there a need for separate criteria in screening for anemia? Am J Clin Nutr. 1978;31:377–380. doi: 10.1093/ajcn/31.3.377. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine. Iron deficiency anemia: Recommended guidelines for the prevention, detection, and management among U.S. children and women of childbearing age. National Academy Press; Washington, DC: 1993. [PubMed] [Google Scholar]
- 16.Owen GM, Yanochik-Owen A. Should there be a different definition of anemia in black and white children? Am J Public Health. 1977;67:865–866. doi: 10.2105/ajph.67.9.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dallman PR, Siimes MA, Stekel A. Iron deficiency in infancy and childhood. Am J Clin Nutr. 1980;33:86–118. doi: 10.1093/ajcn/33.1.86. [DOI] [PubMed] [Google Scholar]
- 18.Finch CA. Iron nutrition. Ann N Y Acad Sci. 1977;300:221–227. doi: 10.1111/j.1749-6632.1977.tb19320.x. [DOI] [PubMed] [Google Scholar]
- 19.Cook JD, Finch CA. Assessing iron status of a population. Am J Clin Nutr. 1979;32:2115–2119. doi: 10.1093/ajcn/32.10.2115. [DOI] [PubMed] [Google Scholar]
- 20.Reeves JD, Yip R, Kiley VA, Dallman PR. Iron deficiency in infants: The influence of mild antecedent infection. J Pediatr. 1984;105:874–880. doi: 10.1016/s0022-3476(84)80069-4. [DOI] [PubMed] [Google Scholar]
- 21.Walter T, Olivares M, Pizarro F, Munoz C. Iron, anemia and infection. Nutr Rev. 1997;55:111–124. doi: 10.1111/j.1753-4887.1997.tb06462.x. [DOI] [PubMed] [Google Scholar]
- 22.Graham EA, Felgenhauer J, Detter JC, Labbe RF. Elevated zinc protoporphyrin associated with thalassemia trait and hemoglobin E. J Pediatr. 1996;129:105–110. doi: 10.1016/s0022-3476(96)70196-8. [DOI] [PubMed] [Google Scholar]
- 23.Tillyer ML, Tillyer CR. Use of red cell distribution width and erythrocyte zinc protoporphyrin in differential diagnosis of a and B thalassaemia and iron deficiency. J Clin Pathol. 1994;47:205–208. doi: 10.1136/jcp.47.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jindadamrongwech S, Wisedpanichkij R, Bunyaratvej A, Hathirat P. Red cell parameters in α-thalassemia with and without β-thalassemia trait or hemoglobin E trait. Southeast Asian J Trop Med Public Health. 1997;28:97–99. [PubMed] [Google Scholar]
- 25.Life Sciences Research Office. Assessment of the iron nutrition status of the U.S. population based on data collected in the second national health and nutrition survey, 1976–1980. Federation of American Societies for Experimental Biology; Bethesda: 1984. [Google Scholar]
- 26.Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Morb Mortal Wkly Rep. 1998;47:1–29. [PubMed] [Google Scholar]
- 27.Aggett PJ, Agostini C, Axelsson I, et al. Iron metabolism and needs in early childhood: Do we know enough? A commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2002;34:337–345. doi: 10.1097/00005176-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Zetterström R. Iron deficiency and iron deficiency anaemia during infancy and childhood. Acta Paediatr. 2004;93:436–439. doi: 10.1080/08035250410027535. [DOI] [PubMed] [Google Scholar]
- 29.Domellöf M, Dewey KG, Lönnerdal B, Hernell O. The diagnostic criteria for iron deficiency in infants should be reevaluated. J Nutr. 2002;132:3680–3686. doi: 10.1093/jn/132.12.3680. [DOI] [PubMed] [Google Scholar]
- 30.Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood. 2003;101:3359–3364. doi: 10.1182/blood-2002-10-3071. [DOI] [PubMed] [Google Scholar]
- 31.Skikne BS, Flowers CH, Cook JD. Serum transferrin receptor: A quantitative measure of tissue iron deficiency. Blood. 1990;75:1870–1876. [PubMed] [Google Scholar]
- 32.Cook JD, Boy E, Flowers C, del Carmon Daroca M. The influence of high-altitude living on body iron. Blood. 2005;106:1441–1446. doi: 10.1182/blood-2004-12-4782. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics Committee on Nutrition. Pediatric Nutrition Handbook. Washington, DC: American Academy of Pediatrics; 2004. [Google Scholar]
- 34.Vigushin DM, Pepys MB, Hawkins PN. Metabolic and scinti-graphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest. 1993;91:1351–1357. doi: 10.1172/JCI116336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feelders RA, Vreugdenhil G, Eggermont AM, Kuiper-Kramer PA, Van Eijk HG, Swaak AJ. Regulation of iron metabolism in the acute-phase response: Interferon γ and tumour necrosis factor α induce hypoferraemia, ferritin production and a decrease in circulating transferrin receptors in cancer patients. Eur J Clin Invest. 1998;28:520–527. doi: 10.1046/j.1365-2362.1998.00323.x. [DOI] [PubMed] [Google Scholar]
- 36.Piomelli S, Seaman C, Zullow D, Curran A, Davidow B. Threshold for lead damage to heme synthesis in urban children. Proc Nat Acad Sci. 1982;79:3335–3339. doi: 10.1073/pnas.79.10.3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slavin W. Graphite furnace AAS for biological materials. Sci Total Environ. 1988;71:17–35. [Google Scholar]
- 38.Erhardt JG, Estes JE, Pfeiffer CM, Biesalski HK, Craft NE. Combined measurement of ferritin, soluble transferrin receptor, retinol binding protein, and C-reactive protein by an inexpensive, sensitive, and simple sandwich enzyme-linked immunosorbent assay technique. J Nutr. 2005;134:3127–3132. doi: 10.1093/jn/134.11.3127. [DOI] [PubMed] [Google Scholar]
- 39.National Committee on Clinical Laboratory Standards. Erythrocyte protophyrin testing: Approved guideline. National Committee on Clinical Laboratory Standards; Villanova, PA: 1996. [Google Scholar]
- 40.Centers for Disease Control and National Center for Health Statistics. NHANES Data. Centers for Disease Control and Prevention, Department of Health and Human Services; Hyattsville, MD: 2003. [Google Scholar]
- 41.Johnson-Spear MA, Yip R. Hemoglobin difference between black and white women with comparable iron status: Justification for race-specific anemia criteria. Am J Clin Nutr. 1994;60:117–121. doi: 10.1093/ajcn/60.1.117. [DOI] [PubMed] [Google Scholar]
- 42.Deinard AS, Schwartz S, Yip R. Developmental changes in serum ferritin and erythrocyte protoporphyrin in normal (nonanemic) children. Am J Clin Nutr. 1983;38:71–75. doi: 10.1093/ajcn/38.1.71. [DOI] [PubMed] [Google Scholar]
- 43.Dallman PR, Siimes MA. Percentile curves for hemoglobin and red cell volume in infancy and childhood. J Pediatr. 1979;94:26–31. doi: 10.1016/s0022-3476(79)80344-3. [DOI] [PubMed] [Google Scholar]
- 44.Saarinen UM, Siimes MA. Developmental changes in red blood cell counts and indices of infants after exclusion of iron deficiency by laboratory criteria and continuous iron supplementation. J Pediatr. 1978;92:412–416. doi: 10.1016/s0022-3476(78)80429-6. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control (Department of Health and Human Services) Pediatric nutrition surveillance. Centers for Disease Control; Atlanta, GA: 1998. [Google Scholar]
- 46.Kahn JL, Binns HJ, Chen T, Tanz RR, Listernick R. Persistence and emergence of anemia in children during participation in the special supplemental nutrition program for women, infants, and children. Arch Pediatr Adolesc Med. 2002;156:1028–1032. doi: 10.1001/archpedi.156.10.1028. [DOI] [PubMed] [Google Scholar]
- 47.Labbe RF, Dewanji A, McLaughlin K. Observations on the zinc protoporphyrin/heme ratio in whole blood. Clin Chem. 1999;45:146–148. [PubMed] [Google Scholar]
- 48.Labbe RF, Dewanji A. Iron assessment tests: Transferrin receptor vis-a-vis zinc protophyrin. Clin Biochem. 2004;37:165–174. doi: 10.1016/j.clinbiochem.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 49.Rettmer RL, Carlson TH, Origenes ML, Jack RM, Labbe RF. Zinc protoporphyrin/heme ratio for diagnosis of preanemic iron deficiency. Pediatrics. 1999;104:e37. doi: 10.1542/peds.104.3.e37. [DOI] [PubMed] [Google Scholar]
- 50.Lott DG, Zimmerman MB, Labbe RF, Kling PJ, Widness JA. Erythrocyte zinc protoporphyrin is elevated with prematurity and fetal hypoxia. Pediatrics. 2005;116:414–432. doi: 10.1542/peds.2004-1601. [DOI] [PubMed] [Google Scholar]
- 51.Mei Z, Parvanta I, Cogswell ME, Gunter EW, Grummer-Strawn M. Erythrocyte protoporphyrin or hemoglobin: Which is a better screening test for iron deficiency in children and women? Am J Clin Nutr. 2003;77:1229–1233. doi: 10.1093/ajcn/77.5.1229. [DOI] [PubMed] [Google Scholar]
- 52.Kazal LA., Jr Prevention of iron deficiency in infants and toddlers. Am Fam Physician. 2002;66:1217–1224. [PubMed] [Google Scholar]
- 53.White KC. Anemia is a poor predictor of iron deficiency among toddlers in the United States: For heme the bell tolls. Pediatrics. 2005;115:315–320. doi: 10.1542/peds.2004-1488. [DOI] [PubMed] [Google Scholar]
- 54.Soldin OP, Miller M, Soldin SJ. Pediatric reference ranges for zinc protoporphyrin. Clin Biochem. 2003;36:21–25. doi: 10.1016/s0009-9120(02)00405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Domellof M, Lönnerdal B, Abrams SA, Hernell O. Iron absorption in breast-fed infants: Effect of age, iron status, iron supplements and complementary foods. Am J Clin Nutr. 2002;76:198–204. doi: 10.1093/ajcn/76.1.198. [DOI] [PubMed] [Google Scholar]
- 56.Leong WI, Bowlus CL, Tallkvist J, Lönnerdal B. Iron supplementation during infancy—Effects on expression of iron transporters, iron absorption, and iron utilization in rat pups. Am J Clin Nutr. 2003;78:1203–1211. doi: 10.1093/ajcn/78.6.1203. [DOI] [PubMed] [Google Scholar]
- 57.Lind T, Hernell O, Lonnerdal B, Stenlund H, Domelloff M, Persson LA. Dietary iron intake is positively associated with hemoglobin concentration during infancy not during the second year of life. J Nutr. 2004;134:1064–1070. doi: 10.1093/jn/134.5.1064. [DOI] [PubMed] [Google Scholar]
- 58.Conrad ME, Crosby WH. The natural history of iron deficiency induced by phlebotomy. Blood. 1962;20:173–185. [PubMed] [Google Scholar]
- 59.Jacob RA, Sandstead HH, Klevay LM, Johnson LK. Utility of serum ferritin as a measure of iron deficiency in normal males undergoing repetitive phlebotomy. Blood. 1980;56:786–791. [PubMed] [Google Scholar]
- 60.Domellöf M, Lönnerdal B, Dewey KG, Cohen RJ, Rivera LL, Hernell O. Sex differences in iron status during infancy. Pediatrics. 2002;110:545–552. doi: 10.1542/peds.110.3.545. [DOI] [PubMed] [Google Scholar]
- 61.Thorsdottir I, Gunnarsson BS, Atladottir H, Michaelsen KF, Palsson G. Iron status at 12 months of age—Effects of body size, growth and diet in a population with high birth weight. Eur J Clin Nutr. 2003;57:505–513. doi: 10.1038/sj.ejcn.1601594. [DOI] [PubMed] [Google Scholar]
- 62.Hay G, Sandstad B, Whitelaw A, Borch-Iohnsen B. Iron status in a group of Norwegian children aged 6–24 months. Acta Paediatr. 2004;93:592–598. [PubMed] [Google Scholar]
- 63.Lozoff B, Kaciroti K, Walter T. Iron deficiency in infancy: applying a physiologic framework for prediction. Amer J Clin Nutr. doi: 10.1093/ajcn/84.6.1412. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]


