Abstract
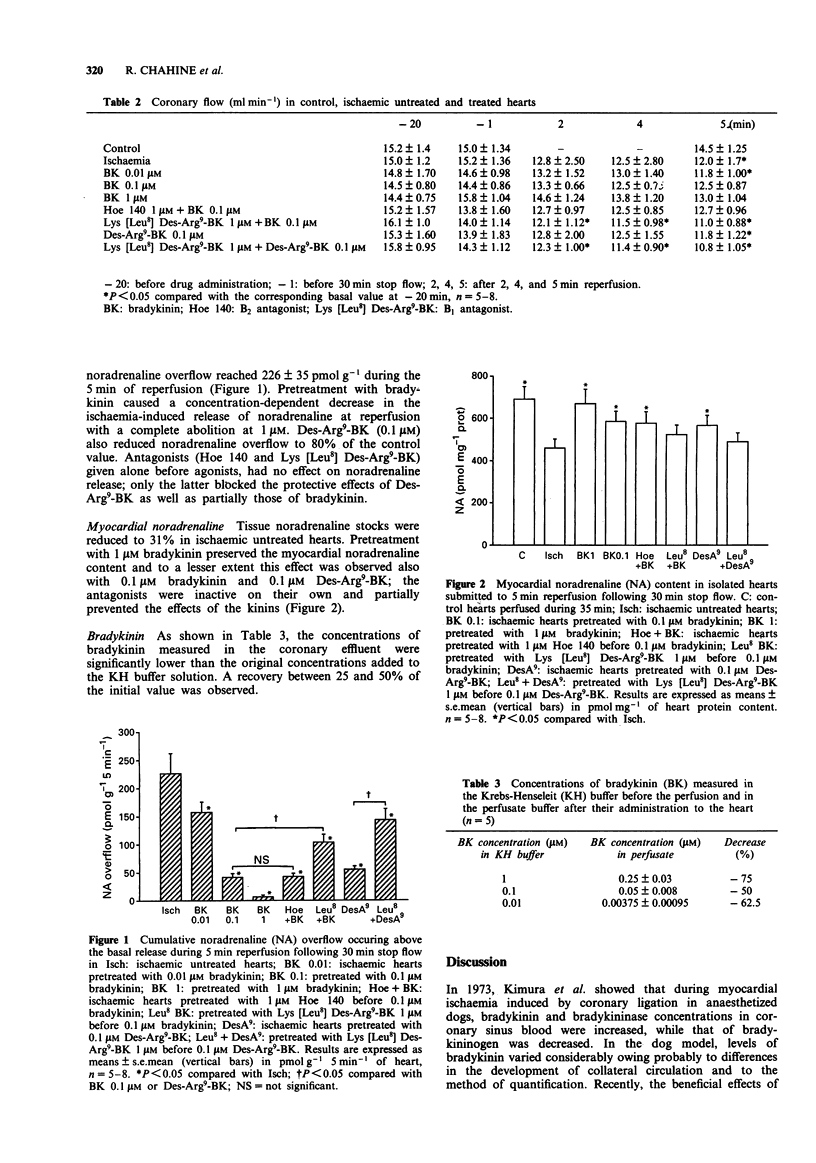
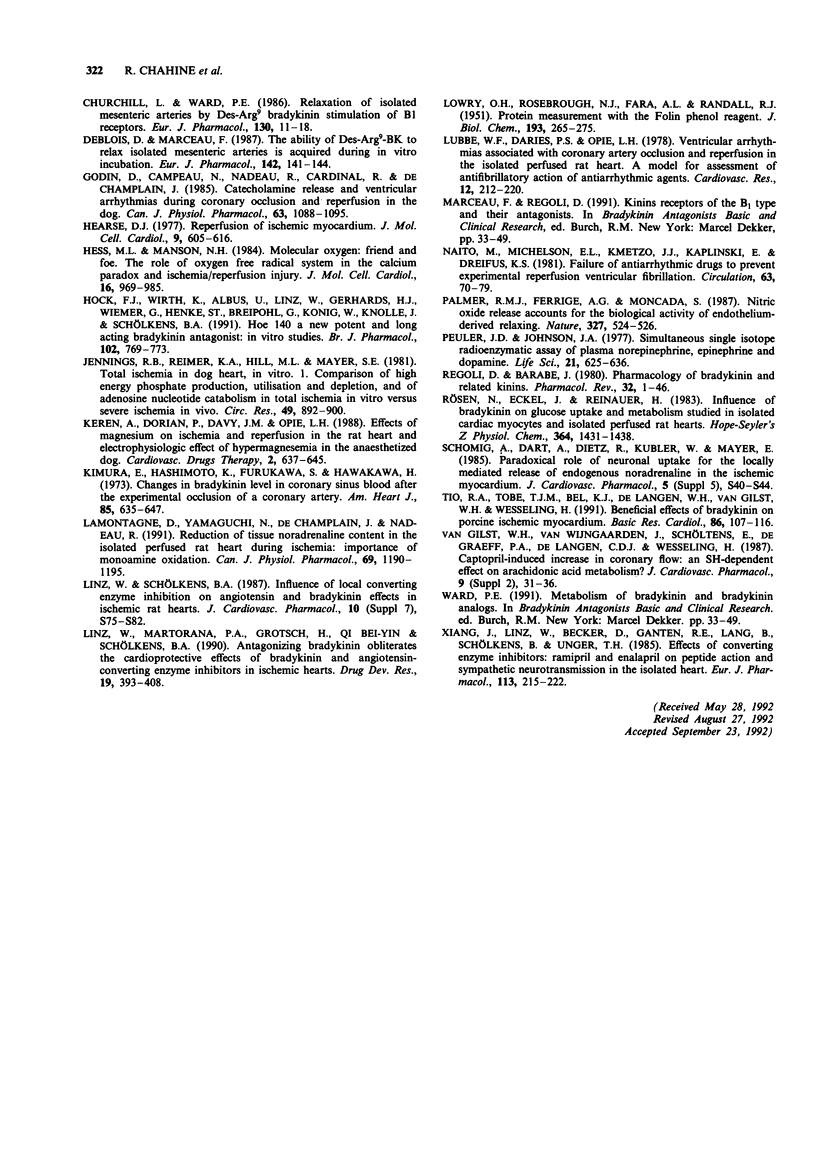
1. We studied the role of bradykinin (BK) and its active metabolite Des-Arg9-BK on noradrenaline release in association with the incidence of ventricular arrhythmias at reperfusion of the ischaemic myocardium. 2. Experiments were performed in Langendorff perfused isolated hearts of rats subjected to 30 min no flow followed by 5 min reperfusion. The electrocardiogram was monitored continuously and noradrenaline was measured in the effluent as well as in the myocardial tissue. 3. In untreated hearts, cumulative noradrenaline overflow following global ischaemia reached 226 +/- 35 pmol g-1 of heart (n = 8, P < 0.05) during the 5 min of reperfusion along with ventricular tachycardia and/or fibrillation. A decrease in myocardial noradrenaline (-31%) was also observed. 4. Bradykinin perfused at concentrations between 0.01 and 1 microM, 10 min before flow was stopped and at reperfusion, inhibited noradrenaline overflow in a concentration-dependent manner. At a concentration of 1 microM, bradykinin completely abolished noradrenaline overflow. For the same concentration of bradykinin, myocardial noradrenaline contents were significantly higher (n = 5-8, P < 0.05). Ventricular fibrillation but not ventricular tachycardia was also prevented. 5. Des-Arg9-BK (0.1 microM) in the same experimental conditions had similar effects. While Hoe 140, a selective antagonist at B2 receptors, did not abolish the effects of bradykinin, Lys [Leu8] Des-Arg9-BK, an antagonist at B1 receptors, abolished the effects of both Des-Arg9-BK and bradykinin. 6. These results suggest that the cardioprotective action of bradykinin in the preparation may be mediated partially by an inhibitory effect on noradrenaline liberation which could be mediated by the activation of B1 receptors.
Full text
PDF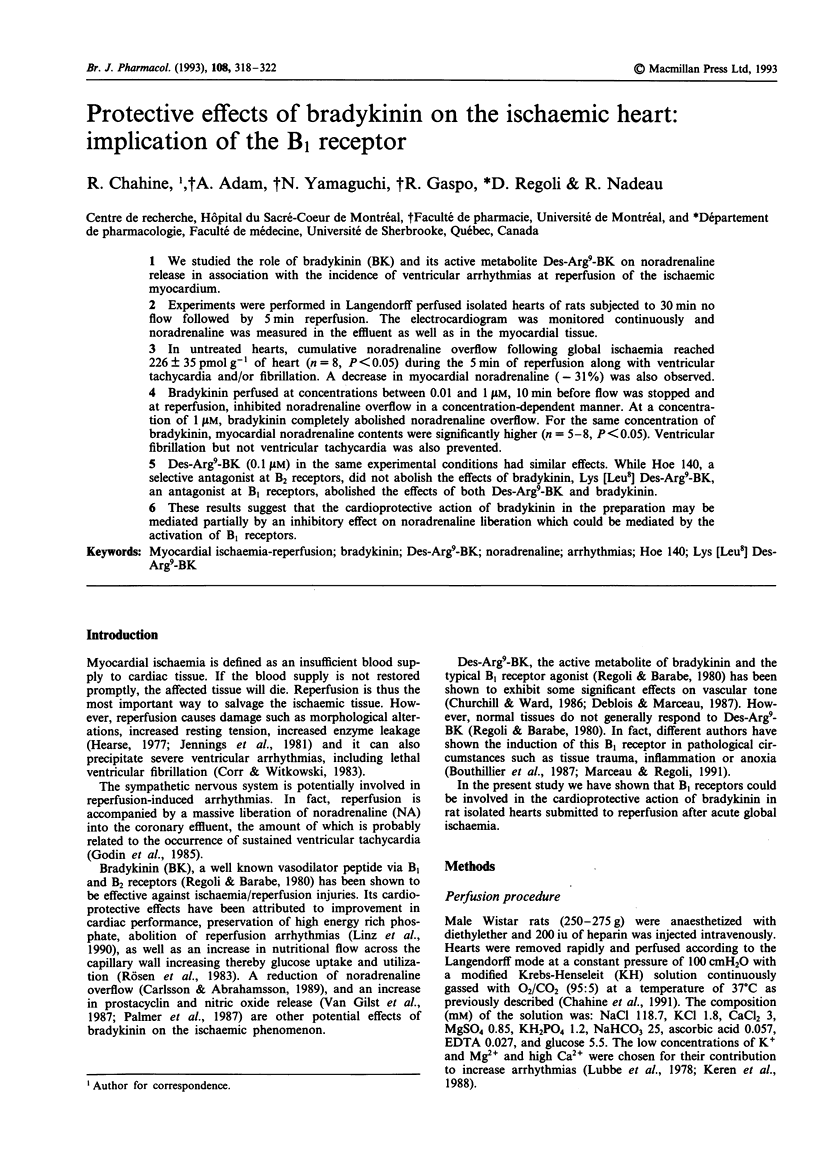


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adam A., Damas J., Calay G., Renard C., Remacle-Volon G., Bourdon V. Quantification of rat T-kininogen using immunological methods. Application to inflammatory processes. Biochem Pharmacol. 1989 May 15;38(10):1569–1575. doi: 10.1016/0006-2952(89)90303-1. [DOI] [PubMed] [Google Scholar]
- Bouthillier J., Deblois D., Marceau F. Studies on the induction of pharmacological responses to des-Arg9-bradykinin in vitro and in vivo. Br J Pharmacol. 1987 Oct;92(2):257–264. doi: 10.1111/j.1476-5381.1987.tb11319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsson L., Abrahamsson T. Ramiprilat attenuates the local release of noradrenaline in the ischemic myocardium. Eur J Pharmacol. 1989 Jul 18;166(2):157–164. doi: 10.1016/0014-2999(89)90055-1. [DOI] [PubMed] [Google Scholar]
- Chahine R., Chen X., Yamaguchi N., de Champlain J., Nadeau R. Myocardial dysfunction and norepinephrine release in the isolated rat heart injured by electrolysis-induced oxygen free radicals. J Mol Cell Cardiol. 1991 Mar;23(3):279–286. doi: 10.1016/0022-2828(91)90064-s. [DOI] [PubMed] [Google Scholar]
- Churchill L., Ward P. E. Relaxation of isolated mesenteric arteries by des-Arg9-bradykinin stimulation of B1 receptors. Eur J Pharmacol. 1986 Oct 14;130(1-2):11–18. doi: 10.1016/0014-2999(86)90178-0. [DOI] [PubMed] [Google Scholar]
- Deblois D., Marceau F. The ability of des-Arg9-bradykinin to relax rabbit isolated mesenteric arteries is acquired during in vitro incubation. Eur J Pharmacol. 1987 Oct 6;142(1):141–144. doi: 10.1016/0014-2999(87)90664-9. [DOI] [PubMed] [Google Scholar]
- Godin D., Campeau N., Nadeau R., Cardinal R., de Champlain J. Catecholamine release and ventricular arrhythmias during coronary occlusion and reperfusion in the dog. Can J Physiol Pharmacol. 1985 Sep;63(9):1088–1095. doi: 10.1139/y85-179. [DOI] [PubMed] [Google Scholar]
- Hearse D. J. Reperfusion of the ischemic myocardium. J Mol Cell Cardiol. 1977 Aug;9(8):605–616. doi: 10.1016/s0022-2828(77)80357-x. [DOI] [PubMed] [Google Scholar]
- Hess M. L., Manson N. H. Molecular oxygen: friend and foe. The role of the oxygen free radical system in the calcium paradox, the oxygen paradox and ischemia/reperfusion injury. J Mol Cell Cardiol. 1984 Nov;16(11):969–985. doi: 10.1016/s0022-2828(84)80011-5. [DOI] [PubMed] [Google Scholar]
- Hock F. J., Wirth K., Albus U., Linz W., Gerhards H. J., Wiemer G., Henke S., Breipohl G., König W., Knolle J. Hoe 140 a new potent and long acting bradykinin-antagonist: in vitro studies. Br J Pharmacol. 1991 Mar;102(3):769–773. doi: 10.1111/j.1476-5381.1991.tb12248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings R. B., Reimer K. A., Hill M. L., Mayer S. E. Total ischemia in dog hearts, in vitro. 1. Comparison of high energy phosphate production, utilization, and depletion, and of adenine nucleotide catabolism in total ischemia in vitro vs. severe ischemia in vivo. Circ Res. 1981 Oct;49(4):892–900. doi: 10.1161/01.res.49.4.892. [DOI] [PubMed] [Google Scholar]
- Keren A., Dorian P., Davy J. M., Opie L. H. Effects of magnesium on ischemic and reperfusion arrhythmias in the rat heart and electrophysiologic effects of hypermagnesemia in the anesthetized dog. Cardiovasc Drugs Ther. 1988 Dec;2(5):637–645. doi: 10.1007/BF00054203. [DOI] [PubMed] [Google Scholar]
- Kimura E., Hashimoto K., Furukawa S., Hayakawa H. Changes in bradykinin level in coronary sinus blood after the experimental occlusion of a coronary artery. Am Heart J. 1973 May;85(5):635–647. doi: 10.1016/0002-8703(73)90169-5. [DOI] [PubMed] [Google Scholar]
- LOWRY O. H., ROSEBROUGH N. J., FARR A. L., RANDALL R. J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951 Nov;193(1):265–275. [PubMed] [Google Scholar]
- Lamontagne D., Yamaguchi N., Ribuot C., de Champlain J., Nadeau R. Reduction of tissue noradrenaline content in the isolated perfused rat heart during ischemia: importance of monoamine oxidation. Can J Physiol Pharmacol. 1991 Aug;69(8):1190–1195. doi: 10.1139/y91-174. [DOI] [PubMed] [Google Scholar]
- Linz W., Schölkens B. A. Influence of local converting enzyme inhibition on angiotensin and bradykinin effects in ischemic rat hearts. J Cardiovasc Pharmacol. 1987;10 (Suppl 7):S75–S82. doi: 10.1097/00005344-198706107-00012. [DOI] [PubMed] [Google Scholar]
- Lubbe W. F., Daries P. S., Opie L. H. Ventricular arrhythmias associated with coronary artery occlusion and reperfusion in the isolated perfused rat heart: a model for assessment of antifibrillatory action of antiarrhythmic agents. Cardiovasc Res. 1978 Apr;12(4):212–220. doi: 10.1093/cvr/12.4.212. [DOI] [PubMed] [Google Scholar]
- Naito M., Michelson E. L., Kmetzo J. J., Kaplinsky E., Dreifus L. S. Failure of antiarrhythmic drugs to prevent experimental reperfusion ventricular fibrillation. Circulation. 1981 Jan;63(1):70–79. doi: 10.1161/01.cir.63.1.70. [DOI] [PubMed] [Google Scholar]
- Palmer R. M., Ferrige A. G., Moncada S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature. 1987 Jun 11;327(6122):524–526. doi: 10.1038/327524a0. [DOI] [PubMed] [Google Scholar]
- Peuler J. D., Johnson G. A. Simultaneous single isotope radioenzymatic assay of plasma norepinephrine, epinephrine and dopamine. Life Sci. 1977 Sep 1;21(5):625–636. doi: 10.1016/0024-3205(77)90070-4. [DOI] [PubMed] [Google Scholar]
- Regoli D., Barabé J. Pharmacology of bradykinin and related kinins. Pharmacol Rev. 1980 Mar;32(1):1–46. [PubMed] [Google Scholar]
- Rösen P., Eckel J., Reinauer H. Influence of bradykinin on glucose uptake and metabolism studied in isolated cardiac myocytes and isolated perfused rat hearts. Hoppe Seylers Z Physiol Chem. 1983 Oct;364(10):1431–1438. doi: 10.1515/bchm2.1983.364.2.1431. [DOI] [PubMed] [Google Scholar]
- Tio R. A., Tobé T. J., Bel K. J., de Langen C. D., van Gilst W. H., Wesseling H. Beneficial effects of bradykinin on porcine ischemic myocardium. Basic Res Cardiol. 1991 Mar-Apr;86(2):107–116. doi: 10.1007/BF02190543. [DOI] [PubMed] [Google Scholar]
- Xiang J. Z., Linz W., Becker H., Ganten D., Lang R. E., Schölkens B., Unger T. Effects of converting enzyme inhibitors: ramipril and enalapril on peptide action and sympathetic neurotransmission in the isolated heart. Eur J Pharmacol. 1985 Jul 17;113(2):215–223. doi: 10.1016/0014-2999(85)90738-1. [DOI] [PubMed] [Google Scholar]


