Abstract
Objective: To examine the course of panic disorder (PD) and panic disorder with agoraphobia (PDA) in 235 primary care patients during a 3-year period.
Method: Patients were recruited from primary care waiting rooms and diagnosed using the Structured Clinical Interview for DSM-IV. They were reassessed at 6 months, 1 year, and annually thereafter for diagnosis, treatment, and other clinical and demographic variables. Recruitment occurred between July 1997 and May 2001.
Results: At intake, 85 patients were diagnosed with PD and 150 were diagnosed with PDA. Patients with PD were significantly more likely to achieve recovery (probability estimate, 0.75) from their disorder than patients with PDA (0.22) at the end of 3-year follow-up (p < .0001). There was no difference in recurrence rates between the 2 disorders. Women were more likely to recover from PD (p = .001). At intake, comorbid generalized anxiety disorder (p = .004), higher Global Assessment of Functioning score (p = .0003), and older age at panic onset (p = .05) were related to recovery from PDA, and comorbid major depressive disorder (p = .05) and psychosocial treatment (p = .002) predicted remaining in an episode of PDA. The relationship between psychosocial treatment and poor recovery must be interpreted with caution and is most likely due to the treatment bias effect.
Conclusion: Primary care patients with PDA have a chronic course of illness, whereas those with PD have a more relapsing course. Given the significant burden of PD and PDA in primary care, attention to factors relevant to the course of these disorders is important for recognition and for continued improvement of treatment interventions in this setting.
Panic disorder (PD) affects 1.5% to 3.7% of the general population and is associated with significant impairment and disability.1–5 Individuals with PD often initially present to the primary care setting due to the physical characteristics of the disorder (e.g., chest pain, dizziness, shortness of breath).6 Prevalence of PD in primary care is much higher than in the general population, with a reported median prevalence of 4% to 6%.3 Despite this high frequency of PD in the primary care setting, the disorder continues to be poorly recognized and often undertreated, which can impact the course of illness.3,7,8
Treatment studies in the psychiatric setting, which use known efficacious pharmacologic and psychological treatments, indicate that a majority of PD patients do not fully recover from PD even when receiving adequate levels of treatment.9 Only 20% to 50% of patients experience initial symptom improvement, and after medication withdrawal there are recurrence rates of 25% to 85%.10–12 Recovery rates are even lower in individuals diagnosed with PD with agoraphobia (PDA), with estimates ranging from 18% to 64%.9 Thus, treatment studies indicate that recovery is difficult to sustain and that long-term follow-up is essential to identifying those who may be at risk for recurrence.
Naturalistic longitudinal studies are able to provide information about the long-term course of illness and variables associated with course. Data from several studies in the psychiatric setting indicate that the clinical course of PD and PDA is chronic and relapsing.13,14 For example, the Harvard/Brown Anxiety Research Project, a naturalistic, longitudinal study of patients recruited from psychiatric settings, reported that the probability of remitting from PD after 1 year was 0.39, and this decreased to 0.17 for PDA.13 In this same study, nearly one third of both PD and PDA patients were likely to experience a recurrence within a year after recovery. Simon et al.15 examined the naturalistic course of recurrence in PD patients and reported that nearly half of those who recovered had a recurrence within a 2-year follow-up period.
Longitudinal studies also can provide information on patient characteristics that are related to course of illness. Identification of patients who are likely to sustain recovery or who are likely to have a recurrence is important to development and implementation of treatment interventions. Identification of factors associated with chronicity is particularly important in the primary care setting, where patients with PD and PDA are high utilizers of the health care system.3,16 Panic disorder patients use medical services at higher rates than nonpsychiatric and other psychiatric patients6 and are overrepresented in specialty clinics.16,17 Thus, an understanding of the course of illness and identification of factors associated with recovery and recurrence in this setting can help improve physician recognition of high-risk patients and lead to the development of targeted interventions that may ultimately decrease the health care burden of PD patients.
In the current study, we examined the 3-year longitudinal course of PD and PDA in a sample of primary care patients. This is the first study, to our knowledge, that has examined the course of these disorders in the primary care setting. Additionally, we examined the clinical and demographic predictors of recovery.
METHOD
Participants
This study was part of the larger Primary Care Anxiety Project (PCAP), a naturalistic, longitudinal study of anxiety disorders in primary care patients. Participants were recruited from 15 internal medicine and family medicine clinics in New England between July 1997 and May 2001. Inclusion criteria for screening eligibility required that participants be English-speaking, at least 18 years of age, and scheduled for a medical appointment on the day of recruitment. Exclusion criteria for screening included current pregnancy or no current address or phone number. A total of 14,320 patients were approached in the waiting rooms, and 4383 (31%) completed an anxiety screening questionnaire that was designed for this study. Of the 4383 patients screened, 2755 (63%) screened positive for anxiety symptoms. Those who screened positive for any anxiety disorder symptoms were asked to participate in the Structured Clinical Interview for DSM-IV (SCID).18 Of those asked to participate in the SCID interview, 456 declined to participate, and 665 repeatedly cancelled or failed to show up for their appointments. The SCID was administered to 1634 individuals, and 539 met criteria to be enrolled in the study. Criteria to be enrolled in PCAP included being diagnosed with at least 1 of the following anxiety disorders, according to the SCID interview: generalized anxiety disorder (GAD), PDA, PD, agoraphobia without a history of PD, posttraumatic stress disorder, social phobia, or mixed anxiety-depressive disorder. Exclusion criteria for participation in PCAP included not having an anxiety disorder diagnosis or endorsing symptoms consistent with a psychotic disorder. A total of 539 patients who completed the SCID were diagnosed with an anxiety disorder and enrolled in the study. This report focuses on the 235 individuals diagnosed at intake with PD (N = 85) or PDA (N = 150). The study was approved by the institutional review boards at each participating site.
Procedure
Research assistants recruited participants from the waiting rooms of the primary care practices. Participants were given a complete description of the study, and informed consent was obtained. Participants completed the screening questionnaire in the waiting room and, if screened positive, were asked to participate in a SCID interview to be conducted during a separate appointment. Once enrolled, participants were evaluated at 6 and 12 months and yearly thereafter. This report will focus on the clinical course of PD and PDA during the first 3 years of PCAP.
Assessment Measures
Screening questionnaire
The screening instrument (available from the authors upon request) was developed specifically for the PCAP study. It is a self-report measure that inquires about the presence of essential features of the DSM-IV anxiety disorders. The instrument differs from existing screening measures (e.g., the Primary Care Evaluation of Mental Disorders [PRIME-MD]) in that it screens for symptoms of all anxiety diagnoses but does not assess all criteria for each disorder. A separate validation study was conducted in 73 patients who completed the screening instrument and the SCID. Forty-five patients screened negative, and none of these was positive for an anxiety disorder according to the SCID interview. Twenty-six participants screened positive, and 8 of these were true positive according to the SCID interview. Eighteen (69%) were false positives. Two patients were excluded during the SCID for psychotic symptoms.
Intake interview
The SCID was used to obtain demographic information and diagnose anxiety disorders and other comorbid diagnoses at intake. Modules assessing anxiety, mood, psychosis, eating disorders, and substance use were utilized for PCAP diagnoses.
Follow-up interview
The Longitudinal Interval Follow-up Evaluation (LIFE)19 is an interviewer-administered instrument used to assess the weekly course of anxiety disorders, psychosocial functioning, and treatment status. Using the LIFE, the interviewer assigned psychiatric status ratings (PSRs) to measure the severity of psychiatric disorders on a weekly basis. At each assessment, the interviewer assessed symptoms from the previous year (or 6 months, depending on time frame) on a weekly basis, using major events (i.e., holidays, season change, birthdays) to guide the interview. All individuals with PD and PDA were coded on each of 4 PD PSR scales. The first PSR scale rates panic attacks from “1 = no symptoms” to “6 = one panic attack or more per day.” In addition to rating panic attacks, 3 other PSR scales, corresponding to DSM-IV PD criteria, were utilized for examining panic course: (1) persistent concern about having additional panic attacks, (2) worry about the implications of panic attacks, and (3) change in behavior related to the attacks. These 3 scales are coded as “1 = absent” or “2 = present” on a 2-point scale. Participants with PDA received an additional weekly score on the 6-point agoraphobia scale ranging from “1 = no symptoms” to “6 = avoidance results in being nearly or completely housebound.”
In this study, course of illness was examined through recovery and recurrence. For PD, recovery was defined as a period of 8 consecutive weeks with panic symptoms at a PSR of 1 or 2 and the absence (i.e., PSR = 1) of persistent concern, worry about implications, and change in behavior. A PD recurrence occurred after a period of recovery and was defined as 1 week of a panic attack PSR of 5 or 6 and at least 4 weeks of persistent concern, worry about the implications, or change in behavior, the first week of which must coincide with the first week of panic attacks. To meet criteria for recovery from PDA, a participant must have met the criteria for PD recovery (given above) and, during the same 8-week period, also have had minimal or no agoraphobia symptoms (PSR of 1 or 2). Recurrence of PDA is the same as that described for PD in addition to 4 or more weeks of a PSR of 4, 5, or 6 for agoraphobia symptoms. For a recurrence of PDA, the persistent concern, worry, or change in behavior and the agoraphobia symptoms were required to occur within the same 4-week period.
Psychosocial functioning and severity of symptoms were assessed using the Global Assessment of Functioning (GAF) score obtained through the LIFE. The GAF was rated on a 0-to-100 scale, with higher scores indicating better functioning.
Previous research has found the LIFE to have adequate reliability and validity for psychiatric diagnoses and psychosocial functioning measures.20
Medical illness questionnaire
Using the medical history form developed for PCAP (available from the authors upon request), participants were asked if they had any of the following illnesses: asthma, cancer, diabetes, epilepsy, stroke, heart problems, or kidney, liver, lung, or thyroid disease. For the purposes of this study, medical illness was coded as a dichotomous yes/no response for the presence of at least 1 self-reported current medical illness.
Treatment questionnaire
Psychiatric and psychosocial treatments were assessed at intake and at each follow-up. Information on psychiatric medications was obtained as part of the LIFE, using the psychotropic/ auxiliary drug treatment schedule (available from the authors upon request), an interviewer-administered form developed for PCAP that assesses psychotropic medications and dosage taken each week since the last interview or currently taking at the time of the initial interview. Psychosocial treatment was assessed using 2 different questionnaires. Participants were asked about the types of mental health treatment received using a form developed specifically for PCAP (available from the authors upon request). The following modalities were assessed: individual therapy, group therapy, family/couple therapy, self-help groups, day treatment, inpatient hospital treatment, residential treatment, or medication management. Additionally, information about specific types of therapeutic techniques was obtained using the Psychosocial Treatments Interview-Revised.21 This is an interviewer-administered questionnaire that was used to specify the type and frequency of a variety of psychotherapy techniques (e.g., cognitive-behavioral therapy, psychodynamic psychotherapy).
Statistical Analyses
Analyses were conducted using SAS statistical software, version 8.2 (SAS Institute, Cary, N.C.). Course data were examined using standard survival analysis techniques. Cox regressions were used to examine individual predictors of course in PD and PDA. Analyses were conducted using PROC FREQ, PROC PHREG, and PROC LIFETEST. A series of individual proportional hazards regression analyses were conducted to examine intake characteristics that may be predictive of recovery from PD and PDA. There were not enough recurrence events to examine predictors of recurrence in this study. Univariate analyses examined the relationship between each predictor and recovery. We examined the following predictors: age, gender, race, education, marital status, full-time employment status, age at PD onset, presence of ongoing medical illness, GAF, psychosocial treatment, psychotropic treatment, and each of the following comorbid diagnoses: social phobia, GAD, posttraumatic stress disorder, and major depressive disorder. Statistical significance was set at p < .05 with no corrections for multiple analyses.
RESULTS
Characteristics of PD and PDA at Intake
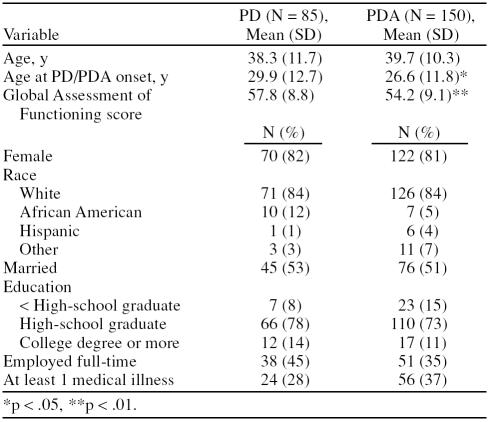
At intake, 85 participants were diagnosed with PD and 150 were diagnosed with PDA. Table 1 presents the demographic characteristics of PD and PDA participants at intake. Overall, patients in both groups were similar, and there were no significant differences between the 2 groups with regard to age, gender, marital status, education, employment status, or presence of medical illness. However, individuals diagnosed with PDA were less likely to be African American (Fisher exact p = .012) and had an earlier age at PD onset (t = −1.98, df = 233, p < .05) and a lower GAF score (t = −2.96, df = 233, p < .01) compared with those individuals diagnosed with PD.
Table 1.
Demographic Characteristics at Intake of Patients With Panic Disorder (PD) or Panic Disorder With Agoraphobia (PDA)
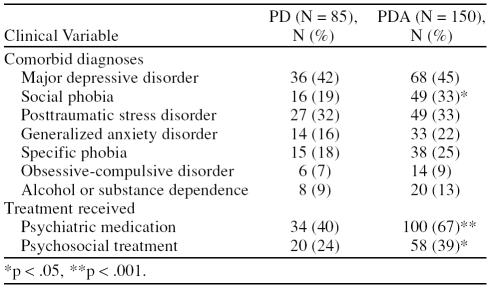
Clinical Features
Table 2 presents the clinical characteristics at intake for the participants with PD and PDA. Major depressive disorder was the most common comorbid diagnosis in both PD (42%) and PDA (45%). Posttraumatic stress disorder was the most frequent comorbid anxiety disorder in both PD (32%) and PDA (33%). The presence of comorbid social phobia was significantly more likely in patients with PDA (33%) than patients with PD (19%) (χ2 = 5.19, df = 1, p < .05).
Table 2.
Clinical Characteristics at Intake of Patients Diagnosed With Panic Disorder (PD) or Panic Disorder With Agoraphobia (PDA)
Treatment Received
At intake, patients with PDA were significantly more likely to be receiving psychiatric medication (67%) than those with PD (40%) (χ2 = 15.74, df = 1, p < .001). Furthermore, those diagnosed with PDA were also more likely to be receiving psychosocial treatment (39%) than those with PD (24%) (χ2 = 5.61, df = 1, p < .05).
Course of PD and PDA
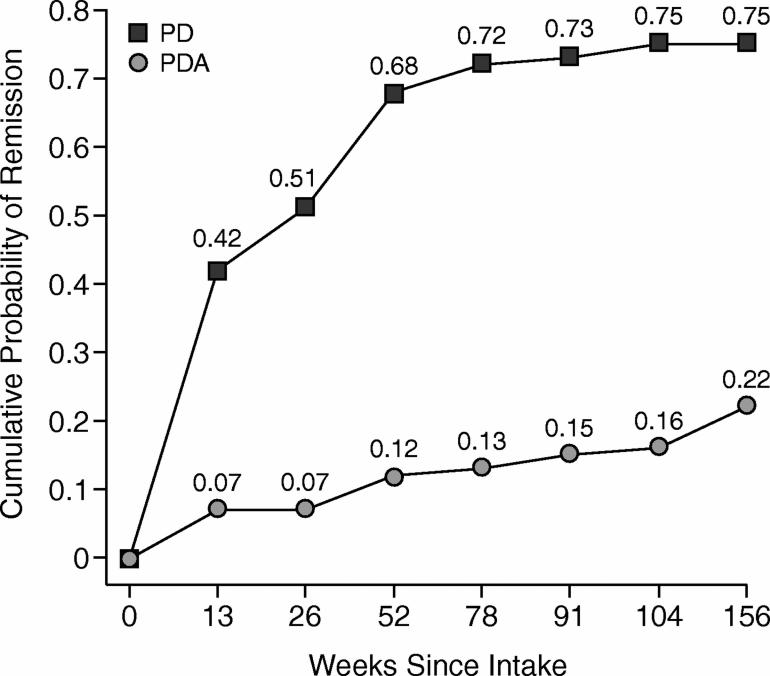
Recovery
Figure 1 presents the Kaplan-Meier survival curve for PD and PDA participants who achieved recovery. At 1 year, the probability of recovery from PD was 0.68, and from PDA, 0.12. By the end of 3 years, the probability of recovery increased to 0.75 for PD and 0.22 for PDA. Panic disorder patients were significantly more likely to achieve recovery at 3 years than patients with PDA (log-rank χ2 = 85.27, df = 1, p < .0001).
Figure 1.
Unadjusted Cumulative Probability of Recovery for Panic Disorder (PD) and Panic Disorder With Agoraphobia (PDA)
Recurrence
Recurrence was examined for those individuals who had experienced a recovery during the 3-year observation. Of the 63 patients with PD who remitted, the probability of recurrence was 0.35. The probability of recurrence for the 30 participants with PDA who remitted during the follow-up period was 0.52. There was no significant difference in recurrence rates between PD and PDA (log-rank χ2 = 2.24, df = 1, NS).
Predictors of PD and PDA Course
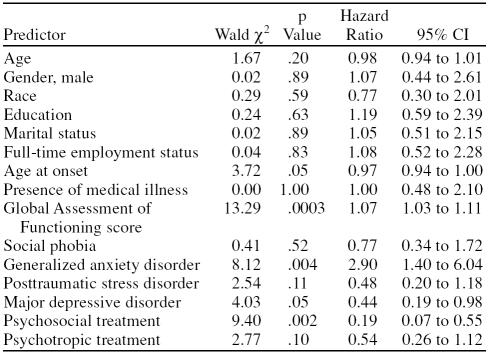
Gender was the only significant predictor of PD course. Women were more likely than men to remit from PD (Wald χ2 = 10.62, hazard ratio [HR] = 5.42, p = .001). Recovery from PDA was associated with several clinical features (Table 3). Patients who recovered from PDA during the 3-year follow-up were more likely to have a higher GAF score (i.e., higher psychosocial functioning and less severe symptoms) at intake (Wald χ2 = 13.29, HR = 1.07, p = .0003), be in an episode of comorbid GAD at intake (Wald χ2 = 8.12, HR = 2.90, p = .004) and have an older age at PDA onset (Wald χ2 = 3.72, HR = 0.97, p = .05). Furthermore, remaining in an episode of PDA (i.e., no recovery) was related to being in an episode of major depressive disorder at intake (Wald χ2 = 4.03, HR = 0.44, p = .05) and to receiving psychosocial therapy at intake (Wald χ2 = 9.40, HR = 0.19, p = .002).
Table 3.
Proportional Hazards Regression Analyses Examining Predictors of Recovery From Panic Disorder With Agoraphobia
Potential differences in treatment rates during the 3 weeks prior to patient recovery were explored to determine if differential treatment may explain the recovery rates. In participants who recovered from PD, 25% (16/63) reported taking a selective serotonin reuptake inhibitor (SSRI) only, 3% (2/63) reported taking a benzodiazepine only, and 3% (2/63) reported taking both a benzodiazepine and an SSRI in the 3 weeks prior to recovery. In participants who remitted from PDA, 23% (7/30) reported taking an SSRI only, 10% (3/30) reported taking a benzodiazepine only, and 23% (7/30) reported taking both a benzodiazepine and an SSRI in the 3 weeks prior to recovery. Fisher exact test revealed that individuals with PDA were more likely to be taking combined medication prior to recovering from an episode of panic (p < .004) than those who were recovering from an episode of PD. There were no significant differences between the groups with regard to taking either SSRIs or benzodiazepines alone.
DISCUSSION
This is the first study to examine the naturalistic clinical course of PD and PDA in the primary care setting. Results indicate that three quarters of patients with PD remitted from their panic symptoms during the 3-year follow-up, as compared with approximately one quarter of patients with PDA. This course pattern indicates that PDA in primary care was characterized by a chronic course of illness with very few episodes of recovery, whereas PD had rather high rates of recovery. The data support the conclusion that agoraphobia is associated with a poorer outcome,13,14,22 even in the primary care setting. Despite the large discrepancy in recovery rates, there was no difference between the disorders in likelihood of experiencing a recurrence. Thus, despite known efficacious treatments for PD and PDA, the chronic and fluctuating course suggests there is continued need for improved treatment intervention in the primary care setting.
Interestingly, there were very few clinical or demographic characteristics predictive of recovery from PD. Gender was the only variable related to recovery from PD in this primary care sample. Specifically, women were 5 times more likely than men to remit from PD. This is not consistent with previous literature, as most naturalistic studies have reported no significant gender differences in recovery rates.23,24 We conducted post hoc analyses to investigate potential differences between men and women in selected demographic and clinical variables at intake and found no significant differences. Interpretation of the gender difference in this study is certainly tempered by the small sample of men (N = 15) who had course data and the fact that only 4 men remitted from PD. Further research is needed to determine if these results are unique to our sample or if there are gender differences in the course of PD for primary care patients.
Recovery from PDA was associated with several clinical features, including having higher levels of psychosocial functioning and the presence of comorbid GAD at intake. In contrast, the presence of comorbid major depressive disorder and receiving psychosocial treatment predicted remaining in an episode of PDA (i.e., not recovering). The psychosocial treatment data must be interpreted with caution, and providers should not interpret these results to mean that psychosocial treatment is harmful. Naturalistic studies, by design, do not control treatment, which can lead to a treatment bias effect. Patients who have more severe symptoms are more likely to seek and receive treatment. In primary care settings, medications are often the first-line treatment, with referrals for psychosocial treatment reserved for refractory cases. Thus, those receiving psychotherapy may be particularly symptomatic and less likely to recover from PDA.
Surprisingly, comorbid GAD at intake predicted recovery from PDA, whereas comorbid major depressive disorder limited recovery. Previous naturalistic and treatment studies have demonstrated that patients with PDA and comorbid major depressive disorder are less likely to recover from PDA as compared to those without major depressive disorder.25–27 However, the relationship between GAD and PDA is intriguing. In naturalistic studies, co-morbidity of other anxiety disorders is typically assessed as the presence or absence of another anxiety disorder or as the number of comorbid disorders present at the time of assessment. However, when examining specific anxiety disorders, rather than any anxiety disorder, there appears to be a differential impact of comorbidity on recovery from PD and PDA.22,28
Treatment of PD or PDA can lead to improvement in secondary anxiety disorders (e.g., GAD) that were not targeted for treatment.28–30 This may be due to possible overlap of symptomatology between PDA and GAD.28 For example, GAD is similar to PDA in that it can be associated with a variety of somatic complaints (e.g., chest pain) and subsequent worry about these symptoms.31,32 In order to test this hypothesis, we conducted a post hoc survival analysis of GAD and PDA course in the 33 PCAP patients diagnosed with both disorders. For this analysis, we used the same PDA definition cited in the Method section of this article and defined GAD recovery, according to previous PCAP publications,33 as minimal or no GAD symptoms (PSR of 1 or 2) for 8 consecutive weeks. Thirty patients with comorbid GAD and PDA had data for the full 3 years, and the data appear to indicate a similar course trajectory for GAD and PDA in these patients. A total of 12 patients (40%) remitted from PDA and 10 patients (33%) remitted from GAD by the end of 3 years. Thus, the data suggest that GAD prediction of PDA recovery in this primary care sample may be a reflection of similar recovery rates in patients with comorbid GAD and PDA. A prospective, controlled study would be needed to adequately evaluate the relationship between fluctuation of symptoms, treatment, and recovery of multiple anxiety disorders. However, it is clear that providers need to be aware of psychiatric comorbidity in primary care patients with PD and PDA, since there may be significant differential impact on the course of illness.
There were several limitations to this study that need to be addressed. This sample was primarily female. Although a preponderance of women is consistent with the 2:1 prevalence rates typically found in anxiety disorders,1,5 the generalizability of the data could be improved with a more balanced gender ratio, particularly given our findings that men were less likely to remit from PD. There were high rates of clinical comorbidity in this sample. This is consistent with what is typically found in community populations, but comorbidity is known to influence the course of illness, both positively and negatively, as our data demonstrate, and this can make interpretation difficult.24,34 We utilized more stringent criteria for PD/PDA recovery and recurrence, making our course data not directly comparable to other studies. To define recovery and recurrence, we examined panic attacks and the individual components of the disorder (e.g., persistent concern, implications, and change in behavior) as enumerated in the DSM-IV. In contrast, other longitudinal studies have not assessed these specific components.14,15 The examination of the individual symptoms of PD ultimately allows for a greater degree of symptom specificity and a more accurate reflection of recovery and recurrence in relation to diagnostic criteria. Finally, we used a broad definition of psychosocial treatment that included any type of psychotherapy reported by the patient, regardless of the known effectiveness. This could potentially wash out the effects of empirically supported treatments, such as cognitive-behavioral therapy, that are likely to positively impact recovery from PD or PDA. Very few patients in this study who received psychosocial treatment endorsed engagement in therapy techniques associated with cognitive-behavioral therapy, suggesting there is continued need for delivery of evidence-based treatments, even in the specialty psychiatric setting.
In summary, this is the first study to examine the course of PD and PDA in primary care patients, and the findings suggest that these 2 disorders have distinct courses of illness and different factors relevant to recovery. In terms of implications for treatment providers, identification of PD and PDA is only the first step in management of these disorders. The apparent chronic and relapsing course indicates that continual attention to patient symptoms is necessary even after resolution of the disorder. Comorbidity clearly impacts the course of PD and PDA, making identification of numerous disorders important, yet taxing on the time of the primary care provider. Effective collaborations with mental health specialists could promote improved treatment for the patient with multiple psychiatric disorders and decrease the burden on the treating physician. Recent evidence demonstrates the efficacy of new treatment paradigms (e.g., integrative treatment approaches)35 targeting multiple psychiatric disorders or adaptation of existing treatment paradigms (e.g., collaborative care models)36 to improve treatment outcomes for anxiety in the primary care setting.
Given the significant burden of PD and PDA in the primary care setting with regard to functional impairment,4 health care utilization,3 and subsequent treatment costs,37,38 factors relevant to the course of these disorders are important and warrant continued research efforts in this treatment setting.
Financial disclosure: Dr. Weisberg has received honoraria from Cephalon and Eli Lilly. Dr. Culpepper is a consultant for AstraZeneca, Eli Lilly, Forest, Pfizer, and Wyeth and is a member of the speakers/ advisory boards for AstraZeneca, Forest, Pfizer, and Wyeth. Dr. Keller is a consultant for or has received honoraria from Collegium, Cypress, Cyberonics, Eli Lilly, Forest, Janssen, Organon, Otsuka, Pfizer, Pharmastar, Sepracor, Vela, and Wyeth; has received grant/research support from Eli Lilly, Pfizer, and Wyeth; and is a member of the advisory boards for Abbott, Bristol-Myers Squibb, Cyberonics, Cypress, Eli Lilly, Forest, GlaxoSmithKline, Janssen, Novartis, Organon, Pfizer, Sepracor, and Wyeth. Drs. Francis, Smith, and Edelen and Ms. Dyck report no additional financial or other relationships relevant to the subject of this article.
Footnotes
The Primary Care Anxiety Project is supported by an unrestricted grant from Pfizer Inc. Dr. Weisberg's time and effort are supported by a Career Development Award from the National Institute of Mental Health (K23 MH069595).
Presented in part at the 17th World Conference of Family Doctors (WONCA), October 13–17, 2004, Orlando, Fla., and at the 25th annual conference of the Anxiety Disorders Association of America, March 17–20, 2005, Seattle, Wash.
The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the Uniformed Services University of the Health Sciences or the U.S. Department of Defense.
Financial disclosure is listed at the end of this article.
REFERENCES
- Kessler RC, McGonagle KA, and Zhao S. et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994 51:8–19. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Wells KB, Judd LL.. Functioning and well-being of patients with panic disorder. Am J Psychiatry. 1996;153:213–218. doi: 10.1176/ajp.153.2.213. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Stein MB, and Russo J. et al. Panic disorder in the primary care setting: comorbidity, disability, service utilization, and treatment. J Clin Psychiatry. 1999 60:492–499. [DOI] [PubMed] [Google Scholar]
- Stein MB, Roy-Byrne PP, and Craske MG. et al. Functional impact and health utility of anxiety disorders in primary care outpatients. Med Care. 2005 43:1164–1170. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, and Jin R. et al. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006 63:415–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaubler TS, Katon W.. Panic disorder in the general medical setting. J Psychosom Res. 1998;44:25–42. doi: 10.1016/s0022-3999(97)00134-7. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Russo J, and Dugdale DC. et al. Undertreatment of panic disorder in primary care: role of patient and physician characteristics. J Am Board Fam Pract. 2002 15:443–450. [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, and Kroenke K. et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA. 1994 272:1749–1756. [PubMed] [Google Scholar]
- Roy-Byrne PP, Cowley DS.. Course and outcome in panic disorder: a review of recent follow-up studies. Anxiety. 1994;1:151–160. doi: 10.1002/anxi.3070010402. [DOI] [PubMed] [Google Scholar]
- Pollack MH. The pharmacotherapy of panic disorder. J Clin Psychiatry. 2005 66suppl 4. 23–27. [PubMed] [Google Scholar]
- Mavissakalian M, Perel JM.. Clinical experiments in maintenance and discontinuation of imipramine therapy in panic disorder with agoraphobia. Arch Gen Psychiatry. 1992;49:318–323. doi: 10.1001/archpsyc.49.4.318. [DOI] [PubMed] [Google Scholar]
- Rickels K, Schweizer E.. Panic disorder: long-term pharmacotherapy and discontinuation. J Clin Psychopharmacol. 1998;18:12S–18S. doi: 10.1097/00004714-199812001-00004. [DOI] [PubMed] [Google Scholar]
- Keller MB, Yonkers KA, and Warshaw MG. et al. Remission and relapse in subjects with panic disorder and panic with agoraphobia: a prospective short-interval naturalistic follow-up. J Nerv Ment Dis. 1994 182:290–296. [DOI] [PubMed] [Google Scholar]
- Pollack MH, Otto MW, and Rosenbaum JF. et al. Longitudinal course of panic disorder: findings from the Massachusetts General Hospital Naturalistic Study. J Clin Psychiatry. 1990 51suppl A. 12–16. [PubMed] [Google Scholar]
- Simon NM, Safren SA, and Otto MW. et al. Longitudinal outcome with pharmacotherapy in a naturalistic study of panic disorder. J Affect Disord. 2002 69:201–208. [DOI] [PubMed] [Google Scholar]
- Katon W. Panic disorder: relationship to high medical utilization, unexplained physical symptoms, and medical costs. J Clin Psychiatry. 1996 57suppl 10. 11–18.discussion 19–22. [PubMed] [Google Scholar]
- Leon AC, Olfson M, Portera L.. Service utilization and expenditures for the treatment of panic disorder. Gen Hosp Psychiatry. 1997;19:82–88. doi: 10.1016/s0163-8343(96)00154-5. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, and Gibbon M. et al. Structured Clinical Interview for DSM-IV Axis I Disorders. New York, NY: Biometrics Research, New York State Psychiatric Institute; 1996 [DOI] [PubMed] [Google Scholar]
- Keller MB, Warshaw MG, and Dyck I. et al. LIFE-IV: The Longitudinal Interval Follow-up Evaluation for DSM-IV. Providence, RI: Department of Psychiatry and Human Behavior, Brown University; 1997 [Google Scholar]
- Warshaw MG, Keller MB, Stout RL.. Reliability and validity of the Longitudinal Interval Follow-up Evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Steketee G, Perry JC, and Goisman RM. et al. The Psychosocial Treatments Interview for anxiety disorders: a method for assessing psychotherapeutic procedures in anxiety disorders. J Psychother Pract Res. 1997 6:194–210. [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Massion AO, and Shea MT. et al. Predictors of remission in patients with panic with and without agoraphobia: prospective 5-year follow-up data. J Nerv Ment Dis. 1997 185:517–519. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Zlotnick C, and Allsworth J. et al. Is the course of panic disorder the same in women and men? Am J Psychiatry. 1998 155:596–602. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Dyck IR, and Warshaw M. et al. Factors predicting the clinical course of generalised anxiety disorder. Br J Psychiatry. 2000 176:544–549. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, and Otto MW. et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005 162:1179–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley DS, Flick SN, Roy-Byrne PP.. Long-term course and outcome in panic disorder: a naturalistic follow-up study. Anxiety. 1996;2:13–21. doi: 10.1002/(SICI)1522-7154(1996)2:1<13::AID-ANXI2>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Martinsen EW, Olsen T, and Tonset E. et al. Cognitive-behavioral group therapy for panic disorder in the general clinical setting: a naturalistic study with 1-year follow-up. J Clin Psychiatry. 1998 59:437–442. [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH.. Diagnostic comorbidity in panic disorder: effect on treatment outcome and course of comorbid diagnoses following treatment. J Consult Clin Psychol. 1995;63:408–418. doi: 10.1037//0022-006x.63.3.408. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Abel JL, Newman H.. Effects of psychotherapy on comorbid conditions in generalized anxiety disorder. J Consult Clin Psychol. 1995;63:479–483. doi: 10.1037//0022-006x.63.3.479. [DOI] [PubMed] [Google Scholar]
- Tsao JC, Lewin MR, Craske MG.. The effects of cognitive-behavior therapy for panic disorder on comorbid conditions. J Anxiety Disord. 1998;12:357–371. doi: 10.1016/s0887-6185(98)00020-6. [DOI] [PubMed] [Google Scholar]
- Carter CS, Maddock RJ.. Chest pain in generalized anxiety disorder. Int J Psychiatry Med. 1992;22:291–298. doi: 10.2190/RGC5-PJK2-7TG5-KL1B. [DOI] [PubMed] [Google Scholar]
- Logue MB, Thomas AM, and Barbee JG. et al. Generalized anxiety disorder patients seek evaluation for cardiological symptoms at the same frequency as patients with panic disorder. J Psychiatr Res. 1993 27:55–59. [DOI] [PubMed] [Google Scholar]
- Rodriguez BF, Weisberg RB, and Pagano ME. et al. Characteristics and predictors of full and partial recovery from generalized anxiety disorder in primary care patients. J Nerv Ment Dis. 2006 194:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce SE, Machan JT, and Dyck I. et al. Infrequency of “pure” GAD: impact of psychiatric comorbidity on clinical course. Depress Anxiety. 2001 14:219–225. [DOI] [PubMed] [Google Scholar]
- Norton PJ, Hope DA.. Preliminary evaluation of a broad-spectrum cognitive-behavioral group therapy for anxiety. J Behav Ther Exp Psychiatry. 2005;36:79–97. doi: 10.1016/j.jbtep.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Craske MG, and Stein MB. et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry. 2005 62:290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, and Kessler RC. et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999 60:427–435. [DOI] [PubMed] [Google Scholar]
- Marciniak MD, Lage MJ, and Dunayevich E. et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety. 2005 21:178–184. [DOI] [PubMed] [Google Scholar]