Abstract
Objectives. We assessed whether there were associations between maternal mental health and individual and co-occurring parenting stressors related to social and financial factors and child health care access.
Methods. We used cross-sectional data from the 2000 National Survey of Early Childhood Health. The 5-item Mental Health Inventory was used to measure self-reported mental health.
Results. After we controlled for demographic covariates, we found that the following stressors increased the risk of poor maternal mental health: lack of emotional (odds ratio [OR] = 3.4; 95% confidence interval [CI] = 2.0, 5.9) or functional (OR=2.2; 95% CI=1.3, 3.7) social support for parenting, too much time spent with child (OR=3.5; 95% CI=2.0, 6.1), and difficulty paying for child care (OR=2.3; 95% CI=1.4, 3.9). In comparison with mothers without any parenting stressors, mothers reporting 1 stressor had 3 times the odds of poor mental health (OR = 3.1; 95% CI = 2.1, 4.8), and mothers reporting 2 or more stressors had nearly 12 times the odds (OR = 11.7; 95% CI = 7.1, 19.3).
Conclusions. If parenting stressors such as those examined here are to be addressed, changes may be required in community support systems, and improvements in relevant social policies may be needed.
Mothers of young children are at considerable risk for mental health problems such as depression and depressive symptoms, with an estimated national prevalence of these mothers reporting 2 or more depressive symptoms at 19%.1 Depression contributes considerably to the burden of disease and is a chronic disease risk factor.2 Moreover, a large body of literature suggests that maternal mental health has a strong influence on child health and development.1,3–10 Population-level data identifying risks for poor maternal mental health could be useful in efforts to address such problems and their consequences.
Rearing young children requires considerable social, financial, and health care resources.11,12 Psychological stress is likely to result if such resources are scarce; for example, evidence shows that low socioeconomic status1,13–16 and the absence of social support17,18 are associated with maternal mental health problems such as depression and anxiety. However, although many parents of young children have difficulty paying for basic child-rearing needs, feel they do not spend sufficient time with their children, and have difficulty obtaining adequate access to health care for their children,19,20 information is lacking on whether such stressors are independently associated with poor maternal mental health.
We examined individual and co-occurring parenting-related stressors (hereafter “parenting stressors”) from the social (i.e., lack of social support, time spent with children), financial (i.e., difficulty paying for child-rearing needs), and child health care (i.e., lack of health insurance coverage, missed or delayed needed care) domains. We view these stressors as intermediaries between socioeconomic status and parent mental health; that is, low socioeconomic status increases the likelihood of these stressors, which influences parent mental health. We hypothesized that the presence of individual social, financial, and health care parenting stressors would increase the risk of poor maternal mental health and that increasing numbers of stressors would result in increased levels of risk.
METHODS
Study Design and Sample
We used data from the 2000 National Survey of Early Childhood Health (NSECH), a nationally representative, cross-sectional telephone survey of the parents of 2068 children aged 4 to 35 months conducted by the National Center for Health Statistics. Interviews were conducted in English or Spanish. The response rate for the survey was 65.6%. We used sampling weights to adjust for households with multiple telephones, households that did not respond, households without telephones, and oversampling of minority children. A detailed description of the NSECH is available elsewhere.20,21
Respondents, mostly mothers (87%; n = 1793), were the adults primarily responsible for their children’s health care. In some cases, respondents were fathers (11%), grandparents (2%), or other guardians (less than 1%). The study sample was made up of mothers who provided information on all study variables (n = 1747).
Measures
Maternal mental health.
Maternal mental health, the dependent variable, was assessed with the 5-item Mental Health Inventory, a validated and reliable self-reported measure of depressive and anxiety symptoms, behavioral–emotional control, and positive affect.22,23 Respondents were asked how often during the past month they had been (1) very nervous, (2) calm and peaceful, (3) down-hearted and blue, (4) so down in the dumps that nothing could cheer them up, and (5) happy. Responses were rated on a 6-point Likert-type scale ranging from “all of the time” to “none of the time.” An average score (range: 0–100) was calculated, with questions 2 and 5 reverse scored. Respondents with scores below 65 (the value closest to the 20th percentile) were defined as being in “poor mental health.”22
Parenting stressors.
Parenting stressors related to social and financial factors were examined. As a means of measuring emotional and functional support for parenting, parents were asked whether there was someone they could (1) “turn to for day-to-day emotional help with parenting” (emotional support) and (2) “count on to watch your child if you need a break” (functional support). Parents responded yes or no to each item.
To assess amount of time spent with the child, parents were asked “Would you say that you spend the right amount of time with your child, or would you like to spend a lot more, a little more, a little less, or a lot less time?” The “a lot more time” and “a little more time” responses were combined, as were the “a little less time” and “a lot less time” responses. Respondents in the resulting 2 categories were compared with respondents who reported that they spent the right amount of time with their child.
As a measure of financial parenting stressors, respondents were asked whether they had “a lot of trouble, some trouble, or no trouble at all paying for” (1) prenatal care during pregnancy; (2) medical expenses for their child’s birth; (3) their child’s health and medical expenses; (4) supplies such as formula, food, diapers, clothes, and shoes; and (5) child care. Financial difficulty was defined dichotomously as “a lot of trouble” or “some trouble” versus “no trouble at all.”
Absence of child health insurance during the 12 months before the interview was used as a measure of potential health care access (i.e., characteristics of the health care delivery system or the population at risk that influence potential care seekers’ use of health services24). Realized access was defined as actual use of health care services.24 Mothers were asked whether, in the 12 months prior to the interview, the child needed medical care but (1) received it later than they would have liked or (2) did not receive it. Mothers who answered yes to either question were defined as having a child with missed or delayed health care.
Study Covariates
Guided by the framework of Gershoff et al.25 regarding child development and the role of socioeconomic factors, marital status, race/ethnicity, and other factors in parenting stress, as well as by the existing literature on parenting and mental health,1,12–15,26,27 we examined several child, maternal, and family demographic variables available in the NSECH data as study covariates: child age, maternal age, maternal race/ethnicity (Hispanics were divided into 2 groups according to whether they were interviewed in English or Spanish), maternal education, maternal marital and employment status, annual household income, and number of children younger than 18 years living in the household. When possible, we dichotomized covariates to reduce degrees of freedom. Sensitivity analyses showed that different covariate categorizations did not lead to changes in the results.
Data Analysis
We used Stata version 8.2 (Stata Corp, College Station, Tex) for the statistical analysis, adjusting variance estimations for the multistage cluster sampling survey design and weighting procedure. We first assessed child, maternal, and household characteristics and the bivariate associations of these characteristics with poor maternal mental health. Second, we determined bivariate associations between each parenting stressor and poor mental health. We used the Pearson χ2 test of independence to assess bivariate associations.
Third, we conducted logistic regression analyses that included each parenting stressor as a predictor (model 1), determining the number of parenting stressors that exhibited independent associations (at the P < .05 level) with poor mental health in model 1. We categorized number of stressors as 0, 1, or 2 or more because of the limited number of mothers reporting 3 or 4 stressors (n = 43). We constructed a regression model that included number of stressors as a predictor (model 2). Both regression models were adjusted for the study covariates. We used the score test for trend of odds (a test used to identify a trend of odds across ordered groups)28 to identify whether there were increasing odds of poor mental health with increasing numbers of parenting stressors. Fourth, we used the Pearson χ2 test of independence to assess bivariate associations between family characteristics and number of parenting stressors.
Finally, we examined specific maternal profiles based on parenting stressors that showed independent associations with poor mental health in model 1. All possible combinations of parenting stressors were examined in terms of their probability of leading to poor maternal mental health. We used logistic regression coefficients adjusted for the study covariates to estimate these probabilities. We conducted this analysis to provide additional details on the probability of poor mental health in the presence of specific co-occurring parenting stressors.
RESULTS
The data in Table 1 ▶ indicates that child age and maternal educational level were not significantly associated with maternal mental health; however, mothers who were younger, employed, or single were more likely to be in poor mental health, as were mothers living in lower income households (P < .05). Also, mothers with 2 children were more likely to be in poor mental health than those with 1 child or with 3 or more children (P < .01).
TABLE 1—
Child, Maternal, and Household Characteristics: 2000 National Survey of Early Childhood Health (n = 1747)
| Characteristic | No. | Overall Sample, % (95% CI) | Respondents With Poor Mental Health,a % (95% CI) |
| Child age, mo | |||
| 4–11 | 485 | 25.0 (22.3, 27.7) | 15.8 (11.8, 20.9) |
| 12–23 | 708 | 38.8 (35.6, 42.0) | 20.4 (16.3, 25.1) |
| 24–35 | 554 | 36.2 (32.9, 39.5) | 23.9 (18.9, 29.8) |
| Maternal age,* y | |||
| <30 | 978 | 53.2 (50.0, 56.6) | 24.0 (20.0, 28.5) |
| ≥ 30 | 769 | 46.7 (43.4, 50.0) | 16.6 (13.3, 20.5) |
| Maternal race/ethnicity | |||
| White | 688 | 63.1 (60.3, 65.9) | 19.5 (15.9, 23.8) |
| Black | 372 | 14.5 (12.6, 16.3) | 24.5 (18.9, 31.2) |
| Hispanic, interviewed in English | 276 | 7.5 (6.3, 8.7) | 23.2 (16.9, 30.9) |
| Hispanic, interviewed in Spanish | 357 | 10.8 (9.3, 12.3) | 19.9 (13.7, 28.0) |
| Other | 54 | 4.1 (2.9, 5.4) | 18.7 (8.5, 36.4) |
| Maternal educational level | |||
| High school or less | 939 | 54.7 (51.5, 58.0) | 23.0 (19.1, 27.4) |
| More than high school | 808 | 45.3 (42.0, 48.6) | 17.6 (14.0, 21.8) |
| Maternal employment status* | |||
| Employed | 963 | 53.5 (50.2, 56.8) | 23.3 (19.4, 27.7) |
| Not employed | 784 | 46.5 (43.2, 49.8) | 17.3 (13.8, 21.6) |
| Household income,*** $ | |||
| ≤ 17 500 | 469 | 23.0 (20.3, 25.6) | 26.5 (20.8, 33.2) |
| 17 501–35 000 | 491 | 27.0 (24.0, 29.9) | 24.9 (19.3, 31.5) |
| 35 001–60 000 | 307 | 19.6 (17.0, 22,2) | 15.3 (10.5, 21.7) |
| > 60 000 | 299 | 20.8 (18.1, 23.6) | 13.2 (9.0, 19.0) |
| Don’t know/refused to answer | 181 | 9.6 (7.7, 11.7) | 20.4 (12.0, 32.6) |
| Maternal marital status*** | |||
| Married | 1093 | 68.3 (65.2, 71.3) | 15.9 (13.1, 19.2) |
| Single | 654 | 31.8 (28.7, 34.8) | 30.5 (25.0, 36.7) |
| No. of children* | |||
| 1 | 544 | 28.3 (25.4, 31.1) | 18.7 (14.3, 24.1) |
| 2 | 608 | 35.7 (32.5, 38.9) | 25.2 (20.1, 31.0) |
| 3 or more | 595 | 36.0 (32.8, 39.3) | 17.3 (13.5, 22.0) |
Note. CI = confidence interval.
aDefined as a respondent with a score below the 20th percentile (i.e., with a score less than 65 out of 100) on the 5-item Mental Health Inventory.
* P < .05; ***P < .001.
Table 2 ▶ shows that nearly 14% of mothers did not have emotional support for parenting and that 12% did not have functional support. These mothers were more likely to be in poor mental health than those who had support (P < .001). Thirty-seven percent of mothers reported spending too little time with their child, and 11% reported spending too much time; in comparison with those who reported spending the right amount of time, both groups (but the latter much more so) were more likely to be in poor mental health (P < .001).
TABLE 2—
Bivariate Associations Between Specific Self-Reported Parenting Stressors and Poor Maternal Mental Health: 2000 National Survey of Early Childhood Health (n = 1747)
| No. | Overall Sample, % (95% CI) | Respondents With Poor Mental Health,a % (95% CI) | |
| Social stressors | |||
| Emotional supportb | |||
| Yes | 1424 | 86.3 (84.2, 88.4) | 16.8 (14.1, 19.9)*** |
| No | 323 | 13.7 (11.6, 15.8) | 44.2 (36.1, 52.6) |
| Functional supportb | |||
| Yes | 1529 | 88.4 (86.3, 90.5) | 17.5 (14.8, 20.6)*** |
| No | 218 | 11.6 (9.5, 13.7) | 43.6 (34.0, 53.6) |
| Time spent with child | |||
| Right amount | 893 | 51.6 (48.3, 54.9) | 14.0 (11.0, 17.6)** |
| Too little | 718 | 37.2 (34.1, 40.3) | 22.7 (18.6, 27.5) |
| Too much | 136 | 11.2 (8.8, 13.7) | 43.5 (32.1, 55.6) |
| Financial stressorsc | |||
| Prenatal care | |||
| Yes | 151 | 7.7 (6.0, 9.3) | 28.4 (19.0, 40.1) |
| No | 1596 | 92.3 (90.7, 94.0) | 19.9 (17.1, 23.0) |
| Birthing expenses | |||
| Yes | 198 | 12.4 (10.0, 14.7) | 24.1 (16.5, 33.7) |
| No | 1549 | 87.6 (85.3, 89.9) | 20.0 (17.2, 23.3) |
| Medical expenses | |||
| Yes | 221 | 13.2 (10.8, 15.5) | 28.1 (20.1, 37.7)* |
| No | 1526 | 86.8 (84.5, 89.2) | 19.4 (16.6, 22.6) |
| Supplies (e.g., food, diapers) for child | |||
| Yes | 379 | 23.0 (20.1, 26.0) | 34.9 (27.9, 42.6)*** |
| No | 1368 | 77.0 (74.0, 79.9) | 16.3 (13.6, 19.3) |
| Child care | |||
| Yes | 231 | 14.0 (11.6, 16.4) | 44.7 (35.4, 54.3)*** |
| No | 1516 | 86.0 (83.6, 88.4) | 16.6 (14.0, 19.6) |
| Child health care stressors | |||
| Lack of health insurance for child in past 12 mo | |||
| Yes | 348 | 16.2 (13.9, 18.6) | 31.4 (24.1, 39.7)*** |
| No | 1399 | 83.8 (81.5, 86.0) | 18.4 (15.6, 21.7) |
| Missed or delayed care for child | |||
| Yes | 228 | 12.5 (10.5, 14.6) | 27.4 (20.4, 35.7)* |
| No | 1519 | 87.5 (85.4, 89.5) | 19.6 (16.6, 22.8) |
Note. CI = confidence interval.
aDefined as a respondent with a score below the 20th percentile (i.e., with a score less than 65 out of 100) on the 5-item Mental Health Inventory.
bTo measure emotional and functional support for parenting, parents were asked whether there was someone they could (1) “turn to for day-to-day emotional help with parenting” (emotional support) and (2) “count on to watch your child if you need a break” (functional support). Parents responded yes or no to each item.
cRespondents were asked whether they had “a lot of trouble, some trouble, or no trouble at all paying for” different needs related to child rearing. Financial difficulty was defined dichotomously as reports of “a lot of trouble” or “some trouble” versus “no trouble at all.”
* P < .05; **P < .01; ***P < .001.
Financial difficulties were common: 23% of mothers reported having trouble paying for food, diapers, clothes, and other supplies for their child; 14%, for child care; 13%, for medical care; 12%, for birthing care; and 8%, for prenatal care. Mothers who reported having trouble paying for supplies or child care were more likely to be in poor mental health than those who did not have such difficulties (P < .001). About 16% of children were uninsured in the 12 months prior to the interview, and nearly 13% missed medical care or had delayed care. Mothers with uninsured children and those with children with missed or delayed care were both significantly more likely to be in poor mental health (P < .05).
Table 3 ▶ shows results from the multivariate logistic regression analysis of poor mental health. Model 1 shows that 3 social stressors—lack of emotional support, lack of functional support, and reports of too much time spent with the child—were independently associated with poor mental health. Having trouble paying for child care was the only financial stressor independently associated with poor mental health. Child health care access was not independently associated with poor mental health. Model 2 shows that there was a trend toward increasing odds of poor mental health with increasing numbers of parenting stressors (P<.001, according to score test for trend of odds). In comparison with mothers who did not report any parenting stressors, those reporting 1 stressor had about 3 times the odds of being in poor mental health, and those reporting 2 or more stressors had about 12 times the odds of being in poor mental health.
TABLE 3—
Results of Multiple Logistic Regression Analysis of Poor Maternal Mental Health According to Self-Reported Parenting Stressors: 2000 National Survey of Early Childhood Health (n = 1747)
| Poor Mental Healtha | ||
| Model 1, Odds Ratio (95% CI) | Model 2, Odds Ratio (95% CI) | |
| Social stressors | ||
| Social support | ||
| No emotional supportb | 3.44 (2.02, 5.86)*** | |
| No functional supportb | 2.17 (1.27, 3.73)** | |
| Time with child | ||
| Right amount (reference) | 1.00 | |
| Too little | 1.23 (0.81, 1.89) | |
| Too much | 3.47 (1.97, 6.11)*** | |
| Financial stressorsc | ||
| Trouble paying for prenatal care | 1.31 (0.69, 2.47) | |
| Trouble paying for birthing care | 0.89 (0.47, 1.69) | |
| Trouble paying for medical care | 0.87 (0.49, 1.55) | |
| Trouble paying for supplies for child | 1.38 (0.90, 2.13) | |
| Trouble paying for child care | 2.34 (1.41, 3.88)*** | |
| Child health care stressors | ||
| Lack of health insurance for child | 1.46 (0.87, 2.44) | |
| Missed or delayed care for child | 0.94 (0.56, 1.57) | |
| No. of parenting stressorsd | ||
| 0 (reference) | 1.00 | |
| 1 | 3.14 (2.06, 4.77)*** | |
| ≥ 2 | 11.70 (7.08, 19.33)*** | |
Note. CI = confidence interval. Values were adjusted for child age, maternal age, maternal race/ethnicity, maternal education, maternal marital and employment status, household income, and number of children in the household.
aDefined as a respondent with a score below the 20th percentile (i.e., with a score less than 65 out of 100) on the 5-item Mental Health Inventory.
b To measure emotional and functional support for parenting, parents were asked whether there was someone they could (1) “turn to for day-to-day emotional help with parenting” (emotional support) and (2) “count on to watch your child if you need a break” (functional support). Parents responded yes or no to each item.
cRespondents were asked whether they had “a lot of trouble, some trouble, or no trouble at all paying for” different needs related to child rearing. Financial difficulty was defined dichotomously as reports of “a lot of trouble” or “some trouble” versus “no trouble at all.”
dDefined as the sum of no emotional support, no functional support, having too much or too little time with child, and trouble paying for child care. Stressors not showing independent associations with poor mental health were not included.
** P < .01; ***P < .001.
There was a trend toward increasing probability of poor mental health as number of parenting stressors increased. Yet, there was great variability in the probability of poor mental health within profiles involving the same number of parenting stressors (Figure 1 ▶). The following stressor profiles were among those with the highest probability of exhibiting an association with poor maternal mental health: reports of trouble paying for child care; reports of both trouble paying for child care and lack of emotional support; reports of both too much time spent with child and lack of functional support; reports of both too much time spent with child and no emotional or functional support; reports of trouble paying for child care, too much time spent with child, and lack of emotional support; and reports of all 4 stressors.
FIGURE 1—
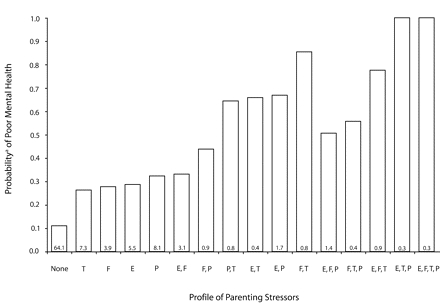
Probability of poor mental health for all possible combinations of parenting stressors: National Survey of Early Childhood Health, 2000.
Note. T = too much time spent with child, F = lack of functional support, E = lack of emotional support, P = had trouble paying for child care. Poor mental health was defined as scores below the 20th percentile on the 5-item Mental Health Inventory. As a means of measuring emotional and functional support for parenting, parents were asked whether there was someone they could “turn to for day-to-day emotional help with parenting” (emotional support) and “count on to watch your child if you need a break” (functional support). Parents responded yes or no to each item. The number at the base of each bar represents the proportion of the total weighted sample in that profile category.
aProbabilities were adjusted for child age, maternal age, maternal race/ethnicity, maternal education, household income, maternal marital status, maternal employment, and number of children in the household.
Table 4 ▶ shows that numbers of parenting stressors (i.e., the stressors associated with poor maternal mental health) were not evenly distributed according to the demographic characteristics of mothers and children. Mothers with children between ages 12 and 35 months tended to report more parenting stressors than mothers with children in other age groups (P < .05). Black mothers and Hispanic mothers who interviewed in Spanish were more likely to report parenting stressors (P < .001), as were mothers of low socioeconomic status (i.e., having less than a high school education or being a member of a low-income family; P < .01) and mothers who were single (P < .01).
TABLE 4—
Child, Maternal, and Household Characteristics, by Number of Parenting Stressors: 2000 National Survey of Early Childhood Health (n = 1747)
| No. of Parenting Stressors,a % (95% CI) | ||||
| No. | 0 | 1 | 2 or more | |
| Child age, mo* | ||||
| 4–11 | 485 | 73.7 (68.0, 78.6) | 18.3 (14.1, 23.4) | 8.1 (5.3, 12.1) |
| 12–23 | 708 | 62.9 (57.8, 67.8) | 25.7 (21.4, 30.4) | 11.4 (8.4, 15.5) |
| 24–35 | 554 | 58.8 (52.8, 64.5) | 11.4 (8.4, 15.5) | 12.6 (9.2, 17.1) |
| Maternal age, y | ||||
| < 30 | 978 | 61.2 (56.6, 65.6) | 26.1 (22.2, 30.4) | 12.7 (9.9, 16.3) |
| ≥ 30 | 769 | 67.4 (62.7, 71.8) | 23.6 (19.7, 27.9) | 9.1 (6.7, 12.2) |
| Maternal race/ethnicity*** | ||||
| White | 688 | 67.7 (63.0, 72.0) | 23.1 (19.3, 27.5) | 9.2 (9.7, 12.6) |
| Black | 372 | 65.1 (58.3, 71.3) | 23.2 (18.1, 29.4) | 11.7 (7.6, 17.5) |
| Hispanic, interviewed in English | 276 | 68.6 (61.1, 75.2) | 24.9 (18.8, 32.0) | 6.6 (3.8, 11.1) |
| Hispanic, interviewed in Spanish | 357 | 35.2 (28.7, 42.4) | 39.3 (32.3, 46.8) | 25.4 (19.9, 31.8) |
| Other | 54 | 73.0 (56.8, 84.7) | 19.8 (9.9, 35.8) | 7.2 (2.3, 20.2) |
| Maternal educational level** | ||||
| High school or less | 939 | 59.3 (54.7, 63.7) | 27.6 (23.5, 32.0) | 13.2 (10.4, 16.6) |
| More than high school | 808 | 69.9 (65.3, 74.1) | 21.7 (18.0, 25.8) | 8.4 (6.0, 11.8) |
| Maternal employment status | ||||
| Employed | 319 | 63.4 (58.9, 67.7) | 27.0 (23.0, 31.4) | 9.6 (7.3, 12.6) |
| Not employed | 784 | 64.9 (60.1, 69.4) | 22.5 (18.9, 26.7) | 12.6 (9.6, 16.5) |
| Household income,** $ | ||||
| ≤ 17 500 | 469 | 54.8 (48.2, 61,2) | 31.3 (25.5, 37.8) | 13.9 (9.8, 19.3) |
| 17 501–35 000 | 491 | 61.6 (55.2, 67.7) | 25.4 (20.2, 31.6) | 13.0 (9.3, 17.8) |
| 35 001–60 000 | 307 | 70.7 (63.1, 77.3) | 20.4 (15.0, 27.0) | 8.9 (4.8, 16.1) |
| > 60 000 | 299 | 74.9 (67.8, 80.8) | 18.1 (13.0, 24.6) | 7.0 (4.1, 11.9) |
| Don’t know/refused to answer | 181 | 56.5 (45.3, 67.1) | 32.0 (22.0, 43.9) | 11.6 (6.6, 19.5) |
| Maternal marital status** | ||||
| Married | 209 | 68.0 (64.1, 71.6) | 23.1 (19.8, 26.7) | 9.0 (6.9, 11.6) |
| Single | 1538 | 55.7 (49.9, 61.4) | 28.8 (23.7, 34.5) | 15.5 (11.5, 20.4) |
| No. of children | ||||
| 1 | 544 | 64.5 (59.8, 69.9) | 24.9 (20.4, 30.0) | 10.6 (7.1, 15.6) |
| 2 | 608 | 60.9 (55.2, 66.3) | 26.9 (22.1, 32.3) | 12.3 (9.0, 16.6) |
| ≥ 3 | 595 | 67.0 (61.3, 72.2) | 23.0 (18.4, 28.3) | 10.1 (7.3, 13.8) |
Note. CI = confidence interval.
aDefined as the sum of no emotional support, no functional support, having too much or too little time with child, and trouble paying for child care. Stressors not showing independent associations with poor mental health were not included.
* P < .05; **P < .01; ***P < .001.
DISCUSSION
We found that parenting stressors related to social and financial factors and child health care were commonly reported. More than one third of the sampled mothers reported 1 or more social or financial parenting stressors associated with poor mental health. The risk of poor mental health was particularly high when social and financial parenting stressors were both present. Those who lacked emotional support and had trouble paying for child care were at heightened risk of poor maternal mental health, as were those who lacked functional support and reported spending too much time with their child. Approximately 36% of mothers experienced at least 1 or more of these parenting stressors, suggesting an important focus for intervention.
Social and financial parenting stressors were disproportionately found among low-income families and families from racial/ethnic minority groups. Given the higher rates of multiple parenting stressors in these groups, one would expect to see concomitantly higher rates of poor maternal mental health. Although our results confirmed findings of higher rates of poor mental health among mothers in low-income families,13,14,17,18,26 we found no significant differences in poor mental health according to race/ethnicity. The reasons why relationships between parenting stressors and maternal mental health may differ in different racial/ethnic groups are unclear, but there may be differences in the expression of mental health symptoms according to cultural background, or perhaps certain minority populations are more resilient in terms of mental health status despite limited social and financial parenting resources.
Because we found a high frequency of parenting stressors and a substantially higher risk of poor maternal mental health in the presence of multiple stressors, we suggest an examination of relevant social policies and community services that can address these stressors (e.g., addressing poor coverage rates and low benefit caps for safety-net programs).29 It is estimated that only about half of eligible families in the United States are enrolled in the Temporary Assistance for Needy Families (TANF) program30 and the Special Supplemental Food Program for Women, Infants, and Children (WIC).31
Changes in coverage policies for welfare recipients under the Personal Responsibility and Work Opportunity Reconciliation Act (Pub L No. 104–193) require further scrutiny. For example, this legislation requires parents, as early as 6 weeks after the birth of their child, to participate in employment, training, or other employment-related activities if they are to continue receiving benefits. This situation, in conjunction with reductions in the availability of child care assistance in many states32 (child care subsidies are projected to fall from 2.4 million in 2003 to 2 million by 2009 if federal funding remains flat33), may have a significant impact on the parenting stressors examined in this study, particularly the stressors shown to be associated with poor maternal mental health.
The balance of time necessary for parenting young children is in jeopardy for many US families with young children, with more than one third of mothers in this study reporting too little time spent with their children and 10% reporting spending too much time. Public- and private-sector family leave policies for parents with young children are more restrictive in the United States than in other top industrialized countries, probably at the detriment of parents’ well-being as well as that of their children. Parents must make significant sacrifices in terms of either the time they have for parenting or the income they need to build a family. Ensuring that adequate paid family leave policies for parents with young children are in place and ensuring that family leave insurance and quality child care are affordable and accessible may help address the parenting stressors examined in this study.
At the community level, the capacity of organizations serving families with young children might be improved to help families meet parenting and psychosocial needs.34 For example, family resource centers can provide a single portal for families to access a network of community support services.35 Other possible strategies include home visiting models in which information about child rearing and development, information on availability of health and social services, and functional social support are provided to underserved families with young children.36 There are many potential community-based approaches to assisting families; however, research is required to assess the impact and cost-effectiveness of such programs.37
Given that parenting stressors increase the risk of symptoms indicating poor mental health, health care providers that serve families with young children can play a role in addressing stressors. The frequent interactions between such health care providers and families represent important opportunities to screen parents,38–40 discuss their mental health needs, and refer them to relevant services in the community.
Family practitioners and pediatricians can discuss parenting stressors as well, especially those that involve a high risk for poor mental health. Should these doctors suspect parents of having mental health problems such as depression, the parents can be screened or given appropriate referrals for mental health services.41 According to the parenting stressor profile in question, the clinician can refer families to community resources. However, if such strategies are to succeed, adequate primary care, mental health care, and community resources must be in place and be well coordinated.
Limitations
Our study had several limitations. First, our use of secondary NSECH data limited the scope of our study as well as our ability to control for potential confounders such as parents’ physical health, children’s developmental transitions, and changes in children’s health status that could have influenced depressive symptoms. Second, the NSECH response rate of 65.6% may have affected the generalizability of our results; however, the survey weights we used in the analyses were designed to adjust for nonresponse. Third, because our data were cross-sectional, they did not allow for demonstrations of causality.
Fourth, although the parenting stressors we assessed were associated with poor maternal mental health, relationships may have been bidirectional. For example, depressed parents may have had greater difficulty obtaining social support, feeling satisfied with the amount of time they spent with their child, and achieving financial stability. Fifth, our measure of maternal mental health was based on self-reported symptoms rather than clinical diagnoses. However, research has shown that depressive symptoms are sensitive predictors of poor child health and development.42 The Mental Health Inventory does not specifically measure depression; rather, it assesses general symptoms of common affective problems that are closely associated with depression.43 Therefore, our data should be viewed with caution until causality is established through prospective studies involving clinical assessments of depressive symptoms and more objective measures of parenting stressors.
Sixth, the findings of this study can be generalized only to mothers of young children, even though the stressors examined here may be equally common among fathers and parents of older children. Finally, because of the small number of fathers who took part in the NSECH, we focused only on mothers. Future research is needed to examine the effects of parenting stressors on paternal mental health.
Conclusions
Our findings showed that parenting stressors related to social and financial factors and child health care are commonly reported by mothers with young children, especially low-income mothers and those who are members of racial/ethnic minority groups. Social and financial parenting stressors increase the risk of poor maternal mental health, and mothers who report multiple stressors are at particularly high risk. Minimizing these types of stressors in families with young children may require shifting societal resources to support programs such as TANF, WIC, and child care support; family leave; and community programs. Further efforts can focus on encouraging primary care providers to identify parenting stressors, screen parents for depression, and help them gain access to available resources in the community.
Peer Reviewed
Contributors R. Mistry originated the main ideas of this study. All of the authors contributed to the conceptualization and refinement of the study. R. Mistry and G. D. Stevens were responsible for the design, analysis, and writing of the article. G. D. Stevens, H. Sareen, R. De Vogli, and N. Halfon offered critical reviews and editorial comments.
Human Participant Protection This study was approved by the Office for the Protection of Research Subjects at the University of California, Los Angeles. Informed consent was obtained from all study participants.
References
- 1.Lyons-Ruth K, Wolfe R, Lyubchik A, Steingard R. Depressive symptoms in parents of children under age 3: sociodemographic predictors, current correlates, and associated parenting behaviors. In: Halfon N, McLearn KT, Schuster MA, eds. Child Rearing in America: Challenges Facing Parents With Young Children. Cambridge, England: Cambridge University Press; 2000:217–259.
- 2.Murray CJL, Lopez AD, eds. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass: Harvard School of Public Health; 1996.
- 3.Beardslee WR, Bemporad J, Keller MB, Klerman GL. Children of parents with major affective disorder: a review. Am J Psychiatry. 1983;140:825–832. [DOI] [PubMed] [Google Scholar]
- 4.Downey G, Coyne JC. Children of depressed parents: an integrative review. Psychol Bull. 1990;108: 50–76. [DOI] [PubMed] [Google Scholar]
- 5.Cummings EM, Davies PT. Maternal depression and child development. J Child Psychol Psychiatry. 1994;35:73–112. [DOI] [PubMed] [Google Scholar]
- 6.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458–490. [DOI] [PubMed] [Google Scholar]
- 7.Cummings EM, Davies PT, Campbell SB. Development Psychopathology and Family Process: Theory, Research and Clinical Implications. New York, NY: Guilford Press; 2000.
- 8.Sharp D, Hay DF, Pawlby S, Schmucker G, Allen H, Kumar R. The impact of postnatal depression on boys’ intellectual development. J Child Psychol Psychiatry. 1995;36:1315–1336. [DOI] [PubMed] [Google Scholar]
- 9.Gross D, Conrad B, Fogg L, Willis L, Garvey C. A longitudinal study of maternal depression and pre-school children’s mental health. Nurs Res. 1995;44: 96–101. [PubMed] [Google Scholar]
- 10.Oyserman D, Bybee D, Mowbray C. Influences of maternal mental illness on psychological outcomes for adolescent children. J Adolesc. 2002;25:587–602. [DOI] [PubMed] [Google Scholar]
- 11.Leibowitz A. Home investment in children. J Political Economy. 1974;82:111–131. [Google Scholar]
- 12.Kilburn ME, Wolfe BL. Resources devoted to child development by families and society. In: Halfon N, McLearn KT, Schuster MA, eds. Child Rearing in America: Challenges Facing Parents With Young Children. Cambridge, England: Cambridge University Press; 2002:21–49.
- 13.Kessler RC, Cleary PD. Social class and psychological distress. Am Sociol Rev. 1980;45:463–478. [PubMed] [Google Scholar]
- 14.Belle D, Longfellow C, Makosky V, Saunders E, Zelkowitz P. Income, mothers’ mental health, and family functioning in a low-income population. ANA Publ. June 1981:28–37. [PubMed]
- 15.Heneghan AM, Silver EJ, Bauman LJ, Westbrook LE, Stein RE. Depressive symptoms in inner-city mothers of young children: who is at risk? Pediatrics. 1998;102:1394–1400. [DOI] [PubMed] [Google Scholar]
- 16.Kahn RS, Wise PH, Kennedy BP, Kawachi I. State income inequality, household income, and maternal mental and physical health: cross sectional national survey. BMJ. 2000;321:1311–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall LA, Williams CA, Greenberg RS. Supports, stressors, and depressive symptoms in low-income mothers of young children. Am J Public Health. 1985; 75:518–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mathiesen KS, Tambs K, Dalgard OS. The influence of social class, strain and social support on symptoms of anxiety and depression in mothers of toddlers. Soc Psychiatry Psychiatr Epidemiol. 1999;34:61–72. [DOI] [PubMed] [Google Scholar]
- 19.Young KT, Davis K, Schoen C. The Commonwealth Fund Survey of Parents With Young Children. New York, NY: Commonwealth Fund; 1998.
- 20.Halfon N, Olson L, Inkelas M, et al. Summary statistics from the National Survey of Early Childhood Health. Vital Health Stat 15. 2000;No. 3.
- 21.Blumberg SJ, Olson L, Osborn L, Srinath KP, Harrison MA. Design and operation of the National Survey of Early Childhood Health, 2000. Vital Health Stat 1. 2002;No. 40. [PubMed]
- 22.Stewart AL, Hays RD, Ware JE Jr. The MOS Short-Form General Health Survey: reliability and validity in a patient population. Med Care. 1988;26: 724–735. [DOI] [PubMed] [Google Scholar]
- 23.Berwick DM, Murphy JM, Goldman PA, Ware JE Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29: 169–176. [DOI] [PubMed] [Google Scholar]
- 24.Andersen R, Aday LA. Access to medical care in the U.S.: realized and potential. Med Care. 1978;16: 533–546. [DOI] [PubMed] [Google Scholar]
- 25.Gershoff ET, Aber JL, Raver CC. Child poverty in the United States: an evidence-based conceptual framework for programs and policies. In: Jacobs F, Wertlieb D, Lerner RM, eds. Promoting Positive Child, Adolescent, and Family Development Through Research Policies and Programs. Thousand Oaks, Calif: Sage Publications; 2003:81–136.
- 26.Birtchnell J, Masters N. Poverty and depression. Practitioner. 1989;233:1141–1146. [PubMed] [Google Scholar]
- 27.Mirowsky J, Ross CE. Age and the effect of economic hardship on depression. J Health Soc Behav. 2001;42:132–150. [PubMed] [Google Scholar]
- 28.Epitab—tables for epidemiologists. In: Stata Survival Analysis and Epidemiological Tables. College Station, Tex: StataCorp; 2003:20–70.
- 29.Parrot S, Wu N. States Are Cutting TANF and Child Care Programs. Washington, DC: Center on Budget and Policy Priorities; 2003.
- 30.Zedlewski SR. Left Behind or Staying Away? Eligible Parents Who Remain Off TANF. Washington, DC: Urban Institute; 2002.
- 31.Special Supplemental Food Program for Women, Infants, and Children (WIC): Eligibility and Coverage Estimates, 1994 Update—U.S. and Outlying Areas. Alexandria, Va: US Dept of Agriculture, Office of Analysis and Evaluation; 1995.
- 32.Child Care: Recent State Policy Changes Affecting the Availability of Assistance for Low-Income Families. Washington, DC: US General Accounting Office; 2003.
- 33.Matthews H, Ewen D. President’s Budget Projects 300,000 Low-Income Children to Lose Child Care by 2010. Washington, DC: Center for Law and Social Policy; 2004.
- 34.Brooks-Gunn J. Big cities and their families: integration of research and practice. In: Kahn AJ, Kamerman SB, eds. Children and Their Families in Big Cities: Strategies for Service Reform. New York, NY: Columbia University School of Social Work, Cross National Studies Research Program; 1996.
- 35.Waddell B, Shannon M, Durr R. Using Family Resource Centers to Support California’s Young Children and Their Families. Los Angeles, Calif: Center for Healthier Children, Families and Community, University of California, Los Angeles; 2001.
- 36.Gomby DS. Home visiting: recent program evaluations: analysis and recommendations. Future Child. 1999;9:4–26. [PubMed] [Google Scholar]
- 37.Halfon N, McLearn KT, Schuster MA, eds. Child Rearing in America: Challenges Facing Parents With Young Children. Cambridge, England: Cambridge University Press; 2000.
- 38.Orr ST, James S. Maternal depression in an urban pediatric practice: implications for health care delivery. Am J Public Health. 1984;74:363–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kahn RS, Wise PH, Finkelstein JA, Bernstein HH, Lowe JA, Homer CJ. The scope of unmet maternal health needs in pediatric settings. Pediatrics. 1999;103: 576–581. [DOI] [PubMed] [Google Scholar]
- 40.Olson AL, Dietrich AJ, Prazar G, et al. Two approaches to maternal depression screening during well child visits. J Dev Behav Pediatr. 2005;26:169–176. [DOI] [PubMed] [Google Scholar]
- 41.Pignone MP, Gaynes BN, Rushton JL, et al. Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2002;136:765–776. [DOI] [PubMed] [Google Scholar]
- 42.Campbell SB, Cohn JF, Meyer T. Depression in first-time mothers: mother-infant interaction and depression chronicity. Dev Psychol. 1995;31:349–357. [Google Scholar]
- 43.Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry. 2002;63(suppl 8):24–34. [PubMed] [Google Scholar]


