Abstract
Objective
To establish statewide medication, disease management, and other clinical programs to serve as advanced pharmacy practice experience (APPE) training sites for the University of Colorado at Denver and Health Sciences Center School of Pharmacy, and to guarantee year-round support for the programs by providing pharmacy students with the necessary competencies to carry a significant proportion of each program's workload.
Methods
Partnerships with pharmacies willing to use students to expand their scope of clinical practice or support existing programs were established. Partners were asked to choose the clinical program(s) they wished implemented or supported and were guaranteed that APPE students would contribute to carrying each program's clinical service workload for 48 week/year under the supervision of the partners' pharmacists. In addition, partners implementing new programs were offered other support, including equipment, supplies, and training and mentoring for their pharmacists.
Evaluation
Twenty-two partnerships involving anticoagulation, diabetes, immunization, medication reconciliation, and other clinical programs were established with hospital, community, and community health center pharmacies. The partnerships provided 213 APPE placements in the 2006-2007 academic year.
Conclusion
This work demonstrates that by using innovative approaches, a pharmacy school can form new partnerships with hospital, community health center, and community pharmacies, as well as work with existing clinical programs, to create a variety of medication, disease management, and other APPEs to meet its increasing placement needs and evolving accreditation standards.
Keywords: pharmacy student, competency, advanced pharmacy practice experience, accreditation standards
INTRODUCTION
Accreditation standards for American colleges and schools of pharmacy have undergone substantial change over the last decade. In 1997, the Accreditation Council for Pharmacy Education (ACPE) announced its intention to stop accrediting baccalaureate pharmacy programs and published its Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. The 1997 document emphasized experiential education and that emphasis was further strengthened in the new standards and guidelines adopted in January 2006.1 Consequently, experiential educators are faced with the challenges of improving the quality of introductory and advanced pharmacy practice experience (IPPE and APPE) courses and increasing the quantity of experiential training sites.2-7
Accreditation standards state that upon graduation students must be competent to practice independently and ensure optimal medication therapy outcomes through multiple means including medication and disease management programs.1 To meet those standards, the University of Colorado at Denver and Health Sciences Center School of Pharmacy (UCDHSC-SOP) has taken the position that students should be taught the competencies required for pharmacy practice early in the curriculum8-11 and that students in APPE courses should be given the responsibility to apply those competencies in practice settings. Advanced pharmacy practice experience training, if it is to help students develop the self-confidence and experience needed to practice independently, must give each student multiple opportunities to carry significant patient care responsibilities in a variety of practice settings including medication and disease management programs. Accordingly, colleges and schools of pharmacy must establish strategies to identify and, if necessary, create those opportunities. This paper describes a strategy used by UCDHSC-SOP involving partnerships with community pharmacies and community health center and hospital pharmacies willing to utilize students in APPE training to help implement and operate new clinical programs or support existing programs.
DESIGN
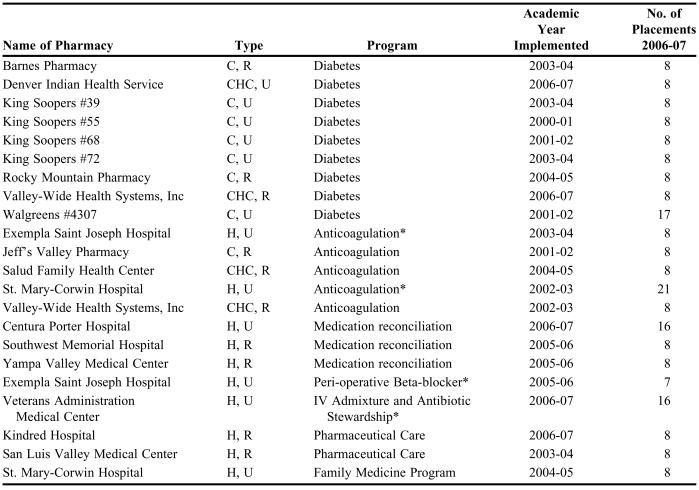
The UCDHSC-SOP sought partnerships with community pharmacies and community health center and hospital pharmacies willing to utilize students to help implement and operate new medication and disease management or other programs, or support existing programs. Partners were asked to name their choice of program (eg, diabetes, anticoagulation, medication reconciliation) and guaranteed that an APPE student would work with them on the program for 48 weeks per year (8 students, each for 6 weeks). Partners interested in implementing new programs were offered training and mentoring for their pharmacists to operate and supervise those programs and were asked to provide a private clinic area for each program. In addition, the partners were promised equipment and supplies, help to address legal requirements, assistance in establishing policies and procedures, and liaison with local healthcare practitioners. Table 1 lists the partnership organizations and the types of programs developed. The following are descriptions of the partnership programs.
Table 1.
Partnership Programs Established to Address Patient Care Needs and Facilitate Advanced Pharmacy Practice Experiences
*Existing program supported by students rather than implementation of a new program
C = community pharmacy; CHC = community health center pharmacy; H = hospital pharmacy; U = urban; R = rural
Diabetes, Lipid and Hypertension Programs
The diabetes/lipid/hypertension programs were based on the American Diabetes Association's evidence-based guidelines. The core program, modifiable to meet the needs of individual patients and practice sites, consists of 6 monthly meetings between the pharmacist and the patient, with the first visit focused on patient evaluation, visits 2-5 on patient self-management education, and visit 6 on assessment of health outcomes. Patients visited each clinic by appointment. The pharmacy students carried out the care planned for each appointment (education, “point of care” laboratory monitoring, etc) and at the end of each appointment, presented the case to their on-site preceptor, including recommendations to improve care based on their evaluation of the case. The preceptor reviewed the case and approved the student's recommendations or, if necessary, redirected him/her to ensure patient safety. The student completed the appointment by documenting the case activities and forwarding a progress note cosigned by the preceptor to the patient's physician, including any recommendations for changes in therapy that had been approved by the preceptor.
Several strategies were used to provide the faculty support needed to implement the diabetes/lipid/hypertension programs. The King Soopers and Walgreens programs were established by 2 “shared” pharmacy faculty members; however, both of those positions eventually transformed into full-time King Soopers and Walgreens appointments. Other programs were implemented by school faculty members with 20%-100% salary offset provided by competitive grant funds.
Each faculty member for each program established a working relationship with one or a small group of local physicians and provided care to patients with diabetes who were referred to the pharmacy-based program by those physicians. That approach allowed the policies and procedures of the clinics to be established in collaboration with the physicians and facilitated didactic and clinical skills training for the partners' pharmacists. It also allowed the faculty members to transition the workload of running the clinics to the fourth-year pharmacy students under the supervision of the partners' pharmacists and eventually for the faculty members to withdraw to serve in an off-site consulting support role. In addition, it permitted the partners to grow the clinics' workload incrementally over time with the gradual inclusion of more physicians and patients.
Anticoagulation (Warfarin) Clinics
The community and community health center pharmacy anticoagulation clinics focused on maintaining patients' International Normalized Ratio (INR) values within the accepted target ranges for their medical conditions and, similar to the diabetes/lipid/hypertension clinics, were based on the principle of patient self-management. Patient care, including the role of students in delivering that care, was provided in a manner similar to that used in the diabetes/lipid/hypertension clinics (see above). New patients were seen on a frequent basis for self-management education and until their INR values were stabilized and then on a regular maintenance basis.
The Salud community health center partnership was established by a UCDHSC-SOP faculty member with 20% salary offset provided by grant funds. The partnership with Jeff's Valley community pharmacy was initially established as an outreach activity of the St. Mary-Corwin program (see below) but evolved into a standalone program with grant support from UCDHSC-SOP and didactic and clinical anticoagulation training from St. Mary-Corwin Hospital. The Valley-Wide Health Systems (VWHS) community health center anticoagulation partnership was initially operated full time, with student support, by a pharmacist added to the VWHS staff through a competitive grant obtained by UCDHSC-SOP. That pharmacist trained other VWHS pharmacists to operate the program and, subsequent to his resignation, the program has operated under their supervision with students carrying the majority of the program's workload.
Exempla Saint Joseph Hospital and St. Mary-Corwin Hospital (www.warfarinfo.com) had existing pharmacist-run anticoagulation programs and those partnerships demonstrated student support of existing programs rather than assistance to implement new programs. No faculty member or other resources were involved in those partnerships other than the guarantee of students to support the 2 programs. Each student was given direct patient care responsibilities including writing notes and medication orders, educating patients and caregivers, and documenting activities. Each student's patient care activities were reviewed with a preceptor on a daily basis before orders and notes were entered in the patients' medical records and cosigned by the preceptor.
Other Programs
The medication reconciliation programs were implemented to meet Joint Commission on Accreditation of Health Care Organizations (JCAHO) accreditation standards.12 The students established a list of new patients' current home therapies including prescription, nonprescription, and herbal and complementary medications, and the dosage, frequency and route of administration of those medications. The students compared admission, transfer, and/or discharge medication orders to the information they established and assessed the appropriateness of all medications. They brought discrepancies and recommendations to the attention of each patient's physician under the oversight of the hospital's pharmacists and documented their activities in patients' health care records.
Students in Southwest Memorial Hospital operated a vaccination program (all students in the UCDHSC-SOP second-professional year curriculum completed the American Pharmacists Association's Pharmacy-Based Immunization Delivery, a national certificate program for pharmacists). They followed a hospital-approved protocol for identifying patients with immunization deficits and immunized those willing to receive vaccine(s). In addition, the students provided tuberculosis skin testing and tetanus vaccination services to the hospital's employees. Vaccination services were also provided by students in the Indian Health, King Soopers, and Walgreens diabetes clinics.
After gaining experience with the student-supported anticoagulation program, Exempla Saint Joseph Hospital formed a second partnership with UCDHSC-SOP for students to support an established pharmacy-run perioperative beta-blocker program. The program screened adult non-cardiac preoperative patients for cardiovascular risk and brought moderate and high-risk patients to the attention of the patients' surgeons and/or anesthesiologists for beta-blocker initiation. In addition, the service screened all postoperative patients to ensure that beta-blockers were continued.
The VAMC partnership differed from all other partnerships in that it involved 2 streams of students who supported an intravenous (IV) admixture and an antibiotic stewardship service. Each service was supported by 1 student at a time, but the responsibilities were exchanged halfway through the 6-week APPE to give the students a 3-week experience performing each service. Each student was given a 1-day introduction to the antibiotic stewardship program and then expected to provide pharmaceutical care to all inpatients receiving intravenous antibiotic therapy (usually 25-30 patients per day). The student assessed the indication for each antibiotic on a daily basis and, as new information (eg, culture and sensitivity data) became available, the student brought recommendations to his/her preceptor's attention for approval. Each student was given a 3-day introduction to the IV admixture service, including training in sterile techniques and for the remainder of his/her 3 weeks was expected to prepare non-chemotherapy IV admixtures under supervision.
Kindred Hospital was a long-term acute care facility that specialized in ventilator weaning, wound care, and traumatic brain injury. The pharmacy students participated in daily rounds with a multidisciplinary healthcare team. The students were also responsible for providing pharmaceutical care services including anticoagulation therapy, pharmacokinetic monitoring, and drug information services to 35-45 patients/day. Students in the San Luis Valley Regional Medical Center partnership supported a rehabilitation program for patients recovering from strokes, heart attacks, and accidents (primarily motor vehicle-related). The team conducted daily rounds and the students, under the supervision of the hospital's pharmacists, were responsible for identifying patients' drug-related problems and making recommendations for the resolution of those problems. The St. Mary-Corwin Hospital family medicine partnership provided pharmaceutical care support to a family medicine residency program.
ASSESSMENT
The UCDHSC-SOP established 22 patient care partnerships with community pharmacies and community center and hospital pharmacies between 2001 and 2007. These included 9 diabetes/lipid/hypertension clinics, 5 anticoagulation clinics, and 8 other programs involving antibiotic stewardship/IV admixture preparation, pharmaceutical care, and medication reconciliation, perioperative beta-blockade, and vaccination services. Ten partnerships were formed with rural partners and 12 with urban partners. Eighteen of the partnerships established clinical programs that did not previously exist and 4 involved existing services. Nine were established with the on-site support of UCDHSC-SOP faculty members and 11 were established with equipment, supplies, and other support derived from competitive grant funds obtained by UCDHSC-SOP faculty members. Ten partnerships were established without UCDHSC-SOP involvement other than the guarantee of at least 8 APPE students per year to support each partner's program.
The partnerships provided 213 advanced pharmacy practice experiences in the 2006-2007 academic year. The school's class size was 130 students and the 213 placements represented more than 20% of all APPE placements needed. The UCDHSC-SOP APPE program is comprised of 7 courses and, on average, each student in 2006-2007 completed approximately 1.5 APPE courses in a partnership program.
Students demonstrated the competencies expected of them in delivering patient care services at the partnership sites. The UCDHSC-SOP implemented a competency-based APPE assessment system in 2004 and, of the 372 students who have completed a partnership APPE since that time, only 1 received a failing grade (for reasons not associated with patient care activities).13
DISCUSSION
This paper describes a strategy for developing advanced pharmacy practice experiences. It demonstrates that a pharmacy school can form partnerships with hospital, community health center, and community pharmacies to create a variety of medication, disease management, and other programs in which students in APPE courses are expected to carry a substantial workload including providing patient care services. It also demonstrates that a pharmacy school can form partnerships that allow students to support existing clinical programs and create a significant proportion of the placements needed for its APPE program.
The concept of partnerships between pharmacy schools and practice sites to enhance pharmacy practice is not new and there are multiple examples of academic outreach programs involving community and hospital pharmacies.14-19 Similarly, recognition that pharmacy students can provide patient care services is not new. There are multiple examples which describe and quantify the value of baccalaureate and PharmD students in experiential courses including examples of student-supported programs.20-31 However, none describe the development of a variety of statewide programs established on the promise of year-round support by APPE students expected to arrive on site with the necessary competencies to carry a significant proportion of each program's clinical workload.
Recent publications from AACP and ACPE state that graduates must be independent practitioners competent to provide direct patient care, including medication and disease management.1,5 Individual schools and colleges must decide how best to achieve that objective and the traditional and still well-established approach has been to provide students with an initial didactic education followed by APPE training which relies on preceptors to teach students how to apply knowledge in practice settings.4,32,33 However, that approach means students arrive at APPE practice sites as dependent rather than independent learners. This enhances the view that students are likely to disrupt rather than enhance normal pharmacy operations.1,34-37 The result is that colleges and schools may have difficulty finding enough APPE placements to meet their needs and that preceptors expect remuneration for student supervision.3,6
Traditional views of clerkship education have been challenged and increased expectations for pharmacy students in experiential education have been discussed.4,5,36,38-40 The UCDHSC-SOP has taken the position that APPE education should provide students with patient care responsibilities for the purpose of building the experience and self-confidence needed by independent pharmacy practitioners. Students should be given increasing patient care responsibilities throughout the IPPE program8-11 and should start their final year of supervised training competent to care for patients in medication and disease management and other clinical programs. Pharmacy students in APPE training, similar to the education of physicians, should be given patient care responsibilities consistent with that expectation. Physicians are expected to function throughout their final year of supervised training at the level of an independent practitioner before becoming board certified (written communication, DC Leach, Executive Director, Accreditation Council for Graduate Medical Information, Chicago, Ill, August 2006). In medicine, students must complete a residency before becoming fully licensed independent practitioners and, therefore, it is during their final year of residency that they are expected to function at the level of an independent practitioner. In contrast, pharmacy students are not required to complete a residency program before becoming fully licensed independent practitioners and, accordingly, it is throughout their APPE training that they should be expected to function at the level of an independent practitioner.
Many of today's preceptors were themselves trained in a traditional teacher-centered model, which allowed them very little independent activity as students. As a result, it can be difficult for them to allow APPE students to function independently.23 Accordingly, it has been important to identify institutions that recognize the first professional doctor of pharmacy program as a major change from previous programs and to identify preceptors who are willing to give significant patient care and other responsibilities to students. In addition, it has been important to identify institutions and preceptors who value the work performed by students and who, as a result, do not expect remuneration for the supervision of those students.
The strategy requires students to provide clinical services year round and the fact that programs have been sustained for as long as 5 years is evidence that the students have functioned at a level that has made the partnerships successful. The school's post-baccalaureate PharmD APPE program consisted of seven 6-week courses running over 42 weeks per year. That was changed to seven 6-week courses running over 48 weeks per year in the new curriculum, which permits year-round service. Each student is asked to select one 6-week vacation period during the APPE year and, by not permitting all the students to choose the same 6 weeks, each partnership site can be guaranteed 8 students per year. The 4 weeks without any students are split into two 2-week blocks at the end of the fall and spring semesters. The partners are able to schedule patient appointments around those gaps or, if necessary, use their own pharmacists to provide service.
The first professional degree doctor of pharmacy curriculum is a general degree program; thus, it is an accreditation requirement that students gain experience across a broad range of pharmacy practice sites. Accordingly, it is important that partnerships have been developed with hospital, community health center, and community pharmacies; that the partners have chosen to implement a variety of clinical programs; and that the partnerships do not preclude students from experiencing a wide variety of activities at a partnership site. For example, the Southwest Memorial Hospital partnership exposes students to unit-dose drug distribution activities while the community pharmacy partnerships expose students to traditional dispensing and patient counseling activities.
Many partners chose to implement diabetes clinics and, given the morbidity and mortality associated with the disease, it would be of value to have 17 diabetes clinics, which is the minimum number needed to provide each student with 1 experience in this setting (130 students per class and 8 students per clinic per year). Similarly, it would be valuable to have additional medication and disease management and other programs in order to give each fourth-professional year student multiple opportunities to develop the experience and self-confidence needed to be independent practitioners. However, it is unclear how many partnerships the school can sustain. Assigning students to partnerships in the metropolitan Denver area is a simple task, but it is more difficult to guarantee students to a large number of rural sites. Some students, including those who are single parents, have legitimate reasons not to want to undertake an APPE course in a remote rural area. Also, for every student sent to a rural site there is the responsibility of finding housing for him/her and support for the associated costs. Nonetheless, the development of multiple partnerships has not been difficult. Health care foundations and other organizations have recognized that there are disadvantaged populations in Colorado, particularly with respect to the care and education of patients with chronic diseases in rural areas, and have supported the UCDHSC-SOP in its efforts to implement partnership programs with approximately $2.5 million in funding. Agreements are in place to develop an additional 7 diabetes/lipid/hypertension programs, 3 anticoagulation programs, and a medication reconciliation program in the 2007-2008 academic year.
The primary limitation of this paper is that it does not compare the educational outcomes of the new partnership APPE courses with those of the school's longstanding traditional APPE courses. The expectation for fourth-professional year students to function at the level of independent practitioners is significantly different from the traditional APPE model where students are expected to learn by observing skilled practitioners. Given evolving accreditation standards, it will be important to measure and compare the educational outcomes of the school's new and traditional APPE courses.
A further limitation is that it is beyond the scope of this paper to present health outcome data for each partnership. Nonetheless, preliminary data from 1 diabetes clinic has been published and shows a significant reduction from baseline in mean body weight, glycosylated hemoglobin A1c, systolic and diastolic blood pressure, and LDL-cholesterol in the first 53 patients to complete the self-management program.41 The VWHS anticoagulation clinic currently cares for approximately 100 patients and conducts approximately 200 appointments per month. The clinic's proportion of INR values in therapeutic range for the past year was 66%, which is consistent with published standards.42,43 By continuing to refer patients to the partnership programs, physicians have demonstrated an ongoing acceptance and support of the programs and, by implication, that the programs are helping patients to achieve improved health outcomes.
CONCLUSIONS
A strategy to develop advanced pharmacy practice experiences was introduced. The UCDHSC-SOP has partnered with hospital, community, and community health center pharmacies willing to utilize students in APPE training to help implement and operate medication and disease management and other services, and to support existing programs. The strategy is helping the School to pursue its mission to educate pharmacy students in accordance with evolving accreditation standards, promote the development of pharmacy practice in Colorado, and provide service to Colorado communities.
ACKNOWLEDGMENTS
This work described in this paper was supported by financial contributions from The Caring for Colorado Foundation, The Colorado Health Foundation, The Colorado Trust Foundation, The Herman and Ethel Horwich Charitable Trust, King Soopers and Walgreens.
REFERENCES
- 1. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Adopted January 15, 2006. Available at http://www.acpe-accredit.org/. Accessed June 28, 2006.
- 2.Lin Ay, Altiere RJ, Harris WT, et al. Leadership: the nexus between challenge and opportunity. Reports of the 2002-03 Academic Affairs, Professional Affairs, and Research and Graduate Affairs Committees. Am J Pharm Educ. 2003;67(3) Article S05. [Google Scholar]
- 3.Harralson AF. Financial, personnel, and curricular characteristics of advanced practice experience programs. Am J Pharm Educ. 2003;67(1) Article 17. [Google Scholar]
- 4.Littlefield LC, Haines ST, Harralson AF, Schwartz AH, Sheaffer SL, Zeolla MM, Flynn AA. Academic pharmacy's role in advancing practice and assuring quality in experiential education: report of the 2003-2004 professional affairs committee. Am J Pharm Educ. 2004;68(3) Article S8. [Google Scholar]
- 5.Cohen JL, Nahata MC, Roche VF, Smith RE, Wells BG, Helling D, Maine LL. Pharmaceutical care in the 21st century: from pockets of excellence to standard of care. Report of the 2003-04 Argus Commission. Am J Pharm Educ. 2004;68(3) Article S9. [Google Scholar]
- 6.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice experience placements: a 5-year update. Am J Pharm Educ. 2005;69(3) Article 45. [Google Scholar]
- 7. Reynolds JR, Briceland LL, Carter JT, Easton MR, Rider JM, Staton AG, Talluto BA, Tice BP, Flynn AA. Experiential education delivery: ensuring success through support and development of the faculty and administrative team. Report of the 2004-2005 American Association of Colleges of Pharmacy Professional Affairs Committee. Available at http://www.aacp.org/site/page.asp?TRACKID=&VID=1&CID=1184&DID=6825 Accessed June 28, 2006.
- 8.Turner CJ, Jarvis C, Altiere R, Clark L. A patient-focused and outcomes-based experiential course for first year pharmacy students. Am J Pharm Educ. 2000;64:312–9. [Google Scholar]
- 9.Jarvis C, James VL, Giles J, Turner CJ. (2004) Nutrition and nurturing: a service-learning nutrition pharmacy course. Am J Pharm Educ. 2004;68(2) Article 43. [Google Scholar]
- 10.Turner CJ, Altiere R, Clark L, Dwinnell B, Barton AJ. An interdisciplinary introductory pharmacy practice experience course. Am J Pharm Educ. 2004;68(1) Article 10. [Google Scholar]
- 11.Turner CJ, Altiere R, Clark L, Maffeo C, Valdez C. Competency-based introductory pharmacy practice experiential courses. Am J Pharm Educ. 2005;69(2) Article 21. [Google Scholar]
- 12.Hunter WB, Frisch CJ, Cardwell JR. Case example: design and implementation of a medication reconciliation process in preparation for conversion to a paperless system. In: Piscoran S, editor. Medication Reconciliation Handbook. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations; 2006. pp. 104–108. [Google Scholar]
- 13.Turner CJ, Altiere R, Fish D, Giles J, Page R, Sintek C, Ulrich H, Valdez C, Vondracek S, Zadvorny E. An assessment system which maps CAPE outcomes in an advanced pharmacy practice experience program. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700360. Article 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz MA, Ray MD. College of pharmacy-teaching hospital relationships: report of a survey. Am J Hosp Pharm. 1985;42:803–10. [PubMed] [Google Scholar]
- 15.Kennedy DT, Ruffin DM, Goode J-VR, Small RE. The role of academia in community-based pharmaceutical care. Pharmacotherapy. 1997;17:1352–6. [PubMed] [Google Scholar]
- 16.Scott DM, Narducci WA, Jungnickel PW, Miller LG, Ranno AE, Maloley PA. Pharmaceutical care preceptor training and assessment in community pharmacy clerkship sites. Am J Pharm Educ. 1999;63:265–71. [Google Scholar]
- 17.Farris KB, Kassam R, Cox CE, Volume CI, Cave D, Schopflocher DP, Tessier G. Evaluation of a practice enhancement program to implement pharmaceutical care. Am J Pharm Educ. 1999;63:277–84. [Google Scholar]
- 18.Reutzel TJ, Hogan M, Kazerooni PV. Development of a patient-based practice model in community pharmacypractice: academic-practice interface. Am J Pharm Educ. 1999;63:119–26. [Google Scholar]
- 19.Cerulli J, Briceland LL. A streamlined training program for community pharmacy advanced practice preceptors to enable optimal experiential learning opportunities. Am J Pharm Educ. 2004;68(1) Article 9. [Google Scholar]
- 20.Briceland LL, Kane MP, Hamilton RA. Evaluation of patient-care interventions by Pharm.D. clerkship students. Am J Hosp Pharm. 1992;49:1130–2. [PubMed] [Google Scholar]
- 21.Slaughter RL, Erickson SR, Thomson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacotherapy. 1994;28:665–70. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 22.Chisholm MA, Hawkins DW, Taylor AT. Providing pharmaceutical care: are pharmacy students beneficial to patients? Hosp Pharm. 1997;32:370–5. [Google Scholar]
- 23.Sauer BL, Heeren DL, Walker RG, King JH, Musallam NA. Computerized documentation of activities of Pharm.D. clerkship students. Am J Health-Syst Pharm. 1997;54:1727–32. doi: 10.1093/ajhp/54.15.1727. [DOI] [PubMed] [Google Scholar]
- 24.Dennehy CE, Kroon LA, Byrne M, Koda-Kimble MA. Increase in number and diversity of clinical interventions by PharmD students over a clerkship rotation. Am J Pharm Educ. 1998;62:373–9. [Google Scholar]
- 25.Stratton TP, Cochran GA. A rural geriatric health experience. Am J Pharm Educ. 1998;62:151–5. [Google Scholar]
- 26.Isetts BJ. Evaluation of pharmacy students' abilities to provide pharmaceutical care. Am J Pharm Educ. 1999;63:11–20. [Google Scholar]
- 27.Brockmiller H, Abel SR, Koh-Knox CP, Birk CW. Cost impact of Pharm.D. candidates' drug therapy recommendations. Am J Health-Syst Pharm. 1999;56:882–4. doi: 10.1093/ajhp/56.9.882. [DOI] [PubMed] [Google Scholar]
- 28.Reddick JB, Murphy JE. Evaluating the clinical interventions of students during clerkships using a cognitive services claim form. Am J Pharm Educ. 2000;64:38–43. [Google Scholar]
- 29.Freml JM, Farris KB, Fang G, Currie J. Iowa Priority's brown bag medication reviews: a comparison of pharmacy students and pharmacists. Am J Pharm Educ. 2004;68(2) Article 50. [Google Scholar]
- 30.Mobley Smith MA, Koronkowski MJ, Petersen NM. Enhancing student learning through integrating community-based geriatric educational outreach into ambulatory care advanced practice experiential training. Am J Pharm Educ. 2004;68(1) Article 20. [Google Scholar]
- 31.Skledar SJ, McKaveney TP, Ward CO, Culley CM, Ervin KC, Weber RJ. Advanced practice internship: experiential learning in a drug use and disease state management program. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700368. Article 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dugan BD. Enhancing community pharmacy through advanced pharmacy practice experiences. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700121. Article 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thomas RA. Developing structured-learning exercises for a community advanced pharmacy practice experience. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700123. Article 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson RJ. Assessment of clinical service contracts between hospital pharmacies and colleges of pharmacy. Hosp Pharm. 1992;27:503–7. [PubMed] [Google Scholar]
- 35.Commission to Implement Change in Pharmaceutical Education. Background Paper II: Entry-level, curricular outcomes, curricular content and educational process. Am J Pharm Educ. 1993;57:377–85. [Google Scholar]
- 36.Austin Z, Duncan-Hewitt W. Faculty, student, and practitioner development within a community of practice. Am J Pharm Educ. 2005;69(3) Article 55. [Google Scholar]
- 37.Davis SM, Rudd CC. Cost of training doctor of pharmacy students in a clinical practice setting. Am J Hosp Pharm. 1990;47:2288–90. [PubMed] [Google Scholar]
- 38.Slack MK, Draugalis JR. Models for estimating the impact of clerkship students on pharmacy practice sites. Am J Hosp Pharm. 1994;51:525–30. [PubMed] [Google Scholar]
- 39.Raehl CL, Bond CA, Pitterle ME. Clinical pharmacy services in hospitals educating pharmacy students. Pharmacotherapy. 1998;18:1093–1102. [PubMed] [Google Scholar]
- 40.Broadhead RS, Facchinetti NJ. Clinical clerkships in professional education: a study in pharmacy and other ancillary professions. Soc Med Sci. 1985;20:231–40. doi: 10.1016/0277-9536(85)90236-9. [DOI] [PubMed] [Google Scholar]
- 41. Ellis SL, McCollum M, Lorenzo J, Turner CJ. Clinical outcomes associated with a rural community pharmacy diabetes program developed in collaboration with the University of Colorado School of Pharmacy. American College of Clinical Pharmacy, 2006 Spring Practice and Research Forum, Abstract 120. Available at www.pharmacotherapy.org/pdf/ACCP-Spring_Abstracts_2006.pdf/. Accessed September 1, 2006.
- 42.Chiquette E, Amato MG, Bussey HI. Comparison of an anticoagulation clinic with usual medical care: anticoagulation control, patient outcomes, and health care costs. Arch Intern Med. 1998;158:1641–7. doi: 10.1001/archinte.158.15.1641. [DOI] [PubMed] [Google Scholar]
- 43.Witt D, Sadler M, Shanahan R, Mazzoli G, Tillman D. Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest. 2005;127:1515–22. doi: 10.1378/chest.127.5.1515. [DOI] [PubMed] [Google Scholar]