Abstract
Objective
To assess the effect of simulation-based learning on doctor of pharmacy (PharmD) students' ability to perform accurate blood pressure assessments and to measure student satisfaction with this novel teaching method.
Methods
Didactic lectures on blood pressure assessment were combined with practical sessions using a high-fidelity computerized patient simulator. Before and after the simulation sessions, students completed a written objective examination to assess knowledge and completed a survey instrument to determine their attitudes regarding the learning experience. Individual clinical skills were assessed using the patient simulator.
Results
Ninety-five students completed the study. Significant improvement was seen in students' knowledge and their ability to accurately determine blood pressure following simulation sessions. Survey responses indicated that students felt confident that simulation-based learning would improve their ability to perform accurate blood pressure assessments.
Conclusion
Pharmacy students showed significant improvement in clinical skills performance and in their knowledge of the pharmacotherapy of hypertension. Students expressed high levels of satisfaction with this type of learning experience.
Keywords: patient simulation, cardiovascular disease, hypertension, blood pressure
INTRODUCTION
Cardiovascular disease remains the leading cause of mortality in the United States. In 2003, the American Heart Association reported that over 65 million Americans have high blood pressure.1 Nearly 2,500 Americans die of cardiovascular disease each day. Pharmacists can improve the care of patients with cardiovascular disease, including hypertension,2-6 and pharmacist involvement improves not only clinical outcomes but economic outcomes as well.7-9 Thus, colleges and schools of pharmacy are challenged with preparing students to perform appropriate intervention activities, such as blood pressure monitoring, patient counseling on antihypertensive medications, and pharmacotherapeutic recommendations for the management of hypertension. The standard of education to this point has been to provide structured didactic lectures, patient case scenarios, problem-based learning (PBL) techniques, and clinical assessment laboratories to teach the fundamentals of blood pressure assessment and management of hypertension.
Studies have evaluated training and assessment programs involving simulation of patients with hypertension using either live actors or clinical preceptors.10,11 The inherent problem with training programs for blood pressure measurement is the inability to objectively verify the accuracy of each reading. When using human patients or actors, there is no way to verify that the blood pressure measurement the student obtains is accurate since a reading taken by an instructor just minutes later could reflect either an error in the student's reading or simply the normal fluctuation in blood pressure that humans experience. The assessment technique is relatively simple to perform, but the ultimate goal for the students is to obtain accurate readings each time they perform blood pressure measurement. An innovative approach to ensure accuracy of measurements is the use of programmable computerized patient simulators. Patient simulation provides a precisely controlled environment where the instructor can adjust the simulator's blood pressure and other vital signs to exact numbers. Some patient simulators even allow the instructor to view the rate at which the student is deflating the blood pressure cuff.
Patient simulation in medical education has been established in medical and nursing schools throughout the United States. Simulation-based learning (SBL) has been utilized in many disciplines, including anesthesiology,12,13 cardiology,14 obstetrics,15 emergency medicine,16,17 critical care medicine,18 team training,19,20 emergency preparedness,21 pediatrics,22 nursing,23,24 and pharmacy.25 The recommendations from the panel on General Professional Education of the Physician of the Association of American Medical Colleges and the subsequent Edinburgh Declaration supported a shift in medical education from large classroom instruction to interactive, competency-based learning.26,27 SBL represents one way of complying with these recommendations.
The purpose of this prospective trial was to assess the use of SBL on students' ability to perform accurate blood pressure assessments and to complete objective written examinations of hypertension therapy. Student satisfaction with this novel teaching method was also measured.
METHODS
SBL opportunities for pharmacy students were developed and investigated by the University of Pittsburgh School of Pharmacy.25 The patient simulator is located at the Peter M. Winter Institute for Simulation, Education, and Research (WISER) Institute, a state-of-the-art center for simulation education and research. The mannequins are controlled by Sim-Man (Laerdal Corporation, Stavanger, Norway) computer program and can be programmed to have palpable pulses, audible heart, lung, and abdominal sounds, visible hemodynamic parameters (including continuous electrocardiogram) on a monitor, and visible blood pressure cuff deflation rates. The facilitator can program the software for any blood pressure by simply entering it on the control screen. These patient simulation models also have the capability to respond by speaking. This study was approved by the Institutional Review Board of the University of Pittsburgh.
Use of a patient simulator for hands on experience in accurately measuring blood pressure was incorporated into the pharmacy curriculum of the University of Pittsburgh School of Pharmacy. The Pharmacotherapy of Cardiovascular Disease, a required course in the second-professional year, combines didactic lecturing, case presentations, small group practicals, small group literature evaluation presentations, active learning, and simulation education/evaluation. A patient simulator from the WISER Institute was brought to the classroom immediately after the didactic lecture on assessment of blood pressure and again 2 weeks after this initial practice session.
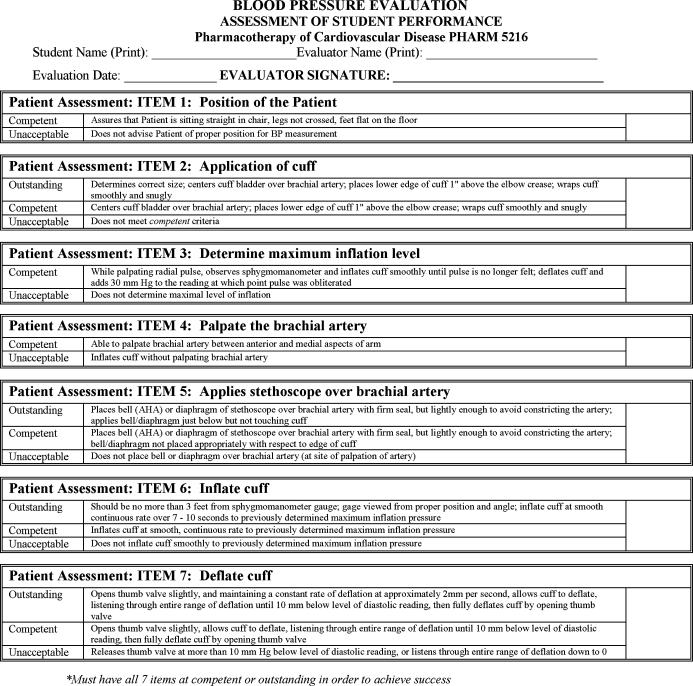
Prior to classroom practice sessions with the patient simulator, students were presented with the blood pressure grading rubric (Appendix 1) utilized to standardize assessment of student performance. Each student group, comprised of an average of 6 students, participated in one 15-minute simulation session with the human patient simulator in the large classroom setting. Each group was oriented to the capabilities of the mannequin. Two facilitators controlled the simulation for each group, with one facilitator programming the mannequin and the other facilitator at the bedside guiding students and assessing student competence. Figure 1 shows the facilitator in the simulation room providing feedback to the students. The Sim-Man software was programmed with 10 different vital signs; parameters were adjusted prior to each student's attempt to obtain a blood pressure assessment. The simulation software allows the facilitator to preprogram blood pressures to change over time or to simply enter a blood pressure on the control panel. The facilitator responsible for programming the simulator provided immediate verbal feedback to each individual student in addition to completing the grading rubric. Also, the facilitator could monitor the rate of cuff deflation via a real-time adjusting bar graph on the computer screen and see the exact numeric value of the blood pressure.
Figure 1.
The facilitator discusses pharmacy students' performance immediately after their participation in a simulation-based learning session using a patient mannequin.
At the end of the semester, each student group was assigned a 1-hour simulation session at the WISER Center for a final practical skills evaluation. During this session, each student's ability to obtain appropriate blood pressure and pulse assessments was graded for a total of 10% of their final grade for the practical sessions of the course.
Students were given a written objective examination prior to and after the hypertension section of the course to assess knowledge of blood pressure assessment. This examination was anonymous and for study purposes only. All students were evaluated by our traditional methods for the course grade, including written examinations and clinical performance assessment during all practical sessions throughout the course.
Students also completed an anonymous presimulation and postsimulation survey instrument. Each student randomly selected a code for use on both survey instruments so that changes could be assessed while maintaining anonymity. The survey instruments consisted of 4 questions that assessed students' attitudes toward their ability to accurately perform blood pressure assessment. Responses were based on a Likert scale on which 1 = poor or strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, and 5 = excellent or strongly agree.28,29 On the postsimulation survey instrument, students were also asked what they liked most about this experience, what they liked least, and for any additional written comments they would like to make.
A chi-square test was used for categorical data and analysis of variance (ANOVA) was used for assessment of rubric scores.
RESULTS
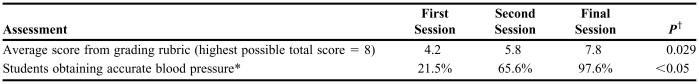
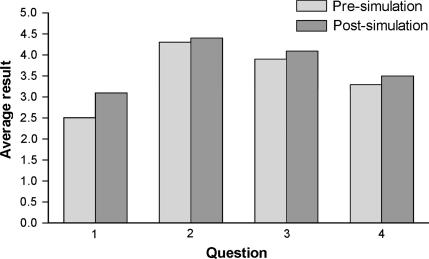
Descriptive statistics of the students in the Pharmacotherapy of Cardiovascular Disease course are shown in Table 1. One hundred two students completed the patient simulation sessions and 95 (93%) completed the written examinations and survey instruments. Seven students did not complete the anonymous examination and survey instrument, as this was not a requirement of the course. Students' blood pressure measurement skills showed significant improvement after each practice session with the patient simulator (Table 2) and also in posttest scores taken after the final session at the WISER Institute (Table 3). Survey results indicated that students had a positive attitude towards SBL even before they had any experience with this type of learning (Figure 2). Students were confident that patient simulation would improve their ability to measure blood pressure and their opinion changed little after the sessions (presimulation = 4.3 vs. postsimulation = 4.4; p value >0.05).
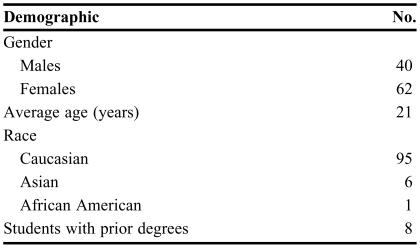
Table 1.
Descriptive Statistics of Second-Professional Year Pharmacy Students Enrolled in a Course Using Simulation-based Learning to Teach Blood Pressure Assessment, N = 102
Table 2.
Assessment of Pharmacy Students' Ability to Perform Accurate Blood Pressure Measurements
*Accurate blood pressure was defined as a reading within 5 mm Hg of the programmed blood pressure
†Difference between first and final session
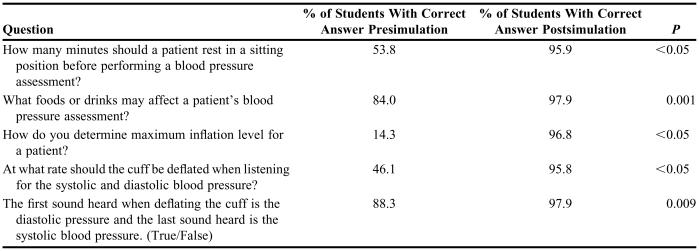
Table 3.
Presimulation and Postsimulation Examination on Blood Pressure Assessment, N = 95
Figure 2.
Presimulation and postsimulation survey results of students participating in simulation-based learning using a patient mannequin. (Question 1: How confident are you in your ability to perform a blood pressure assessment? Question 2: Do you feel that patient simulation of blood pressure monitoring will increase your ability to perform a blood pressure assessment on a patient? Question 3: Do you feel that it is a pharmacist's responsibility to perform blood pressure assessments for their patients? Question 4: Do you feel that a didactic lecture on measuring blood pressure will improve your ability to perform a blood pressure assessment?)
Student comments were extremely positive regarding the use of SBL throughout the course. Students perceived an advantage to learning on virtual patients with the use of the high-fidelity mannequins in comparison to learning on actual patients. Some comments stated that this learning environment improved their confidence and provided a safe learning environment where they were not frustrating the patients on whom they were learning. The overwhelming response throughout the class was that this teaching method should be used throughout the curriculum and that it provided the knowledge and practice that is warranted for training pharmacists.
DISCUSSION
SBL utilizing patient simulators is an innovative and novel approach to pharmacy education, providing students with an opportunity to participate in making assessments for “patients” in a safe, non-threatening environment that closely resembles an actual patient care setting. An important advantage is the ability for students in the early learning phase of their education to repeat the experience as many times as necessary to achieve competence without involving actual patients. In addition, critical clinical situations can be simulated to offer a complexity that parallels real life situations.
We have shown that SBL can improve knowledge as well as pharmacy students' performance of blood pressure assessment. Performance measurements can quickly and accurately be assessed utilizing high fidelity simulators. Students respond in a positive way to this type of innovative and interactive learning.
Schools of pharmacy have been using teaching techniques such as computerized simulations, actor simulations, case discussions, PBL, and experiential learning, in addition to didactic lecturing, for years. With advancements in technology, there are many other potential methods for teaching and learning, including SBL and other forms of virtual reality simulations. Other healthcare professions have demonstrated significant success with the use of SBL at several levels of education, including classroom instruction, clinical performance skills, and team performance training. There is support for SBL as a superior option compared to other forms of learning including PBL. Steadman and colleagues reported that fourth-year medical students undergoing SBL performed better on final assessment examinations and showed greater overall improvement in scores than students undergoing PBL.30 This confirms that “hands-on” SBL in a controlled setting better prepares students for “real-world” practice than do traditional methods of teaching.
The University of Pittsburgh School of Pharmacy is dedicated to advancing the quality of education with innovative strategies. Based on the positive experience with SBL in teaching blood pressure assessments at our institution, we are expanding the use of SBL into other areas of cardiovascular pharmacotherapy, such as dysrhythmia management, myocardial infarction, and heart failure. We are also utilizing SBL in advanced experiential learning rotations. Other potential uses for this simulation tool include assessing students' communication skills during patient interactions or during interactions with other health care professionals. This tool may also provide excellent continuing education opportunities for pharmacists who are required to respond to patient care emergencies in institutional settings.
In order to utilize simulation education via patient mannequins, technically advanced skills will be needed to incorporate this mode of learning into the curriculum. Faculty members could partner with existing simulation training centers, medical schools, nursing schools, or other training facilities to replicate this educational technique. Advanced training in patient case design, case simulation development, debriefing tool preparation, and objective assessments techniques will be vital.
CONCLUSIONS
In this study, pharmacy students showed significant improvement in clinical skills performance of blood pressure assessment and knowledge of the pharmacotherapy of hypertension as demonstrated by test scores. This method of teaching resulted in high levels of student satisfaction as well as increased competence. Introducing “real-life” clinical scenarios early in the pharmacy curriculum using patient mannequins and SBL can lead to an improvement in overall patient care, which is our ultimate goal as pharmacists.
ACKNOWLEDGEMENTS
We would like to acknowledge the WISER Institute for the support and use of the patient simulators. We would also like to thank Teresa McKaveney for her editorial assistance.
Appendix 1. Blood Pressure Assessment Grading Rubric
REFERENCES
- 1.American Heart Association. Dallas, Tex: American Heart Association; 2005. Heart Disease and Stroke Statistics – 2006 Update. [Google Scholar]
- 2.Reid F, Murray P, Storrie M. Implementation of a pharmacist-led clinic for hypertensive patients in primary care-a pilot study. Pharm World Sci. 2005;27:202–7. doi: 10.1007/s11096-004-2563-y. [DOI] [PubMed] [Google Scholar]
- 3.Chabot I, Moisan J, Gregoire JP, Milot A. Pharmacist intervention program for control of hypertension. Ann Pharmacother. 2003;37:1186–93. doi: 10.1345/aph.1C267. [DOI] [PubMed] [Google Scholar]
- 4.Mangum SA, Kraenow KR, Narducci WA. Identifying at-risk patient through community pharmacy-based hypertension and stroke prevention screening projects. J Am Pharm Assoc. 2003;43:50–5. [PubMed] [Google Scholar]
- 5.Carter BL, Zillich AJ, Elliott WJ. How pharmacists can assist physicians with controlling blood pressure. J Clin Hypertens. 2003;5:31–7. doi: 10.1111/j.1524-6175.2003.01460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22:1533–40. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- 7.Borenstein Je, Graber G, Saltiel E, et al. Physician-pharmacist comanagement of hypertension: a randomized, comparative trial. Pharmacotherapy. 2003;23:109–16. doi: 10.1592/phco.23.2.209.32096. [DOI] [PubMed] [Google Scholar]
- 8.Cote I, Gregoire JP, Moisan J, Chabot I, Lacroix G. A pharmacy-based health promotion programme in hypertension. Pharmacoeconomic. 2003;21:415–28. doi: 10.2165/00019053-200321060-00005. [DOI] [PubMed] [Google Scholar]
- 9.Cote I, Moisan J, Gregoire JP. Health-related quality of life in hypertension: impact of a pharmacy intervention programme. J Clin Pharm Therap. 2005;30:355–62. doi: 10.1111/j.1365-2710.2005.00663.x. [DOI] [PubMed] [Google Scholar]
- 10.James D, Nastasic S, Horne R, Davies G. The design and evaluation of a simulated-patient teaching programme to develop the consultation skills of undergraduate pharmacy students. Pharm World Sci. 2001;23:212–6. doi: 10.1023/a:1014512323758. [DOI] [PubMed] [Google Scholar]
- 11.Ragucci KR, Fermo JD, Mazur JN. Objective structured clinical examinations for an ambulatory care pharmacy rotation. Am J Health-Syst Pharm. 2005;62:927–9. doi: 10.1093/ajhp/62.9.927. [DOI] [PubMed] [Google Scholar]
- 12.Yee B, Naik VN, Joo HS, et al. Nontechnical skills in anesthesia crisis management with repeated exposure to simulation-based education. Anesthesiology. 2005;103:241–8. doi: 10.1097/00000542-200508000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Berkenstadt H, Kantor GS, Yusim Y, et al. The feasibility of sharing simulation-based evaluation scenarios in anesthesiology. Anesth Analg. 2005;101:1068–74. doi: 10.1213/01.ane.0000168272.10598.51. [DOI] [PubMed] [Google Scholar]
- 14.Mueller MP, Christ T, Dobrev D, et al. Teaching antiarrhythmic therapy and ecg in simulator-based interdisciplinary undergraduate medical education. Br J Anaesth. 2005;95:300–4. doi: 10.1093/bja/aei174. [DOI] [PubMed] [Google Scholar]
- 15.Deering S, Brown J, Hodor J, Satin AJ. Simulation training and resident performance of singleton vaginal breech delivery. Obstet Gynecol. 2006;107:86–9. doi: 10.1097/01.AOG.0000192168.48738.77. [DOI] [PubMed] [Google Scholar]
- 16.Bond WF, Deitrick LM, Arnold DC, et al. Using simulation to instruct emergency medicine residents in cognitive forcing strategies. Acad Med. 2004;79:438–46. doi: 10.1097/00001888-200405000-00014. [DOI] [PubMed] [Google Scholar]
- 17.McLaughlin SA, Doezema D, Sklar DP. Human simulation in emergency medicine training: a model curriculum. Acad Emerg Med. 2002;9:1310–8. doi: 10.1111/j.1553-2712.2002.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 18.Rodgers PL, Jacob H, Rashwan AS, et al. Quantifying learning in medical students during a critical care medicine elective: a comparison of three evaluation instruments. Crit Care Med. 2001;29:1268–73. doi: 10.1097/00003246-200106000-00039. [DOI] [PubMed] [Google Scholar]
- 19.DeVita MA, Schaefer J, Lutz J, Wang H, Dongilli T. Improving medical emergency team (MET) performance using a novel curriculum and a computerized human patient simulator. Qual Saf Health Care. 2005;14:326–31. doi: 10.1136/qshc.2004.011148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blum RH, Raemer DB, Carroll JS, Dufresne RL, Cooper JB. A method for measuring the effectiveness of simulation-based team training for improving communication skills. Anesth Analg. 2005;100:1375–80. doi: 10.1213/01.ANE.0000148058.64834.80. [DOI] [PubMed] [Google Scholar]
- 21.Kyle RR, Via DK, Lowy RJ, et al. A multidisciplinary approach to teach responses to weapons of mass destruction and terrorism using combined simulation modalities. J Clin Anesth. 2004;16:152–8. doi: 10.1016/j.jclinane.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Fiedor ML. Pediatric simulation: a valuable tool for pediatric medical education. Crit Care Med. 2004;32:S72–S74. doi: 10.1097/01.ccm.0000110732.68981.52. [DOI] [PubMed] [Google Scholar]
- 23.Rhodes ML, Curran C. Use of the human patient simulator to teach clinical judment skills in a baccalaurate nursing program. Comput Informat Nurs. 2005;23:256–62. doi: 10.1097/00024665-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Henneman EA, Cunnigham H. Using clinical simulation to teach patient safety in an acute/critical care nursing course. Nurse Educator. 2005;30:172–7. doi: 10.1097/00006223-200507000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Federation for Medical Education. The Edinburgh Declaration. Ann Comm Educ. 1989;2:111–3. [Google Scholar]
- 27.Association of American Medical Colleges. Washington, D.C: Report on the General Professional Education of the Physician; 1984. Physicians for the twenty-first century. [Google Scholar]
- 28.Cohen L, Manion L, Morrison K. Research Methods in Education. 5th ed. London: RoutledgeFalmer; 2000. [Google Scholar]
- 29.Jamieson S. Likert scales: how to (ab)use them. Med Educ. 2004;38:1212–8. doi: 10.1111/j.1365-2929.2004.02012.x. [DOI] [PubMed] [Google Scholar]
- 30.Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34:151–7. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]