Abstract
PURPOSE:
To investigate possible adverse effects of a yellow-tinted intraocular lens (IOL) on scotopic sensitivity and hue discrimination.
SETTING:
Departments of Ophthalmology, Columbia University and New York University School of Medicine, New York, New York, USA.
METHODS:
Nine patients with a yellow-tinted IOL in 1 eye and a colorless ultraviolet IOL in the fellow eye and 9 young phakic subjects with and without a yellow-tinted clip-on lens were tested. Hue discrimination was measured with the Farnsworth-Munsell (FM) 100-hue test. Dark-adapted thresholds to 440 nm, 500 nm, and 650 nm light were measured at 23 locations using a modified Humphrey perimeter, and dark-adapted thresholds to white light were measured at 15 degrees temporal retina.
RESULTS:
In the 9 patients, there were no significant differences in dark-adapted sensitivities to 440, 500, 650 nm, or white light stimuli and no differences in FM 100-hue error scores between eyes with yellow-tinted IOLs and those with colorless IOLs. Similarly, in young phakic subjects, there were no significant differences in FM 100-hue error scores or dark-adapted sensitivity to the white light with and without the yellow-tinted clip-on lens. However, with the clip-on lens, mean sensitivities to the 440 nm, 500 nm, and 650 nm stimuli were significantly decreased by 2.7 to 2.8 dB, 0.7 to 1.0 dB, and 0 to 1.2 dB, respectively.
CONCLUSION:
Results suggest that implantation of a yellow-tinted IOL has a minimum to insignificant effect on scotopic sensitivity and hue discrimination.
The human crystalline lens blocks wavelengths of light below 400 nm and filters considerable amounts of visible short wavelength light.1 Moreover, the yellowing of the crystalline lens that occurs with age results in a progressive increase in absorbance within the short wavelength range of the visible spectrum.2-6 Conventional intraocular lenses (IOLs) that meet standards of practice block ultraviolet (UV) light but transmit approximately 90% of wavelengths above 400 nm. Recently, IOLs that not only block UV light but also attenuate short wavelength light were developed in an attempt to approximate the adult human crystalline lens. For example, the AcrySof Natural IOL (Alcon) contains 0.04% of a covalently bound yellow polymerizable chromophore that confers a yellow tint to the IOL. Nevertheless, compared to the transmission spectrum of the human crystalline lens, the decrease in transmission between 450 nm and 550 nm is considerably less than that in a 53-year-old person.7 Benefits conferred by IOLs that absorb blue light (short-wavelength light) include a reduction in the amount of high-energy short wavelength light that is transmitted to the retina and a reduction in chromatic aberration.8
Several recent studies report the effects of these IOLs on visual function. For example, Espindle et al.9 used the National Eye Institute Visual Functioning Questionnaire and the 12-Item Short Form Health Survey to assess changes in patient-reported quality of life as well as vision and health-related function after cataract extraction. The results in this study showed no significant differences in these measures between patients with a short-wavelength absorbing IOL (AcrySof Natural SN60AT) and those with a clear IOL (AcrySof SA60AT). Other studies report no significant differences in best corrected visual acuity (BCVA) or contrast sensitivity measured under photopic and mesopic conditions.10,11 Similarly, there are no differences in color vision evaluated with the Farnsworth-Munsell (FM) 100-hue test between patients with bilateral AcrySof Natural IOLs and patients with bilateral AcrySof UV-blocking IOLs and age-matched phakic control subjects.10,12 Retrospective and prospective case studies also show that with some exceptions,13 mixed pseudophakia (implantation of a colorless IOL in 1 eye and a yellow-tinted IOL in the other eye) is not problematic in terms of differences between the 2 eyes in color perception or contrast sensitivity.11,14
Despite these reports, questions have been raised regarding the possibility that short-wavelength absorbing IOLs may reduce visual performance at scotopic light levels.15-17 Scotopic or rod-system sensitivity depends on the number of photons absorbed by rhodopsin, a rod photopigment. The probability of absorption is wavelength dependent and maximum at approximately 507 nm. In addition, it is reported that scotopic or rod-system sensitivity decreases with age.18,19 Older adults with healthy retinas exhibit, on average, a 1 log unit elevation in absolute threshold under dark-adapted conditions.19 Most of the increase in threshold or decrease in sensitivity can be attributed to increased lens density and pupillary miosis,18 age-related loss of rod photoreceptor cells,20 and slower photopigment regeneration.19
These findings stress the importance of investigating the possible adverse effects of short-wavelength absorbing filtering IOLs on scotopic sensitivity. Previous studies17,21 evaluated the effects of IOL implantation on scotopic vision using scotopic luminous efficiency curves published by the Comission Internationale de l'Eclairage rather than using direct measurement. Thus, we compared hue discrimination and scotopic sensitivity in patients with an AcrySof Natural IOL in 1 eye and an AcrySof UV-light absorbing IOL in the fellow eye. We also measured hue discrimination and scotopic sensitivity in a group of healthy young individuals in the presence and absence of a clip-on yellow lens (Alcon Laboratories) composed of the same material and chromophore as the AcrySof Natural IOL.
SUBJECTS AND METHODS
Nine patients who had implantation of the single-piece AcrySof Natural piece SN60AT IOL in 1 eye and the single-piece AcrySof SA60AT IOL in the fellow eye were recruited for the study after cataract extraction by 1 surgeon (R.E.B.). The patients were tested 9 to 24 months (mean and median 16 months) after IOL implantation. Patients were excluded if they had ocular or systemic disease other than cataract. Cataract extraction was performed using topical anesthesia and a clear corneal incision of approximately 3.0 mm. Surgery included capsulorhexis and phacoemulsification. The posterior capsule was left intact. The IOL was folded and passed through the microincision, where it was implanted in the capsular bag.
In addition to the patient group, 9 young phakic subjects were recruited for the study. Inclusion criteria included no evidence of ocular or systemic disease that might affect the visual system.
Informed consent was obtained from all patients and subjects before their participation. Procedures adhered to the tenets of the Declaration of Helsinki, and the protocol was approved by the Columbia University Medical Center Institutional Review Board for Human Research.
Hue Discrimination
Hue discrimination was evaluated monocularly using the FM 100-hue test under standard illuminance conditions. The eyes of the patients were tested individually; in the young phakic subjects, the right eye or the eye with the greater visual acuity was tested. All phakic subjects were tested with and without a yellow-filter clip-on lens using a counterbalanced design. In both groups, the nontested eye was occluded and subjects were corrected for the viewing distance of 0.5 m. Error scores and significant axes were calculated using the Kinnear method.
Dark-Adapted Spectral Sensitivity
After pupil dilation (tropicamide 1%, phenylephrine 2.5%) and 40 minutes of dark adaptation, thresholds to Goldmann V stimuli 200 msec in duration were measured monocularly using a modified Humphrey Field Analyzer (model 620) as detailed by Jacobson et al.22 Dark-adapted thresholds to 440 nm (8.7 nm half bandwidth), 500 nm (7.3 nm half bandwidth), and 650 nm (10.9 nm half bandwidth) stimuli were measured at 23 test locations with eccentricities at 4 degrees, 12 degrees, and 24 degrees using the full-threshold technique. In addition to obtaining thresholds to the 3 narrow-band stimuli at 23 test locations, thresholds to white-light stimuli (1 degree in diameter, 1 second in duration) were measured with a Goldmann Weekers adaptometer at 15 degrees temporal retina using an ascending method of limits procedure. A counterbalanced design was used to determine the test order of the eye for the patients and use of a clip-on lens for the phakic subjects.
RESULTS
Demographics
Patients
The mean age of the patients was 63.3 years ± 20 (SD). The youngest was 16 years and the oldest, 79 years. Two were 74 years old; the ages of the other 5 were 46, 67, 70, 71, and 73 years. Refractive errors before surgery ranged from 0 to ±7.00 diopters (D). In all eyes, the BCVA was 20/30 or greater; there was no significant difference in visual acuity between the eyes.
Young Phakic Subjects
The mean age of the 3 men and 6 women in the young phakic subject group was 24.5 ± 1.4 years (range 22 to 27 years). Refractive errors ranged from 0 to 4.75 D, and BCVA was ≥20/20.
Complications
One patient developed posterior capsule opacification (PCO) in both eyes after surgery. The patient was treated with a neodymium:YAG laser capsulotomy, and visual acuity after treatment was 20/30 in each eye
Hue Discrimination
Figure 1 shows polar plots of typical examples of FM 100-hue results in a patient and in a young phakic subject. The plot for the eye of a patient with the AcrySof Natural SN60AT IOL (Figure 1, A) shows an error score of 56 with no suggested axis, and the plot for the other eye with the AcrySof SA60AT IOL (Figure 1, B) shows an error score of 52 with no suggested axis. The polar plots for the right eye of a young phakic subject with the yellow clip-on lens (Figure 1, C) and without the yellow clip-on lens (Figure 1, D) show error scores of 20 and 16, respectively, with no suggested axes. Table 1 shows the FM-100 hue error scores in all 9 patients and in the 9 phakic subjects. In the patients, the Wilcoxon matched pairs test showed no significant differences in error scores between the eye with the AcrySof Natural SN60AT IOL and the eye with the AcrySof SA60AT IOL. Two eyes with an AcrySof Natural IOL and 1 with an AcrySof IOL had evidence of a tritan axis (Table 1). Similarly, there were no significant differences in error scores in the phakic subjects with and without the yellow-tinted clip-on lens. One subject had a tritan axis that was present with and without the yellow-tinted clip-on.
Figure 1.
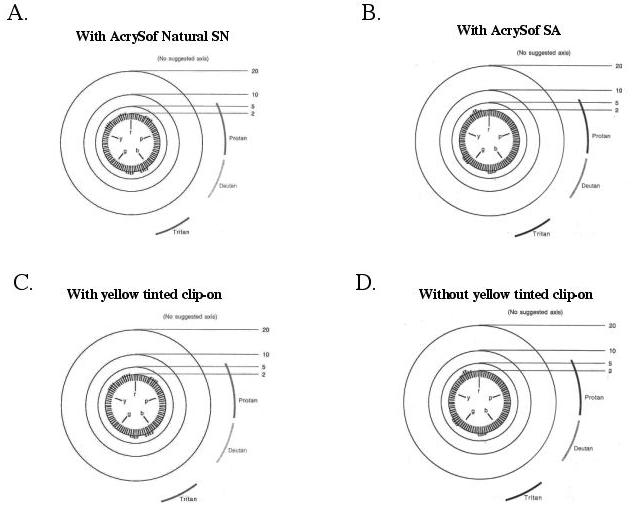
Examples of FM 100-hue polar plots obtained from a patient and from a young phakic subject. A: The polar plot for the eye of a patient with the AcrySof Natural IOL. B: The polar plot for the fellow eye with the AcrySof IOL. C and D: The polar plots for the right eye of a young phakic subject with (C) and without (D) the yellow clip-on lens.
Table 1.
Farnsworth-Munsell 100-hue error scores.
| Patients |
Young Phakic Subjects |
|||
|---|---|---|---|---|
| Patient or Subject No. |
SN60AT IOL |
SA60AT IOL |
With Clip-On | Without Clip-On |
| 1 | 88 | 36† | 20 | 16 |
| 2 | 132* | 140 | 52 | 84 |
| 3 | 52 | 40 | 108* | 64* |
| 4 | 36 | 64 | 32 | 12 |
| 5 | 96* | 104 | 48 | 100 |
| 6 | 24 | 56 | 36 | 36 |
| 7 | 180 | 104† | 20 | 20 |
| 8 | 152† | 100* | 20 | 28 |
| 9 | 56 | 52 | 36 | 28 |
| Mean | 90.7 | 77.3 | 41.3 | 43.1 |
Slight tritan axis
Slight protan axis
Dark-Adapted Spectral Sensitivity
Patients
Figure 2 shows an example of dark-adapted sensitivities for a 500 nm light obtained from the eye of a patient with the AcrySof Natural IOL on the modified Humphrey Field Analyzer. The figure shows the values in decibels for each of the 23 locations tested. The values in parentheses are repeat measurements. Dark-adapted sensitivity values were similar in all 9 patients. The values in the youngest patient and in the patient who had a history of PCO fell well within the range of values in the group. Figure 3, A, shows the sensitivity differences between the eye with the AcrySof Natural IOL and the eye with the AcrySof IOL for the 3 narrow-band test wavelengths and for the white-light stimuli in each of the 9 patients. To better compare the modified Humphrey Field Analyzer results with those obtained on the Goldmann Weekers adaptometer at 15 degrees temporal retina, the data obtained at the 7 locations at an eccentricity of 12 degrees were averaged for each patient and sensitivity differences to the 440 nm, 500 nm, 650 nm stimuli calculated (Figure 3, A). Data points above the horizontal line indicate sensitivity is greater with the AcrySof Natural IOL, and data points below the line indicate sensitivity is greater with the AcrySof IOL. In the case of the 440 nm stimulus, sensitivity was greater in the eye with the AcrySof Natural IOL in 3 patients, and in the eye with the AcrySof IOL in 5 patients. For the 500 stimulus, sensitivity was greater in 3 patients with the AcrySof Natural IOL and in 5 patients with the AcrySof IOL. For the 650 nm stimulus, it was greater in 2 patients with the AcrySof Natural IOL and in 5 with the AcrySof IOL. For the white-light stimulus, sensitivity was greater in 7 patients with the AcrySof IOL.
Figure 2.
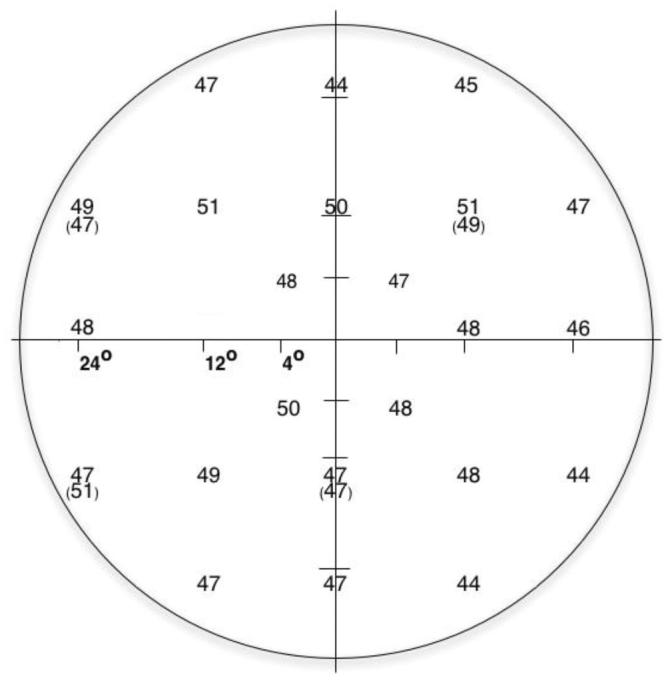
An example of dark-adapted sensitivity values to the 500 nm test light in 1 of the 9 patients on the modified Humphrey Field Analyzer.
Figure 3.
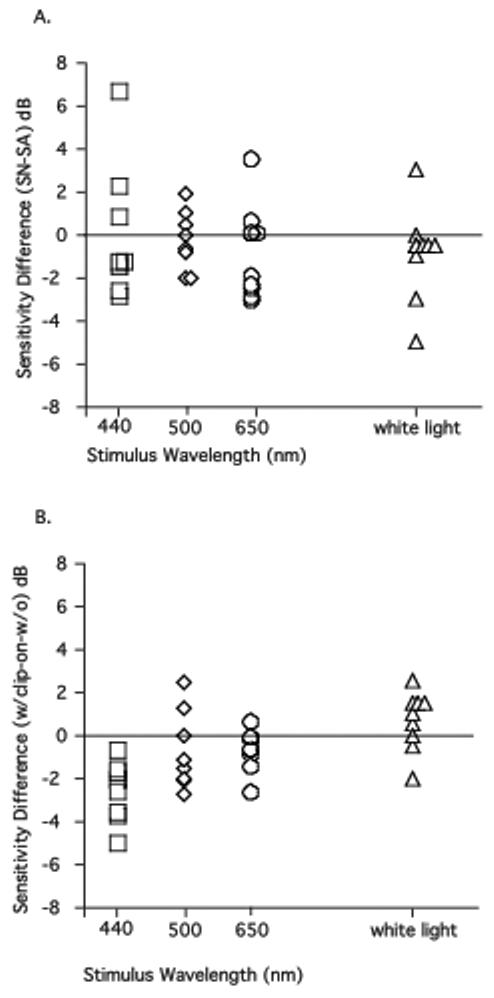
A: Mean differences in dark-adapted sensitivities in the 9 patients between eyes with the AcrySof Natural SN60AT IOL and fellow eyes with the AcrySof SA60AT IOL to 440 nm (squares), 500 nm (diamonds), 650 nm (circles) stimuli presented at an eccentricity of 12 degrees and to the white-light stimulus at 15 degrees (triangles). B: Mean differences in dark-adapted sensitivities with and without the yellow-tinted clip-on lens in the 9 young phakic subjects to 440 nm (squares), 500 nm (diamonds), 650 nm (circles) stimuli at an eccentricity of 12 degrees and to the white-light stimulus at 15 degrees (triangles).
Because of an effect of eccentricity on sensitivity (P<.001), data were analyzed separately for 4 degrees, 12 degrees, and 24 degrees. Mean sensitivities for the 440 nm stimulus were decreased with the AcrySof Natural IOL compared with the AcrySof IOL by mean values of 0.2 dB, 0.5 dB, and 0.1 dB (ie, 0.02 log unit, 0.05 log unit, and 0.01 log unit, respectively) at 4 degrees, 12 degrees, and 24 degrees. They were decreased for the 500 nm stimulus by 0.5 dB, 0.4 dB, and 0.2 dB (0.05 log unit, 0.04 log unit, and 0.02 log unit, respectively) at the 3 eccentricities and for the 650 nm stimulus by 0.7 dB, 0.9 dB, and 0.6 dB. A 2-way repeated-measures analysis of variance (ANOVA) of these data indicated that although test wavelength and IOL had significant effects on sensitivity values, there were no significant interactions between test wavelength and IOL. The differences in sensitivities were not significant at any eccentricity. Sensitivities to white light at 15 degrees temporal retina were decreased by a mean of 0.9 dB (0.09 log unit). A paired-comparison t test showed no significant difference between the 2 IOLs in the white-light stimulus at 15 degrees temporal retina.
Young Phakic Subjects
Figure 3, B, shows the difference in dark-adapted sensitivity values with and without the yellow clip-on lens in the 9 young phakic subjects. As in Figure 3, A, the sensitivity differences to the 440 nm, 500 nm, 650 nm stimuli are shown for locations at an eccentricity of 12 degrees. Sensitivity was decreased by the yellow clip-on lens for the 440 nm stimulus in all 9 subjects, for the 500 nm stimulus in 5 subjects, and for the 650 nm stimulus in 4 subjects. Sensitivity to white light was increased by the yellow clip-on in 6 subjects.
Mean sensitivities were decreased to the 440 nm stimulus with the yellow clip-on lens by 2.8 dB, 2.7 dB, and 2.7 dB (0.28 log unit, 0.27 log unit, and 0.27 log unit, respectively) at retinal eccentricities of 4 degrees, 12 degrees, and 24 degrees. However, sensitivities to the 500 nm stimulus were only decreased by 0.7 dB, 1.0 dB, and 0.9 dB (0.07 log unit, 0.1 log unit, and 0.09 log unit, respectively) and to 650 nm by 0 dB, 0.7 dB, and 1.2 dB. A 2-way repeated-measures ANOVA indicated that test wavelength and the yellow clip-on lens had significant effects on sensitivity values. There were also significant interactions between test wavelength and the IOL, and post-hoc Tukey tests showed significant differences (P≤.05) in sensitivity values at 4 degrees, 12 degrees, and 24 degrees for the 3 wavelengths. Sensitivities to white light were increased by the yellow clip-on by a mean value of 0.67 dB (0.07 log unit). A paired-comparison t test showed no significant difference with or without the clip-on lens to the white-light stimulus at 15 degrees temporal retina.
DISCUSSION
We investigated the possible adverse effects of the AcrySof Natural IOL on scotopic sensitivity and color vision in a group of patients with mixed pseudophakia. We also studies the effects of a clip-on yellow-lens composed of the same material and chromophore as the AcrySof Natural IOL on scotopic sensitivity and color vision in a group of young phakic subjects. We found no significant differences in dark-adapted sensitivities to 440 nm, 500 nm, and 650 nm or to white-light stimuli and no differences in FM 100-hue error scores between the 2 eyes of the patients with mixed pseudophakia. In the group of young phakic subjects, the yellow-tinted clip-on lens did not affect hue discrimination; there were no significant differences in error scores. The FM 100-hue results in both groups are in agreement with those in previous studies that found no differences between patients with bilateral AcrySof Natural IOLs and those with bilateral AcrySof UV-blocking IOLs and age-matched phakic controls.10,12
With regard to the dark-adapted spectral sensitivity findings, sensitivities to the 440 nm, 500 nm, and 650 nm lights were significantly decreased in the young phakic subjects with the yellow-tinted lens. The patients, however, showed no significant differences in sensitivities between the 2 IOLs. The results in the young phakic subjects are consistent with the predicted scotopic spectral sensitivity functions in observers with a yellow-tinted IOL.21 As expected, we found that sensitivities to the 500 nm and 650 nm were only minimally decreased by the yellow tinted clip-on lens in the young phakic subjects. These results suggest that visual performance under scotopic conditions and color perception will not be impaired after implantation of an AcrySof Natural IOL. This conclusion is relevant given the possible benefits conferred by a short-wavelength filtering IOL.
Some studies show an association between cataract surgery and age-related macular degeneration (ARMD). For instance, Pollack et al.23 report that the rate of progression from dry to wet ARMD was more than 4 times greater in the first year after cataract surgery in patients older than 65 years. The Beaver Dam Eye Study24 reported an increased risk for progression of ARMD and incidence of late ARMD, defined as exudative macular degeneration or pure geographic atrophy. Wang et al.25 pooled data from the Beaver Dam and Blue Mountain Eye studies to obtain a combined cohort of more than 6000 patients followed over a 5-year period and concluded that the 5-year risk for developing late-stage ARMD after cataract surgery was 2 to 5 times the risk in phakic subjects of similar age, sex, and smoking behavior. Although the reasons for these associations are not understood, the role of exposure to short-wavelength or blue light has been given consideration.
Given the possibility of increased risks for development of ARMD after cataract extraction and the possible benefits of implanting a short-wavelength filtering IOL, we suggest the benefits outweigh any minimum to insignificant effects the IOL may have on dark-adapted spectral sensitivity and hue discrimination.
Footnotes
No author has a financial or proprietary interest in any material or method mentioned.
Presented at the annual meetings of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, USA, May 2005 and April–May 2006.
Supported by grants from Alcon Laboratories, Fort Worth, Texas, and the National Eye Institute (EY 12951, EY 02115), Bethesda, Maryland, and by unrestricted funds from Research to Prevent Blindness, New York, New York, USA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Boettner EA, Wolter JR. Transmission of the ocular media. Invest Ophthalmol. 1962;1:776–783. [Google Scholar]
- 2.Lindstrom RL, Doddi N. Ultraviolet light absorption in intraocular lenses. J Cataract Refract Surg. 1986;12:285–289. doi: 10.1016/s0886-3350(86)80011-6. [DOI] [PubMed] [Google Scholar]
- 3.Weale RA. Aging and vision. Vision Res. 1986;26:1507–1512. doi: 10.1016/0042-6989(86)90170-7. [DOI] [PubMed] [Google Scholar]
- 4.Weale RA. Age and the transmittance of the human crystalline lens. J Physiol. 1988;395:577–587. doi: 10.1113/jphysiol.1988.sp016935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaillard ER, Zheng L, Merriam JC, Dillon J. Age-related changes in the absorption characteristics of the primate lens. Invest Ophthalmol Vis Sci. 2000;41:1454–1459. [PubMed] [Google Scholar]
- 6.Mellerio J. Yellowing of the human lens: nuclear and cortical contributions. Vision Res. 1987;27:1581–1587. doi: 10.1016/0042-6989(87)90166-0. [DOI] [PubMed] [Google Scholar]
- 7.Ernest PH. Light-transmission-spectrum comparison of foldable intraocular lenses. J Cataract Refract Surg. 2004;30:1755–1758. doi: 10.1016/j.jcrs.2003.12.054. [DOI] [PubMed] [Google Scholar]
- 8.Schwiegerling J. Blue-light-absorbing lenses and their effect on scotopic vision. J Cataract Refract Surg. 2006;32:141–144. doi: 10.1016/j.jcrs.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Espindle D, Crawford B, Maxwell A, et al. Quality-of-life improvements in cataract patients with bilateral blue light-filtering intraocular lenses: clinical trial. J Cataract Refract Surg. 2005;31:1952–1959. doi: 10.1016/j.jcrs.2005.03.060. [DOI] [PubMed] [Google Scholar]
- 10.Marshall J, Cionni RJ, Davison J, et al. Clinical results of the blue-light filtering AcrySof Natural foldable acrylic intraocular lens. J Cataract Refract Surg. 2005;31:2319–2323. doi: 10.1016/j.jcrs.2004.11.061. [DOI] [PubMed] [Google Scholar]
- 11.Rodríguez-Galietero A, Montés-Micó R, Muñoz G, Albarrán-Diego C. Comparison of contrast sensitivity and color discrimination after clear and yellow intraocular lens implantation. J Cataract Refract Surg. 2005;31:1736–1740. doi: 10.1016/j.jcrs.2005.02.039. [DOI] [PubMed] [Google Scholar]
- 12.Cionni RJ, Tsai JH. Color perception with AcrySof Natural and AcrySof single-piece intraocular lenses under photopic and mesopic conditions. J Cataract Refract Surg. 2006;32:236–242. doi: 10.1016/j.jcrs.2005.12.129. [DOI] [PubMed] [Google Scholar]
- 13.Shah SA, Miller KM. Explantation of an AcrySof Natural intraocular lens because of a color vision disturbance. Am J Ophthalmol. 2005;140:941–942. doi: 10.1016/j.ajo.2005.05.043. [DOI] [PubMed] [Google Scholar]
- 14.Olson MD, Miller KM. Implanting a clear intraocular lens in one eye and a yellow lens in the other eye: a case series. Am J Ophthalmol. 2006;141:957–958. doi: 10.1016/j.ajo.2005.11.051. [DOI] [PubMed] [Google Scholar]
- 15.Mainster MA. Violet and blue light blocking intraocular lenses: photoprotection versus photoreception [perspective] Br J Ophthalmol. 2006;90:784–792. doi: 10.1136/bjo.2005.086553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mainster MA. Intraocular lenses should block UV radiation and violet but not blue light. Arch Ophthalmol. 2005;123:550–555. doi: 10.1001/archopht.123.4.550. [DOI] [PubMed] [Google Scholar]
- 17.Mainster MA, Sparrow JR. How much blue light should an IOL transmit? [perspective] Br J Ophthalmol. 2003;87:1523–1529. doi: 10.1136/bjo.87.12.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson GR, Owsley C. Scotopic sensitivity during adulthood. Vision Res. 2000;40:2467–2473. doi: 10.1016/s0042-6989(00)00108-5. [DOI] [PubMed] [Google Scholar]
- 19.Jackson GR, Owsley C, McGwin GJ. Aging and dark adaptation. Vision Res. 1999;39:3975–3982. doi: 10.1016/s0042-6989(99)00092-9. [DOI] [PubMed] [Google Scholar]
- 20.Curcio CA, Owsley C, Jackson GR. Spare the rods, save the cones in aging and age-related maculopathy. Invest Ophthalmol Vis Sci. 2000;41:2015–2018. [PubMed] [Google Scholar]
- 21.Werner JS. Night vision in the elderly: consequences for seeing through a “blue filtering” intraocular lens. Br J Ophthalmol. 2005;89:1518–1521. doi: 10.1136/bjo.2005.073734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobson SG, Voigt WJ, Parel JM, et al. Automated light- and dark-adapted perimetry for evaluating retinitis pigmentosa. Ophthalmology. 1986;93:1604–1611. doi: 10.1016/s0161-6420(86)33522-x. [DOI] [PubMed] [Google Scholar]
- 23.Pollack A, Marcovich A, Bukelman A, Oliver M. Age-related macular degeneration after extracapsular cataract extraction with intraocular lens implantation. Ophthalmology. 1996;103:1546–1554. doi: 10.1016/s0161-6420(96)30464-8. [DOI] [PubMed] [Google Scholar]
- 24.Klein R, Klein BEK, Wong TY, et al. The association of cataract and cataract surgery with the long-term incidence of age-related maculopathy. Arch Ophthalmol. 2002;120:1551–1558. doi: 10.1001/archopht.120.11.1551. [DOI] [PubMed] [Google Scholar]
- 25.Wang JJ, Klein R, Smith W, et al. Cataract surgery and the 5-year incidence of late-stage age-related maculopathy; pooled findings from the Beaver Dam and Blue Mountains Eye Studies. Ophthalmology. 2003;110:1960–1967. doi: 10.1016/s0161-6420(03)00816-9. [DOI] [PubMed] [Google Scholar]


