Abstract
Background
Since the introduction of the sentinel lymph node (SLN) biopsy in breast cancer patients there is a renewed interest in lymphatic drainage to the internal mammary (IM) chain nodes. We evaluated the frequency of lymphatic drainage to the IM chain, the rate of SLNs that contain metastases and the clinical implications of IM LN metastases.
Methods
Between June 1999 and April 2005 506 consecutive patients underwent SLN biopsy as a staging procedure for clinically T1-2N0 breast cancer. In all patients preoperative lymphoscintigraphy was combined with the intraoperative use of a gammaprobe. In patients with IM SLNs visualized on lymphoscintigraphy, LNs were extirpated through an intercostal parasternal incision.
Results
SLNs were visualized by preoperative lymphoscintigraphy in 99% of all patients (502/506): axillary SLNs in 499 patients (99%), ipsilateral IM LNs in 109 patients (22%). In 85 patients with visualized IM SLNs the IM nodes could be removed (78%). In 20 of the latter 85 patients IM SLNs contained metastases (24%). IM metastases were associated with axillary LN metastases (P < 0.001). In 17 patients IM metastases led to extension of the radiotherapy field, while additional (adjuvant) systemic therapy was given in six patients.
Conclusion
SLNs in the IM chain are common in breast cancer patients and can be extirpated in the majority of these patients. The proportion of patients in whom radiotherapeutic treatment was adjusted due to IM LN metastases was substantial. We advocate retrieval of IM SLNs when visualized by preoperative lymphoscintigraphy.
Keywords: Internal mammary lymph nodes, Breast cancer, Sentinel node, Metastasis
The internal mammary (IM) chain is well known as a site of metastases in patients with breast cancer. The presence of IM lymph node (LN) metastases is a poor prognostic sign as reflected by the UICC-TNM staging system that classifies IM LN metastases as stage N3.1 In earlier times dissection of the IM LNs, as part of an extended mastectomy with IM node dissection, was advocated by some authors but randomized trials failed to show any beneficial effect of the procedure that was accompanied by significant morbidity.2–4 Since then, interest in the IM LN chain has waned.
Since the introduction of the sentinel lymph node (SLN) biopsy in breast cancer patients there has been a renewed interest in the IM LNs. Drainage to this basin is frequently seen on preoperative lymphoscintigraphy, while the localization of the primary tumor and the nanocolloid injection technique appear to influence the frequency of visualized IM nodes.5–7 Various authors advocate removal of these IM SLNs,8,9 but the clinical implications of IM LN biopsy are still unclear.
In this study we evaluated the frequency of lymphatic drainage to the IM chain, the rate of metastases in the IM SLN and the clinical implications of IM LN metastases.
PATIENTS AND METHODS
Between June 1999 and April 2005, 523 consecutive patients underwent surgical treatment including SLN biopsy as a staging procedure for clinically stage T1-2N0 breast cancer. Data regarding all procedures were collected prospectively in a database of the nuclear medicine department.
A diagnosis of invasive breast cancer was established preoperatively by fine-needle aspiration or image-guided large core needle biopsy. Sixteen patients who underwent SLN biopsy as a secondary operative procedure following previous excisional biopsy of the primary tumor and one patient who eventually turned out to have multicentric breast cancer were excluded from the study.
The study cohort consisted of 506 patients. At the time of the introduction of the sentinel node procedure the ethical committee of the hospital approved the routine use of the SLN biopsy as a staging procedure. All patients received written information regarding the SLN procedure and the possibility of SLNs in the IM chain. The unknown clinical implications of surgically removing IM LNs were discussed with the patients.
On the day of the operation, all patients received a combination of peritumoral intraparenchymal and subcutaneous injections of an average of 77.7 MBq (53–150 MBq) of 99mTc nanocolloid in a total volume of 0.6 ml of physiologic saline, given in two to three equal doses. In case of a nonpalpable breast tumor the tracer was injected around the tumor using a 7.5-MHz ultrasound probe (Aloka). After injection the area was massaged until the appearance of the SLN. Continuous visualization was done and imaging started as soon as lymphatic drainage was visualized on the persistence scope and at 2–3 h after injection in both the anterior and lateral direction. Images were obtained during a 2-min imaging time on the Toshiba 901 HG single-head gamma camera, using low-energy high-resolution collimators. A skin marker was placed on the projection of the SN using a handheld γ-ray detection probe (Europrobe, PI Medical diagnostic equipment BV).
The operative procedure was carried out in the afternoon of the same day of the 99mTc nanocolloid injection. A γ-ray detection probe and a peritumoral injection of patent blue dye (Bleu patenté V, Laboratoire Guerbet, Aulnay-sous-Bois, France) were intraoperatively used for SLN identification. During the operation axillary sentinel nodes were retrieved first and frozen section analysis was done to enable axillary dissection during the same operative procedure in case of LN metastases. When no axillary SLN was visualized on preoperative lymphoscintigraphy, the axilla was nonetheless explored in search for a blue dye containing SLN. When no axillary SLN was identified by either means, axillary LN dissection was performed. Following retrieval of axillary SLNs, surgical exploration for IM SLNs was done. When an IM SLN was visualized on preoperative lymphoscintigraphy, the γ-ray detection probe was used to guide a parasternal intercostal incision through the best-suited intercostal space to harvest the visualized node. A partial rib resection was not routinely done for sentinel IM nodes that were localized behind the ribs.
In addition to frozen section analysis of the axillary SLNs, all collected SLNs were formalin-fixed, paraffin embedded and cut at five levels of 250 μm. Pathological evaluation followed hematoxylin-eosin and immunohistochemical cytokeratin-8 staining. The presence of axillary and IM LN metastases was classified according to the 2002 version of the UICC-TNM-classification.1
To assess the additional operative time of IM SLN biopsy we compared the time between incision and skin closure needed for lumpectomy and mastectomy with and without IM SLN biopsy. We selected four groups of ten patients: those who underwent lumpectomy with or without IM SLN biopsy and those who had had mastectomy with or without IM SLN biopsy. In all patients the operative procedure had started with axillary SLN biopsy. We only evaluated patients who did not have axillary dissection to avoid the potential bias of extra time awaiting the result of frozen section analysis. For each category we selected the last ten patients to avoid the learning curve effect.
To evaluate the impact of IM LN metastases on subsequent systemic treatment we assessed the proposed adjuvant treatment strategy in the absence and presence of metastases in these nodes, applying the Dutch national guidelines for treatment of breast cancer (version 2005, http//www.oncoline.nl, summarized in Table 1). Locoregional radiotherapy, comprising the affected breast and/or thoracic wall, and the ipsilateral axillary, periclavicular and parasternal fields was indicated in patients with four or more metastatic axillary LNs. In patients with IM LN metastases with 0–3 tumor-positive axillary LNs a parasternal irradiation was given: in combination with irradiation of the breast in patients who had breast-conserving therapy or as parasternal radiotherapy following mastectomy.
TABLE 1.
Indications for adjuvant chemo- and hormonal systemic therapy according to the Dutch national guidelines 2005
| Axillary lymph node metastases | |
|---|---|
| Primary tumor characteristics | |
| Tumor >3 cm | |
| Tumor >2 cm and BR grade II | |
| Tumor >1 cm and BR grade III | |
| Other conditions | |
| Age | <35 years: always systemic therapy 60-69 years: chemotherapy when ER- or ≥4 axillary lymph node metastases ≥70 years: no chemotherapy |
| ER status | Hormonal therapy for the aforementioned indications at all ages if the tumor is ER receptor positive. |
BR, Bloom-Richardson; ER, estrogen receptor.
Chi-square analysis was performed to evaluate differences in IM SLN visualization rates between groups of patients with various clinicopathological variables and to explore the relation between IM and axillary LN metastases. The ANOVA test was used to explore the relation between age and the visualization of IM SLNs, as well as for the analysis of operative time differences.
RESULTS
The median age of the 506 patients was 60 years (range 24–92 years) and there were three male patients (0.8%). The distribution of primary tumor characteristics is summarized in Table 2.
TABLE 2.
Comparison of characteristics of patients who had visualized internal mammary sentinel lymph nodes (IM SLNs) versus those who had not visualized IM SLNs on preoperative lymphoscintigraphy
| All patients | IM SLN visualized | IM SLN not visualized | P | ||||
|---|---|---|---|---|---|---|---|
| n = 506 | n = 109 | n = 397 | |||||
| Median age (years) | 60 (range 24–92) | 57 (range 30–91) | 61 (range 24–92) | 0.016* | |||
| Gender | 0.36 | ||||||
| Male | 3 | (0.6) | 0 | (0) | 3 | (0.8) | |
| Female | 503 | (99.4) | 109 | (100) | 394 | (99.2) | |
| T-stage | 0.47 | ||||||
| T1 | 316 | (62.5) | 73 | (67.0) | 243 | (61.2) | |
| T2 | 184 | (36.4) | 36 | (33.0) | 148 | (37.3) | |
| T3 | 4 | (0.8) | 0 | (0) | 4 | (1.0) | |
| Tx | 2 | (0.4) | 0 | (0) | 2 | (0.5) | |
| Tumor localization | <0.001 | ||||||
| Cranial | 47 | (9.3) | 11 | (10.1) | 36 | (9.1) | |
| Craniolateral | 230 | (45.5) | 30 | (27.5) | 200 | (50.4) | |
| Lateral | 25 | (4.9) | 2 | (1.8) | 23 | (5.8) | |
| Caudolateral | 40 | (7.9) | 10 | (9.2) | 30 | (7.6) | |
| Caudal | 18 | (3.6) | 1 | (3.6) | 17 | (4.3) | |
| Caudomedial | 30 | (5.9) | 13 | (11.9) | 17 | (4.3) | |
| Medial | 11 | (2.2) | 4 | (3.7) | 7 | (1.8) | |
| Craniomedial | 80 | (15.8) | 34 | (31.2) | 46 | (11.6) | |
| Central | 25 | (4.9) | 4 | (3.7) | 21 | (5.3) | |
| Malignancy grade | 0.63 | ||||||
| BRI | 206 | (40.7) | 48 | (44.0) | 158 | (39.8) | |
| BRII | 196 | (38.7) | 38 | (34.9) | 158 | (39.8) | |
| BRIII | 104 | (20.6) | 23 | (21.1) | 81 | (20.4) | |
| Estrogen receptor status | 0.24 | ||||||
| Positive | 427 | (84.4) | 88 | (80.7) | 339 | (85.4) | |
| Negative | 79 | (15.6) | 21 | (19.3) | 58 | (14.6) | |
| Axillary lymph node involvement | 0.58 | ||||||
| No axillary metastases | 296 | (58.5) | 68 | (62.4) | 228 | (57.4) | |
| 1–3 lymph node metastases | 174 | (34.4) | 35 | (32.1) | 139 | (35.0) | |
| *4 lymph node metastases | 36 | (7.1) | 6 | (5.5) | 30 | (7.6) | |
Values in parentheses are percentages.
BR, Bloom-Richardson grade.
* Age difference between the groups was compared by ANOVA.
Visualization and Retrieval of Sentinel Lymph Nodes in the IM Chain (Fig. 1)
FIG. 1.
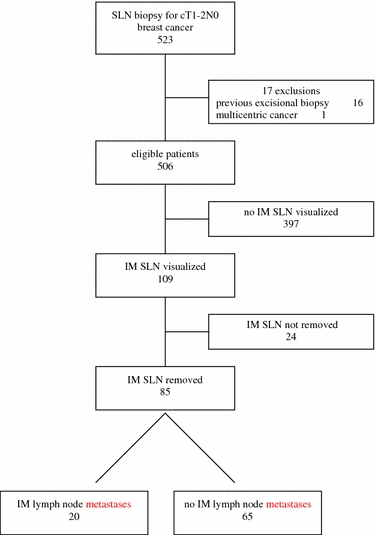
Summary of search for internal mammary sentinel lymph nodes (IM SLNs).
SLNs were visualized on preoperative lymphoscintigraphy in 502 of the 506 patients (99%). Axillary SLNs were visualized in 499 of 502 patients (99%), while one or more IM SLNs were found in 109 patients (22%). Three of the 109 patients with visualized IM SLNs had IM sentinel nodes only (3%); in one of these latter patients, an axillary SN was removed following patent blue dye injection and axillary exploration. Location of the tumor in the craniomedial and caudomedial aspect of the breast was associated with drainage to the IM nodes (P < 0.001), and patients with visualized internal mammary nodes were younger (Table 2).
IM SLNs could be retrieved through a parasternal intercostal incision in 85 of the 109 patients (78%). Parasternal exploration for IM SLNs added 16 min to the mean operative time in patients who underwent breast conservative therapy (P = 0.02). For patients who underwent mastectomy the operative time was not significantly prolonged (Table 3). Complications (pleural breeching, internal mammary vessel damage) of the intercostal surgical exploration were rare; in particular there were no pneumothoraxes or bleeding complications necessitating drainage or reoperation (Table 4).
TABLE 3.
Operative time of surgical exploration for internal mammary sentinel lymph nodes (IM SLNs) (n = 40)
| Mean operative time in minutes (range) | P | ||
|---|---|---|---|
| Axillary SLN biopsy/lumpectomy/IM SLN biopsy | 60 | (27–76) | 0.02 |
| Axillary SLN biopsy/lumpectomy/no IM SLN biopsy | 44 | (32–83) | |
| Axillary SLN biopsy/mastectomy/IM SLN biopsy | 72 | (42–104) | 0.8 |
| Axillary SLN biopsy/mastecomy/no IM SLN biopsy | 69 | (30–100) |
TABLE 4.
Complications of surgical exploration for internal mammary sentinel lymph nodes (IM SLNs) (n = 109)
| n | ||
|---|---|---|
| Intraoperative complications | ||
| Pleural breeching | 4 | (4) |
| Internal mammary vessel damage | 6 | (6) |
| Postoperative complications | ||
| Pneumothorax | − | |
| Bleeding necessitating reoperation | − | |
Values in parentheses are percentages.
IM LN Metastases
Metastases in the IM SLN were observed in 20 of the 85 patients who underwent successful IM SLN exploration (24%), and 42% of the patients with axillary SLNs (210/499). There was a correlation between IM metastases and axillary metastases (P = 0.002). In 16 of the 20 patients with IM LN metastases, the axillary SLN contained metastases too (80%). Conversely, IM metastases were found in 1% of patients without axillary metastases (4/297), in 7% of patients with 1–3 axillary metastases (13/174) and in 8 % of patients with ≥4 axillary metastases (3/36).
Clinical Implications of Metastases in the IM SLN (Table 5)
TABLE 5.
Clinical postsurgical implications of internal mammary lymph nodes IM LN metastases (n = 20)
| No. | Tumor characteristics | Axillary metastases | Postsurgical treatment | Treatment changed due to IM metastases | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IM SLN not considered | IM SLN considered | ||||||||||
| Size (cm) | Grade (BR) | ER | (n) | CT | HT | RT | CT | HT | RT | ||
| Axilla N4+/age<70 | |||||||||||
| 1) 63, BCT | 1.5 | I | + | 7 | + | + | LR | + | + | LR | No |
| 2) 45, BCT | 1.6 | III | + | 4 | + | + | LR | + | + | LR | No |
| 3) 47, mastectomy | 1.8 | I | + | 4 | + | + | LR | + | + | LR | No |
| Axilla N1-3+/age<70 | |||||||||||
| 4) 39, mastectomy | 2.5 | II | + | 3 | + | + | BCT | + | + | BCT+PS | RT |
| 5) 46, BCT | 3.5 | III | − | 3 | + | − | BCT | + | − | BCT+PS | RT |
| 6) 58, BCT | 1.8 | II | + | 2 | + | + | BCT | + | + | BCT+PS | RT |
| 7) 45, BCT | 2.4 | I | + | 2 | + | + | BCT | + | + | BCT+PS | RT |
| Axilla N1-N1a or unfavorable primary tumor characteristics/age<70 | |||||||||||
| 8) 43, BCT | 1.8 | I | + | 1mi | − | − | BCT | + | + | BCT+PS | CT/HT/RT |
| 9) 54, BCT | 2.2 | II | + | 1mi | + | + | BCT | + | + | BCT+PS | RT |
| 10) 66, BCT | 2.5 | II | + | 1mi | − | + | BCT | − | + | BCT+PS | RT |
| 11) 50, BCT | 2.5 | III | + | 1mi | + | + | BCT | + | + | BCT+PS | RT |
| 12) 42, mastectomy | 3.0 | I | + | 1 | + | + | No | + | + | PS | RT |
| Axilla N0/favorable tumor characteristics/age<70 | |||||||||||
| 12) 54, BCT | 2.1 | I | + | 0 | − | − | BCT | + | + | BCT+PS | CT/HT/RT |
| 14) 60, BCT | 2.5 | I | + | 0 | − | − | BCT | + | + | BCT+PS | CT/HT/RT |
| 15) 67, mastectomy | 0.8 | I | + | 0 | − | − | No | − | + | PS | HT/RT |
| 16) 61, BCT | 1.1 | I | − | 0 | − | − | BCT | + | − | BCT+PS | CT/RT |
| Age>70 | |||||||||||
| 17) 82, mastectomy | 2.8 | II | + | 2 | − | + | No | − | + | PS? | RT? |
| 18) 71, BCT | 2.1 | II | + | 1 | − | + | BCT | − | + | BCT+PS | RT |
| 19) 72, BCT | 2.1 | II | + | 1mi | − | + | BCT | − | + | BCT+PS | RT |
| 20) 85, mastectomy | 0.9 | I | + | 1mi | − | − | No | − | + | PS? | HT/RT? |
BCT, breast-conserving therapy; BR, Bloom-Richardson grade; ER, estrogen receptor status; Nax+, number of positive axillary lymph nodes; IM SLN, internal mammary sentinel lymph node; ST, systemic therapy; CT, chemotherapy; HT, hormonal therapy; RT, radiotherapy; PS, parasternal radiotherapy; 1mi, micrometastases.
Adjuvant systemic therapy was already indicated in 14 of the 20 patients with IM metastases due to concomitant axillary LN metastases or unfavorable primary tumor characteristics: ten patients would be candidates for postoperative chemotherapy and 14 would receive hormonal treatment. Based on tumor-positive IM SLNs six additional patients would receive systemic treatment. This proportion reflects 7% of the patients in whom IM SLNs were removed. In four patients chemotherapy was indicated and in five patients hormonal therapy.
In 3 of the 20 patients axillary tumor load (≥4 tumor-positive lymph nodes) was a reason for locoregional radiotherapy including the IM lymphatic chain, leaving 17 patients in whom the radiotherapy field was adjusted because of metastases in the IM SLN. These 17 patients in whom the radiotherapeutic strategy was changed made up 20% of the patients in whom IM sentinel nodes were visualized.
Conversely, there were three patients with ≥4 axillary metastases and IM SLNs without metastases, and in these patients parasternal irradiation was omitted. In addition, parasternal irradiation could also be omitted in 30 patients with ≥4 axillary metastases who had no IM lymphatic drainage on preoperative lymphoscintigraphy.
DISCUSSION
In the present study, SLNs in the IM chain were visualized in approximately one-fifth of the patients who underwent surgery for primary breast cancer. Retrieving these nodes by parasternal intercostal exploration was feasible in the majority of patients. One-fifth of the retrieved IM LNs contained metastases and radiation treatment was adjusted in most of these patients.
In this prospective cohort of patients who underwent SLN biopsy for clinically T1-2N0 breast cancer, IM SLNs were seen on the preoperative lymphoscintigraphy in 22% of the patients.5,6,8,10,11 The visualization rate in our study was rather high and the likely result of the tracer injection technique (Table 6). We used a combination of a parenchymatous peritumoral and a subcutaneous injection technique of the 99mTc nanocolloid, and this technique is associated with a higher visualization rate of IM SLNs than the subcutaneous or periareolar injection of the radiotracer.5–7,12,13 Apart from the effect of the injection technique we observed a higher frequency of lymphatic drainage to the IM LNs in patients with cranio- and caudomedially located tumors, as reported by others,8,14,15 as well as an effect of age: IM SLNs were more common in young patients.
TABLE 6.
Visualization and surgical extirpation rate of internal mammary sentinel lymph nodes (IM SLNs) in breast cancer patients
| Author | Year | n | Method of tracer injection | Visualized IM SLNs (%) | Surgically removed IM SLNs (%)* |
|---|---|---|---|---|---|
| Madsen et al. | 2006 | 506 | PT and SC | 22 | 78 |
| Leidenius et al.10 | 2005 | 984 | IT | 14 | 88 |
| Paredes et al.6 | 2005 | 383 | SC, later IT/PT | 0–17 | 73 |
| Farrus et al.5 | 2004 | 225 | SC, later IT/PT | 11–17 | 69 |
| Estourgie et al.8 | 2003 | 681 | IT | 22 | 87 |
| van der Ent et al.11 | 2002 | 256 | PT | 25 | 63 |
* Proportion of the visualized IM SLNs. SC, subcutaneous; PT, peritumoral; IT, intratumoral.
Retrieving SLNs from the IM chain does not appear to be very troublesome. Approximately 15 min extraoperative time is needed during breast conservative surgery, while extra time is negligible in patients who undergo mastectomy. Although the success rate was lower than for SLNs in the axilla, 78% of the visualized IM nodes could be harvested by the described parasternal intercostal exploration. Others reported similar ‘surgical identification’ rates (69–88%, see Table 6).5,6,8,10,11 It can be difficult to retrieve the usually very small IM SLNs when they are localized directly behind one of the ribs. ‘Blind’ retrocostal dissection is not without risks, and we consider a rib resection not justified as long as the place of parasternal lymph node exploration is not well defined. Although the pleural cavity was breeched occasionally during the procedure and a number of patients had postoperative hematomas, postoperative drainage of a pneumothorax or a reoperation for a bleeding complication of the parasternal wound was never necessary. Other studies also reported low morbidity rates.8,9,11,16,17
In the present study IM LN metastases were found in 24% of the patients who underwent surgical extirpation of these SLNs, while others usually reported lower rates of metastases containing IM SLNs (9–26%).8–11,18 In patients with IM metastases axillary metastases were common: 80% had concomitant axillary metastases.19 Conversely, axillary metastases were accompanied by IM metastases in 8% of the cases. Isolated IM metastases were rare affecting 5% of the patients with harvested IM SLNs and approximately 1% of patients without axillary LN metastases.8,10,19
Successful exploration of SLNs from the IM chain had a substantial impact on subsequent radiotherapeutic treatment. In 20% of these patients adjustment of radiotherapy was considered necessary. Although randomized data about the use of radiotherapy in patients with IM metastases are lacking, adding a parasternal irradiation in these patients appears conceivable. After all radiotherapy does affect locoregional control in other high-risk patient groups such as patients with ≥4 axillary metastases and node-negative patients with young age, poor tumor differentation and large tumor size.20 We consider patients with IM metastases at risk for locoregional recurrence and therefore feel that parasternal irradiation is indicated in patients with IM metastases. Conversely, absence of IM lymphatic drainage or metastases in retrieved IM SLNs justified omission of parasternal radiotherapy in 7% of all the patients.
Systemic treatment strategy was rarely influenced by IM metastases. Due to axillary metastases and unfavorable primary tumor characteristics, half of the patients already would have received chemotherapy and even more would have had hormonal therapy. In the remaining group of patients, old age and negative estrogen receptor status further limited the proportion of patients that would receive adjuvant systemic therapy based on IM LN metastases. However, since prognosis of patients with both axillary and IM metastases is poor when compared with axillary or IM metastases alone,3 patients with IM and axillary metastases might need different chemotherapy schedules. That would increase the proportion of patients in whom adjuvant systemic treatment would be adjusted.
Is IM SLN biopsy worthwhile? One may argue that more extensive radiotherapy was indicated in less than 5% of all patients and additional systemic treatment in only 1%, and thus consider IM SLN biopsy hardly “worth the effort.”10 We feel that the group of patients with visualized SLNs should be taken as a reference, and that the proportion of patients in whom less radiotherapy was given should also be taken into account. As a consequence, we do consider the clinical implications of IM SLN biopsy substantial.
In conclusion, lymphatic drainage of breast cancer to IM LNs is a common feature and retrieving these nodes is relatively easy. The clinical impact of metastases in IM lymph nodes is substantial and justifies surgical exploration for these nodes. We advocate routine parasternal intercostal exploration for IM SLNs whenever preoperative lymphoscintigraphy visualizes IM SLNs. For that purpose we also advocate the (additional) intraparenchymatous tracer injection to optimize the visualization of IM SLNs.
Footnotes
No financial support was received for this study.
References
- 1.UICC TNM classification of malignant tumours. New York: Wiley Liss, 2002
- 2.Lacour J, Le MG, Hill C, et al. Is it useful to remove internal mammary nodes in operable breast cancer? Eur J Surg Oncol 1987; 13:309–314 [PubMed]
- 3.Veronesi U, Cascinelli N, Greco M, et al. Prognosis of breast cancer patients after mastectomy and dissection of internal mammary nodes. Ann Surg 1985; 202:702–707 [DOI] [PMC free article] [PubMed]
- 4.Veronesi U, Marubini E, Mariani L, et al. The dissection of internal mammary nodes does not improve the survival of breast cancer patients. 30-year results of a randomised trial. Eur J Cancer 1999; 35:1320–1325 [DOI] [PubMed]
- 5.Farrus B, Vidal-Sicart S, Velasco M, et al. Incidence of internal mammary node metastases after a sentinel lymph node technique in breast cancer and its implication in the radiotherapy plan. Int J Radiat Oncol Biol Phys 2004; 60:715–721 [DOI] [PubMed]
- 6.Paredes P, Vidal-Sicart S, Zanon G, et al. Clinical relevance of sentinel lymph nodes in the internal mammary chain in breast cancer patients. Eur J Nucl Med Mol Imag 2005; 32:1283–1287 [DOI] [PubMed]
- 7.Rubello D, Zavagno G, Bozza F, et al. Analysis of technical and clinical variables affecting sentinel node localization in patients with breast cancer after a single intradermal injection of 99mTc nanocolloidal albumin. Nucl Med Commun 2004; 25:1119–1124 [DOI] [PubMed]
- 8.Estourgie SH, Tanis PJ, Nieweg OE, et al. Should the hunt for internal mammary chain sentinel nodes begin? An evaluation of 150 breast cancer patients. Ann Surg Oncol 2003; 10:935–941 [DOI] [PubMed]
- 9.Galimberti V, Veronesi P, Arnone P, et al. Stage migration after biopsy of internal mammary chain lymph nodes in breast cancer patients. Ann Surg Oncol 2002; 9:924–928 [DOI] [PubMed]
- 10.Leidenius MH, Krogerus LA, Toivonen TS, et al. The clinical value of parasternal sentinel node biopsy in breast cancer. Ann Surg Oncol 2006; 13:321–326 [DOI] [PubMed]
- 11.van der Ent FW, Kengen RA, van der Pol HA, et al. Halsted revisited: internal mammary sentinel lymph node biopsy in breast cancer. Ann Surg 2001; 234:79–84 [DOI] [PMC free article] [PubMed]
- 12.Knox SM, Ley CA. Comparison of intraparenchymal and intradermal injection for identification of the sentinel node in patients with breast cancer. Proc (Bayl Univ Med Cent) 2002; 15:366–368 [DOI] [PMC free article] [PubMed]
- 13.Krynyckyi BR, Kim CK, Goyenechea MR, et al. Clinical breast lymphoscintigraphy: optimal techniques for performing studies, image atlas, and analysis of images. Radiographics 2004; 24:121–145 [DOI] [PubMed]
- 14.Bevilacqua JL, Gucciardo G, Cody HS, et al. A selection algorithm for internal mammary sentinel lymph node biopsy in breast cancer. Eur J Surg Oncol 2002; 28:603–614 [DOI] [PubMed]
- 15.Byrd DR, Dunnwald LK, Mankoff DA, et al. Internal mammary lymph node drainage patterns in patients with breast cancer documented by breast lymphoscintigraphy. Ann Surg Oncol 2001; 8:234–240 [DOI] [PubMed]
- 16.Dupont EL, Salud CJ, Peltz ES, et al. Clinical relevance of internal mammary node mapping as a guide to radiation therapy. Am J Surg 2001; 182:321–324 [DOI] [PubMed]
- 17.Johnson N, Soot L, Nelson J, et al. Sentinel node biopsy and internal mammary lymphatic mapping in breast cancer. Am J Surg 2000; 179:386–388 [DOI] [PubMed]
- 18.Hong J, Chog E, Soni N, et al. Extra-axillary sentinel node biopsy in the management of early breast cancer. Eur J Surg Oncol 2005; 31:942–948 [DOI] [PubMed]
- 19.Cserni G, Szekeres JP. Internal mammary lymph nodes and sentinel node biopsy in breast cancer. Surg Oncol 2001; 10:25–33 [DOI] [PubMed]
- 20.Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005; 366:2087–2106 [DOI] [PubMed]


