Abstract
Introduction
Radionuclide therapy has distinct similarities to, but also profound differences from external radiotherapy.
Review
This review discusses techniques and results of previously developed dosimetry methods in thyroid carcinoma, neuro-endocrine tumours, solid tumours and lymphoma. In each case, emphasis is placed on the level of evidence and practical applicability. Although dosimetry has been of enormous value in the preclinical phase of radiopharmaceutical development, its clinical use to optimise administered activity on an individual patient basis has been less evident. In phase I and II trials, dosimetry may be considered an inherent part of therapy to establish the maximum tolerated dose and dose-response relationship. To prove that dosimetry-based radionuclide therapy is of additional benefit over fixed dosing or dosing per kilogram body weight, prospective randomised phase III trials with appropriate end points have to be undertaken. Data in the literature which underscore the potential of dosimetry to avoid under- and overdosing and to standardise radionuclide therapy methods internationally are very scarce.
Developments
In each section, particular developments and insights into these therapies are related to opportunities for dosimetry. The recent developments in PET and PET/CT imaging, including micro-devices for animal research, and molecular medicine provide major challenges for innovative therapy and dosimetry techniques. Furthermore, the increasing scientific interest in the radiobiological features specific to radionuclide therapy will advance our ability to administer this treatment modality optimally.
Keywords: Radionuclide therapy, Radiation dosimetry, Radiotherapy, Thyroid carcinoma, Neuro-endocrine tumours, Radio-immunotherapy, Solid tumours, Lymphoma
Introduction
Radionuclide therapy (or “targeted”, “metabolic-or “molecular-radiotherapy) may be defined as a radiation therapy that uses local, loco-regional or generally administered open (i.e. “unsealed”) radionuclides to achieve a transfer of radiation energy to a pathological target tissue and by this means to exert a destructive tissue effect. This “internal-radiation therapy has distinct similarities to, but also profound differences from the more commonly used external radiotherapy (EBRT).
The tissue effect is expressed as the absorbed radiation dose in grays (Gy), i.e. the amount of transferred energy in joules per unit mass of target tissue. The fundamental use of this unit is similar to that in EBRT, and there is a similar relationship between radiation dose and response in terms of cell killing/survival. Therefore, calculation of the radiation absorbed dose to a targeted tissue makes sense at any point in treatment. In this respect, radionuclide therapy dosimetry may be considered an inherent part of radionuclide therapy in principle, as in EBRT.
In the literature, there is considerable confusion over the proper use of the term “dose”, which actually refers to the “radiation dose-in the SI unit “grays”. However, dose in the context of radionuclide therapy is frequently used when actually the “administered activity-in GBq or mCi is meant. To avoid confusion, the terms “radiation dose-and “absorbed dose-are used when indicating Gy and the term “activity dose-when indicating GBq.
Individual patient dosimetry has the following goals [1]:
To establish individual minimum effective and maximum tolerated absorbed doses
To establish a dose-response relation to predict tumour response and normal organ toxicity on the basis of pre-therapy dosimetry
To objectively compare the dose–response results of different radionuclide therapies, either between different patients or between different radiopharmaceuticals, as well as to perform comparisons with the results routinely obtained with external radiotherapy
To increase the knowledge of clinical radionuclide radiobiology, in part with the aim of developing new approaches and regimens
In EBRT, the absorbed dose can be calculated relatively straightforwardly from the energy loss in the body from the point where the radiation enters the body to the target. Radiation in radionuclide therapy is directed to its target by a vehicle (hence “radiopharmaceutical”), which exhibits more or less specific binding to the target tissue. This is a highly dynamic metabolic process, both biochemically and physically, within the time interval of the decaying isotope, and entails a much more complex spatial and temporal radiation distribution than that in EBRT. Pharmacokinetics such as circulation, metabolisation, target expression heterogeneity and cellular uptake and release, as well as radiobiological phenomena such as biological or physical (“cross-fire”) bystander effects [2], play a determining role in the final radiation dose to the target. EBRT is typically a fractionated high dose rate radiotherapy in which episodes of radiation, aimed to cause as much lethal damage as possible, are interspersed with episodes of non-treatment, during which repair and repopulation occur. Radionuclide therapy is radiotherapy with a low and continuously decreasing dose rate, which requires a unique radiobiological approach [3, 4].
Integral activities can be determined numerically or by compartmental models [5] and presently rely heavily on the detection of the activity distribution by gamma cameras. Because the electron range is inferior to the spatial resolution of most molecular imaging devices, the “perfect-dosimetric study cannot be achieved, and calculations are always an approximation. Using the temporal and spatial radionuclide distribution data, radiation doses to target organs have generally been calculated using the MIRD formalism, formerly used for calculation of the biodistribution of diagnostic radiopharmaceuticals. Commercially available software such as MIRDOSE3 or the newer OLINDA/EXM [6, 7] is available for calculation of internal absorbed doses in organs and tumours. Although these models make important assumptions about anatomy (standard man and woman) and radiopharmaceutical distribution (uniformity of uptake in source and target) that are not necessarily valid in individual patients, they do provide a practical and standardised model for clinical end-users.
Nevertheless, to date the need for dosimetry to individually optimise the therapeutic activity to be administered has been far from self-evident. Radionuclide therapy dosimetry has not gained wide acceptance as a clinical tool among the (nuclear) medical community because of an imbalance between the accuracy and the complexity of the procedure. A number of studies have even completely discarded dosimetry, instead using fixed activities for all patients or activities based on kg or m2 body dimensions. [8-10]. To underline that this is unjustified, this review will describe the significant progress that has been achieved over recent years, especially in the fields of instrumentation (with provision of clinically useful instruments), physical modelling and radiobiology. Furthermore, the EURATOM Council Directive 97/43 stipulated that in medical exposures for radiotherapeutic purposes, including nuclear medicine, “exposures of target volumes shall be individually planned”. In this context, the nuclear medicine physician is at present confronted with a “dosimetric dilemma”, because official guidelines and recommendations for most treatments do not include advanced dosimetric calculations. Therefore, this review primarily aims to provide the nuclear medicine practitioner with an up-to-date overview of clinically applied dosimetry techniques in radionuclide therapy. For those working at a more basic level of dosimetry, information is provided on the clinical application of methods and areas of further development. Given the large size of the field of radionuclide therapy, this review is limited to those oncology indications for which there is substantial literature concerning dose calculations, with in-depth discussion thereof. As it would be impossible to cover all areas of the complex subject of dosimetry, appropriate references will be provided where necessary, e.g. regarding basic physics, (radio)biology, radiopharmaceuticals and preclinical aspects.
Radioiodine therapy in differentiated thyroid carcinoma
Radioiodine therapy has proven to be a safe and effective method in the treatment of patients with differentiated thyroid carcinoma (DTC) after total or near-total thyroidectomy [11, 12]. It has been shown to be useful not only for ablation of benign remnant thyroid tissue, facilitating subsequent diagnostic testing, but also for treatment of any remaining cancerous cells either in the thyroid bed or at metastatic sites. Dosimetry plays an important role in answering questions concerning biodistribution since the biological half-time of radioactive iodine differs substantially between individual patients and even within distinct lesions of the same patient. It has proven exceptionally helpful in clinical trials of new drugs, for example retinoids, and in assessment of the use of recombinant TSH [13], as well as in the study of other questions such as the phenomenon of “stunning”. However, its possible role in extending therapy doses to the level of individual maximum effectiveness is currently less obvious.
There is at present no consensus on the activity dose of 131I to be administered in various settings according to recent European and American guidelines [14, 15], largely because of the lack of prospective, randomised data. In the majority of cases, 1.1-3.7 GBq (30-100 mCi) is prescribed empirically for the first radioiodine therapy after thyroidectomy in newly diagnosed DTC, to ablate the remaining glandular tissue. Activity doses as low as 1 GBq are used when the size of the thyroid remnant is small, as measured by the postoperative radioiodine uptake in the neck, and/or to reduce local complications that could arise from radiation thyroiditis/oedema, which has been reported in 10-20% of cases, although usually mild. The effectiveness of this ablative approach based on standard activities is reported to be about 80%. For the treatment of residual tumour, relapses or lymph node metastases, generally higher activities of 3.7-7.4 GBq (100-200 mCi) are used.
Approaches in which quantitative dosimetry is performed to estimate the activity dose needed to deliver an effective radiation dose are scarce in the literature. Maxon and co-workers, using sequential planar scintigraphy, established in the early 1980s that an effective mean radiation dose of at least 300 Gy is required for successful remnant ablation [16]. The validity of this recommendation remains unclear as it conflicts somewhat with clinical experience. It also neglects microdosimetry of radioiodine and dose heterogeneity, which may well determine the overall response. As far as metastases are concerned, these authors concluded in the same study that a radiation dose of at least 80 Gy is associated with a significant increase in response, while a dose of less than 35 Gy offers little chance of success. In a later study [17], they found that when metastatic disease was present only in lymph nodes, a target radiation dose of at least 140 Gy was successful in 86% of patients and 90% of involved nodes. When nodal metastases were associated with either residual thyroid tissue or other metastatic foci, a single treatment calculated to deliver at least 85 Gy to the metastases proved successful in 74% of patients and 81% of nodes. The aforementioned doses were mean absorbed doses for the whole remnant or tumour; no data were provided on the dose distribution in smaller tumour parts. It is also unclear what causes the large difference between radiation dose values for remnants and metastases. This method requires sequential measurements with a scintillation camera 24, 48 and 72 h after administration of 74 MBq (2 mCi) of 131I. De Keizer et al. [18] recently calculated thyroid tumour doses with a similar methodology but with the use of recombinant TSH. A tumour dose of >80 Gy was found in only 20% of metastases visible on post-therapy 131I scanning. In 55% of patients, progressive disease was evident after 3 months and none of these patients had radiation doses to the tumour in excess of 30 Gy, confirming the existence of a clinical dose-response relation.
In cases of distant metastases, higher amounts of 131I are given in single doses and subsequent cumulative therapies. Most centres use a fixed dose of 7.4 GBq (200 mCi), but some use (much) higher activity doses. In order to avoid serious complications (bone marrow suppression, lung fibrosis), the commonly used “maximum safe-administered dose concept published by Benua et al. [19] restricts the blood absorbed dose to less than 2 Gy (200 rad) and the whole-body retention to 4.4 GBq (120 mCi) at 48 h in the absence of diffuse lung metastases. According to the protocol, activity concentration in the whole body as measured by 131I should not exceed 2,960 MBq (80 mCi) after 48 h when diffuse, functioning lung metastases are present. These measurements can be camera based without blood sampling. More recently, the blood dose formula derivation proposed by Hänscheid et al. [13] has provided a new tool for patient-specific blood dose assessment representing marrow dosimetry in DTC therapy. For more precise dosimetry, e.g. in dosimetric studies or for higher targeted blood absorbed doses, sequential blood sampling is recommended [20, 21]. The calculated radiation dose serves as a surrogate parameter for the organ at risk, the bone marrow, since to date direct determination of the bone marrow absorbed dose is not feasible. This method has been applied successfully in clinical practice. Dorn et al. [22] used a dosimetric study prior to therapy with 150-400 MBq 131I and obtained daily images up to 4-5 days. They maximised the administered activity to an absorbed dose of 3 Gy to the bone marrow or 30 Gy to the lungs, corresponding to the LD5/5 in EBRT, while aiming at >100 Gy to all known metastases. This resulted in a mean of 22.1 GBq (597 mCi) and a range of 7.4-38.5 GBq (200-1,040 mCi) activity administered per treatment. Many institutions will find it difficult to deliver these amounts owing to radioprotection restrictions, limiting the applicability of this method. To date, bone marrow depression has rarely been reported, while the rate of dose-related leukaemia has been estimated to be approximately 1% after 5-10 years. Lung fibrosis as a consequence of micronodular iodine-avid metastases has been reported in 1% of patients suffering from pulmonary metastases. The downside of these high-dose strategies may be an increase in the occurrence of these side-effects. On the other hand, assuming this “maximum safe dose-to be an optimal dosing strategy, extrapolation to a “fixed activity dose-strategy of 7.4 GBq (200 mCi), as is widely applied, would “under-treat-54% and “over-treat-3% of patients [23]. To date, there are no randomised and prospective trials that directly compare a low- and high-activity dose strategy in patients with metastases.
The treatment of DTC in childhood varies substantially from the standard approach in adults mainly owing to the different tumour biology in this age group. Usually activities of 50-100 MBq/kg are given, treatment data on children being scarce and non-systematic.
There are a number of potential drawbacks of dosimetry that may preclude its use in many centres. One problem is the uncertainty of volume determinations by neck ultrasound shortly after thyroid surgery since the differentiation between scar tissue, haematoma and thyroid remnant is often difficult. The same holds true for the use of computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET) in the evaluation of distant metastatic lesions, especially in the case of diffuse lung metastases. Also, it is difficult to predict radioiodine kinetics during therapy from prior diagnostic studies owing to the large difference in administered and measured activity and potential subsequent biological effects. PET studies using the cyclotron product 124I-NaI, if possible in combination with PET/CT tomography, may prove to be particularly valuable in improving treatment planning and patient-specific dosimetry. Compared with conventional methods, including CT and 131I scanning, this technique was found to be superior in terms of lesion detection and functional assessment [24]. Using three-dimensional 124I-PET voxel-based dosimetry, Sgouros et al. [25] showed a wide range of mean absorbed dose values for individual tumours, from 1.2 to 540 Gy. Unfortunately, no correlation with response was reported in that study. However, this wide variation certainly implies that the assessment of meaningful dose-effect relationships and clinical dosimetry should include further development of a quantitative approach.
131I-mIBG therapy in neuroblastoma and phaeochromocytoma
For more than two decades, mIBG labelled with the γ/β emitter iodine-131 (131I-mIBG) has been used to treat neural crest-derived tumours, essentially neuroblastoma and phaeochromocytoma, both in relapsed and in newly diagnosed patients. In high-stage neuroblastoma, the treatment may represent (a) palliative therapy [26], (b) first-line therapy, as a single agent or combined with chemotherapy [27], (c) consolidation therapy after induction of a “good partial remission-[28] and, more recently, (d) second-line therapy after failed induction chemotherapy, combined with topotecan and stem cell rescue in children with metastatic neuroblastoma [29] or with myeloablative chemotherapy and autologous stem cell transplantation in refractory neuroblastoma [9]. In neuroblastoma, important efforts have been made to develop clinically useful dosimetry methods to predict the radiation dose to the red marrow as the critical organ for bone marrow toxicity, in order to apply optimal and individual dose maximisation in children with highly aggressive tumours. Three different methods of activity administration have evolved from the experience of treating such patients.
The first approach, developed in Amsterdam, the Netherlands, is to give fixed activity dose “fractions-of 7.4-11.1 GBq (200-300 mCi), more recently combined with hyperbaric oxygen or topotecan. This approach has been proven to have a synergistic effect on cell killing in vitro when used in combination with 131I-mIBG [30]. Intervals between fractions are determined by blood count recovery and the treatment is continued to maximum response [31]. An advantage of this method is its simplicity, which may be viewed as important in very sick children and in those who require prompt treatment, especially when receiving first-line therapy. Another important advantage of lower activity doses is the shorter isolation and hospitalisation period required for reasons of radioprotection, which may be regarded as highly significant in these usually very sick children with a grave prognosis. As whole-body and tumour radiation doses are never calculated, any kind of dose-response assessment and optimisation on the basis of absorbed radiation dose is, however, impossible. Furthermore, the relatively low dose rate of radiation compared with (ultra-)high doses may be viewed as radiobiologically suboptimal. The clinical results of this approach need to be verified in a multicentre phase III trial that should include a dosimetric assessment of the whole-body dose.
The second approach originates from the United Kingdom, where there has been a long tradition of using pre-therapy dosimetry. In a phase I/II study on advanced, chemo-refractory stage III/IV patients, Lashford et al. observed that 80% of patients developed grade 3 or 4 haematotoxicity at a whole-body absorbed dose of 2.5 Gy established from a pre-therapy 131I-mIBG scan [32]. Monsieurs et al. used 123I-mIBG prior to therapy to the same effect [33]. Previously, Tristam et al. had shown a highly skewed distribution of tumour radiation doses after a fixed, diagnostic activity [34]. Matthay et al. found a good correlation between whole-body and tumour dose [35]. As radiation dose is principally related to response, this approach may lead to a more standardised whole-body and tumour absorbed dose [36] and may offer more possibilities of dose escalation, especially in the presence of an altered biodistribution, e.g. due to partial kidney failure or high tumour load. Recently, an ESIOP experimental mIBG protocol has been proposed in which the aim is to deliver a total whole-body absorbed dose of 4.0 Gy in two fractions, in combination with topotecan, after failure of induction chemotherapy. Post-therapy dosimetry is performed after a first fixed fraction of 440 MBq/kg (12 mCi/kg), with calculation of the activity dose to be administered with the subsequent second fraction in order to arrive at the desired total whole-body absorbed dose of 4 Gy. The importance of this protocol is that whole-body and tumour absorbed dose can be estimated and the relation to both toxicity and response can be established, unlike with the non-dosimetry protocols. The schedule of intensification of mIBG therapy by dose escalation and radiosensitisation with topotecan with a haematopoietic autograft has been shown to be safe and practicable [29]. The next step will be to prove that this approach will also lead to a better outcome in neuroblastoma patients.
The third approach can be derived from recent publications from the United States, in which patients received high activity doses of mIBG on the basis of an activity dose of 550-660 MBq per kilogram body weight (15-18 mCi/kg), with stem cell support if necessary. In an early study, Sisson and co-workers examined predictors of toxicity and found the best correlation to be between whole-body absorbed dose and platelet ratio; however, comparable and statistically significant correlations were found with GBq/kg body weight and GBq/m2 body surface [37]. This observation was supported by Matthay and colleagues [35], who found the amount of 131I (GBq/kg) and whole-body dose (Gy), but not administered activity dose (GBq), to be significantly correlated with platelet and neutrophil nadir. In a recent study by Dubois et al. [38], substantial haematotoxicity was seen at 660 MBq/kg (18 mCi/kg) in a group of patients with advanced, heavily pre-treated neuroblastoma, including myeloablative chemotherapy in 81%. Of these patients, 36% required autologous haematopoietic stem cell transplantation. The resulting median whole-body absorbed dose was 2.92 Gy with a median administered activity dose of 13.5 GBq (366 mCi, range 198-895 mCi). Interestingly, whole-body radiation dose was shown to correlate with failure to engraft platelets or red cells in those patients receiving autologous stem cell transplantation. An encouraging response rate of 27% was reported, however. The same authors recently established a maximum tolerated dose (MTD) of 440 MBq/kg (12 mCi/kg) with myeloablative chemotherapy and autologous stem cell transplantation [9]. The advantage is that there is no need for planning/simulation in this high-dose protocol, which may increase in importance if multiple centres participate.
Malignant, metastatic phaeochromocytoma is a very rare disease but can be excellently treated by 131I-mIBG in both a palliative and a curative setting. Literature data on dosimetry are scarce and casuistic. In 1997, Loh et al. reviewed the literature concerning 116 previously treated cases [39]. They found a cumulative activity dose of 3.6-85.9 GBq (96-2,322 mCi, mean 490 α 350 mCi) in 1-11 (mean 3.3 α 2.2) therapies, with a mean single activity dose of 5.8 GBq (158 mCi). Dose prescriptions were as a fixed activity dose of 3.7-11.1 GBq (100-300 mCi or 3-9 mCi/kg). A recent study was performed in order to evaluate the performance of mIBG therapy with high activities after debulking surgery [40]. The median individual cumulative activity dose was 37.6 GBq (1,015 mCi), with a range of 14.3-62.5 GBq (386-1,690 mCi), in one to three consecutive therapies. Grade 3 platelet toxicity was observed after 79% of therapies, and grade 3 and 4 neutrophil toxicity after 53% and 19% of therapies, respectively. All patients had stem cells harvested before therapy, but 11 patients showed spontaneous reconstitution and only one required stem cell return. Response rate was 10/12 patients (83%).
Radiopeptide therapy for neuro-endocrine tumours
Several clinical trials have investigated the use of peptide receptor radionuclide therapy (PRRT) with a radiolabelled somatostatin analogue as one of the newly developed targeted tools for neuro-endocrine tumours [41-44]. Individual pre-therapeutic dosimetry is necessary for patient selection and therapy planning because there are huge inter-patient differences in radiopeptide uptake in normal organs and tumour tissues. This may be related to varying somatostatin receptor densities on tumour cells, as well as to factors such as tumour volume, interstitial pressure and viability. The dosimetric studies that have been performed in this treatment have been the most sophisticated in the field and exemplory for other types of treatment. Initial studies were performed with the radiopeptide used in diagnostics, [111In-DTPA0]-octreotide, given in high activities. Results were encouraging, with symptomatic and biochemical responses in a large percentage of patients, although objective responses were rare [42]. The analogue [90Y-DOTA0,Tyr3]-octreotide has been investigated in various phase I-II trials [41, 43]. 90Y-labelled lanreotide has also been investigated (in the MAURITIUS trial) [45]. For dosimetry of 90Y from post-therapeutic bremsstrahlung, images that substantially lack quality must be quantified. Therefore, two alternative approaches have been developed as a surrogate for the original radiopeptide, namely therapy simulation with either the 111In-labelled peptide or the 86Y-labelled peptide [46, 47]. These methods are intended to provide pre-therapy assessment of the optimal activity administration [48-51] (Table 1). The variation that can be appreciated among the various combinations in the table may be primarily technical/methodological in origin but also biological, based on differences in somatostatin receptors and isotope/chelator affinity. The reader is referred to the respective papers for more detailed information.
Table 1.
Absorbed doses to principal organs and to tumour (Gy/GBq ±SD), deriving from different radiopeptides
| Stabin 1997 [109], Kwekkeboom 2001 [50] | Kwekkeboom 2001 [50] | Cremonesi 1999 [47] | Forster 2001 [110] | Helisch 2004 [111] | Forrer 2004 [112] | |
|---|---|---|---|---|---|---|
| Therapy | [111In-DTPA0, Tyr3]-octreotide | [177Lu-DOTA0, Tyr3]-octreotate | [90Y-DOTA0, Tyr3]-octreotide | [90Y-DOTA0, Tyr3]-octreotide | [90Y-DOTA0, Tyr3]-octreotide | [90Y-DOTA0, Tyr3]-octreotide |
| Dosimetry | [111In-DTPA0, Tyr3]-octreotide | [177Lu-DOTA0, Tyr3]-octreotate | [111In-DOTA0, Tyr3]-octreotide | [86Y-DOTA0, Tyr3]-octreotide | [86Y-DOTA0, Tyr3]-octreotide | [111In-DOTA0, Tyr3]-octreotide |
| Patients | 16 | 5 | 30 | 3 | 8 | 5 |
| Kidneys | 0.52 α 0.24 | 1.65 α 0.47 | 3.9 α 1.9b | 2.73 α 1.41 | 2.84 α 0.64 | |
| Kidneys + protection | 0.88 α 0.19 | 1.71 α 0.89 | ||||
| Liver | 0.065 α 0.01 | 0.21 α 0.07 | 0.72 α 0.57 | 0.66 α 0.15 | 0.72 α 0.40 | 0.92 α 0.35 |
| Spleen | 0.34 α 0.16 | 2.15 α 0.39 | 7.62 α 6.30 | 2.32 α 1.97 | 2.19 α 1.11 | 6.57 α 5.25 |
| Red marrow | 0.03 α 0.01 | 0.07 α 0.004 | 0.03 α 0.01 | 0.49 α 0.002 | 0.06 α 0.02 | 0.17 α 0.02 |
| Tumour (range) | 0.72-6.8a | 3.9-37.9 | 1.4-31 | 3.21-19.58 | 2.1-29.5 | 2.4-41.7 |
Although [90Y-DOTA0,Tyr3]-octreotide (or -lanreotide) and its imageable counterpart [111In-DOTA0,Tyr3]-octreotide (or -lanreotide) are not chemically identical, the latter has been used for dosimetric simulation, based on the hypothesis that the similar physical and biological half-lives yield a comparable in vivo pharmacokinetics and biodistribution, especially concerning the renal uptake, which depends on aspecific phenomena. A drawback of this method is that the small structural modification may affect the somatostatin receptor binding affinity [52]. Regarding biodistribution, the organs receiving the highest predicted absorbed doses, in a first series of 18 patients, included the spleen (7.6 α 6.3 mGy/MBq), the kidneys (3.3 α 2.2 mGy/MBq) and the tumour (1.4-31 mGy/MBq, mean 10). When the series was enlarged to 30 patients, a slightly higher kidney absorbed dose (3.9 α 1.9 mGy/MBq) was observed [43]. Shortcut approaches involving use of the commercially available molecule [111In-DTPA0]-octreotide or OctreoScan® have been proposed [53]. Nonetheless, probably as a result of the quite different biokinetics and receptor affinity of [90Y-DOTA0,Tyr3]-octreotide and [111In-DTPA0]-octreotide, which are indeed chemically different, comparative data obtained appear not to be sufficiently overlapping for this tracer.
A thorough dosimetric study using PET with [86Y-DOTA0,Tyr3]-octreotide, biochemically identical to the therapeutic molecule, was carried out in 24 patients [54]. This offers substantial advantages in terms of spatial resolution and quantification, but the short half-life of the radionuclide leaves later phases of the biokinetics to estimates based on extrapolation.
The newest radiopeptide, [177Lu-DOTA0,Tyr3]-octreotate, offers further advantages. 177Lu has a lower energy (Emax 0.49 MeV) and penetration range (Rmax 2 mm) emission, but a longer half-life (6.7 days). The low abundance gamma emissions (113 and 208 keV) allow for dosimetry and imaging prior to as well as post therapy. Moreover, octreotate has a six- to ninefold higher affinity for somatostatin receptor 2, the somatostatin receptor most frequently expressed in neuro-endocrine tumours. Unfortunately, to date a thorough dosimetric analysis is lacking, but data deriving from a study comparing [177Lu-DOTA0,Tyr3]-octreotate with [111In-DTPA0]-octreotide indicate that, compared with [90Y-DOTA0,Tyr3]-octreotide, [177Lu-DOTA0,Tyr3]-octreotate delivers a lower burden to organs, with absorbed doses of 1.8-2.7 mGy/MBq to the spleen, 1.0-2.2 mGy/MBq to the kidneys (lowered to 0.7-1.1 mGy/MBq with protection) and 0.1-0.3 mGy/MBq to the liver. Red marrow absorbed dose, derived by the blood approach, ranged from 0.05 to 0.08 mGy/MBq [44].
Due to their marked radiosensitivity, the kidneys undoubtedly represent the critical organ, particularly after [90Y-DOTA0,Tyr3]-octreotide. Renal irradiation arises from the proximal tubular re-absorption of the radiopeptide and the resulting retention in the interstitium. According to EBRT studies, the renal maximum tolerated absorbed dose is conventionally considered to be in the range of 23-25 Gy. According to the National Council on Radiation Protection and Measurements (NCRPM) an absorbed dose of 23 Gy to the kidneys causes detrimental deterministic effects in 5% of patients within 5 years [55]. Sporadic cases of delayed renal failure, in some cases end-stage disease requiring dialysis, have been observed, especially in patients who have received an activity dose of more than 7.4 GBq/m2 [56]. Nephrotoxicity is accelerated by other risk factors, such as pre-existing hypertension or diabetes. Given the high kidney retention of radiopeptides, positively charged molecules, such as L-lysine and L-arginine, are used to competitively inhibit the proximal tubular re-absorption of the radiopeptide. This results in a reduction in the renal absorbed dose of between 9% and 53% [57]. Doses are further reduced by up to 39% by prolonging infusion over 10 h and by up to 65% by prolonging it over 2 days after radiopeptide administration, thus covering more extensively the elimination phase through the kidneys [43]. Despite kidney protection, renal function loss may become clinically evident years after PRRT. A median decline in creatinine clearance of 7.3% per year was reported in patients treated with [90Y-DOTA0,Tyr3]-octreotide and of 3.8% per year in patients treated with [177Lu-DOTA0,Tyr3]-octreotate. Cumulative and per cycle renal absorbed dose, age, hypertension and diabetes are considered factors contributing to the decline of renal function after PRRT [58]. Clinical experience and dosimetric studies clearly indicate that the renal absorbed dose estimated by conventional dosimetry does not accurately correlate with the renal toxicity observed in patients treated with [90Y-DOTA0,Tyr3]-octreotide. Consideration of additional parameters, such as patient-specific kidney volume and distribution of the radionuclide, appears to give a better correlation with the clinical effects [59]. Assessment of individual kidney volume by CT scan yields a wide variability when compared with the standardised phantom. Moreover, autoradiographic studies, performed on human kidney after in vivo injection of 111In-peptides, have demonstrated that the majority of radioactivity is deposited within the renal cortex, mainly in the juxtamedullary region. This leads to a higher deposition of energy per unit mass, compared with conventional dosimetry. Hence, calculation of the kidney absorbed dose assuming a homogeneous renal distribution of radioactivity is inadequate. New techniques accounting for the difference in radioactivity placement in the kidneys, on the basis of a CT-based volumetric analysis, appear more realistic [60].
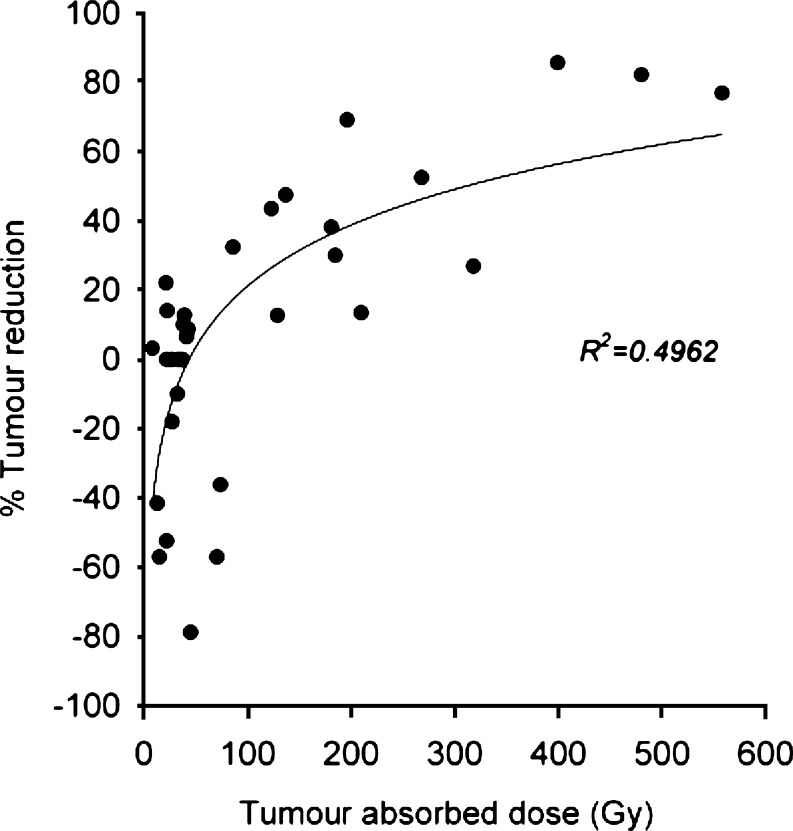
Even if predicted absorbed doses are much lower than the threshold for toxicity, the other target organ that gives rise to concerns about acute and permanent toxicity after PRRT is the bone marrow, particularly in repeated administrations [41-43]. Acute haematological grade 3 or 4 toxicity is not uncommon, especially after [90Y-DOTA0,Tyr3]-octreotide, and sporadic cases of myelodysplastic syndromes or even overt acute myeloid leukaemia have been reported with all three therapeutic radio-compounds. Bone marrow dosimetry is usually modelled through a blood-based method, in which an equivalent distribution of the radioactivity from blood throughout the bone marrow is conservatively considered [61, 62]. Currently, the potential risk of kidney and red marrow limits the amount of radioactivity that may be administered. Indeed, when tumour masses are irradiated with suitable doses, volume reduction may be observed (Fig. 1) [63]. Tumour remission is positively correlated with high uptake during [111In-DTPA0] octreotide scintigraphy. Nevertheless, tumour radiation dose depends not only directly on the administered activity and the uptake versus time, but also on the tumour load. This is confirmed by clinical data regarding the response characteristics: patients with a limited number of liver metastases respond to PRRT, whilst patients with a high tumour load do not [45]. Mathematical models have shown that 177Lu is better in small tumours (optimal diameter 2 mm), whilst 90Y is better in larger ones (optimal diameter 34 mm): very small masses are likely not to absorb all the β-energy released in the tumour cells by 90Y, while larger tumours will suffer from lack of uniformity of activity distribution of 177Lu. Finally, differences in dose rate must be taken into account: the longer physical half-life of 177Lu means a longer period is needed to deliver the same radiation dose than when using 90Y. This may allow more time for tumour re-population [64]. Therefore, combination therapy with 90Y and 177Lu, either simultaneously or in distinct settings, has been suggested to overcome the difficulties of real clinical situations involving different sized lesions.
Fig. 1.
Tumour dose-response relationship in 13 patients treated with 90Y-DOTATOC. Tumour volumes were assessed by CT before and after treatment. Tumour dose estimates were derived from CT scan volume measurements and quantitative 86Y-DOTATOC imaging performed before treatment. Data were further computed using the MIRDOSE spherical model. Reprinted by permission of the Society of Nuclear Medicine from [63]
Treatment of solid tumours by radiolabelled antibodies
Most clinical radioimmunotherapy (RIT) studies have been performed in colorectal cancer, using antibodies against CEA, TAG-72, A33 and KSA. Other tumours studied have included ovarian cancer (anti-MX35, anti-folate receptor Mov18, anti-HMFG1), prostate cancer (anti-PMSA), breast cancer (anti-mucin BrE3, NR-LU-10), glioma (anti-tenascin) and renal cancer (anti-G250) [65].
Although at later time points after injection of radiolabelled monoclonal antibodies, adequate to high uptake may serve to delineate deposits of solid tumours, the relatively unfavourable therapeutic window between the anti-tumour effect and toxicity hampers the introduction of these agents in the clinic. Solid tumours are generally more radioresistant than, for example, malignant lymphoma. The absorbed doses required to achieve a response of tumour deposits are higher than those needed to obtain a response in malignant lymphoma. Activity doses leading to adequate absorbed doses in tumour deposits therefore result in significant radiation-induced toxicity, primarily of the bone marrow, as the most radiation-sensitive organ; myeloablation may be the goal as well as the result of this.
Most studies aim at administration of the MTD that results in acceptable toxicity to the bone marrow, as the organ responsible for dose-limiting toxicity. Several methods have been reported for calculation of the absorbed dose to the bone marrow, e.g. region of interest analysis of scintigraphic data or a model based on radioactivity in the blood. When radiolabelled antibodies bind to blood, bone and bone marrow components or when the radionuclide accumulates in bone or bone marrow upon metabolisation of the radionuclide-antibody complex, calculation of the red marrow dose is more complex than when using radiolabelled antibodies that lack these characteristics [66, 67]. The use of a model for bone marrow dosimetry using blood activity may result in better reproducibility of the bone marrow dosimetry. Wessels et al. [68] observed that historical variations as high as 200-700% between different institutions performing marrow absorbed dose calculations could be dramatically reduced to −29% to +20% by a central computing facility and the use of similar methodology, based on the standard American Association of Physicists in Medicine (AAPM)/Sgouros blood model [66].
In a study using 131I-labelled murine monoclonal antibody G250 in patients with metastatic renal cell cancer, haematological toxicity correlated with whole-body absorbed radiation dose [69]. In a retrospective analysis of 114 patients who underwent 131I-labelled antibody therapy, absorbed dose-based definitions of MTD and escalation variables proved to be better than activity-based methods [70]. In a study in which therapeutic doses of 131I-cG250 (the chimeric variant of G250) were administered, no correlation was found between haematological toxicity and either the radiation absorbed dose to the whole body or bone marrow or the administered activity [71]. Juweid et al. observed that besides red marrow dose, baseline blood counts, multiple bone and/or marrow metastases and recent chemotherapy are important factors related to haematological toxicity after radio-immunotherapy [72], making a dosimetric approach to identify the optimal radionuclide dose more complicated.
One way to overcome the unfavourable therapeutic index of tumour response and normal organ toxicity is to focus on treatment of patients with minimal residual disease. For example, patients with ovarian cancer in complete remission after debulking and chemotherapy have an approximately 50% chance of relapse. Compared with results in matched controls, Nicholson et al. observed an increase in 5-year survival from 55% to 80% following intraperitoneal administration of 90Y-labelled HMFG1 in patients with ovarian cancer in complete remission after chemotherapy [73]. However, a more recent randomised clinical trial in patients with ovarian cancer in complete remission after debulking and chemotherapy did not reveal a benefit in disease-free and overall survival after treatment with 90Y-labelled murine HMFG1 [74]. Introduction of 90Y-muHMFG1 did not delay the time to relapse and did not result in prolonged survival as compared with the control group. One can argue that 90Y is far from ideal for treatment of minimal residual disease owing to its high β-energy, and that radionuclides with lower range emissions, such as 177Lu, have more favourable characteristics for this purpose. Furthermore, relatively large antibody doses were used, which may have resulted in saturation of the epitopes on cancer cells and subsequently in low tumour-to-non-tumour ratios of radioactivity uptake. Obviously, clinical dosimetry could play an important role in explaining these differences in therapy results.
A very significant advance that promises to increase the radiation dose to the tumour while reducing that to the bone marrow is the development of pre-targeting strategies. In pre-targeting, the tumour is first targeted with a specific non-radioactive monoclonal antibody construct. The antibody construct is allowed to accumulate in the tumour and to clear from the blood and non-target tissues. Subsequently, a small radioactive hapten is injected which has high affinity for the antibody construct. The radioactive hapten targets the antibody construct, while demonstrating rapid renal excretion. Examples of these approaches are the use of bispecific monoclonal antibodies and the biotin-avidin system [75, 76]. As pre-targeting increases the tumour/normal organ uptake ratio [77], these approaches hold great promise for enhanced therapeutic efficacy. However, the use of multiple drugs poses the problem of fine-tuning dosing and timing of the interval between injections. Optimisation of the dosing and timing schedule is needed for optimal targeting of the tumour by the radioactive compound, while assuring low normal organ uptake. Robust dosimetric analysis of tumour and normal organ uptake of the radioactive small molecule is a requirement for the successful development and implementation of pre-targeting strategies [78, 79].
Radioimmunotherapy of B-cell lymphoma
Research in RIT in lymphoma has resulted in two FDA-approved radiopharmaceuticals, 90Y-ibritumomab or Zevalin® (IDEC Pharmaceuticals and Schering AG) and 131I-tositumomab or Bexxar® (Glaxo Smith Kline), for the treatment of B-cell lymphoma [80, 81]. Both are directed against CD20, albeit not against the same epitope. They are both approved for the treatment of relapsed or refractory follicular/low-grade or transformed B-cell lymphoma including rituximab-refractory follicular B-cell lymphoma in the US, but only Zevalin is approved in the EU and only for follicular lymphoma. Pre-treatment with unlabelled monoclonal antibody (=preload) as part of the treatment with Zevalin and Bexxar is current practice, as it leads to a more favourable biodistribution. This has been studied in animal models, as well as in the setting of myeloablative RIT [82-84]. The preload may clear peripheral B cells from the circulation, improving tumour targeting of subsequently administered radiolabelled monoclonal antibodies. This optimisation has been accomplished by diagnostic and dosimetric 111In or 131I tracer studies. On the other hand, the intrinsic therapeutic efficacy of the antibody is a confounding factor, making evaluation of the relation between absorbed dose and treatment response more difficult than for other radiopharmaceuticals [85, 86].
Bexxar has been developed using the whole-body absorbed dose as a substitute for bone marrow dosimetry by administering a trace amount of 131I-labelled CD20 antibody and determining the total body clearance prior to therapy in order to calculate the patient-specific injected activity dose that should deliver the specified absorbed dose to the whole body. The method has been further simplified to an estimation based on three points [87]. In a dose escalation study with absorbed doses to the whole body ranging in 0.1-Gy increments from 0.25 to 0.85 Gy, the MTD was found to be 0.75 Gy in patients who had not received prior high-dose chemotherapy with stem cell support and who had platelet counts of ≥150 × 109/litre. A comparison between the therapeutic activity calculated on the basis of the diagnostic pre-therapy tracer study and the amount calculated per kilogram body weight showed that, using the latter method, 50% of the patients would have been either over- or underdosed by 10% or more, and 16% of the patients by 25% or more. Interestingly, a correlation between the duration of complete remission (CR) and the absorbed dose to the whole body was found. Patients receiving a whole-body absorbed dose between 0.65 and 0.85 Gy showed longer CR than patients receiving between 0.25 and 0.55 Gy [88]. In contrast, Zevalin has been developed with the notion that dosimetry may be dispensable. In a randomised study comparing Zevalin with rituximab alone, a secondary objective was to determine whether dosimetry was required [10]. A tracer dose of 185 MBq (5 mCi) 111In was administered for dosimetric purposes with the first infusion, followed by a therapeutic activity dose of 0.4 mCi/kg (15 MBq/kg) Zevalin 7 days later. The absorbed doses to normal organs and the marrow were found to be within the specified limits of 20 Gy for solid organs and 3 Gy for red marrow in 72 patients. The median estimated absorbed dose to the tumour was 15 Gy (range 0.6-24 Gy). There was no significant correlation between dosimetric and pharmacokinetic parameters and haematological toxicity, although the correlation between nadir of the neutrophil count and the whole blood half-life of 90Y exhibited borderline statistical significance. It was concluded that dosimetry may be excluded for populations of Zevalin patients who meet certain criteria for pre-treatment platelet count and percentage of marrow involvement by tumour.
A possible explanation for this discrepancy may be found in the photon energy emitted by 131I; this may account for a large part of the cross-absorbed dose to the bone marrow, which is almost independent of the amount of bone marrow involvement. It has been reported that the self-absorbed dose accounts for 64% of the whole absorbed dose to the red marrow [89], leaving 36% as the cross-absorbed dose. Scintigraphic assessment of absorbed dose to the bone marrow has its shortcomings owing to over- and underlying tissues as well as to the local variability in bone marrow involvement by the disease targeted. It is especially difficult to use pharmacokinetic data for calculation of the absorbed bone marrow dose, since bone marrow involvement is a strong confounder. Other important issues are the bone to bone marrow ratio and variable values for the activity concentration in the blood and red marrow [90, 91]. A fixed ratio between blood and bone marrow has been used in bone marrow dosimetry based on blood radioactivity levels [10, 64]. However, it has been suggested that the red marrow to blood ratio is not fixed, but increases continuously up to 72 h post injection in both patients and rats [92]. Furthermore, haematological toxicity, like tumour response, is a deterministic effect of radiation, characterised by a sigmoid rather than by a linear dose relationship [93]. A sigmoid relationship may be discernible in a reasonably homogeneous population, but is likely to be more difficult to identify if the population is heterogeneous. The bone marrow reserve may be more relevant to the magnitude of toxicity than is the absorbed dose. Another particular challenge to haematology RIT dosimetry may be tumour regression during energy deposition, as is frequently the case in rapidly responding lymphoma. This may lead to underestimation of absorbed dose, since dose is per definition energy per unit mass [94]. The opposite will be the case if the tumour grows during energy deposition. To avoid this pitfall, repeated volume assessments during therapy would be necessary, or alternatively one could use voxel-based dosimetry, which is likely to be less sensitive to changes in mass.
Myeloablative RIT at the MTD for normal organs is by definition dependent on dosimetry. Dose-limiting organs may be the lungs, kidneys or liver. In high-dose RIT using the 131I-labelled mouse antibody tositumomab, the lungs were found to be the dose-limiting organ in 28 of 29 patients and the kidneys in the remaining patient [95]. The opposite was found when the pharmacokinetics of the chimeric 131I-labelled rituximab were studied, i.e. the kidneys were found to be the critical organ [96]. These differences may be due to the significant difference in half-life between the antibodies, the chimeric and murine antibodies having half-lives of 88 h and 56 h, respectively. The MTD for myeloablative 131I-tositumomab was established to be 25 Gy to the lungs. Studies of myeloablative RIT using 90Y are ongoing and encouraging results have been reported [97].
In several experimental studies, Auger emitters have been therapeutically superior to β emitters when taken to the MTD [98, 99]. This is likely to be due primarily to lower bone marrow toxicity but is perhaps also attributable to the deposition of more energy in single cells or small tumour cell clusters. Auger emitters would thus be advantageous in an adjuvant setting, in leukaemia, but they may also be superior where there is tumour bulk. The challenge is how to estimate absorbed dose in single cells, but one may begin in patients with a significant amount of circulating tumour cells that can be studied ex vivo [100]. Interestingly, Kaminski reported that in a number of patients who relapsed following RIT the relapse occurred only at sites previously not known to be involved with tumour [101]; this indicates a possibility that small tumour manifestations receive lower absorbed doses than expected on the basis of antigen density and tumour diameter [102].
Discussion
As stated by DeNardo [103], “claims for specific dosimetry have to demonstrate that the frequency of excess toxicity and/or tumour underdosing significantly decreases”. Dosimetry should provide a quantification procedure that is primarily of additional benefit over empirical, fixed dosing with or without visual scintigraphic assessment. In standard oncology practice, a new therapeutic agent undergoes phase I, II and III testing before becoming a standard treatment. In a phase I study, the maximum tolerated dose is established and side-effects recorded. Dosimetry should play an essential role in this phase and establish a threshold dose above which clinically significant side-effects occur. In phase II, the new radionuclide therapy is evaluated in terms of effect on tumour response and survival. Here, dosimetry should enable the determination of a clinical dose-response relationship. In phase III, the new therapy is compared with the standard one. At this stage, dosimetry helps to elucidate the clinical effects in a larger patient group, e.g. it may be observed that some subgroups have a better or worse result. Moreover, multicentre trials offer the opportunity to compare results in different institutions and countries, as well as provide the opportunity to standardise the dosimetry procedure in a larger context. Evidence-based medicine entails randomised and prospective trials. However, after 60 years of treating thyroid cancer patients, international guidelines still cannot provide a consensus on the amount of radioiodine that should be given. Undoubtedly, the need for randomised trials will increase in the coming years, as in other areas. This underlines the importance of stepping up scientific efforts to include optimal dosimetry not only as an inherent part of radionuclide therapy, but also as an inherent part of these studies. In this context, there was a remarkable recent editorial in the Journal of Clinical Oncology [104], discussing the limitations of the body surface principle that forms the basis for chemotherapy dosing. Indeed, the bioavailability of chemotherapy, and hence the dose to the target, suffers from a similar metabolic variability as is observed for radionuclides, and this variability seems to be more important than can be accounted for by the body surface in square metres as the sole parameter. Interesting parallels may be drawn for translational research, for example in pharmacokinetic modelling and molecular imaging.
Many modern gamma cameras are optimised for photons below 200 keV and are less suitable for radionuclide therapy dosimetry if higher energy photons are involved. SPECT overcomes the problem of superimposition of target and other activity, but spatial resolution at depth is always worse than in planar imaging, so quantification has to rely on more or less representative phantom models [105]. PET has a 30-40 times higher sensitivity for a given spatial resolution that is typically 5 × 5 mm. This is a major advantage over SPECT in pharmacokinetic dynamic modelling. Correction for attenuation has become relatively easy with the new PET/CT and SPECT/CT cameras, but other correction factors, e.g. for scatter, linearity and calibration, are also critical. Partial volume effects are a major issue in the quantification of small tumours and occur at below about twice the spatial resolution. This is thus more of a problem for SPECT (spatial resolution for 131I, 25-30 mm) than for PET (spatial resolution 6-8 mm). Finally, as discussed in the radiopeptide section, the radionuclides used for dosimetry must show similar biochemical and physical behaviour to those used for therapy. As previously highlighted, the use of 124I PET and 86Y-DOTATOC PET dosimetry [25, 59] has been a landmark development. PET/CT and SPECT/CT and “molecular-radiopharmaceutical developments offer major opportunities for radionuclide therapy dosimetry [1]. Further improvements in the performance of these cameras, and hence dosimetry, can be foreseen. Also, the proliferation of microsystems such as micro-PET/SPECT/CT/MRI is allowing dynamic in vivo animal research, increasing our knowledge of radiopharmaceutical biodistribution, improving quantitation and permitting early selection of therapeutic radiopharmaceuticals. Table 2 lists some of the most important methodological issues involved in performing accurate dosimetry today.
Table 2.
Methodological issues in performing clinical dosimetry
| - Diagnostic tracer and/or therapeutic activity study |
| - Planar and/or tomographic (SPECT and/or PET) quantification |
| - Dynamic and/or multiple time point activity sampling |
| - Linearity of detector response in low and/or high activity |
| - Correction factors for attenuation, scatter and/or partial volume effects |
| - Nuclear medicine and/or radiological volume and response |
| - Standard (MIRD,...) and/or simulative (Monte Carlo,...) modelling |
| - Tissue heterogeneity and/or spatial resolution limits |
| - Treatment of minimal residual disease and/or partial volume effects |
| - Disease-induced and/or therapy-induced changes in parameters |
| - Macro- and/or microdosimetry techniques |
| - Animal and/or human dosimetry data |
Radiobiology is a science in itself. Nevertheless, up to now very little consideration has been given to the effects of radionuclide therapy at the cellular and molecular level [106]. Rather, extrapolations have been made from EBRT, despite the fundamental differences in radiation kinetics. The majority of observations in EBRT have been made under the condition of a high dose rate, while clinical radionuclide therapy entails a decreasing, low dose rate. The effect of fractionated EBRT is primarily influenced by the 4 R’s of radiobiology: repair of DNA damage, repopulation of tissues, re-oxygenation of tumour and redistribution in the cell cycle. In radionuclide therapy, with its decreasing dose rate, tumour DNA repair takes place simultaneously with sublethal damage. Bystander effects, i.e. radiation-like effects in unhit cells, may be of significance in low-dose, low dose rate radiotherapy [2]. Furthermore, it is becoming increasingly apparent that the physical paradigm of direct cell killing by double-strand DNA breaks is insufficient. Non-DNA targets, such as cell membrane or RNA, may also be critical to target cell death or dysfunction. Moreover, new molecular-targeted oncology treatments may not produce direct cell death, but rather alter biochemical pathways or cellular homeostasis, that may interact with classical radiation targets or produce new radiation targets [107]. In this paradigm, the concept of radiation dose may need re-definition and the future radiation dose may be determined in terms of the biological and functional changes produced and observed, such as by blood markers and by PET, SPECT and/or MRI. Biologically effective dose (BED) is a concept which has been successfully applied to radionuclide therapy through the landmarking studies of Barone et al. [59] using 86Y-labelled DOTATOC and kidney toxicity. BED is the product of the total physical dose multiplied by the “relative effectiveness”, which takes into account radiobiological parameters such as dose rate, radionuclide decay and tumour cell repair time, and allows direct quantitative comparison with EBRT. It should be noted that late-responding normal tissues and slow-growing tumours allow easier modelling than early-responding normal tissues and fast-growing tumours because of repopulation during treatment in the latter. Nevertheless, this may be regarded as a major development, stimulating further research [108] aimed towards the creation of a firm fundamental basis for radionuclide radiotoxicity and radiodosimetry. In future, it looks as if we shall no longer be looking at a “Holy Gray”, but rather at the worldly “BEGray”.
In conclusion, recent developments in molecular medicine, PET/CT and SPECT/CT cameras and radiobiology offer major scientific and clinical opportunities in radionuclide therapy dosimetry. However, only prospective, randomised trials with adequate methodology can provide the evidence that applied clinical dosimetry results in better patient outcome than is achieved with fixed activity dosing methods.
References
- 1.Flux G, Bardies M, Monsieurs M, Savolainen S, Strand S-E, Lassmann M. The impact of PET and SPECT on dosimetry for targeted radionuclide therapy. Z Med Phys. 2006;16:47–59. doi: 10.1078/0939-3889-00291. [DOI] [PubMed] [Google Scholar]
- 2.Boyd M, Ross SC, Dorrens J, Fullerton NE, Tan KW, Zalutsky MR, et al. Radiation-induced biological bystander effect elicited in vitro by targeted radiopharmaceuticals labelled with α-, β-, and Auger electron-emitting radionuclides. J Nucl Med. 2006;47:1007–1015. [PubMed] [Google Scholar]
- 3.Dale R, Carabe-Fernandez A. The radiobiology of conventional radiotherapy and its application to radionuclide therapy. Cancer Biother Radiopharm. 2005;20:47–51. doi: 10.1089/cbr.2005.20.47. [DOI] [PubMed] [Google Scholar]
- 4.ICRU Report 67. Dose specifications in nuclear medicine. ICRU 2002.
- 5.Siegel JA, Thomas SR, Stubbs JB, Stabin MG, Hays MT, Koral KF, et al. MIRD pamphlet no. 16: Techniques for quantitative radiopharmaceutical biodistribution data acquisition and analysis for use in human radiation dose estimates. J Nucl Med. 1999;40:37S–61S. [PubMed] [Google Scholar]
- 6.Stabin MG. MIRDOSE: personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 1996;37:538–546. [PubMed] [Google Scholar]
- 7.Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 2005;46:1023–1027. [PubMed] [Google Scholar]
- 8.Leslie WD, Ward L, Salamon EA, Ludwig S, Rowe RC, Cowden EA. A randomized comparison of radioiodine doses in Graves’ hyperthyroidism. J Clin Endocrinol Metab. 2003;88:978–983. doi: 10.1210/jc.2002-020805. [DOI] [PubMed] [Google Scholar]
- 9.Matthay KK, Tan JC, Villablanca JG, Yanik GA, Veatch J, Franc B, et al. Phase I dose escalation of iodine-131-metaiodobenzylguanidine with myeloablative chemotherapy and autologous stem-cell transplantation in refractory neuroblastoma: a new approaches to Neuroblastoma Therapy Consortium Study. J Clin Oncol. 2006;24:500–506. doi: 10.1200/JCO.2005.03.6400. [DOI] [PubMed] [Google Scholar]
- 10.Wiseman GA, White CA, Sparks RB, Erwin WD, Podoloff DA, Lamonica D, et al. Biodistribution and dosimetry results from a phase III prospectively randomized controlled trial of Zevalin radioimmunotherapy for low-grade, follicular, or transformed B-cell non-Hodgkin’s lymphoma. Crit Rev Oncol Hematol. 2001;39:181–194. doi: 10.1016/S1040-8428(01)00107-X. [DOI] [PubMed] [Google Scholar]
- 11.Schlumberger MJ. Papillary and follicular thyroid carcinoma. N Engl J Med. 1998;338:297–306. doi: 10.1056/NEJM199801293380506. [DOI] [PubMed] [Google Scholar]
- 12.Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994;97:418–428. doi: 10.1016/0002-9343(94)90321-2. [DOI] [PubMed] [Google Scholar]
- 13.Hänscheid H, Lassmann M, Luster M, Thomas SR, Pacini F, Ceccarelli C, et al. Iodine biokinetics and dosimetry in radioiodine therapy of thyroid cancer: procedures and results of a prospective international controlled study of ablation after rhTSH or hormone withdrawal. J Nucl Med. 2006;47:648–654. [PubMed] [Google Scholar]
- 14.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006;16:109–142. doi: 10.1089/thy.2006.16.109. [DOI] [PubMed] [Google Scholar]
- 15.Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JWA, Wiersinga W. European consensus for the management of patients with differentiated thyroid cancer of the follicular epithelium. Eur J Endocrinol. 2006;154:787–803. doi: 10.1530/eje.1.02158. [DOI] [PubMed] [Google Scholar]
- 16.Maxon HR, Thomas SR, Hertzbert VS, Kereiakes JG, Chen IW, Sperling MI, et al. Relation between effective radiation dose and outcome of radioiodine therapy for thyroid cancer. N Engl J Med. 1983;309:937–941. doi: 10.1056/NEJM198310203091601. [DOI] [PubMed] [Google Scholar]
- 17.Maxon HR, Englaro EE, Thomas SR, Hertzberg VS, Hinnefeld JD, Chen LS, et al. Radioiodine-131 therapy for well-differentiated thyroid cancer—a quantitative radiation dosimetric approach: outcome and validation in 85 patients. J Nucl Med. 1992;33:1132–1136. [PubMed] [Google Scholar]
- 18.de Keizer B, Brans B, Hoekstra A, Zelissen PM, Koppeschaar HPF, Lips CJ, et al. Tumour dosimetry and response in patients with metastatic differentiated thyroid cancer using recombinant human thyrotropin before radioiodine therapy. Eur J Nucl Med Mol Imaging. 2003;30:367–373. doi: 10.1007/s00259-002-1076-y. [DOI] [PubMed] [Google Scholar]
- 19.Benua RS, Cicale NR, Sonenberg M, Rawson RW. The relation of radioiodine dosimetry to results and complications in treatment of metastatic thyroid cancer. Am J Roentgenol Radium Ther Nucl Med. 1962;87:171–182. [PubMed] [Google Scholar]
- 20.de Keizer B, Hoekstra A, Konijnenberg MW, de Vos F, Lambert B, van Rijk PP, et al. Bone marrow dosimetry and safety of high 131I activities given after recombinant human thyroid-stimulating hormone to treat metastatic differentiated thyroid cancer. J Nucl Med. 2004;45:1549–1554. [PubMed] [Google Scholar]
- 21.Luster M, Sherman SI, Skarulis MC, Reynolds JR, Lassmann M, Hanscheid H, et al. Comparison of radioiodine biokinetics following the administration of recombinant human thyroid stimulating hormone (rhTSH) and after thyroid hormone withdrawal in thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2003;30:1371–1377. doi: 10.1007/s00259-003-1230-1. [DOI] [PubMed] [Google Scholar]
- 22.Dorn R, Kopp J, Vogt H, Heidenreich P, Carroll RG, Gulec SA. Dosimetry-guided radioactive iodine treatment in patients with metastatic differentiated thyroid cancer: largest safe dose using a risk-adapted approach. J Nucl Med. 2003;44:451–456. [PubMed] [Google Scholar]
- 23.Hurley JR, Becker DV. The use of radioiodine in the management of thyroid cancer. In: Freeman LM, Weissmann HS, editors. Nuclear medicine annual. New York: Raven Press; 1983. p. 329. [Google Scholar]
- 24.Freudenberg LS, Antoch G, Jentzen W, Pink R, Knust J, Gorges R, et al. Value of 124I-PET/CT in staging of patients with differentiated thyroid cancer. Eur Radiol. 2004;14:2092–2098. doi: 10.1007/s00330-004-2350-0. [DOI] [PubMed] [Google Scholar]
- 25.Sgouros G, Kolbert KS, Sheikh A, Pentlow KS, Mun EF, Barth A, et al. Patient-specific dosimetry for 131I thyroid cancer therapy using 124I PET and 3-dimensional-internal dosimetry (3D-ID) software. J Nucl Med. 2004;45:1366–1372. [PubMed] [Google Scholar]
- 26.Hoefnagel CA, Voute PA, de Kraker J, Marcuse HR. Radionuclide diagnosis and therapy of neural crest tumors using iodine-131 metaiodobenzylguanidine. J Nucl Med. 1987;28:308–314. [PubMed] [Google Scholar]
- 27.Hoefnagel CA, De Kraker J, Valdes Olmos RA, Voute P. [131I]MIBG as a first-line treatment in high-risk neuroblastoma patients. Nucl Med Commun. 1994;15:712–717. doi: 10.1097/00006231-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Meller S. Targeted radiotherapy for neuroblastoma. Arch Dis Child. 1997;77:389–391. doi: 10.1136/adc.77.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gaze MN, Chang YC, Flux GD, Mairs RJ, Saran FH, Meller ST. Feasibility of dosimetry-based high-dose 131I-meta-iodobenzylguanidine with topotecan as a radiosensitizer in children with metastatic neuroblastoma. Cancer Biother Radiopharm. 2005;20:195–199. doi: 10.1089/cbr.2005.20.195. [DOI] [PubMed] [Google Scholar]
- 30.McCluskey AG, Boyd M, Ross SC, Cosimo E, Clark AM, Angerson WJ, et al. [131I] meta-iodobenzylguanidine and topotecan combination treatment of tumors expressing the noradrenaline transporter. Clin Cancer Res. 2005;11:7929–7937. doi: 10.1158/1078-0432.CCR-05-0982. [DOI] [PubMed] [Google Scholar]
- 31.De Kraker J, Hoefnagel CA, Caron H, Valdes Olmos RA, Zsiros J, Heij HA, et al. First-line targeted radiotherapy, a new concept in the treatment of advanced stage neuroblastoma. Eur J Cancer. 1995;31A:600–602. doi: 10.1016/0959-8049(95)00063-O. [DOI] [PubMed] [Google Scholar]
- 32.Lashford LS, Lewis IJ, Fielding SL, Flower MA, Meller ST, Kemshead JT, et al. Phase I/II study of iodine-131 metaiodobenzylguanidine in chemoresistant neuroblastoma: a United Kingdom Children’s Cancer Study Group investigation. J Clin Oncol. 1992;10:1889–1896. doi: 10.1200/JCO.1992.10.12.1889. [DOI] [PubMed] [Google Scholar]
- 33.Monsieurs M, Brans B, Bacher K, Dierckx R, Thierens H. Patient dosimetry for 131I-MIBG therapy for neuroendocrine tumours based on 123I-MIBG scans. Eur J Nucl Med Mol Imaging. 2002;29:1581–1587. doi: 10.1007/s00259-002-0973-4. [DOI] [PubMed] [Google Scholar]
- 34.Tristam M, Alaamer AS, Fleming JS, Lewington VJ, Zivanovic MA. Iodine-131-metaiodobenzylguanidine dosimetry in cancer therapy: risk versus benefit. J Nucl Med. 1996;37:1058–1063. [PubMed] [Google Scholar]
- 35.Matthay KK, Panina C, Huberty J, Price D, Glidden DV, Tang HR, et al. Correlation of tumor and whole-body dosimetry with tumor response and toxicity in refractory neuroblastoma treated with 131I-MIBG. J Nucl Med. 2001;42:1713–1721. [PubMed] [Google Scholar]
- 36.Flux GD, Guy MJ, Beddows R, Pryor M, Flower MA. Estimation and implications of random errors in whole-body dosimetry for targeted radionuclide therapy. Phys Med Biol. 2002;47:3211–3223. doi: 10.1088/0031-9155/47/17/311. [DOI] [PubMed] [Google Scholar]
- 37.Sisson JC, Shapiro B, Hutchinson RJ, Carey JE, Zasadny KR, Zempel SA, et al. Predictors of toxicity in treating patients with neuroblastoma by radiolabeled metaiodobenzylguanidine. Eur J Nucl Med. 1994;21:46–52. doi: 10.1007/BF00182305. [DOI] [PubMed] [Google Scholar]
- 38.DuBois SG, Messina J, Maris JM, Huberty J, Glidden DV, Veatch J, et al. Haematological toxicity of high-dose iodine-131-metaiodobenzylguanidine therapy for advanced neuroblastoma. J Clin Oncol. 2004;22:2452–2460. doi: 10.1200/JCO.2004.08.058. [DOI] [PubMed] [Google Scholar]
- 39.Loh K-C, Fitgerald PA, Matthay KK, Yeo PPB, Price DC. The treatment of malignant pheochromocytoma with iodine-131 metaiodobenzylguanidine (131I-MIBG): a comprehensive review of 116 reported patients. J Endocrinol Invest. 1997;20:648–658. doi: 10.1007/BF03348026. [DOI] [PubMed] [Google Scholar]
- 40.Rose B, Matthay KK, Price D, Huberty J, Klencke B, Norton JA, et al. High-dose 131I-mIBG therapy for 12 patients with malignant phaeochromocytoma. Cancer. 2003;98:239–248. doi: 10.1002/cncr.11518. [DOI] [PubMed] [Google Scholar]
- 41.de Jong M, Valkema R, Jamar F, Kvols LK, Kwekkeboom DJ, Breeman WA, et al. Somatostatin receptor-targeted radionuclide therapy of tumors: preclinical and clinical findings. Semin Nucl Med. 2002;32:133–140. doi: 10.1053/snuc.2002.31027. [DOI] [PubMed] [Google Scholar]
- 42.Waldherr C, Pless M, Maecke HR, Schumacher T, Crazzolara A, Nitzsche EU, et al. Tumor response and clinical benefit in neuroendocrine tumors after 7.4 GBq 90Y-DOTATOC. J Nucl Med. 2002;43:610–616. [PubMed] [Google Scholar]
- 43.Valkema R, de Jong M, Bakker WH, Breeman WA, Kooij PP, Lugtenburg PJ, et al. Phase I study of peptide receptor radionuclide therapy with [In-DTPA]octreotide: the Rotterdam experience. Semin Nucl Med. 2002;32:110–122. doi: 10.1053/snuc/2002.31025. [DOI] [PubMed] [Google Scholar]
- 44.Bodei L, Cremonesi M, Grana C, Rocca P, Bartolomei M, Chinol M, et al. Receptor radionuclide therapy with 90Y-[DOTA]0-Tyr3-octreotide (90Y-DOTATOC) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31:1038–1046. doi: 10.1007/s00259-004-1571-4. [DOI] [PubMed] [Google Scholar]
- 45.Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders RA, et al. Radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol. 2005;23:2754–2762. doi: 10.1200/JCO.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 46.Virgolini I, Britton K, Buscombe J, Moncayo R, Paganelli G, Riva P. In- and Y-DOTA-lanreotide: results and implications of the MAURITIUS trial. Semin Nucl Med. 2002;32:148–155. doi: 10.1053/snuc.2002.31565. [DOI] [PubMed] [Google Scholar]
- 47.Cremonesi M, Ferrari M, Zoboli S, Chinol M, Stabin MG, Orsi F, et al. Biokinetics and dosimetry in patients administered with 111In-DOTA-Tyr3-octreotide: implications for internal radiotherapy with 90Y-DOTATOC. Eur J Nucl Med. 1999;26:877–886. doi: 10.1007/s002590050462. [DOI] [PubMed] [Google Scholar]
- 48.Walrand S, Jamar F, Mathieu I, De Camps J, Lonneux M, Sibomana M, et al. Quantitation in PET using isotopes emitting prompt single gammas: application to yttrium-86. Eur J Nucl Med Mol Imaging. 2003;30:354–361. doi: 10.1007/s00259-002-1068-y. [DOI] [PubMed] [Google Scholar]
- 49.Reubi JC, Schar JC, Waser B, Wenger S, Heppeler A, Schmitt JS, et al. Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med. 2000;27:273–282. doi: 10.1007/s002590050034. [DOI] [PubMed] [Google Scholar]
- 50.Kwekkeboom DJ, Bakker WH, Kooij PP, Konijnenberg MW, Srinivasan A, Erion JL, et al. [177Lu-DOTA0Tyr3]octreotate: comparison with [111In-DTPA0]octreotide in patients. Eur J Nucl Med. 2001;28:1319–1325. doi: 10.1007/s002590100574. [DOI] [PubMed] [Google Scholar]
- 51.Jamar F, Barone R, Mathieu I, Walrand S, Labar D, Carlier P, et al. 86Y-DOTA0)-D-Phe1-Tyr3-octreotide (SMT487)—a phase 1 clinical study: pharmacokinetics, biodistribution and renal protective effect of different regimens of amino acid co-infusion. Eur J Nucl Med Mol Imaging. 2003;30:510–518. doi: 10.1007/s00259-003-1117-1. [DOI] [PubMed] [Google Scholar]
- 52.Cassady JR. Clinical radiation nephropathy. Int J Radiat Oncol Biol Phys. 1995;31:1249–1256. doi: 10.1016/0360-3016(94)00428-N. [DOI] [PubMed] [Google Scholar]
- 53.Cybulla M, Weiner SM, Otte A. End-stage renal disease after treatment with 90Y-DOTATOC. Eur J Nucl Med. 2001;28:1552–1554. doi: 10.1007/s002590100599. [DOI] [PubMed] [Google Scholar]
- 54.Otte A, Herrmann R, Heppeler A, Behe M, Jermann E, Powell P, et al. Yttrium-90 DOTATOC: first clinical results. Eur J Nucl Med. 1999;26:1439–1447. doi: 10.1007/s002590050476. [DOI] [PubMed] [Google Scholar]
- 55.Bernard BF, Krenning EP, Breeman WA, Rolleman EJ, Bakker WH, Visser TJ, et al. D-lysine reduction of indium-111 octreotide and yttrium-90 octreotide renal uptake. J Nucl Med. 1997;38:1929–1933. [PubMed] [Google Scholar]
- 56.de Jong M, Krenning EP. New advances in peptide receptor radionuclide therapy. J Nucl Med. 2002;43:617–620. [PubMed] [Google Scholar]
- 57.Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with 90Y-DOTA0,Tyr3-octreotide and 177Lu-DOTA0, Tyr3-octreotate. J Nucl Med. 2005;46:83S–91S. [PubMed] [Google Scholar]
- 58.Barone R, Borson-Chazot F, Valkema R, Walrand S, Chauvin F, Gogou L, et al. Patient-specific dosimetry in predicting renal toxicity with 90Y-DOTATOC: relevance of kidney volume and dose rate in finding a dose-effect relationship. J Nucl Med. 2005;46:99S–106S. [PubMed] [Google Scholar]
- 59.Konijnenberg MW, Bijster M, Krenning EP, De Jong M. A stylized computational model of the rat for organ dosimetry in support of preclinical evaluations of peptide receptor radionuclide therapy with 90Y, 111In, or 177Lu. J Nucl Med. 2004;45:1260–1269. [PubMed] [Google Scholar]
- 60.Kwekkeboom DJ, Mueller-Brand J, Paganelli G, Anthony LB, Pauwels S, Kvols LK, et al. Overview of results of peptide receptor radionuclide therapy with 3 radiolabeled somatostatin analogs. J Nucl Med. 2005;46:62S–66S. [PubMed] [Google Scholar]
- 61.Stabin MG, Eckerman KF, Bolch WE, Bouchet LG, Patton PW. Evolution and status of bone and marrow dose models. Cancer Biother Radiopharm. 2002;17:427–433. doi: 10.1089/108497802760363213. [DOI] [PubMed] [Google Scholar]
- 62.Sgouros G. Dosimetry of internal emitters. J Nucl Med. 2005;46:18S–27S. [PubMed] [Google Scholar]
- 63.Pauwels S, Barone R, Walrand S, Borson-Chazot F, Valkema R, Kvols LK, et al. Practical dosimetry of peptide receptor radionuclide therapy with 90Y-labeled somatostatin analogs. J Nucl Med. 2005;46:92S–98S. [PubMed] [Google Scholar]
- 64.de Jong M, Breeman WA, Valkema R, Bernard BF, Krenning EP. Combination radionuclide therapy using 177Lu- and 90Y-labeled somatostatin analogs. J Nucl Med. 2005;46:13S–17S. [PubMed] [Google Scholar]
- 65.Jhanwar YS, Divgi C. Current status of ttherapy of solid tumours. J Nucl Med. 2005;46:141S–150S. [PubMed] [Google Scholar]
- 66.Sgouros G, Stabin M, Erdi Y, Akabani G, Kwok C, Brill AB, et al. Red marrow dosimetry for radiolabeled antibodies that bind to marrow, bone, or blood components. Med Phys. 2000;27:2150–2164. doi: 10.1118/1.1288393. [DOI] [PubMed] [Google Scholar]
- 67.Shen S, DeNardo GL, Sgouros G, O’Donnell RT, DeNardo SJ. Practical determination of patient-specific marrow dose using radioactivity concentration in blood and body. J Nucl Med. 1999;40:2102–2106. [PubMed] [Google Scholar]
- 68.Wessels BW, Bolch WE, Bouchet LG, Breitz HB, Denardo GL, Meredith RF, et al. Bone marrow dosimetry using blood-based models for radiolabeled antibody therapy: a multi-institutional comparison. J Nucl Med. 2004;45:1725–1733. [PubMed] [Google Scholar]
- 69.Divgi CR, Bander NH, Scott AM, O’Donoghue JA, Sgouros G, Welt S, et al. Phase I/II radioimmunotherapy trial with iodine-131-labeled monoclonal antibody G250 in metastatic renal cell carcinoma. Clin Cancer Res. 1998;4:2729–2739. [PubMed] [Google Scholar]
- 70.O’Donoghue JA, Baidoo N, Deland D, Welt S, Divgi CR, Sgouros G. Hematologic toxicity in radioimmunotherapy: dose-response relationships for I-131 labeled antibody therapy. Cancer Biother Radiopharm. 2002;17:435–443. doi: 10.1089/108497802760363222. [DOI] [PubMed] [Google Scholar]
- 71.Brouwers AH, Buijs WC, Mulders PF, de Mulder PH, van den Broek WJ, Mala C, et al. Radioimmunotherapy with [131I]cG250 in patients with metastasized renal cell cancer: dosimetric analysis and immunologic response. Clin Cancer Res. 2005;11:7178s–7186s. doi: 10.1158/1078-0432.CCR-1004-0010. [DOI] [PubMed] [Google Scholar]
- 72.Juweid ME, Zhang CH, Blumenthal RD, Hajjar G, Sharkey RM, Goldenberg DM. Prediction of hematologic toxicity after radioimmunotherapy with 131I-labeled anticarcinoembryonic antigen monoclonal antibodies. J Nucl Med. 1999;40:1609–1616. [PubMed] [Google Scholar]
- 73.Nicholson S, Gooden CS, Hird V, Maraveyas A, Mason P, Lambert HE, et al. Radioimmunotherapy after chemotherapy compared to chemotherapy alone in the treatment of advanced ovarian cancer: a matched analysis. Oncol Rep. 1998;5:223–226. doi: 10.3892/or.5.1.223. [DOI] [PubMed] [Google Scholar]
- 74.Verheijen RH, Massuger LF, Benigno BB, Epenetos AA, Lopes A, Soper JT, et al. Phase III trial of intraperitoneal therapy with yttrium-90-labeled HMFG1 murine monoclonal antibody in patients with epithelial ovarian cancer after a surgically defined complete remission. J Clin Oncol. 2006;24:571–578. doi: 10.1200/JCO.2005.02.5973. [DOI] [PubMed] [Google Scholar]
- 75.Boerman OC, van Schaijk FG, Oyen WJ, Corstens FH. Pretargeted radioimmunotherapy of cancer: progress step by step. J Nucl Med. 2003;44:400–411. [PubMed] [Google Scholar]
- 76.Goldenberg DM, Sharkey RM, Paganelli G, Barbet J, Chatal JF. Antibody pretargeting advances cancer radioimmunodetection and radioimmunotherapy. J Clin Oncol. 2006;24:823–834. doi: 10.1200/JCO.2005.03.8471. [DOI] [PubMed] [Google Scholar]
- 77.Shen S, Forero A, LoBuglio AF, Breitz H, Khazaeli MB, Fisher DR, et al. Patient-specific dosimetry of pretargeted radioimmunotherapy using CC49 fusion protein in patients with gastrointestinal malignancies. J Nucl Med. 2005;46:642–651. [PubMed] [Google Scholar]
- 78.Kraeber-Bodere F, Faivre-Chauvet A, Ferrer L, Vuillez JP, Brard PY, Rousseau C, et al. Pharmacokinetics and dosimetry studies for optimization of anti-carcinoembryonic antigen x anti-hapten bispecific antibody-mediated pretargeting of iodine-131-labeled hapten in a phase I radioimmunotherapy trial. Clin Cancer Res. 2003;9:3973S–3981S. [PubMed] [Google Scholar]
- 79.Cremonesi M, Ferrari M, Chinol M, Stabin MG, Grana C, Prisco G, et al. Three-step radioimmunotherapy with yttrium-90 biotin: dosimetry and pharmacokinetics in cancer patients. Eur J Nucl Med. 1999;26:110–120. doi: 10.1007/s002590050366. [DOI] [PubMed] [Google Scholar]
- 80.Witzig TE, Gordon LI, Cabanillas F, Czuczman MS, Emmanouilides C, Joyce R, et al. Randomized controlled trial of yttrium-90-labeled ibritumomab tiuxetan radioimmunotherapy versus rituximab immunotherapy for patients with relapsed or refractory low-grade, follicular, or transformed B-cell non-Hodgkin’s lymphoma. J Clin Oncol. 2002;20:2453–2463. doi: 10.1200/JCO.2002.11.076. [DOI] [PubMed] [Google Scholar]
- 81.Kaminski MS, Zelenetz AD, Press OW, Saleh M, Leonard J, Fehrenbacher L, et al. Pivotal study of iodine I 131 tositumomab for chemotherapy-refractory low-grade or transformed low-grade B-cell non-Hodgkin’s lymphomas. J Clin Oncol. 2001;19:3918–3928. doi: 10.1200/JCO.2001.19.19.3918. [DOI] [PubMed] [Google Scholar]
- 82.Knox SJ, Goris ML, Trisler K, Negrin R, Davis T, Liles TM, et al. Yttrium-90-labeled anti-CD20 monoclonal antibody therapy of recurrent B-cell lymphoma. Clin Cancer Res. 1996;2:457–470. [PubMed] [Google Scholar]
- 83.Press OW, Eary JF, Appelbaum FR, Martin PJ, Badger CC, Nelp WB, et al. Radiolabeled-antibody therapy of B-cell lymphoma with autologous bone marrow support. N Engl J Med. 1993;329:1219–1224. doi: 10.1056/NEJM199310213291702. [DOI] [PubMed] [Google Scholar]
- 84.Blumenthal RD, Fand I, Sharkey RM, Boerman OC, Kashi R, Goldenberg DM. The effect of antibody protein dose on the uniformity of tumor distribution of radioantibodies: an autoradiographic study. Cancer Immunol Immunother. 1991;33:351–358. doi: 10.1007/BF01741594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Illidge TM, Cragg MS, McBride HM, French RR, Glennie MJ. The importance of antibody-specificity in determining successful radioimmunotherapy of B-cell lymphoma. Blood. 1999;94:233–243. [PubMed] [Google Scholar]
- 86.Linden O, Hindorf C, Cavallin-Stahl E, Wegener WA, Goldenberg DM, Horne H, et al. Dose-fractionated radioimmunotherapy in non-Hodgkin’s lymphoma using DOTA-conjugated, 90Y-radiolabeled, humanized anti-CD22 monoclonal antibody, epratuzumab. Clin Cancer Res. 2005;11:5215–5222. doi: 10.1158/1078-0432.CCR-05-0172. [DOI] [PubMed] [Google Scholar]
- 87.Wahl RL, Kroll S, Zasadny KR. Patient-specific whole-body dosimetry: principles and a simplified method for clinical implementation. J Nucl Med. 1998;39:14S–20S. [PubMed] [Google Scholar]
- 88.Wahl RL, Zasadny KR, MacFarlane D, Francis IR, Ross CW, Estes J, et al. Iodine-131 anti-B1 antibody for B-cell lymphoma: an update on the Michigan Phase I experience. J Nucl Med. 1998;39:21S–27S. [PubMed] [Google Scholar]
- 89.Hindorf C, Linden O, Tennvall J, Wingardh K, Strand SE. Evaluation of methods for red marrow dosimetry based on patients undergoing radioimmunotherapy. Acta Oncol. 2005;44:579–588. doi: 10.1080/02841860500244294. [DOI] [PubMed] [Google Scholar]
- 90.Sgouros G. Bone marrow dosimetry for radioimmunotherapy: theoretical considerations. J Nucl Med. 1993;34:689–694. [PubMed] [Google Scholar]
- 91.Siegel JA, Wessels BW, Watson EE, Stabin MG, Vriesendorp HM, Bradley EW, et al. Bone marrow dosimetry and toxicity for radioimmunotherapy. Antibody Immunoconj Radiopharm. 1990;3:213–233. [Google Scholar]
- 92.Hindorf C, Linden O, Tennvall J, Wingardh K, Strand SE. Time dependence of the activity concentration ratio of red marrow to blood and implications for red marrow dosimetry. Cancer. 2002;94:1235–1239. doi: 10.1002/cncr.10291. [DOI] [PubMed] [Google Scholar]
- 93.Zanzonico P, Sgouros G. Predicting myelotoxicity in radioimmunotherapy: what does dosimetry contribute? J Nucl Med. 1997;38:1753–1754. [PubMed] [Google Scholar]
- 94.Hindorf C, Linden O, Stenberg L, Tennvall J, Strand SE. Change in tumor-absorbed dose due to decrease in mass during fractionated radioimmunotherapy in lymphoma patients. Clin Cancer Res. 2003;9:4003S–4006S. [PubMed] [Google Scholar]
- 95.Liu SY, Eary JF, Petersdorf SH, Martin PJ, Maloney DG, Appelbaum FR, et al. Follow-up of relapsed B-cell lymphoma patients treated with iodine-131-labeled anti-CD20 antibody and autologous stem-cell rescue. J Clin Oncol. 1998;16:3270–3278. doi: 10.1200/JCO.1998.16.10.3270. [DOI] [PubMed] [Google Scholar]
- 96.Scheidhauer K, Wolf I, Baumgartl HJ, Von Schilling C, Schmidt B, Reidel G, et al. Biodistribution and kinetics of 131I-labeled anti-CD20 MAB IDEC-C2B8 (rituximab) in relapsed non-Hodgkin’s lymphoma. Eur J Nucl Med Mol Imaging. 2002;29:1276–1282. doi: 10.1007/s00259-002-0820-7. [DOI] [PubMed] [Google Scholar]
- 97.Nademanee A, Forman S, Molina A, Fung H, Smith D, Dagis A, et al. A phase 1/2 trial of high-dose yttrium-90-ibritumomab tiuxetan in combination with high-dose etoposide and cyclophosphamide followed by autologous stem cell transplantation in patients with poor-risk or relapsed non-Hodgkin lymphoma. Blood. 2005;106:2896–2902. doi: 10.1182/blood-2005-03-1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ochakovskaya R, Osorio L, Goldenberg DM, Mattes MJ. Therapy of disseminated B-cell lymphoma xenografts in severe combined immunodeficient mice with an anti-CD74 antibody conjugated with (111)indium, (67)gallium, or (90)yttrium. Clin Cancer Res. 2001;7:1505–1510. [PubMed] [Google Scholar]
- 99.Behr TM, Sgouros G, Vougiokas V, Memtsoudis S, Gratz S, Schmidberger H, et al. Therapeutic efficacy and dose-limiting toxicity of Auger-electron vs. beta emitters in radioimmunotherapy with internalizing antibodies: evaluation of 125I- vs. 131I-labeled CO17-1A in a human colorectal cancer model. Int J Cancer. 1998;76:738–748. doi: 10.1002/(SICI)1097-0215(19980529)76:5<738::AID-IJC20>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 100.Press OW, Eary JF, Appelbaum FR, Martin PJ, Nelp WB, Glenn S, et al. Phase II trial of 131I-B1 (anti-CD20) antibody therapy with autologous stem cell transplantation for relapsed B cell lymphomas. Lancet. 1995;346:336–340. doi: 10.1016/S0140-6736(95)92225-3. [DOI] [PubMed] [Google Scholar]
- 101.Kaminski MS, Zasadny KR, Francis IR, Fenner MC, Ross CW, Milik AW, et al. Iodine-131-anti-B1 radioimmunotherapy for B-cell lymphoma. J Clin Oncol. 1996;14:1974–1981. doi: 10.1200/JCO.1996.14.7.1974. [DOI] [PubMed] [Google Scholar]
- 102.O’Donoghue J. Dosimetric principles of targeted radiotherapy. In: Abrams P, Fritzberg A, editors. Radioimmunotherapy of cancer. New York: Marcel Dekker; 2000. pp. 1–20. [Google Scholar]
- 103.DeNardo GL, Juweid ME, White CA, Wiseman GA, DeNardo SJ. Role of radiation dosimetry in radioimmunotherapy planning and treatment dosing. Critical Rev Oncol Hematol. 2001;39:203. doi: 10.1016/S1040-8428(01)00109-3. [DOI] [PubMed] [Google Scholar]
- 104.Gurney H. Developing a new framework for dose calculation. J Clin Oncol. 2006;24:1489–1490. doi: 10.1200/JCO.2005.05.1607. [DOI] [PubMed] [Google Scholar]
- 105.Ott RJ. Imaging technologies for radionuclide dosimetry. Phys Med Biol. 1996;41:1885–1894. doi: 10.1088/0031-9155/41/10/002. [DOI] [PubMed] [Google Scholar]
- 106.Pouget J-P, Mather SJ. General aspects of the cellular response to low- and high-LET radiation. Eur J Nucl Med. 2001;28:541–561. doi: 10.1007/s002590100484. [DOI] [PubMed] [Google Scholar]
- 107.Coleman NC. Linking radiation oncology and imaging through molecular biology (or now that therapy and diagnosis have separated, it’s time to get together again) Radiology. 2003;228:29–35. doi: 10.1148/radiol.2281021567. [DOI] [PubMed] [Google Scholar]
- 108.Carlsson J, Eriksson V, Stenerlow B, Lundqvist H. Requirements regarding dose rate and exposure time for killing of tumour cells in beta particle radionuclide therapy. Eur J Nucl Med Mol Imaging. 2006;33:1185–1195. doi: 10.1007/s00259-006-0109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stabin MG, Kooij PP, Bakker WH, Inoue T, Endo K, Coveney J, et al. Radiation dosimetry for indium-111-pentetreotide. J Nucl Med. 1997;38:1919–1922. [PubMed] [Google Scholar]
- 110.Forster GJ, Engelbach MJ, Brockmann JJ, Reber HJ, Buchholz HG, Macke HR, et al. Preliminary data on biodistribution and dosimetry for therapy planning of somatostatin receptor positive tumours: comparison of 86Y-DOTATOC and 111In-DTPA-octreotide. Eur J Nucl Med. 2001;28:1743–1750. doi: 10.1007/s002590100628. [DOI] [PubMed] [Google Scholar]
- 111.Helisch A, Förster GJ, Reber H, Buchholz HG, Arnold R, Goke B, et al. Pre-therapeutic dosimetry and biodistribution of 86Y-DOTA-Phe1-Tyr3-octreotide versus 111In-pentetreotide in patients with advanced neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31:1386–1392. doi: 10.1007/s00259-004-1561-6. [DOI] [PubMed] [Google Scholar]
- 112.Forrer F, Uusijarvi H, Waldherr C, Cremonesi M, Bernhardt P, Mueller-Brand J, et al. A comparison of 111In-DOTATOC and 111In-DOTATATE: biodistribution and dosimetry in the same patients with metastatic neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31:1257–1262. doi: 10.1007/s00259-004-1553-6. [DOI] [PubMed] [Google Scholar]