Abstract
Little is known about the relation between communication during cancer genetic counseling and outcome. We assessed associations between counselor-counselee communication and counselee satisfaction, cognitions, anxiety, and fulfillment of major needs, corrected for pre-visit levels as appropriate. In total 171 consecutive new counselees, mainly referred for breast or colon cancer, received pre- and post-visit questionnaires assessing needs/fulfillment, knowledge, perceived control (PPC), anxiety (STAI), and satisfaction. Initial visits were videotaped and counselor eye gaze was recorded. Verbal communication was rated by Roter Interaction Analysis System (RIAS). Asking more medical questions was associated with lower satisfaction levels. Receiving more medical information was related to higher correct knowledge scores, higher reported fulfillment of some needs, and unrelated to perceptions of control. Receiving more psychosocial information and longer counselor eye gaze were related to higher anxiety scores. Longer visits were related to higher correct knowledge scores. Providing medical information appears the most powerful communication aspect to increase counselee satisfaction and address needs. More research is needed on how to address adequately (emotional) needs and increase feelings of control.
KEY WORDS: communication, cancer genetic counseling, needs, outcome
INTRODUCTION
A primary goal of cancer genetic counseling is to educate individuals about cancer (recurrence) risk, cancer prevention, and early detection (ASCO, 1996; Biesecker, 2001; Richards, 1999). Initial visits are largely concerned with the exchange of medical information regarding personal and family history of cancer, hereditary cancer, personal and family cancer risk, DNA-testing, and risk management options (Butow & Lobb, 2004). An important motive for counselees to seek counseling is indeed to receive medical information (Collins et al., 2000; Pieterse et al., 2005a; Van Asperen et al., 2002) and receive emotional support or reduce worries (Collins et al., 2000; Pieterse et al., 2005a; Holloway et al., 2004; Van Asperen et al., 2002). Addressing pre-visit needs well was found associated with higher perceptions of control and lower feelings of anxiety after the first visit (Pieterse et al., 2005b).
Central to the process of counseling is counselor-counselee communication, and insight in communication–outcome associations may help achieve improved counselee outcomes. A number of studies have assessed actual communication during genetic counseling (Aalfs et al., 2006; Armstrong et al., 1998; Benkendorf et al., 2001; Kessler & Jacopini, 1982; Michie et al., 2005; Pilnick, 2002; Smith et al., 2000; Van Zuuren et al., 1997; Van Zuuren, 1997) and in cancer genetic counseling in particular (Butow & Lobb, 2004; Ellington et al., 2005; Pieterse et al., 2005c; Richards et al., 1995). Notwithstanding calls for process-outcome research (Biesecker & Peters, 2001; Pilnick & Dingwall, 2001; Wang et al., 2004), including how communication fulfills counselees’ expectations (Meiser & Halliday, 2002), only few included outcome measures (Duric et al., 2003; Lobb et al., 2004, 2005; Michie et al., 1997a). In breast cancer counseling, discussing more aspects of genetic testing was shown to be associated with decreased post-visit anxiety in female clients (Lobb et al., 2004). Anxiety was higher when counselors used more supportive communication. Inquiring about women's agenda did not improve outcomes. Results from this sample showed that counselors differ in their facilitating behaviors and discussion of prophylactic mastectomy (Lobb et al., 2005). Differences in counselor behavior affected counselees’ decrease in depression. Additionally, counselors’ empathy in dyadic interactions was related to lower post-visit depression yet unrelated to counselees’ satisfaction and post-visit anxiety (Duric et al., 2003).
Evidence from studies on doctor-patient communication in other medical fields and oncology in particular, suggests patient satisfaction to be related to doctor information-giving and patient question-asking, and doctor and patient affective behavior (Ong et al., 2000). Clear factual information appears beneficial to patients’ perceptions of control (Rutter et al., 1996). Others did not find a relationship between doctors’ affective behavior and patient satisfaction, recall or psychological adjustment, nor between ratio doctor to patient talk and length of consultation and satisfaction (Butow et al., 1995). In contrast, results in primary care patients suggest that seeing a more dominant doctor lowers satisfaction (Bertakis et al., 1991); and that longer visits (Hall et al., 1988; Mead et al., 2002), doctor eye gaze (Bensing, 1991; reviewed by Hall et al., 1988), and discussion of psychosocial topics (Roter et al., 1997) increase satisfaction. Additionally, information-giving and eye gaze increased patient recall/understanding (Hall et al., 1988).
This study investigated the influence of communication during initial cancer genetic counseling visits on counselee outcomes. We assessed (1) in how far counselor and counselee communication is related to counselees’ satisfaction and post-visit knowledge, perceived control, and anxiety; and (2) in how far counselor communication is related to counselees’ perception of their major pre-visit needs being met. We expected positive associations between counselee-counselors talk on counselee agenda and medical and psychosocial issues, their respective expressions of concern and empathy, and counselor eye gaze, with favorable post-visit outcomes. It was further expected that counselor communication devoted to medical information, signs of empathy, and attention to psychosocial issues, would result in counselees’ informational and emotional needs being better fulfilled. Hypothesized associations are summarized in the first two columns of Tables I and II.
METHODS
Participants
Counselees were recruited from consecutive new counselees aged 18 years or older and being the first in their family to seek cancer genetic counseling, at the Department of Medical Genetics of the University Medical Center Utrecht, the Netherlands, between March 2001 and August 2003.
Counselors included all clinical geneticists, residents in clinical genetics (two of whom were finishing training), and genetic nurses (four finishing training) providing cancer genetic counseling at the clinic during the study period.
Procedure
The current study was approved by the Medical Ethical Committee of the university hospital. The procedure of approaching eligible counselees is described elsewhere (Pieterse et al., 2005a). Respondents were asked to complete an informed consent form and a pre-visit questionnaire assessing socio-demographics, type of cancer for which referred, and family history of cancer in the week before their first consultation. The consultation was videotaped. Recordings showed counselors’ full face and counselees from behind or from the side. A clinical geneticist was also present if a counselor was in training. At the end of the consultation, the counselor handed out the post-visit questionnaire along with a pre-stamped envelope and asked the counselee to complete it within a day and post it to the research institute.
Measures
Information on counselees’ disease status and indication for DNA-testing was collected from their medical file. At the start of the study, counselors’ gender, age, and profession were assessed.
Pre-counseling, counselee needs were assessed using a counselee-centered instrument, the QUOTE-geneca. As described elsewhere (Pieterse et al., 2005a), based on a pilot study amongst another sample of counselees for hereditary cancer, a set of 25 generic items and a set of 19 cancer-specific items were formulated. Generic items refer to what a counselor should do during counseling and specific items refer to receiving explanations on hereditary cancer in particular. Post-counseling, identical items were administered to measure perceived fulfillment of needs. Respondents indicated pre-visit importance (not important, fairly important, important, extremely important) and post-visit fulfillment (too little, not really enough, adequate, largely adequate). Principal Component Analysis (PCA) identified four generic and four cancer-specific needs with satisfactory internal consistencies (Table III). Scores on each need range from 1 to 4 with high scores indicating high importance/fulfillment.
Satisfaction with the counseling visit was assessed using eight items (Appendix A). Scores range from 8 to 80, with high scores indicating high satisfaction. PCA (Kaiser-Meyer-Olkin measure of sampling adequacy = 0.92; Bartlett's test of sphericity: P = 0.000) revealed one component explaining 69.7% of the variance; items loaded 0.64 to 0.93. Internal consistency was high (α = 0.92).
Knowledge about hereditary breast (7 items) or colon (6 items) cancer was assessed using items adapted from Claes et al. (2003) as described elsewhere (Pieterse et al., 2005b). Only counselees visiting for hereditary breast or colon cancer were asked to respond to the corresponding items. Respondents indicated whether each item was correct, incorrect, or if they didn't know. Correct scores range from 0 to 1 with higher scores indicating more correct knowledge.
Perceived control was assessed using the Perceived Personal Control questionnaire (PPC) (Berkenstadt et al., 1999), translated in Dutch using a forward-backward procedure (Smets et al., 2006). Scores range from 0 to 2, high scores indicating high perceived control. Pre- and post-visit internal consistencies were high (αpre = 0.82; αpost = 0.82).
Anxiety was measured with the state version of the State-Trait Anxiety Inventory (STAI; 10 items) (Van der Ploeg et al., 1980). Scores range from 10 to 40, higher scores indicating greater anxiety. Pre- and post-visit internal consistencies were high (αpre = 0.92; αpost = 0.93).
Coding of Videotapes
Four coders rated verbal communication using an adaptation of the Roter Interaction Analysis System (RIAS), a widely used observation system for coding doctor and patient communication (Roter and Larson, 2002). The adaptation is described elsewhere (Pieterse et al., 2005c) and included adding categories to code the exchange of pedigree data, medical information about relatives, communication within the family, and agenda. Within the RIAS, a communication unit or utterance is defined as the smallest speech segment to which a classification may be assigned, i.e. which conveys a single thought or relates to a single item of interest. An utterance may vary in length from a single word to a lengthy sentence.
The main coder coded 54% of all consultations and recoded 10% of her own consultations. The other coders recoded 10% of the main coder's consultations. Reliability coefficients (Pearson r) for categories with mean occurrence greater than 2% (Roter et al., 1991) proved to be adequate. Intra-coder reliability for counselor and counselee categories averaged 0.81 (range, 0.54–0.96) and 0.91 (range, 0.75–0.97), respectively. Inter-coder reliability for counselor and counselee categories averaged 0.78 (range, 0.54–0.98) and 0.83 (range, 0.59–0.97), respectively.
Additionally, counselors’ contribution to the encounter relative to the total count of utterances, as a measure of verbal dominance; eye gaze, as the time the counselor looked directly into the face of the counselee or his/her companion(s); and visit length were coded.
Statistical Analyses
Participants returning both questionnaires, and those returning the pre-visit questionnaire only were compared on socio-demographics, history of cancer, and levels of pre-visit measures using a Chi-square test, a Mann-Whitney test, and a t-test. Descriptive statistics were used to describe pre- to post-visit change in outcome measures.
Frequencies of counselee and counselor utterances were calculated. If two counselors were present, their utterances were added. Utterances of individuals accompanying counselees were not considered as the focus of this paper was on counselee-specific needs. Relevant verbal coding categories were combined on the basis of their content (Appendix B) in line with the hypotheses. As encounters for one counselor could resemble, multilevel regression analysis was used.
Multilevel regression analyses were conducted in two steps. First, counselee (gender, age, education, personal history of cancer, number of first- and second-degree affected relatives, indication for DNA-testing) and counselor background variables (gender, age, profession), and number of counselors present were included in the model. Where two counselees were seen together, data were used for one randomly selected counselee only. If two counselors were present, characteristics of the counselor with the largest amount of utterances were used. The categories ‘clinical geneticist’ and ‘resident’ were aggregated into ‘doctor’ as opposed to ‘nurse’. Only significant background correlates (p < 0.05) were retained.
Second, for research question 1 all counselor and counselee communication variables were included in the model as hypothesized (Table I) and analyses were controlled for pre-visit levels of correct knowledge, PPC, and STAI. For research question 2, all counselor communication variables were included in the model as hypothesized (Table II). Separate analyses were conducted for each need within the subgroup of counselees with pre-visit importance scores higher than 2.5 on the respective needs.
Frequency predictors and duration predictors (visit length, eye gaze) were tested using separate models. Eye gaze was assessed both as length in minutes and relative to total visit length. Predictors at interval level measurement were recoded to standardized z-scores. If 25% or less of the values was missing on the satisfaction, PPC, STAI, and QUOTE-geneca scales, missing values were replaced by the mean. Significance of the regression coefficients was tested using Chi-square tests. Analyses were carried out using SPSS 11.5 and MLwiN 1.10.
Significance of counselee outcome measures was tested two-sided at α = 0.05. In testing the hypotheses presented in Tables I and II, the Bonferroni-Holmes correction was used to control for Type I error. This is an alternative for the Bonferroni correction and aims to keep the overall α under control when a large number of statistical hypotheses are being tested. In this procedure the p-values for the k hypotheses are ordered from the smallest to the largest. Hypotheses corresponding with the ordered p-values are then numbered from 1 to k. If i is the smallest integer from 1 to k, then alternative hypotheses (H1) with a p-value smaller than α/(k−i+1) are being accepted, while H1 hypotheses with a p-value larger than α/(k−i+1) are being rejected (Holland & Copenhaver, 1988). Following this procedure, overall α was kept at 0.05 in testing the hypotheses formulated in Tables I and II. We chose to present all p-values smaller than α = 0.05 in these tables but to discuss only those findings significant after Bonferroni–Holmes correction.
RESULTS
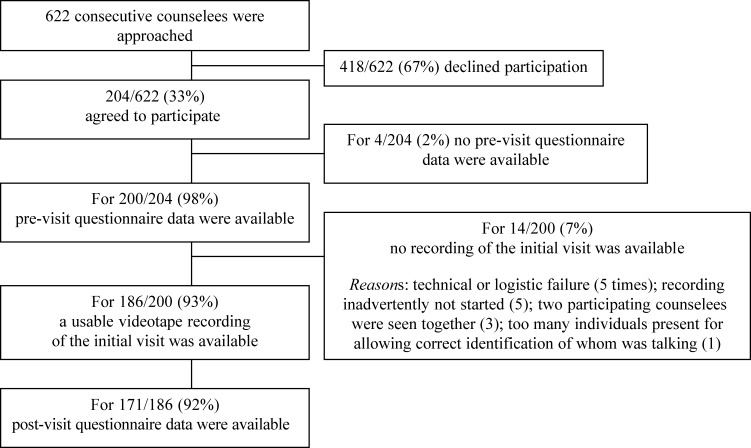
Pre- and post-visit data and a video-recording of the initial visit were available from 171 counselees (Fig. 1). The counselees with a family history of cancer (Table IV) had one to five (MD = 1) first-degree and one to eight (MD = 2) second-degree affected relatives. Participants were, on average, 2.1 years older than decliners (P = 0.022); other background characteristics did not differ (Pieterse et al., 2005a). Participants returning the pre-visit questionnaire only were more likely to be unaffected by cancer (χ2 = 9.76, P = 0.002) than participants returning both questionnaires. They considered it more important to receive explanations on procedural aspects of counseling (t = 2.17, P = 0.031) and heredity of cancer in general (t = 2.00, P = 0.047), and to receive emotional support (t = 2.35, P = 0.020).
Fig. 1.
Details of inclusion of counselees.
Table I.
Resultsa on Hypothesized Positive Associations Between Counselor and Counselee (CE) Communication and Outcome Measures
| Outcome measure | Communication measures | N | Betab | SE | 95% CI | P-value |
|---|---|---|---|---|---|---|
| Satisfaction | Counselor | 164 | ||||
| Empathy | −0.01 | 0.09 | −0.18–0.16 | — | ||
| Medical information | 0.21 | 0.10 | 0.02–0.40 | 0.032 | ||
| Psychosocial information | 0.02 | 0.10 | −0.18–0.21 | — | ||
| Verbal dominance | −0.02 | 0.08 | −0.13–0.17 | — | ||
| Eye gaze | 0.08 | 0.08 | −0.07–0.23 | — | ||
| Counselee | ||||||
| Concern | −0.08 | 0.08 | −0.24–0.08 | — | ||
| Medical questions | −0.31 | 0.08 | −0.47—0.14 | 0.000* | ||
| Counselor and counselee | ||||||
| Discuss CE agenda | −0.14 | 0.09 | −0.31–0.03 | — | ||
| Discuss CE Psychosocial issues | 0.19 | 0.10 | −0.01–0.39 | — | ||
| Visit length | 0.05 | 0.08 | −0.10–0.20 | — | ||
| Correct knowledgec | Counselor | 153 | ||||
| Medical information | 0.22 | 0.08 | 0.07–0.37 | 0.004* | ||
| Eye gaze | 0.17 | 0.07 | 0.03–0.31 | 0.018* | ||
| Counselee | ||||||
| Medical questions | 0.06 | 0.08 | −0.09–0.21 | — | ||
| Counselor and counselee | ||||||
| Visit length | 0.18 | 0.07 | 0.04–0.32 | 0.011* | ||
| Perceived controlc (PPC) | Counselor | 156 | ||||
| Medical information | 0.13 | 0.07 | −0.01–0.28 | — | ||
| Anxietyc (STAI) | Counselor | 160 | ||||
| Empathy | −0.08 | 0.06 | −0.20–0.04 | — | ||
| Medical information | −0.05 | 0.07 | −0.18–0.08 | — | ||
| Psychosocial information | 0.20 | 0.07 | 0.06–0.33 | 0.005* | ||
| Verbal dominance | 0.12 | 0.05 | 0.01–0.22 | 0.033 | ||
| Eye gaze | 0.17 | 0.05 | 0.06–0.28 | 0.002* | ||
| Counselee | ||||||
| Concern | 0.14 | 0.06 | 0.02–0.26 | 0.025 | ||
| Counselor and counselee | ||||||
| Discuss CE Agenda | −0.06 | 0.07 | −0.19–0.07 | — | ||
| Discuss CE psychosocial issues | 0.09 | 0.07 | −0.06–0.24 | — | ||
| Visit length | 0.13 | 0.06 | 0.02–0.24 | 0.018 |
Note. CI= Confidence Interval.
—=P > 0.059.
*Significant after Bonferroni-Holmes correction, overall α = 0.05.
aAll analyses were controlled for counselor and counselee background variables.
bSignificance of predictors was tested using chi-square tests.
cAnalysis was controlled for pre-visit level.
Five clinical geneticists (four female, one male), four residents in clinical genetics (three female, one male) and five genetic nurses (all female) participated. Counselors were aged 29–46 years (M = 38.3; SD = 5.8). Counselors conducted in total 1–30 visits (M = 18.8, MD = 14, SD = 9.2), either alone or as one of two counselors with the largest amount of utterances.
Consultations lasted 44.2 min (SD = 14.1) on average. The counselors conducted 135/171 (79%) visits alone. During 36/171 consultations, a clinical geneticist accompanied a counselor in training. Consultations conducted by 1 versus 2 counselors did not significantly differ in mean number of counselor and counselee utterances per communication category as used in the subsequent analyses, nor in pre- to post-visit change in counselees’ correct knowledge, perceived personal control, and state anxiety, nor in their post-visit satisfaction and reported need fulfillment (data not shown).
In 77/171 (45%) visits, counselees were seen alone. During all other consultations, counselees were accompanied by one (N = 82) or two or more (N = 12) companions. Utterances of counselees comprised an average of 40% of the total communication, compared to 7% for companions.
The counselees’ knowledge and perceived control significantly increased pre- to post-visit, and their anxiety significantly decreased (Table V). The counselees were overall (very) satisfied about the fulfillment of their major pre-visit needs (Table III).
Table II.
Resultsa on Hypothesized Positive Associations Between Counselor Communication and Counselee (CE) Post-Visit Perceptions of the Fulfillment of Major Pre-Visit Needs
| Extent of pre-visit need fulfillment | Counselor communication | N | Betab | SE | 95% CI | P-value |
|---|---|---|---|---|---|---|
| Generic need | ||||||
| Procedural aspects of counseling | Medical information | 130 | 0.09 | 0.09 | -0.08–0.26 | — |
| Sensitive communicationc | Questions CE agenda | 166 | 0.05 | 0.08 | −0.11–0.21 | — |
| Verbal dominancec | 105 | 0.00 | 0.08 | −0.15–0.15 | — | |
| Eye gaze | 0.08 | 0.08 | −0.07–0.24 | — | ||
| Emotional support | Empathy | 104 | 0.08 | 0.10 | −0.12–0.28 | — |
| Psychosocial questions | 0.00 | 0.10 | −0.19–0.19 | — | ||
| Psychosocial information | 0.01 | 0.10 | −0.18–0.21 | — | ||
| Eye gaze | −0.02 | 0.10 | −0.22–0.18 | — | ||
| Assessment of cancer susceptibility | Medical information | 105 | 0.07 | 0.09 | −0.09–0.24 | — |
| Cancer-specific need | ||||||
| Determination/meaning of cancer gene | Medical information | 146 | 0.20 | 0.08 | 0.04–0.36 | 0.017* |
| Emotional aspects of counseling for | Empathy | 118 | 0.16 | 0.09 | −0.02–0.34 | — |
| counselee/family | Psychosocial questions | −0.07 | 0.08 | −0.23–0.10 | — | |
| Psychosocial information | −0.18 | 0.11 | −0.39–0.03 | — | ||
| Medical information | 0.31 | 0.11 | 0.09–0.52 | 0.005* | ||
| Counselee own risk of cancer | Empathy | 122 | 0.14 | 0.09 | −0.04–0.32 | — |
| Psychosocial questions | −0.05 | 0.09 | −0.22–0.12 | — | ||
| Psychosocial information | −0.21 | 0.11 | −0.44–0.01 | — | ||
| Medical information | 0.23 | 0.11 | 0.02–0.45 | 0.030 | ||
| Heredity of cancer | Medical information | 82 | −0.12 | 0.11 | −0.34–0.10 | — |
Note. CI = Confidence Interval.
— = P > 0.061.
*Significant after Bonferroni-Holmes correction, overall α = 0.05.
aAll analyses were controlled for counselor and counselee background variables.
bSignificance of predictors was tested using Chi-square tests.
cA negative association was expected between need and this communication aspect.
Table III.
Pre- and Post-Visit Internal Consistenciesa of the Various Needs, and Mean Levels and Standard Deviation of Post-Visit Need Fulfillment (Scale 1–4) in Counselees Who Considered Need Important Pre-Visit
| Post-visit fulfillment | ||||||
|---|---|---|---|---|---|---|
| Pre-visit need | Items (n)b | α pre-visit | α post-visit | N | M | SD |
| Generic need | ||||||
| Procedural aspect of counseling | 8 | 0.85 | 0.82 | 131 | 3.20 | 0.50 |
| Sensitive communication | 8 | 0.83 | 0.92 | 166 | 3.50 | 0.47 |
| Emotional support | 5 | 0.79 | 0.78 | 104 | 3.09 | 0.57 |
| Assessment of cancer susceptibility | 3 | 0.66 | 0.66 | 105 | 3.30 | 0.53 |
| Cancer-specific need | ||||||
| Determination/meaning of cancer gene | 7 | 0.82 | 0.91 | 146 | 3.15 | 0.65 |
| (Emotional) aspects of counseling | 5 | 0.72 | 0.83 | 118 | 3.00 | 0.62 |
| Counselee own risk of cancer | 3 | 0.83 | 0.83 | 122 | 3.00 | 0.67 |
| Heredity of cancer | 3 | 0.76 | 0.72 | 82 | 3.22 | 0.66 |
aComputed over N = 171.
bOne generic and one cancer-specific item were left out as they loaded < 0.40 on any dimension.
Communication and Counselees’ Post-Visit Satisfaction, Cognitions, and Anxiety
Asking medical questions was related to lower levels of satisfaction and receiving medical information was related to higher levels of correct knowledge (Table I). Receiving psychosocial information was related to higher levels of anxiety. Visit length was related to higher levels of correct knowledge. Counselor eye gaze was associated with higher levels of correct knowledge and anxiety. The latter association remained significant after controlling for visit length (Beta = 0.27, SE = 0.12, P = 0.022). Counselor communication was unrelated to perceived control.
Table IV.
Counselee Demographics, History of Cancer and Indication for DNA-Testing (N = 171)
| N | % | |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 45.0 (10.2) | |
| Range | 18–72 | |
| Gender | ||
| Female | 155 | 91 |
| Male | 16 | 9 |
| Education | ||
| High school level | 93 | 55 |
| Secondary level | 77 | 45 |
| Type of cancer | ||
| Breast cancer | 109 | 64 |
| Colon cancer | 35 | 21 |
| Breast and colon cancer | 9 | 5 |
| Ovarian cancer | 9 | 5 |
| Other cancers | 9 | 5 |
| Personal history of cancer | ||
| Counselee affected with cancer | 83 | 49 |
| Counselee unaffected with cancer | 88 | 51 |
| Family history of cancer | ||
| 1st or 2nd degree relatives affected with cancer | 151 | 90 |
| No 1st or 2nd degree relatives affected with cancer | 17 | 10 |
| DNA-test | ||
| Indicateda | 102 | 62 |
| Not indicated | 32 | 19 |
| Uncertainb | 31 | 19 |
Note. Summations vary due to missing data.
aIndication for testing the counselee or a relative as judged after the initial visit.
bIndication for testing uncertain after the initial visit due to missing medical information.
Counselor Communication and Counselees’ Perception of Needs Fulfillment
The counselees who considered it important to receive explanations on determination and implications of carrying a cancer gene or (emotional) aspects of counseling, perceived these needs as significantly better fulfilled, if they had received more medical information (Table II). Counselor communication was further unrelated to counselees’ perceptions of need fulfillment.
Table V.
Mean Levels and Standard Deviation on Pre- and Post-Visit Measures
| Pre-visit | Post-visit | |||||
|---|---|---|---|---|---|---|
| Outcome measure | Scale | N | M | SD | M | SD |
| Satisfaction | 8–80 | 165 | — | — | 63.27 | 9.37 |
| Correct knowledgea | 0–1 | 153 | 0.67 | 0.20 | 0.83*** | 0.19 |
| Perceived control (PPC)b | 0–2 | 156 | 1.10 | 0.45 | 1.35*** | 0.45 |
| Anxiety (STAI)b | 10–40 | 160 | 20.63 | 6.24 | 18.32*** | 6.10 |
Note. Samples sizes vary due to missing values.
aWilcoxon signed ranks test.
bt-test for paired samples.
***P < 0.001.
Analyses were reran in the whole sample (N = 171), controlling for pre-visit importance scores on needs. Similar results were found (data not shown). Results further showed that importance scores were unrelated to the perceived fulfillment of the various needs, except for counselor sensitive communication, where importance was positively related to perception of need addressed (data not shown).
DISCUSSION
This study was designed to enhance understanding of how communication during initial cancer genetic counseling visits relates to counselee satisfaction and post-visit cognitions and anxiety, and how counselor communication is associated with addressing counselees’ pre-visit needs.
As with cancer patients, results showed that the counselees were less satisfied if they had asked more medical questions (Ong et al., 2000; Siminoff et al., 2000). It is unclear whether counselees asked medical questions out of discontent with the information they were receiving, or whether asking questions in itself was related to lower satisfaction, perhaps inducing a feeling that they needed to be active in order to receive all desired information. Alternatively, counselees may have had the impression that questions were not welcome. Siminoff et al. (2000) suggested that patients asking more questions are more prepared and may thus have higher expectations of the physician and/or information. Yet, in our sample considering needs more important was unrelated to perceptions of need fulfillment, except for counselor's sensitive communication. Seemingly, these counselees’ dissatisfaction had mainly to do with how the visit proceeded.
As expected and in line with findings in primary care (Hall et al., 1988), counselees who received more medical information had more correct knowledge after the visit, regardless of prior knowledge. Counselees who were looked at longer and who had longer visits also reported more correct knowledge after the visit. These results contradict those from Butow et al. (1995) in cancer patients. As discussed in Bensing et al. (1995), length of eye gaze and of the visit are strongly interrelated; however what causal mechanism actually shapes this relationship is unclear. Evidently, looking more at counselees may provide counselors with more cues as to counselees’ understanding of the information, and longer visits may be associated with taking more time to explain medical matters. Alternatively, when looked at longer, counselees may sense greater counselor interest and may then listen more carefully, retaining the information better (Larsen & Smith, 1981).
In line with Lobb et al.'s (2004) findings, counselees’ anxious feelings were associated with attention given to emotional matters, i.e. counselors’ talk about psychosocial issues. Previously (Pieterse et al., 2005b), we found that lower anxiety was related to perceiving one's need for emotional support better fulfilled. Apparently, addressing counselees’ need for emotional support is not (only) achieved by providing (more) psychosocial information. In line with Duric et al.'s (2003) results, counselor empathy was unrelated to counselees’ satisfaction and anxiety. Our finding that counselees’ anxiety was related to counselor eye gaze, may directly be related to the extensiveness of talk on emotional matters. As anxiety was measured shortly after the visit, follow-up data are necessary to determine whether heightened anxiety levels persisted. Evidence suggests it often does not (Aktan-Collan et al., 2001; Van Oostrom et al., 2003). In principle, it is not surprising that discussing emotional matters does not reduce anxiety, the more so if counselees’ anxious feelings are addressed as being legitimate. Differently from Lobb et al. (2004), receiving medical information did not relieve anxiety but appeared unrelated, suggesting that receiving medical information is not necessarily anxiety-provoking nor-diminishing. This is in line with findings in patients, which show that providing fuller information (on prognosis or test results) does not usually lead to adverse reactions (Ley, 1982). Differences between Lobb et al.'s and our findings may be explained by varying measurements; we did not differentiate the medical information in content. Understandably, it is not amount but rather what information is given, that may help relieve fears.
Unexpectedly, communication was unrelated to perceived control. Perceived control may particularly be related to specific information about what to expect (McVey et al., 2001). Berkenstadt et al. (1999) found more perceived control among counselees seeking counseling for various genetic conditions and who had been given a definite diagnosis, a specific recurrence risk, or were offered prenatal diagnosis. In initial cancer genetic counseling visits, the family history of cancer often needs to be assessed further and (if conducted) results from genetic testing are not yet available. Associations may thus rather be found in concluding visits. Moreover, satisfaction and anxiety were unrelated to discussing counselees’ agenda. Eliciting counselees’ agenda is considered as helpful in better addressing counselees’ needs (Lerman et al., 1995; Michie et al., 1997b). As Butow and Lobb (2004) found, counselors asked counselees about their agenda in most (95%) visits. However, it is unclear to what extent counselees’ agenda was indeed followed.
Regarding perceptions of fulfillment of major needs, it appeared that providing medical information is helpful in addressing well need for explanations on some, but not all, medical and emotional issues. Findings were similar within the whole sample of counselees, suggesting that importance attached to needs was not critical to these associations. Lack of association between medical information and meeting the need for explanation on several medical issues may result from a ceiling effect, as counselees were overall satisfied or very satisfied about their fulfillment.
Counselees’ need for emotional support and explanations on (emotional) aspects of counseling and their risk of cancer were not better fulfilled with more counselor empathy, psychosocial communication, or longer eye gaze. With regard to own risk of cancer, some authors (Meiser et al., 2001) suggested that counseling healthy women about breast cancer risks is effective unless also addressing anxious preoccupations. Our data do not support an association between counselor empathy and psychosocial communication, and counselees’ satisfaction about information on their own risk. However, communicating empathy and being attentive to psychosocial issues may still be helpful in increasing counselees’ correct interpretation and recall of risk information.
LIMITATIONS
This study was based on one clinic and the response rate of counselees, discussed elsewhere (Pieterse et al., 2005a), was low. Most participants were female and a majority was referred for hereditary breast cancer. Furthermore, 55% of counselees were higher educated, a proportion similar to that found in another study amongst Dutch counselees (Van Asperen et al., 2002), however appreciably higher than in Dutch adult general practice patients (Van Lindert et al., 2004). The results should therefore only be generalized with caution to men, to the broader population of relatively lower educated females at increased risk of cancer, and to other types of hereditary cancers.
Second, 15/171 counselees did not return the post-visit questionnaire, and they attached more importance to several pre-visit needs than those who did. It is unclear whether non-response was related to lower need fulfillment.
Third, expected group differences were unknown at the start of the study, so an a priori power analysis to determine the number of counselees needed was not possible. Sample sizes may have been too small to detect differences.
Finally, communication was assessed during initial visits; associations may be different in return visits (Graugaard et al., 2005), especially if increased risk of cancer is demonstrated.
CONCLUSION
The provision of medical information appears the most powerful communication aspect to increase counselees’ satisfaction and fulfill needs on explanations about hereditary cancer. This finding is concordant with the primary goal of counseling, which is to inform and educate counselees about risk of cancer and risk management. Reservations in this regard do not appear necessary, as receiving medical information does not seem related to feeling more anxious. A recent meta-analysis supports this contention (Braithwaite et al., 2004). In contrast, ways need to be found as to address counselees’ medical questions satisfactorily. Also, affective and psychosocial communication was found unrelated or even contrary to relieving counselees’ worries or addressing their need for emotional support. No indications were found as to how communication may help increase counselees’ feelings of control. More research is needed in finding ways to address adequately counselees’ informational and emotional needs, and increase their feelings of control.
Appendix A
| 1. The expertise of the counselor(s) | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 2. The communication of the counselor(s) with you (and your partner) | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 3. The degree of ‘client-centeredness,’ that is, the degree to which the counseling was tuned to you | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 4. The information that the counselor(s) gave you | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 5. The manner in which norms and values that are important to you were discussed | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 6. The degree to which you experience the Department of Medical Genetics as accessible for advice | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 7. The organization, structure, and procedures of the Department of Medical Genetics | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 8. This consultation in general | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
Appendix B.
Counselor (CR) and counselee (CE) communication categories used in the analyses
| Categories used in analyses | Component categories (if applicable) | Explanation of category |
|---|---|---|
| Socio-emotional communication | ||
| CR Empathy | Concern | Immediate emotional or psychosocial worries |
| Verbal attention | Legitimize, empathy, partnership, support | |
| Reassurance | Give reassurance | |
| CE Concern | --- | Immediate emotional or psychosocial worries |
| Task-related communication | ||
| CR Medical information | — | Statements or facts relating to medical condition or screening or prophylactic surgery |
| CE Medical questions | — | Questions that ask for information on medical condition or screening or prophylactic surgery |
| CR Psychosocial questions | — | Questions that ask for information on psychosocial issuesa or current feelings |
| CR Psychosocial information | CR Psychosocial information | Statements or facts relating to psychosocial issuesa or current feelings |
| CR Psychosocial education | Statements which suggest resolution or action to be taken by the other relating to psychosocial issuesa or statements aimed at education about psychosocial issuesa | |
| Discuss CE Agenda | CR question Agenda | Questions that ask for information on CE's agenda |
| CE information Agenda | Statements or facts relating to CE's agenda | |
| Discuss CE Psychosocial issues | CR Psychosocial questions | Questions that ask for information on psychosocial issuesa or current feelings |
| CE Psychosocial information | Statements or facts relating to psychosocial issuesa or current feelings | |
| Overall communication measures | ||
| CR verbal dominance | — | Computed as the ratio of all CR utterances to the total count of utterances during the visit |
| CR Eye gaze | — | Length in minutes of time that the CR looks directly into the face of the CE or his/her companion(s) |
aPsychosocial issues encompass the discussion of feelings and emotions that are not active at the moment, as well as discussion about ways in which counselees (or relatives) make decisions related to the problem for which they sought counseling.
ACKNOWLEDGMENTS
The authors wish to thank the participating counselees and counselors for their efforts during the study period. This study was supported by a grant from the Dutch Cancer Society.
APPENDIX
Items Used for Measuring Satisfaction
Finally, we ask about your satisfaction about the consultation you just had at the Department of Medical Genetics. Below, you may express your satisfaction using a report mark from 1 (very bad) to 10 (excellent). Please, circle one mark for each question.
To what extent are you satisfied about …
REFERENCES
- Aalfs C. M., Oort F., De Haes H. C. J. M., Leschot N. J., Smets E. M. A. Counselor-counselee interaction in reproductive genetic counseling: Does a pregnancy in the counselee make a difference? Patient Educ. Couns. 2006;60:80–90. doi: 10.1016/j.pec.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Aktan-Collan K., Haukkala A., Mecklin J. P., Uutela A., Kaariainen H. Psychological consequences of predictive genetic testing for hereditary non-polyposis colorectal cancer (HNPCC): A prospective follow-up study. Int. J. Cancer. 2001;93:608–611. doi: 10.1002/ijc.1372. [DOI] [PubMed] [Google Scholar]
- Armstrong D., Michie S., Marteau T. Revealed identity: A study of the process of genetic counselling. Soc. Sci. Med. 1998;47:1653–1658. doi: 10.1016/S0277-9536(98)00241-X. [DOI] [PubMed] [Google Scholar]
- ASCO Statement of the American Society of Clinical Oncology: Genetic testing for cancer susceptibility. J. Clin. Oncol. 1996;14:1730–1736. doi: 10.1200/JCO.1996.14.5.1730. [DOI] [PubMed] [Google Scholar]
- Benkendorf J. L., Prince M. B., Rose M. A., De Fina A., Hamilton H. E. Does indirect speech promote nondirective genetic counseling? Results of a sociolinguistic investigation. Am. J. Med. Genet. 2001;106:199–207. doi: 10.1002/ajmg.10012. [DOI] [PubMed] [Google Scholar]
- Bensing J. Doctor-patient communication and the quality of care. Soc. Sci. Med. 1991;32:1301–1310. doi: 10.1016/0277-9536(91)90047-G. [DOI] [PubMed] [Google Scholar]
- Bensing J. M., Kerssens J. J., Van der Pasch M. Patient-directed gaze as a tool for discovering and handling psychosocial problems in general practice. J. Nonverbal Behav. 1995;19:223–242. doi: 10.1007/BF02173082. [DOI] [Google Scholar]
- Berkenstadt M., Shiloh S., Barkai G., Bat-Miriam Katznelson M., Goldman B. Perceived personal control (PPC): A new concept in measuring outcome of genetic counseling. Am. J. Med. Genet. 1999;82:53–59. doi: 10.1002/(SICI)1096-8628(19990101)82:1<53::AID-AJMG11>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- Bertakis K. D., Roter D., Putnam S. M. The relationship of physician medical interview style to patient satisfaction. J. Fam. Pract. 1991;32:175–181. [PubMed] [Google Scholar]
- Biesecker B. B. Goals of genetic counseling. Clin. Genet. 2001;60:323–330. doi: 10.1034/j.1399-0004.2001.600501.x. [DOI] [PubMed] [Google Scholar]
- Biesecker B. B., Peters K. F. Process studies in genetic counseling: Peering into the black box. Am. J. Med. Genet. 2001;106:191–198. doi: 10.1002/ajmg.10004. [DOI] [PubMed] [Google Scholar]
- Braithwaite D., Emery J., Walter F., Prevost A. T., Sutton S. Psychological impact of genetic counseling for familial cancer: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2004;96:122–133. doi: 10.1093/jnci/djh017. [DOI] [PubMed] [Google Scholar]
- Butow P. N., Dunn S. M., Tattersall M. H., Jones Q. J. Computer-based interaction analysis of the cancer consultation. Br. J. Cancer. 1995;71:1115–1121. doi: 10.1038/bjc.1995.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butow P., Lobb E. Analyzing the process and content of genetic counseling in familial breast cancer consultations. J. Genet. Couns. 2004;13:403–424. doi: 10.1023/B:JOGC.0000044201.73103.4f. [DOI] [PubMed] [Google Scholar]
- Claes E., Evers-Kiebooms G., Boogaerts A., Decruyenaere M., Denayer L., Legius E. Communication with close and distant relatives in the context of genetic testing for hereditary breast and ovarian cancer in cancer patients. Am. J. Med. Genet. 2003;116A:11–19. doi: 10.1002/ajmg.a.10868. [DOI] [PubMed] [Google Scholar]
- Collins V., Halliday J., Warren R., Williamson R. Assessment of education and counselling offered by a familial colorectal cancer clinic. Clin. Genet. 2000;57:48–55. doi: 10.1034/j.1399-0004.2000.570107.x. [DOI] [PubMed] [Google Scholar]
- Duric V., Butow P., Sharpe L., Lobb E., Meiser B., Barratt A. Reducing psychological distress in a genetic counseling consultation for breast cancer. J. Genet. Couns. 2003;12:243–264. doi: 10.1023/A:1023284219871. [DOI] [PubMed] [Google Scholar]
- Ellington L., Roter D., Dudley W. N., Baty B. J., Upchurch R., Larson S. Communication analysis of BRCA1 genetic counseling. J. Genet. Couns. 2005;14:377–386. doi: 10.1007/s10897-005-3660-3. [DOI] [PubMed] [Google Scholar]
- Graugaard P. K., Holgersen K., Eide H., Finset A. Changes in physician-patient communication from initial to return visits: A prospective study in a haematology outpatient clinic. Patient Educ. Couns. 2005;57:22–29. doi: 10.1016/j.pec.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Hall J. A., Roter D. L., Katz N. R. Meta-analysis of correlates of provider behavior in medical encounters. Med. Care. 1988;26:657–675. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- Holland B. S., Copenhaver M. D. Improved Bonferroni-type multiple testing procedures. Psychol. Bull. 1988;104:145–149. doi: 10.1037/0033-2909.104.1.145. [DOI] [Google Scholar]
- Holloway S., Porteous M., Cetnarskyj R., Anderson E., Rush R., Fry A. Patient satisfaction with two different models of cancer genetic services in south-east Scotland. Br. J. Cancer. 2004;90:582–589. doi: 10.1038/sj.bjc.6601562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler S., Jacopini A. G. Psychological aspects of genetic counseling. II: Quantitative analysis of a transcript of a genetic counseling session. Am. J. Med. Genet. 1982;12:421–435. doi: 10.1002/ajmg.1320120406. [DOI] [PubMed] [Google Scholar]
- Larsen K. M., Smith C. K. Assessment of nonverbal communication in the patient-physician interview. J. Fam. Pract. 1981;12:481–488. [PubMed] [Google Scholar]
- Lerman C., Lustbader E., Rimer B., Daly M., Miller S., Sands C. Effects of individualized breast cancer risk counseling: A randomized trial. J. Natl. Cancer Inst. 1995;87:286–292. doi: 10.1093/jnci/87.4.286. [DOI] [PubMed] [Google Scholar]
- Ley P. Satisfaction, compliance and communication. Br. J. Clin. Psychol. 1982;21:241–254. doi: 10.1111/j.2044-8260.1982.tb00562.x. [DOI] [PubMed] [Google Scholar]
- Lobb E. A., Butow P., Barratt A., Meiser B., Tucker K. Differences in individual approaches: Communication in the familial breast cancer consultation and the effect on patient outcomes. J. Genet. Couns. 2005;14:43–53. doi: 10.1007/s10897-005-1499-2. [DOI] [PubMed] [Google Scholar]
- Lobb E. A., Butow P. N., Barratt A., Meiser B., Gaff C., Young M. A. Communication and information-giving in high-risk breast cancer consultations: Influence on patient outcomes. Br. J. Cancer. 2004;90:321–327. doi: 10.1038/sj.bjc.6601502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McVey J., Madill A., Fielding D. The relevance of lowered personal control for patients who have stoma surgery to treat cancer. Br. J. Clin. Psychol. 2001;40:337–360. doi: 10.1348/014466501163841. [DOI] [PubMed] [Google Scholar]
- Mead N., Bower P., Hann M. The impact of general practitioners’ patient-centredness on patients’ post-consultation satisfaction and enablement. Soc. Sci. Med. 2002;55:283–299. doi: 10.1016/S0277-9536(01)00171-X. [DOI] [PubMed] [Google Scholar]
- Meiser B., Butow P., Baratt A., Gattas M., Gaff C., Haan E. Risk perceptions and knowledge of breast cancer genetics in women at increased risk of developing hereditary breast cancer. Psychol. Health. 2001;16:297–311. doi: 10.1080/08870440108405508. [DOI] [Google Scholar]
- Meiser B., Halliday J. L. What is the impact of genetic counselling in women at increased risk of developing hereditary breast cancer? A meta-analytic review. Soc. Sci. Med. 2002;54:1463–1470. doi: 10.1016/S0277-9536(01)00133-2. [DOI] [PubMed] [Google Scholar]
- Michie S., Bron F., Bobrow M., Marteau T. M. Nondirectiveness in genetic counseling: An empirical study. Am. J. Hum. Genet. 1997;60:40–47. [PMC free article] [PubMed] [Google Scholar]
- Michie S., Lester K., Pinto J., Marteau T. M. Communicating risk information in genetic counseling: An observational study. Health Educ. Behav. 2005;32:589–598. doi: 10.1177/1090198105278562. [DOI] [PubMed] [Google Scholar]
- Michie S., McDonald V., Marteau T. M. Genetic counselling: Information given, recall and satisfaction. Patient Educ. Couns. 1997;32:101–106. doi: 10.1016/S0738-3991(97)00050-5. [DOI] [PubMed] [Google Scholar]
- Ong L. M., Visser M. R., Lammes F. B., de Haes J. C. Doctor-patient communication and cancer patients’ quality of life and satisfaction. Patient Educ. Couns. 2000;41:145–156. doi: 10.1016/S0738-3991(99)00108-1. [DOI] [PubMed] [Google Scholar]
- Pieterse A., Van Dulmen S., Ausems M., Schoemaker A., Beemer F., Bensing J. QUOTE-geneca: Development of a counselee-centered instrument to measure needs and preferences in genetic counseling for hereditary cancer. Psychooncology. 2005;14:361–375. doi: 10.1002/pon.853. [DOI] [PubMed] [Google Scholar]
- Pieterse A. H., Ausems M. G., Van Dulmen A. M., Beemer F. A., Bensing J. M. Initial cancer genetic counseling consultation: Change in counselees’ cognitions and anxiety, and association with addressing their needs and preferences. Am. J. Med. Genet. A. 2005;137:27–35. doi: 10.1002/ajmg.a.30839. [DOI] [PubMed] [Google Scholar]
- Pieterse A. H., Van Dulmen A. M., Ausems M. G. E. M., Beemer F. A., Bensing J. M. Communication in cancer genetic counselling: Does it reflect counselees’ pre-visit needs and preferences? Br. J. Cancer. 2005;92:1671–1678. doi: 10.1038/sj.bjc.6602570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilnick A. ‘There are no rights and wrongs in these situations’: Identifying interactional difficulties in genetic counselling. Soc. Health Illn. 2002;24:66–88. doi: 10.1111/1467-9566.00004. [DOI] [Google Scholar]
- Pilnick A., Dingwall R. Research directions in genetic counselling: A review of the literature. Patient Educ. Couns. 2001;44:95–105. doi: 10.1016/S0738-3991(00)00181-6. [DOI] [PubMed] [Google Scholar]
- Richards M. P. Genetic counselling for those with a family history of breast or ovarian cancer–current practice and ethical issues. Acta Oncol. 1999;38:559–565. doi: 10.1080/028418699431131. [DOI] [PubMed] [Google Scholar]
- Richards M. P. M., Hallowell N., Green J. M., Murton F., Statham H. Counseling families with hereditary breast and ovarian cancer: A psychological perspective. J. Genet. Couns. 1995;4:219–233. doi: 10.1007/BF01408411. [DOI] [PubMed] [Google Scholar]
- Roter D., Larson S. The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Educ. Couns. 2002;46:243–251. doi: 10.1016/S0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Roter D., Lipkin M., Jr., Korsgaard A. Sex differences in patients’ and physicians’ communication during primary care medical visits. Med. Care. 1991;29:1083–1093. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- Roter D. L., Stewart M., Putnam S. M., Lipkin M., Jr., Stiles W., Inui T. S. Communication patterns of primary care physicians. JAMA. 1997;277:350–356. doi: 10.1001/jama.1997.03540280088045. [DOI] [PubMed] [Google Scholar]
- Rutter D. R., Iconomou G., Quine L. Doctor-patient communication and outcome in cancer patients: An intervention. Psychol. Health. 1996;12:57–71. doi: 10.1080/08870449608406922. [DOI] [Google Scholar]
- Siminoff L. A., Ravdin P., Colabianchi N., Sturm C. M. Doctor-patient communication patterns in breast cancer adjuvant therapy discussions. Health Expect. 2000;3:26–36. doi: 10.1046/j.1369-6513.2000.00074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smets E. M., Pieterse A. H., Aalfs C. M., Ausems M. G. E. M., Dulmen A. M. The perceived personal control (PPC) questionnaire as an outcome of genetic counseling: Reliability and validity of the instrument. Am J Med Genet A. 2006;140:843–850. doi: 10.1002/ajmg.a.31185. [DOI] [PubMed] [Google Scholar]
- Smith J. A., Michie S., Allanson A., Elwy R. Certainty and uncertainty in genetic counselling: A qualitative case study. Psychol. Health. 2000;15:1–12. doi: 10.1080/08870440008400284. [DOI] [PubMed] [Google Scholar]
- Van Asperen C., Van Dijk S., Zoeteweij M. W., Timmermans D. R., De Bock G. H., Meijers-Heijboer E. J. What do women really want to know? Motives for attending familial breast cancer clinics. J. Med. Genet. 2002;39:410–414. doi: 10.1136/jmg.39.6.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Ploeg, H. M., Defares, P. B., & Spielberger, C. D. (1980). Handleiding bij de Zelfbeoordelings Vragenlijst (ZBV) [Manual of the Dutch version of the State Trait Anxiety Inventory]. Lisse: Swets and Zeitlinger.
- Van Lindert, H., Droomers, M., & Westert, G. P. (2004). Een kwestie van verschil: Verschillen in zelfgerapporteerde leefstijl, gezondheid en zorggebruik [A matter of difference: Differences in self-reported lifestyle, health and use of care]. Utrecht: Nivel.
- Van Oostrom I., Meijers-Heijboer H., Lodder L. N., Duivenvoorden H. J., van Gool A. R., Seynaeve C. Long-term psychological impact of carrying a BRCA1/2 mutation and prophylactic surgery: A 5-year follow-up study. J. Clin. Oncol. 2003;21:3867–3874. doi: 10.1200/JCO.2003.10.100. [DOI] [PubMed] [Google Scholar]
- van Zuuren F. J. The standard of neutrality during genetic counselling: An empirical investigation. Patient Educ. Couns. 1997;32:69–79. doi: 10.1016/S0738-3991(97)00051-7. [DOI] [PubMed] [Google Scholar]
- van Zuuren F. J., van Schie E. C., van Baaren N. K. Uncertainty in the information provided during genetic counseling. Patient Educ. Couns. 1997;32:129–139. doi: 10.1016/S0738-3991(97)00052-9. [DOI] [PubMed] [Google Scholar]
- Wang C., Gonzalez R., Merajver S. D. Assessment of genetic testing and related counseling services: Current research and future directions. Soc. Sci. Med. 2004;58:1427–1442. doi: 10.1016/S0277-9536(03)00337-X. [DOI] [PubMed] [Google Scholar]